Abstract
Background
The global prevalence of abnormal glycemic level comprising diabetes mellitus (DM) and pre-diabetes (PDM) is rapidly increasing with special concern for the entity silent or undiagnosed diabetes; those unaware of their condition. Identification of people at risk became much easier with the use of risk charts than the traditional methods. The current study aimed to conduct a community-based screening for T2DM to estimate the prevalence of undiagnosed DM and to assess the AUSDRISK Arabic version as a predictive tool in an Egyptian context.
Methods
A cross-sectional study was conducted among 719 Adults aging 18 years or more and not known to be diabetics through a population-based household survey. Each participant was interviewed to fill demographic and medical data as well as the AUSDRISK Arabic version risk score and undergo testing for fasting plasma glucose (FPG) and oral glucose tolerance test (OGTT).
Results
The prevalence of DM and PDM were 5% and 21.7% respectively. The multivariate analysis revealed that age, being physically inactive, history of previous abnormal glycemic level and waist circumference were the predictors for having abnormal glycemic level among the studied participants. At cut off points ≥ 13 and ≥ 9, the AUSDRISK respectively discriminated DM [sensitivity (86.11%), specificity (73.35%), and area under the curve (AUC): 0.887, 95% CI: 0.824–0.950] and abnormal glycemic level [sensitivity (80.73%), specificity (58.06%), and AUC: 0.767, 95% CI: 0.727–0.807], p < 0.001.
Conclusions
Overt DM just occupies the top of an iceberg, its unseen big population have undiagnosed DM, PDM or been at risk of T2DM because of sustained exposure to the influential risk factors. The AUSDRISK Arabic version was proved to be sensitive and specific tool to be used among Egyptians as a screening tool for the detection of DM or abnormal glycemic level. A prominent association has been demonstrated between AUSDRISK Arabic version score and the diabetic status.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM) is a metabolic disorder of multiple etiology characterized by chronic hyperglycemia with disturbances of carbohydrate, fats and protein metabolism resulting from defects in insulin secretion, insulin action or both [1].
Its global prevalence is rapidly increasing. According to the International Diabetic Federation (IDF), it was estimated that nearly 537 million adults (10.5%) all over the world suffer from DM in 2021. Almost one in two (240 million; 44.7%) adults with diabetes are unaware that they have the condition (undiagnosed diabetes) and nearly 90% of diabetic cases are type 2 DM (T2DM). This global estimate is expected to rise to 643 million (11.3%) in 2030 and to 783 million (12.2%) by 2045. The majority of diabetic patients (75%) had their residence in low and middle income countries (LMICs). [1, 2] Along with DM, the magnitude of pre-diabetes (PDM) in the form of impaired glucose tolerance (IGT) and impaired fasting glucose (IFG) is rising worldwide. According to the IDF, worldwide there were 860 million pre-diabetic adults in 2021 (16.8%) and projected to be 992 million (17.5%) and 1171 million (18.3%) by 2030 and 2045 respectively. Those persons are at a very high risk of develo** T2DM. As regards Egypt, it was estimated that 10.9 million had diabetes and this number is expected to rise to 13 million by 2030 and to 20 million by 2045. This makes Egypt to rank in the 10th position among countries with highest prevalence of DM and is expected to be in the 9th position by 2045 [2,3,4].
Multiple modifiable (such as; obesity, sedentary lifestyle, smoking, high blood pressure and unhealthy diet consumption) and non-modifiable (like; age, ethnicity and family history) risk factors result in the development and progress of T2DM. [5] Those risk factors gave the chronic nature of the disease with a long asymptomatic period. This gave the opportunity to identify those individuals who are likely to have DM while being asymptomatic through screening program for further prophylactic intervention. It was proved by the IDF that the onset of T2DM can be delayed or even prevented through lifestyle modification by physical activity and/or healthy diet. [6]
Screening for early detection of T2DM was set to be a major area of interest by the World Health organization (WHO) and IDF since 2003. This was justified by multiple reasons such as the large proportion of people that are unaware of having DM (undiagnosed DM), the rising prevalence of DM and PDM worldwide, its long asymptomatic latency prior to its clinical overtness give an ample opportunity for its complications, the micro-vascular ones in particular, to occur in a good portion of patients before its diagnosis and the evidence-based efficacy of the intensive control of the blood glucose in patients to break the progression of DM complications. [7,8,9]
Screening is the backbone of T2DM preventive strategy. It aims to screen the asymptomatic apparently healthy people to find undiagnosed T2DM, PDM and those who are vulnerable (at risk) to get T2DM followed by appropriate non-pharmaceutical and/ or pharmaceutical intervention to prevent or delay its occurrence. At first screening programs for DM were exclusively one step that implies direct testing by the common invasive, inconvenient, and expensive laboratory tests including the 2-hour oral glucose tolerance test (OGTT), fasting plasma glucose (FPG), or the glycated hemoglobin (HbA1c). A two-step screening has recently evolved and get more popular worldwide. In the first step, the individuals are pre-screened using either risk scoring questionnaires to distinguish those at risk who will undergo diagnostic lab testing in the second step. [10]
Several non-invasive screening risk score charts have been developed and proved to be feasible, less time consuming, and cost effective in detecting T2DM in comparison to the traditional screening that relied for long time on invasive, inconvenient, and expensive techniques including blood sampling. [11, 12] The Finnish Diabetes Risk Score (FINDRISC) has been widely adopted in many European countries and proved to be a valid inexpensive risk assessment tool for T2DM. The German Diabetes Risk Score (GDRS) is another model for identification of individuals at high risk for T2DM and screening for undiagnosed DM, in the German population. [13, 14]
The Australian type 2 Diabetes Risk assessment tool (AUSDRISK) was developed by the Australian Commonwealth Department of Health and Ageing in 2008 to estimate the probability of a person develo** T2DM within the next five years based on multiple risk factors [15]. It was rec alibrated into Arabic language and the AUSDRISK Arabic version was proved to be useful in an Egyptian context as a valid and reliable predictive tool. [16]
The bottom line is that T2DM is an ever-growing, ever-expanding disease of chronic natural history preceded by a long asymptomatic period and causes a variety of debilitating micro-vascular and macro-vascular complications that adversely affect individual health and productivity. The current study refers to the community-based screening as an invaluable approach to reach the apparently healthy individuals who are at risk of T2DM for early appropriate non-pharmaceutical and pharmaceutical intervention.
Methods
The current study aimed to conduct a community-based screening for T2DM to estimate the prevalence of undiagnosed DM and to assess the AUSDRISK Arabic version as a screening tool among Egyptians.
A cross-sectional study was conducted at Damanhur district of El Behera Governorate in Egypt. Based on the prevalence of undiagnosed DM was about 5% [2]. A minimum required sample of 706 adults was required to detect a sensitivity with 81.3% of AUSDRISK. [17] By using precision = 5% with alpha error = 0.05. [18] 719 adults were eligible for the participation of this study aging 18 years or more and not known to be diabetics (as revealed by history taking) and recruited to participate in the study with exclusion of pregnant females or those who had advanced decompensated organ disease.
Sampling approach was adopted at first using simple random sampling, Damanhur district was selected among the 15 districts of El Behera governorate. Then WHO multistage cluster sampling technique was adopted in Damanhur district through the identification of 30 clusters to be involved in the study. Proportional allocation was used in selecting the clusters whereby two thirds (20 clusters) and one third (10 clusters) were rural and urban clusters respectively as adult population in rural areas is approximately double that of urban ones [19]. From each cluster ten households were selected and involved in the study. The selection method was started at the center of each selected cluster. The direction of selection was randomly determined using rotation bottle. The first household was randomly selected as well (as the first person came out). The second household would be the next one with an entrance adjacent to the first selected one and so on. All eligible adults within each household were included in the study. The number of adults per household ranged from 1 to 4.
Each participant was interviewed face to face to fill: (a) Demographic data entailing age, sex, marital status, education level, and residence. (b) Habitual data comprising smoking, physical activity and fruits/vegetables consumption. (c) Medical data upon abnormal lipid profile or hypertension and family history of DM. (d) The AUSDRISK Arabic version which contain 9 questions including the age, the gender, family history of DM, previous history of high blood sugar level, history of hypertension, daily smoking, vegetables and fruits intake, daily physical activity and the measurement of waist circumference. The total score of the AUSDRISK Arabic version was scaled as the following categories (mild risk: ≤ 4 points, moderate risk: 5–10 points and severe risk: ≥ 11 points). [16]
Then they were invited to perform: (a) Anthropometric measurements: weight, height, body mass index (BMI), and waist circumference. BMI is calculated as body weight in kilograms divided by the square of the height in meters (kg/m2) to be fallen into one of the following categories (underweight: <18.5 kg/m2, normal weight: 18.5–24.9 kg/m2, overweight (pre-obesity): 25-29.9 kg/m2, obesity class I: 30-34.9 kg/m2, obesity class II: 35-39.9 kg/m2 and obesity class III: ≥40 kg/m2). [20] (b) Fasting plasma glucose (FPG); plasma glucose level after no caloric intake for at least 8 h. (c) Oral glucose tolerance test (OGTT); plasma glucose level 2 h after intake of 75 g anhydrous glucose dissolved in water used as a glucose load. Participants were diagnosed as diabetics if FPG was ≥ 126 mg/dl or OGTT was ≥ 200 mg/dl and as pre-diabetics if FPG was 110–125 mg/dl or OGTT was 140–199 mg/dl. [21] Participants with pre-diabetes or diabetes were referred to a specialist of internal medicine for management.
Statistical analysis
The collected data were coded, revised, cleaned, tabulated and analyzed through IBM SPSS Statistics version 26 using appropriate statistics [22]. The descriptive statistics including percentages, arithmetic mean and standard deviation (SD) were calculated for various qualitative and quantitative data to describe the study population. The analytic statistical tests comprised Chi squared and student t test. Multivariate logistic regression analysis was done for the studied variables with p value < 0.1 to determine the predictors for having abnormal glycemic level. The receiver operating characteristic curves (ROC) and area under the curve (AUC) were drawn to determine an optimal cutoff point of the AUSDRISK Arabic version to diagnose both DM and abnormal glycemic level and calculate its sensitivity and specificity. P value equal to or less than 0.05 was considered statistically significant.
Results
The socio-demographic features showed that most of the participants were female (69.3%), with mean age of 39.36 ± 14.77 years, married (77.1%) and living in rural areas (67.3%). While 27.8% of the participants were illiterate / Write and read, 25.6% and 40.1% of them completed their higher and middle education, respectively. As regards the habits of the studied participants most of them were nonsmokers (88.3%), physically active (60.5%) and reported eating vegetables or fruits on daily basis (70%). The medical history of the studied participants revealed that 7.2% had history of abnormal glycemic level, 3.1% had abnormal lipid profile, 12.4% had hypertension and 40.3% reported positive family history of DM. [Table 1]
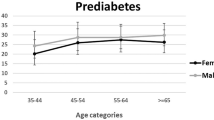
Studied participants overall anthropometric measurements recorded average of 95.42 ± 12.84 cm for waist circumference and 29.28 ± 5.52 kg/m2 for BMI. The BMI frequency was headed by overweight (37.4%) followed by obesity I (27.3%), and normal weight (21.4%). Most of the participants were euglycemic (73.3%, CI: 69.9–76.5%), to a lesser extent pre-diabetic (21.7%, CI: 18.7–24.9%) and the prevalence of undiagnosed DM was 5%, CI: 3.5–6.9%]. The average glycemic level was 92.02 ± 20.43 mg/dl for FPG and 121.54 ± 37.18 mg/dl for OGTT. According to the AUSDRISK Arabic version, 39.4% and 39.1% had moderate and high risk for develo** DM while only 21.5 had mild risk. [Table 2; Fig. 1]
Age owed significant relationship with having abnormal glycemic level. There was significant increment in the mean age among participants having abnormal glycemic level (46.85 ± 14.95) compared to euglycemia (36.64 ± 13.73) (p < 0.001). Salient association of having abnormal glycemic level to lower education among illiterate / read and write (35.5%) and low education level (21.3%) in comparison to the middle (19.4%) ones, p = 0.001. Also urban residency showed higher significant frequency for having abnormal glycemic level (31.5%) than rural areas (24.4%), p = 0.043. Higher frequency having abnormal glycemic level among physically inactive participants (38%) than physically active ones (19.3%) was evident, the differences in between reached significant level, p < 0.001. The recall revealed significant linkage of having abnormal glycemic level to the previous history of high blood sugar (88.8% vs. 21.9%), positive history of hypertension (50.6% vs. 23.3%), and positive family history of DM (34.1% vs. 21.7%) with p < 0.001. The average waist circumference was significantly higher among those having abnormal glycemic level (101.4 ± 12.92 cm) than the euglycemic state (93.25 ± 12.11 cm), p < 0.001. Significant association to BMI was observed where the prevalence of abnormal glycemic level was higher among obese (39.5%) and overweight (20.1%) in comparison to normal weight (13.6%), p < 0.001. None of the gender, smoking, the intake of fruits and vegetables, recall history of abnormal lipid profile had statistically significant connection to the diabetes status. [Table 3]
Multivariate analysis revealed that age, being physically inactive, history of previous abnormal glycemic level and waist circumference were the predictors for having abnormal glycemic level among the studied participants [Table 4].
At a cutoff point of ≥ 13, the sensitivity and specificity of the AUSDRISK Arabic version for detection of undiagnosed DM were 86.11% and 73.35 respectively with 0.887 (confidence interval (CI): 0.824–0.95) area under the curve (AUC), p < 0.001 While the sensitivity and specificity for detection of abnormal glycemic level were 80.73% and 58.06% respectively at a cutoff point ≥ 9 with 0.767 AUC (CI: 0.727–0.807), p < 0.001. [Figure 2]
A dual statistical confirmation of a prominent association between diabetic state and AUSDRISK Arabic version score was proved. DM and PDM participants had a significant higher averaged total AUSDRISK score (19.78 ± 6.44, 12.59 ± 5.53) than the euglycemic ones (7.98 ± 5.09) with F value of 117.419 (P < 0.01). The percentage of DM and PDM increased significantly with AUSDRISK score ≥ 11 (11.4%, 35.6%) compared to the AUSDRISK score 5–10 (1.4%, 15.2%) and AUSDRISK score ≤ 4 (0.00%, 8.4%); X2 = 107.854 (P < 0.01). [Table 5]
Discussion
The burden of T2DM imputes, in part, to its high prevalence. Commonness of T2DM latency and silence adds further burden as they cumulate opportunistic risk for evolution of its micro-vascular and macro-vascular complications. Latency refers to the transition period of PDM that lapses prior to its conversion to T2DM which often takes several years. Silent T2DM represents the undiagnosed/ undetected T2DM. The frequency of undiagnosed T2DM has been noted to reach as high as 50% of patients; they got diagnosed incidentally. In 2019, in the list of top 10 countries with highest number of undiagnosed DM, Egypt booked the eighth seat by 4.8 million adults (20–79 years) not aware of being diseased. [4]
The variability in the prevalence of DM and PDM seen worldwide is multifactorial. Among the implicated factors are the variation in the study type, approach, site, sample size, sampling technique, the diagnostic criteria of glycemic status, characteristics of the involved population (age, gender, ethnicity, etc.). Of note is that high prevalence of undiagnosed DM which reach almost half of the diabetic cases around 5% was a common noteworthy trait in the vast majorities of the studies [2]. In the current study, the biochemical results showed that 73.3%, 21.7% and 5% of the participants had blood glucose levels indicative of euglycemia, PDM, and DM, respectively. It was well evident that 5% of the participants were newly undiagnosed T2DM as none of them was aware of the disease. Close figures for the prevalence of undiagnosed DM have been reported worldwide. In Alexandria, Egypt, a recent cross-sectional study reported a 5.5% age-adjusted prevalence of undiagnosed DM in a sample of 9657 adults aged 18–90 years while delineating the epidemiological profile of DM. [23] A similar prevalence of undiagnosed DM of 5.6% was identified in another cross-sectional study carried out to profile the metabolic syndrome in a sample of 270 adults (> 20 years) recruited from rural and urban districts of Alexandria. [24] Akin undetected DM frequencies of 5.7% and 4.9% were respectively inferred in two separate community-based cross-sectional studies done to investigate the prevalence and risk factors of DM among 402 adults aged 15 + years in Mizan-Aman town, southwest Ethiopia and 587 adults (18 + years) in Dessie Town, Northeast Ethiopia. [25, 26] In Asia, similar findings were reported in a national survey of 18,066 adult Thai population to determine the prevalence of DM; 4.1% of the participants revealed glycemic status consistent with DM. [27]
The increasing prevalence of PDM worldwide is alarming. It constitutes a highly significant expanding reservoir of the futuristic T2DM albeit good proportion of the PDM restore their euglycemia and don’t progress to overt DM. Known DM represents the tip of the iceberg of impaired glucose metabolism where the vast majority of PDM lurks unseen. High prevalence of PDM (latent T2DM) was a worthy finding in the current study where 21.7% of the recruited participants had PDM and were still in the transition period. Comparable with the result of the current study were the elevated prevalence of PDM of 22.4% and 22.3% respectively seen in Peru national population-based survey and the result of a recent meta-analysis. [28, 29] Nevertheless, lower prevalence of PDM of around 15% have been recorded in multiple studies in Egypt and Ethiopia. [23,24,25,26]
The uprising incidence, and prevalence of DM and PDM worldwide didn’t originate from space. It has been strongly attributed to expansion of the avoidable risk factors and the urbanized lifestyle. The American Diabetes Association (ADA) and the National Institute of Diabetes and Digestive and Kidney Diseases have enlisted a set of 11 T2DM and PDM major risk factors. It included 3 unmodifiable; namely are the age 45 + years; risky races/ ethnicities and family history of DM as well as 8 modifiable ones. Those latter are the overweight/ obesity; hypertension or on anti-hypertensive medications; physical inactivity; history of gestational diabetes (GDM) or giving birth of an overweight baby (weight: 9 + pounds), dyslipidemia of low HDL-cholesterol or hypertriglyceridemia; history of cardiovascular stroke; polycystic ovary syndrome and acanthosis nigricans. [30, 31]
In the current study, the univariate analysis revealed 9 risk factors comprising the age, level of education, urban residence, physical inactivity, medical history of high glucose level, history of hypertension, family history of DM as well as the overweight/ obesity and waist circumference, while the multivariate analysis revealed that age, being physically inactive, history of previous abnormal glycemic level and waist circumference were the predictors for having abnormal glycemic level among the studied participants. In agreement with the present results, in Egypt recently it was confirmed an increase in the prevalence of DM among the old age group. In the same vein, the national survey in Thailand, affirmed higher prevalence of DM, undiagnosed DM and PDM in the old age groups in both gender. [23, 27] An inextricable cohesion between DM and ignorance has been frequently proved everywhere. This was seen in Peru where it was asserted a statistically significant association between DM and lower education level in comparison to the higher educational ones. [28] Further proof was illustrated also in Thailand and Egypt. [23, 27] Likewise, the beneficial impact of physical exercise on the glycemic status was robustly shown in recent reviews. The significant benefit of daily 30-minute walking was spotlighted in the control of glycemia, lowering the risk of T2DM by ≈ 50%, decreasing the risk of cardiovascular stroke and its consequent mortality and being a key ingredient of the treatment plan of T2DM. [31,32,33] It is obvious that physical activity did not monopolize the protection against DM development; it used to share it with vegetables and fruits intake abreast. [34, 35] Again in Egypt and Ethiopia, it was endorsed an eminent closeness of DM frequency towards the positive side of the history of hypertension and family history of DM rather than the negative one. [23, 25] In accordance with other studies, the present study provided a titanic testimony to the rationale of the verdict accusing history of dysglycemia as the prime suspect in the causation of having abnormal glycemic level. [36,37,38] Higher frequency of T2DM in overweight/ obese participants than the normal weight ones has been evidenced in different cross-sectional studies. [23,24,25,26, 39] Diabesity is the term adopted to describe the strong co-incidence between T2DM and obesity. [40]
The AUSDRISK Arabic version was proved to be sensitive and specific tool to be used among Egyptians as a screening tool. [16] It was accurate enough in the current study to discriminate undiagnosed T2DM at a cutoff point ≥ 13, (AUC: 887, sensitivity: 86.11% & specificity: 73.35%) and abnormal glycemic level at a cut off > 9 (AUC: 0.767, sensitivity: 80.73% & specificity: 58.06%). According to the AUSDRISK Arabic version score, 39.4% and 39.1% had moderate and high risk for develo** DM while only 21.5 had mild risk. These findings are not identical to previous studies conducted outside [15, 17, 41] and inside [24] Egypt in which 50% of the participants were at high T2DM risk. Involvement of younger age group stood behind this discrepancy as the older the age the more the AUSDRISK score and higher the risk of T2DM and vice versa. Again, the young age caused the lower proportion of participants at high T2DM risk among Australians in a study to predict the risk of T2DM, [42] and among the Egyptian and Malaysian students at Tanta University, in Egypt which brought to light the simplicity and practicality of the AUSDRISK screening power [43].
Derivation, Modeling, and internal validation of the AUSDRISK was launched in 2010 in the Australian diabetes obesity and lifestyle intervention (AusDiab) long-term project through a nested biphasic study. Risk factors have been converted into a feasible, non-invasive, and accurate predictive AUSDRISK model with a cut-off point at 12, AUC, sensitivity and specificity, 0.78, 74% and 67.7% respectively. [15] Reliability of the AUSDRISK screening potentiality for characterizing people at high T2DM risk for further lifestyle change has been tested and verified by a cross-sectional study. At cutoff value of the AUSDRISK ≥ 12, the sensitivity and specificity were 81.3% and 57.7 respectively. [17] Employment of the AUSDRISK to early detect T2DM in a sample of 40–59 year villagers was carried out in a cross-sectional study in Indonesia. It characterized successfully the participants with scores below and above the AUSDRISK cut off level (12 points) with as high as sensitivity and specificity of 93.46% and 70.98% respectively. [44]
The study has a limitation of being restricted to only one Egyptian Governorate, namely, El Behera Governorate. To be generalizable to the overall Egyptian situation, the study needs to be replicated to represent the 27 Egyptian Governorates. Generalizability to the Arab World needs extending the study to represent the 22 member countries of the Arab league. Generalizability to Arab speaking communities all over the globe needs more extensive research efforts.
Conclusion and recommendation
Overt DM just occupies the top of an iceberg, its unseen big population have undiagnosed DM; which is not infrequent (5%), PDM; which is the big reservoir from which overt DM emerge (21.7%) or been at risk of T2DM because of sustained exposure to the influential risk factors. The main risk factors that strongly influence abnormal glycemic level were age, being physically inactive, previous history of abnormal glycemic level and waist circumference. The AUSDRISK Arabic version was proved to be sensitive and specific tool to be used among Egyptians as a screening tool for the detection of DM or abnormal glycemic level. A prominent association has been demonstrated between AUSDRISK Arabic version score and the diabetic status. It is recommended to establish a nationwide program for early detection of undiagnosed DM and those at risk of develo** DM with comprehensive intervention measures for lifestyle modification. Also to apply the AUSDRISK Arabic version during opportunistic screening or mass public surveys to identify population at risk of T2DM.
Data availability
Data is available from the corresponding author on reasonable request.
Abbreviations
- ADA:
-
American Diabetes Association
- AUC:
-
Area under the curve
- AUSDRISK:
-
Australian Type 2 Diabetes Risk Assessment Tool
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- DM:
-
Diabetes Mellitus
- FPG:
-
Fasting Plasma Glucose
- GDM:
-
Gestational diabetes
- HbA1c:
-
Glycated Hemoglobin
- IDF:
-
International Diabetic Federation
- IGT:
-
Impaired glucose tolerance
- IFG:
-
Impaired fasting glucose
- LL:
-
Lower limit
- LMIC:
-
Low and Middle Income Countries
- OGTT:
-
Oral Glucose Tolerance Test
- OR:
-
Odds ratio
- PDM:
-
Pre-diabetes
- ROC:
-
Receiver operating characteristic curves
- SD:
-
Standard Deviation
- T2DM:
-
Type 2 Diabetes Mellitus
- UL:
-
Upper limit
- WHO:
-
World Health Organization
References
World Health Organization. Diabetes 2018. https://www.who.int/news-room/fact-sheets/detail/diabetes. Accessed 01 October 2022.
Intenational Diabetes Federation. IDF Diabetes Atlas 10th edition 2022. https://diabetesatlas.org/. Accessed 01 Oct 2022.
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119.
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract. 2019;157:107843.
Intenational Diabetes Federation. Type 2 diabetes 2020. https://www.idf.org/aboutdiabetes/type-2-diabetes.html. Accessed 01 October 2022.
Intenational Diabetes Federation. Diabetes prevention 2019. https://www.idf.org/aboutdiabetes/prevention.html. Accessed 01 October 2022.
World Health Organization, editor Screening for type 2 diabetes. Report of the World Health Organization and International Diabetes Federation meeting., 2003; 2003.
Heydari I, Radi V, Razmjou S, Amiri A. Chronic complications of diabetes mellitus in newly diagnosed patients. Int J Diabetes Mellitus. 2010;2(1):61–3.
Mattila TK, de Boer A. Influence of intensive versus conventional glucose control on microvascular and macrovascular complications in type 1 and 2 diabetes mellitus. Drugs. 2010;70(17):2229–45.
NICE (National Institute of Health and Care Excellence). Risk assessment for type 2 diabetes - Type 2 diabetes: prevention in people at high risk 2017. https://www.nice.org.uk/guidance/ph38. Accessed 01 October 2022.
Bang H, Edwards AM, Bomback AS, Ballantyne CM, Brillon D, Callahan MA, et al. Development and validation of a patient self-assessment score for diabetes risk. Ann Intern Med. 2009;151(11):775–83.
Diabetes.co.uk. Diabetes Tests 2022. https://www.diabetes.co.uk/Diabetes-screening-test.html. Accessed 01 October 2022.
Lindström J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care. 2003;26(3):725–31.
Paprott R. Evaluation of the german diabetes risk score as a screening tool for undiagnosed diabetes. Robert Koch-Institut; 2012.
Chen L, Magliano DJ, Balkau B, Colagiuri S, Zimmet PZ, Tonkin AM, et al. AUSDRISK: an australian type 2 diabetes risk Assessment Tool based on demographic, lifestyle and simple anthropometric measures. Med J Aust. 2010;192(4):197–202.
Farag HFM, Sultan EA, Elrewany E, Abdel-Aziz BF. Arabic version of the australian type 2 diabetes risk assessment tool (AUSDRISK): translation and validation. BMC Res Notes. 2022;15(1):303.
Malo JA, Versace VL, Janus ED, Laatikainen T, Peltonen M, Vartiainen E, et al. Evaluation of AUSDRISK as a screening tool for lifestyle modification programs: international implications for policy and cost-effectiveness. BMJ Open Diabetes Research and Care. 2015;3(1):e000125.
Naing L. Sample size calculator for sensitivity and specificity studies 2004. https://sites.google.com/site/statisticsayubsadiq/. Accessed 01 October 2022.
Ministry of Health and Population [Egypt]. El-anaty and Associates [Egypt], and ICF International. Egypt demographic and health survey 2014. Egypt and Rockville, Maryland, USA: Cairo; 2015.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization technical report series. 2017;894:i-xii, 1-253.
World Health Organization, About. Diabetes 2020. https://www.who.int/diabetes/action_online/basics/en/index1.html. Accessed 01 October 2022.
IBM Corp. IBM SPSS Statistics for Windows [Computer software]. 26.0 ed. Armonk, NY: IBM Corp; 2019.
Assaad Khalil SH, Megallaa MH, Rohoma KH, Ismael H, AbouSeif M, Kharboush I, et al. Prevalence of type 2 diabetes mellitus in a sample of the adult population of Alexandria, Egypt. Diabetes Res Clin Pract. 2018;144:63–73.
Abd El-Wahab EW, Shatat HZ, Charl F. Adapting a prediction rule for metabolic syndrome risk Assessment suitable for develo** countries. J Prim care community health. 2019;10:2150132719882760.
Aynalem SB, Zeleke AJ. Prevalence of diabetes Mellitus and its risk factors among individuals aged 15 years and above in Mizan-Aman Town, Southwest Ethiopia, 2016: a Cross Sectional Study. Int J Endocrinol. 2018;2018:9317987.
Endris T, Worede A, Asmelash D. Prevalence of diabetes Mellitus, Prediabetes and its Associated factors in Dessie Town, Northeast Ethiopia: A Community-Based study. Diabetes Metab Syndr Obes. 2019;12:2799–809.
Aekplakorn W, Chariyalertsak S, Kessomboon P, Assanangkornchai S, Taneepanichskul S, Putwatana P. Prevalence of Diabetes and Relationship with Socioeconomic Status in the Thai Population: National Health Examination Survey, 2004–2014. Journal of diabetes research. 2018;2018:1654530.
Seclen SN, Rosas ME, Arias AJ, Huayta E, Medina CA. Prevalence of diabetes and impaired fasting glucose in Peru: report from PERUDIAB, a national urban population-based longitudinal study. BMJ Open Diabetes Research & Care. 2015;3(1):e000110.
Eades CE, France EF, Evans JM. Prevalence of impaired glucose regulation in Europe: a meta-analysis. Eur J Public Health. 2016;26(4):699–706.
American Diabetes Association. 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes—2020. Diabetes Care. 2020;43(Supplement 1):14–S31.
NIDDK. Risk Factors for Type 2 Diabetes. 2016. https://www.niddk.nih.gov/health-information/diabetes/overview/risk-factors-type-2-diabetes. Accessed 01 October 2022.
Hamasaki H. Daily physical activity and type 2 diabetes: a review. World J diabetes. 2016;7(12):243–51.
Cannata F, Vadalà G, Russo F, Papalia R, Napoli N, Pozzilli P. Beneficial Effects of Physical Activity in Diabetic Patients. J Funct morphology Kinesiol. 2020;5(3).
Li M, Fan Y, Zhang X, Hou W, Tang Z. Fruit and vegetable intake and risk of type 2 diabetes mellitus: meta-analysis of prospective cohort studies. BMJ Open. 2014;4(11):e005497.
Jiang Z, Sun TY, He Y, Gou W, Zuo LS, Fu Y, et al. Dietary fruit and vegetable intake, gut microbiota, and type 2 diabetes: results from two large human cohort studies. BMC Med. 2020;18(1):371.
Herath H, Herath R, Wickremasinghe R. Gestational diabetes mellitus and risk of type 2 diabetes 10 years after the index pregnancy in sri lankan women-A community based retrospective cohort study. PLoS ONE. 2017;12(6):e0179647.
Li Z, Cheng Y, Wang D, Chen H, Chen H, Ming WK, et al. Incidence rate of type 2 diabetes Mellitus after Gestational Diabetes Mellitus: a systematic review and Meta-analysis of 170,139 women. J Diabetes Res. 2020;2020:3076463.
Vounzoulaki E, Khunti K, Abner SC, Tan BK, Davies MJ, Gillies CL. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ. 2020;369:m1361.
Tino S, Mayanja BN, Mubiru MC, Eling E, Ddumba E, Kaleebu P, et al. Prevalence and factors associated with overweight and obesity among patients with type 2 diabetes mellitus in Uganda-a descriptive retrospective study. BMJ Open. 2020;10(11):e039258.
Leitner DR, Frühbeck G, Yumuk V, Schindler K, Micic D, Woodward E, et al. Obesity and type 2 diabetes: two Diseases with a need for combined treatment strategies - EASO Can lead the way. Obes Facts. 2017;10(5):483–92.
Martin A, Neale EP, Tapsell LC. The clinical utility of the AUSDRISK tool in assessing change in type 2 diabetes risk in overweight/obese volunteers undertaking a healthy lifestyle intervention. Prev Med Rep. 2019;13:80–4.
Bagheri N, Konings P, Wangdi K, Parkinson A, Mazumdar S, Sturgiss E et al. Identifying hotspots of type 2 diabetes risk using general practice data and geospatial analysis: an approach to inform policy and practice. Aust J Prim Health. 2019.
El-Sherbiny AAM. Diabetic risk assessment among egyptian and malaysian medical students, Tanta Faculty of Medicine, Egypt. Tanta Med J. 2015;43(2):72.
Amiruddin R, Stang, Ansar J, Arsyad D, Rahman A. Diabetic Mellitus Type 2 in Wajo South Sulawesi, Indonesia. Int J Curr Res Acad Rev. 2014;2:1–8.
Acknowledgements
Authors would offer special thanks to all study participants for their tolerance and cooperation.
Funding
Authors declare that no funding has been received related to the manuscript.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
HFMF designed the study and participate in writing and editing the manuscript. EE collected and analyzed data and wrote the manuscript. BFA assissted in study design, statistical analysis and writing the paper. EAS performded the analysis and interpretation of data, and writing the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The approval of the ethics committee of the High Institute of Public Health for conducting the research was obtained. An informed written consent was taken from the study participants and also from legal guardians of illiterate participants after explanation of the purpose and benefits of the research. Anonymity and confidentiality were assured and maintained and there was no conflict of interest. All methods were performed in accordance with the relevant guidelines and regulations confirm the Declaration of Helsinki.
Consent for publication
Not applicable.
Conflict of interest
None to be declared.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Farag, H.F.M., Elrewany, E., Abdel-Aziz, B.F. et al. Prevalence and predictors of undiagnosed type 2 diabetes and pre-diabetes among adult Egyptians: a community-based survey. BMC Public Health 23, 949 (2023). https://doi.org/10.1186/s12889-023-15819-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-15819-0