Abstract
Background
Air pollution exposure has been associated with a multitude of diseases and poses a significant concern to public health. For targeted environmental risk communication and interventions to be effective, it is important to correctly identify characteristics associated with worry of harm from air pollution.
Methods
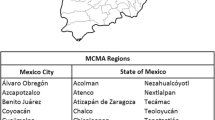
Using responses from 3,630 participants of the Health Information National Trends Survey 4 Cycle 2, we assessed worry of harm from exposure to indoor (IAP) and outdoor (OAP) air pollution separately. Multinomial logistic regression models were used to calculate odds ratios and 95% confidence intervals.
Results
Hispanics were more likely to worry about harm from IAP and OAP compared to non-Hispanic whites. Participants who lived in metropolitan counties were more likely to worry about harm from IAP and OAP compared to those who lived in rural counties. Finally, those who believed their chance of getting cancer was high were more likely to worry about harm from IAP and OAP compared to those who thought their likelihood of getting cancer was low.
Conclusions
Worry of harm from IAP and OAP varied across sociodemographic and cancer-related characteristics. Public health professionals should consider these characteristics when develo** targeted environmental risk communication and interventions.
Similar content being viewed by others
Background
Air pollution refers to both man-made and naturally occurring pollutants in the air we breathe. Although air pollution is often invisible and odorless, exposure to it is ubiquitous and a threat to public health. Air pollutants include, but are not limited to noxious gases, fine particles produced by the burning of fossil fuels, and tobacco smoke. Air pollution increases the risk for develo** heart and respiratory diseases [17]. In addition, air pollution exposure has been associated with the risk for develo** some cancers, the most common being lung [18, 24, 54], breast [48, 50], and bladder [42]. A meta-analysis of 30 cohort studies from 14 countries found that across numerous cancers, exposure to particulate matter (PM) 2.5, PM 10, and nitrogen dioxide was associated with an increase in cancer mortality [26].
There have been efforts at the policy level to control indoor and outdoor air pollution. Some examples in recent years include the Clean Air Act of 1970 in the United States (U.S.) and World Health Organization interim targets concerning PM control on cardiovascular disease mortality, both of which have led to a decrease in particle pollution and ground-level ozone pollution [33, 47]. Nevertheless, approximately seven million people die from air pollution exposure around the world every year [23]. Further, adverse health effects due to air pollution exposure are often concentrated in among those who have been characterized as having low socioeconomic status and individuals suffering from pre-existing conditions [38].
It is important to distinguish between outdoor and indoor air pollution as they each pose different health risks. Outdoor air pollution refers to pollutants such as ground-level ozone, noxious gases, and fine particles produced by burning fossil fuels by motor vehicles and power plants. Exposure to chemicals found in air pollution are harmful to humans because these chemicals are often small enough to penetrate deep inside the lungs and cause a variety of adverse reactions such as early impairment of airway function, chronic system inflammation, oxidative stress, and lung cancer [4, 18, 52].
Indoor air pollution refers to air pollutants found inside our homes, schools, and other building environments. Sources of the most common indoor air pollutants from economically develo** countries often differ from the sources found in economically developed countries like the US. Common indoor air pollutants in the US are derived from secondhand smoke, carbon monoxide exposure from gas and wood stoves primarily used in rural areas [51], and radon exposure from building foundations [49]. Additionally, volatile organic compounds (VOCs) are chemicals found in many household products such as aerosol sprays, cleaners, and pesticides contain toxic and carcinogenic compounds such as benzene and toluene in the air and water [13]. Overall, indoor air pollution remains a major public health concern because people often spend most of their time indoors at work or inside their homes, further intensifying the concentration of exposure to harmful indoor pollutants. In the United States, specifically, “radon, a major indoor air pollutant, is the second leading cause of cancer and responsible for 15,000 to 20,000 deaths each year” [37].
Effective risk communication and targeted interventions, such as household and behavior change interventions, can be productive tools to mitigate the adverse effects of air pollution exposure. Additionally, it is important to inform the public about the risks associated with air pollution in ways that do not create a sense of unwarranted indifference, while at the same time, not creating unwarranted anxiety [19]. Nevertheless, due to individual variability in air pollution exposure and public health risk across the US, develo** a one-size-fits-all risk communication strategy along with targeted interventions can be challenging and ineffective. In order for risk communication to be effective, information should be current and appropriate to the targeted audience [46].
Several studies have examined participants’ perception of harm due to air pollution exposure [16, 32, 35]. However, to our knowledge, there have been no studies that have explicitly measured one’s worry of harm from indoor and outdoor air pollution exposure. Additionally, studies regarding air pollution perception have not been conducted in the U.S. nor have they explored cancer-related characteristics, such as family cancer history and perception of one’s cancer risk [3, 29, 40]. Lastly, many of these studies were focused on either indoor or outdoor air pollution separately or used the term “air pollution” without distinguishing whether it was indoor or outdoor [21, 27, 41]. The purpose of this study was to examine sociodemographic and cancer-related characteristics associated with worry of harm from exposure to indoor air pollution (IAP) and outdoor air pollution (OAP) using data from a nationally representative survey in the US.
Methods
The Health Information National Trends Survey (HINTS) is a nationally representative survey supported by the National Cancer Institute that aims to describe cancer-related knowledge, beliefs, attitudes, and behaviors of adults in the US. HINTS uses a probability sample of U.S. telephone numbers to reach a cross-section of the adult, non-institutionalized, and civilian U.S. population. Data were collected using a computer-assisted telephone interview system administered in English or Spanish. Response rates were calculated using the Response Rate 2 (RR2) formula of the American Association of Public Opinion Research [36]. We utilized data from the 2012 iteration of the HINTS 4 Cycle 2. There was a total of 3,630 participants in the 2012 iteration of the HINTS with an overall response rate of 40%. Racial and ethnic minorities were oversampled to increase the precision of estimates for minority sub-populations. Additional details on the HINTS methodology as well as access to the complete HINTS datasets can be found on hints.cancer.gov as well as previous literature and reports [1, 56].
For this study, we used the questions “How much do you worry that indoor air pollution will harm your health?” and “How much do you worry that outdoor air pollution will harm your health?”. Participants were able to respond: “not at all”, “a little”, “somewhat”, or “a lot” to each question. Due to the lack in significant differences in ORs for the “a little” and “somewhat” responses for indoor and outdoor air pollution and the variables of interest, we combined the two responses into “some or a little” to create a total of three response categories: “a lot”, “some or a little”, and “not at all” (data not shown).
Sociodemographic variables included sex (male and female), age (18–34, 35–49, 50–64, and ≥ 65), race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, and Asian, Pacific Islander, other), whether someone was born in the United States, education level (high school diploma or less, some college or post-high school vocational training, bachelor’s degree or more), annual household income (≤ $20,000, $20,000–34,999, $35,000–49,000, $50,000–74,000, and ≥ $75,000), smoking status (never smoker, former smoker, and current smoker), and whether respondents resided in a rural or metropolitan county. For our analysis, non-metropolitan and metropolitan residence was determined based on Rural Urban Continuum Codes in which categories 1 through 3 (counties with 250,000 residents or more) were considered “metropolitan” and categories 4 through 9 (counties with less than 250,000 residents) were considered “non-metropolitan” [57]. In addition to sociodemographic variables, we also examined cancer-related variables including family history of cancer (No, Not Sure, Yes), previous diagnosis of lung disease, which included chronic lung disease, asthma, emphysema, and/or chronic bronchitis (No, Yes), and perceived likelihood of getting cancer (Very Unlikely or Unlikely, Neither Likely or Likely, and Very Likely or Likely).
Bivariate analyses of sociodemographic variables and cancer-related characteristic variables by worry of harm from IAP and OAP were conducted using the Wald chi-squared test and unadjusted odds ratios and 95% confidence intervals were calculated for each of the variables. In addition, a sensitivity analysis was conducted to confirm there were no major differences in estimates of odds ratios between the separate “somewhat” and “a little” response categories and the combined “some or a little” response category we created for IAP and OAP when compared to the “not at all” response category. There were no major differences in odds ratios between the original IAP and OAP discrete “somewhat” and “a little” response categories and the combined category, therefore we used the combined response (“some or a little”) category for IAP and OAP for our analysis. The final response categories were: “not at all”, “some or a little”, and “a lot” for IAP and OAP. A p-value of less than or equal to 0.05 was used to determine statistical significance. Multinomial logistic regression was used to calculate odds ratios (OR) and 95% confidence intervals (CI) for the association between sociodemographic and cancer-related variables and worry of harm from IAP and OAP (separately). Participants with any missing values were removed from the logistic regression analysis. All models were adjusted for demographic variables including sex, race/ethnicity, education, and non-metropolitan-metropolitan residence. SAS (version 9.4; Cary, NC) was used to conduct all statistical analyses.
Results
The distribution of demographic factors for the sample population and the weighted population are presented in Table 1. Among the sample population, a little more than half consisted of women (n = 2,172, 51.4%). Nearly two-thirds (62.7%) of the respondents were non-Hispanic white, while 1,057 (37.6%) had completed some college or post-high school vocational training, and 926 (31.0%) had an annual household income greater than $75,000. Most respondents (68.5%) reported a known family history of cancer while 20% of respondents (n = 621) believed they had a very likely or likely chance of getting cancer themselves. The prevalence of respondents who had at least some or a little worry of harm for IAP and OAP was 55.2% and 57.0%, respectively. Additionally, the prevalence of respondents who worried “a lot” about harm from IAP and OAP were 12.7% and 17.3%, respectively.
Bivariate analyses
Bivariate associations between worry of harm from IAP and OAP with sociodemographic and cancer characteristic variables are presented in Tables 2 and 3, respectively. Worry of harm from IAP was statistically significantly associated with race/ethnicity, education, non-metropolitan-metropolitan residence, and likelihood of getting cancer (Table 2). Worry of harm from OAP was statistically significantly associated with sex, race/ethnicity, whether someone was born in the U.S., education, smoking status, non-metropolitan-metropolitan residence, previous family history of cancer, previous lung disease diagnosis, and likelihood of getting cancer (Table 3). The magnitude of association was presented as unadjusted odds ratios and 95% confidence intervals calculated for worry of harm from IAP and OAP with sociodemographic and cancer characteristic variables (see: Supplemental Table).
Multivariable analyses
The association of worry of harm from IAP and OAP with select sociodemographic and cancer characteristics is presented in Table 4. Asians, Pacific Islanders, and those from other races (OR: 4.74, 95% CI: 1.93 – 11.67) and Hispanics (OR: 2.44, 95% CI: 1.34 – 4.43) were more likely to worry “a lot” about harm from IAP compared to non-Hispanic whites. Those who obtained a high school diploma or less were more likely to worry “a lot” about harm from IAP compared to those who were a college graduate or obtained a post-graduate degree (OR: 2.38, 95% CI: 1.39 – 4.08). Additionally, those who believed they were very likely or likely to get cancer in their lifetime were approximately two times more likely to worry “a lot” about harm from IAP compared to those who believed they were neither unlikely or likely to get cancer in their lifetime (OR: 1.99, 95% CI: 1.20 – 3.29). Lastly, respondents who were born outside the U.S. were more likely to worry “some or a little” (OR: 1.90, 95% CI: 1.11 – 2.93) and “a lot” (OR: 5.64, 95% CI: 3.52 – 9.01) about IAP than respondents who were born in the U.S.
Women were more likely to worry “a lot” about harm from OAP compared to men (OR: 1.95, CI: 1.24 – 3.08). Asians, Pacific Islanders, and those from other races (OR: 6.25, 95% CI: 2.92 – 13.36) and Hispanics (OR: 3.02, 95% CI: 1.78 – 5.15) were more likely to worry “a lot” about harm from OAP compared to non-Hispanic whites. Those who obtained a high school diploma or less were more likely to worry “a lot” about harm from OAP compared to those who obtained a college graduate or post-graduate degree (OR: 1.64, 95% CI: 1.03 – 2.61). Participants who lived in an metropolitan county were more likely to worry “a lot” about harm from OAP compared to those who live in non-metropolitan counties (OR: 1.88, 95%CI: 1.08 – 3.28). Respondents who were born outside the U.S. were approximately 4.60 times more likely than those born in the U.S. to worry about harm from OAP (OR: 4.60, 95%CI: 2.78 – 7.63). Additionally, those who had a diagnosis of lung disease were more likely to worry “a lot” about harm from OAP compared to those who did not have a diagnosis of lung disease (OR: 2.10, 95% CI: 1.20 – 3.68). Finally, those who believed they were very likely or likely to get cancer in their lifetime were approximately 2.5 times more likely to worry “a lot” about harm from OAP compared to those who believed they were neither unlikely or likely to get cancer in their lifetime (OR: 2.56, 95% CI: 1.57 – 4.19).
Discussion
Data from the 2012 HINTS suggest that there are several subgroups of the U.S. population that worried more about harm from IAP and OAP compared to others. The subgroups included women, Hispanics, Asians/Pacific Islanders, and other races (in comparison to non-Hispanic Whites), people born outside the United States, those who lived in metropolitan counties, as well as people who have a previous family cancer history and/or lung disease diagnosis (in comparison to those who do not have a previous family cancer history and/or lung disease diagnosis). Our findings indicate that such groups should be considered when develo** air pollution risk communication and intervention strategies. Additionally, our results suggest that more communication regarding the prevalence and risks of indoor air pollution exposure is needed.
Our finding that women were nearly twice as likely as men to be worried “a lot” about outdoor air pollution is consistent with what the literature suggests about environmental risks and women. Other studies have found that women, especially those with children, are more aware of and concerned about environmental risks [14, 27]. One possible reason for this is because air pollution has been associated with poor reproductive health outcomes including infertility, miscarriage, and stillbirth [11, 20]. Moreover, one case control study found that prenatal exposure to ambient PM2,5 increased mental stress for pregnant women [45]. Risk communication should also consider perception of air pollution exposure within microenvironments including one’s commute. For example, research suggesting that changing one’s bicycle route to areas with less motorized traffic may decrease exposure to particulate matter, odor, and nasopharyngeal irritation [10] could be included in communication materials as a protective action against air pollution exposure. It is important to understand what factors influence adherence to communication tools such as public service announcements, the AQI, etc. Future research is warranted which includes greater study participation, more detailed questions about indoor and/or outdoor air pollution knowledge, longitudinal data collection, and more information on whether participants live in areas with high levels of air pollution exposure.
Availability of data and materials
The data (HINTS 4, Cycle 2) for the current study are available on the Health Information National Trends Survey website [https://hints.cancer.gov/data/survey-instruments.aspx#H4C2].
Abbreviations
- PM:
-
Particulate Matter
- US:
-
United States
- LMIC:
-
Low-to-Middle-Income Countries
- IAP:
-
Indoor Air Pollution
- OAP:
-
Outdoor Air Pollution
- HINTS:
-
Health Information National Trends Survey
- OR:
-
Odds Ratio
- CI:
-
Confidence Intervals
References
Blake KD, Portnoy DB, Kaufman AR, Lin C-TJ, Lo SC, Backlund E, Hesse BW. Rationale, procedures, and response rates for the 2015 administration of NCI’s Health Information National Trends Survey: HINTS-FDA 2015. J Health Commun. 2016;21(12):1269–75. https://doi.org/10.1080/10810730.2016.1242672.
Borbet TC, Gladson LA, Cromar KR. Assessing air quality index awareness and use in Mexico City. BMC Public Health. 2018;18:538. https://doi.org/10.1186/s12889-018-5418-5.
Börner S, Albino JC, Caraveo LM, Tejeda AC. Exploring Mexican adolescents’ perceptions of environmental health risks: a photographic approach to risk analysis. Cien Saude Colet. 2015;20(5):1617–27. https://doi.org/10.1590/1413-81232015205.11382014.
Boulanger G, Bayeux T, Mandin C, Kirchner S, Vergriette B, Pernelet-Joly V, Kopp P. Socio-economic costs of indoor air pollution: a tentative estimation for some pollutants of health interest in France. Environ Int. 2017;104:14–24. https://doi.org/10.1016/j.envint.2017.03.025.
Burki TK. Burning issues: tackling indoor air pollution. Lancet. 2011;377(9777):1559–60. https://doi.org/10.1016/S0140-6736(11)60626-0.
Calderón-Garcidueñas L, Franco-Lira M, Henríquez-Roldán C, Osnaya N, González-Maciel A, Reynoso-Robles R, Doty RL. Urban air pollution: Influences on olfactory function and pathology in exposed children and young adults. Exp Toxicol Pathol. 2010;62(1):91–102. https://doi.org/10.1016/j.etp.2009.02.117.
Carrillo G, Perez Patron MJ, Johnson N, Zhong Y, Lucio R, Xu X. Asthma prevalence and school-related hazardous air pollutants in the US-México border area. Environ Res. 2018;162:41–8. https://doi.org/10.1016/j.envres.2017.11.057.
Cesaroni G, Badaloni C, Gariazzo C, Stafoggia M, Sozzi R, Davoli M, Forastiere F. Long-term exposure to urban air pollution and mortality in a cohort of more than a million adults in rome. Environ Health Perspect. 2013;121(3):324–31. https://doi.org/10.1289/ehp.1205862.
Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, Forouzanfar MH. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389(10082):1907–18. https://doi.org/10.1016/s0140-6736(17)30505-6.
Cole-Hunter T, Jayaratne R, Stewart I, Hadaway M, Morawska L, Solomon C. Utility of an alternative bicycle commute route of lower proximity to motorised traffic in decreasing exposure to ultra-fine particles, respiratory symptoms and airway inflammation – a structured exposure experiment. Environ Health. 2013;12(1):29. https://doi.org/10.1186/1476-069X-12-29.
Conforti A, Mascia M, Cioffi G, De Angelis C, Coppola G, De Rosa P, De Placido G. Air pollution and female fertility: a systematic review of literature. Reprod Biol Endocrinol. 2018;16(1):117. https://doi.org/10.1186/s12958-018-0433-z.
D’Antoni D, Smith L, Auyeung V, Weinman J. Psychosocial and demographic predictors of adherence and non-adherence to health advice accompanying air quality warning systems: a systematic review. Environ Health. 2017;16(1):100. https://doi.org/10.1186/s12940-017-0307-4.
David E, Niculescu VC. Volatile Organic Compounds (VOCs) as environmental pollutants: occurrence and mitigation using nanomaterials. Int J Environ Res Public Health. 2021;18(24):13147. https://doi.org/10.3390/ijerph182413147.
Deguen S, Padilla M, Padilla C, Kihal-Talantikite W. Do individual and neighborhood characteristics influence perceived air quality? Int J Environ Res Public Health. 2017;14(12):1559. https://doi.org/10.3390/ijerph14121559.
Deng H, Eckel SP, Liu L, Lurmann FW, Cockburn MG, Gilliland FD. Particulate matter air pollution and liver cancer survival. Int J Cancer. 2017;141(4):744–9. https://doi.org/10.1002/ijc.30779.
Egondi T, Kyobutungi C, Ng N, Muindi K, Oti S, van de Vijver S, Rocklöv J. Community Perceptions of Air Pollution and Related Health Risks in Nairobi Slums. Int J Environ Res Public Health. 2013;10(10):4851–68. Retrieved from https://search.proquest.com/docview/1468929399?accountid=14696. https://umaryland.on.worldcat.org/atoztitles/link?sid=ProQ:&issn=16617827&volume=10&issue=10&title=International+Journal+of+Environmental+Research+and+Public+Health&spage=4851&date=2013-10-01&atitle=Community+Perceptions+of+Air+Pollution+and+Related+Health+Risks+in+Nairobi+Slums&au=Egondi%2C+Thaddaeus%3BKyobutungi%2C+Catherine%3BNg%2C+Nawi%3BMuindi%2C+Kanyiva%3BOti%2C+Samuel%3Bvan+de+Vijver%2C+Steven%3BEttarh%2C+Remare%3BRockl%C3%B6v%2C+Joacim&id=doi.
El Morabet R. Effects of Outdoor Air Pollution on Human Health. In: Nriagu J, editor. Encyclopedia of environmental health. 2nd ed. Oxford: Elsevier; 2019. p. 278–86.
Fajersztajn L, Veras M, Barrozo LV, Saldiva P. Air pollution: a potentially modifiable risk factor for lung cancer. Nat Rev Cancer. 2013;13(9):674–8. https://doi.org/10.1038/nrc3572.
Fitzpatrick-Lewis D, Yost J, Ciliska D, Krishnaratne S. Communication about environmental health risks: a systematic review. Environ Health. 2010;9:67. https://doi.org/10.1186/1476-069x-9-67.
Gaskins AJ, Hart JE, Chavarro JE, Missmer SA, Rich-Edwards JW, Laden F, Mahalingaiah S. Air pollution exposure and risk of spontaneous abortion in the Nurses’ Health Study II. Hum Reprod. 2019;34(9):1809–17. https://doi.org/10.1093/humrep/dez111.
Hodgson A, Hitchings R. Urban air pollution perception through the experience of social practices: Talking about breathing with recreational runners in London. Health Place. 2018;53:26–33. https://doi.org/10.1016/j.healthplace.2018.07.009.
Huang L, Rao C, van der Kuijp TJ, Bi J, Liu Y. A comparison of individual exposure, perception, and acceptable levels of PM2.5 with air pollution policy objectives in China. Environ Res. 2017;157:78–86. https://doi.org/10.1016/j.envres.2017.05.012.
Joanna K, Katherine W, Pallavi P. Air pollution and its impacts on health in africa - insights from the State of Global Air 2020. Clean Air J. 2020;30(2). https://doi.org/10.17159/caj/2020/30/2.9270.
Johnson BB. Acculturation, ethnicity, and air pollution perceptions. Risk Anal. 2011;31(6):984–99. https://doi.org/10.1111/j.1539-6924.2010.01557.x.
Kim EH, Kim S, Lee JH, Kim J, Han Y, Kim YM, Ahn K. Indoor air pollution aggravates symptoms of atopic dermatitis in children. PLoS ONE. 2015;10(3):e0119501. https://doi.org/10.1371/journal.pone.0119501.
Kim H-B, Shim J-Y, Park B, Lee Y-J. Long-Term exposure to air pollutants and cancer mortality: a meta-analysis of cohort studies. Int J Environ Res Public Health. 2018;15(11):2608. https://doi.org/10.3390/ijerph15112608.
Laws MB, Yeh Y, Reisner E, Stone K, Wang T, Brugge D. Gender, ethnicity and environmental risk perception revisited: the importance of residential location. J Community Health. 2015;40(5):948–55. https://doi.org/10.1007/s10900-015-0017-1.
Li J, Huang L, Han B, van der Kuijp TJ, **a Y, Chen K. Exposure and perception of PM(2.5) pollution on the mental stress of pregnant women. Environ Int. 2021;156:106686. https://doi.org/10.1016/j.envint.2021.106686.
Li Z, Folmer H, Xue J. Perception of air pollution in the **chuan mining area, China: a structural equation modeling approach. Int J Environ Res Public Health. 2016;13(5):735. https://doi.org/10.3390/ijerph13070735.
Liao X, Tu H, Maddock JE, Fan S, Lan G, Wu Y, Lu Y. Residents’ perception of air quality, pollution sources, and air pollution control in Nanchang China. Atmos Pollut Res. 2015;6(5):835–41. https://doi.org/10.5094/apr.2015.092.
Lin C, Ma Y, Liu R, Shao Y, Ma Z, Zhou L, Chen K. Associations between short-term ambient ozone exposure and cause-specific mortality in rural and urban areas of Jiangsu China. Environ Res. 2022;211:113098. https://doi.org/10.1016/j.envres.2022.113098.
Liu X, Wu Y, Hu Y, Liu D, Zhang J, Chen C, Lu Y. Government employees’ perception of urban air pollution and willingness to pay for improved quality: a cross-sectional survey study in Nanchang China. Environ Sci Pollut Res Int. 2016;23(21):22183–9. https://doi.org/10.1007/s11356-016-7204-1.
Liu Z, Wang F, Li W, Yin L, Wang Y, Yan R, Tse LA. Does utilizing WHO’s interim targets further reduce the risk - meta-analysis on ambient particulate matter pollution and mortality of cardiovascular diseases? Environ Pollut. 2018;242:1299–307. https://doi.org/10.1016/j.envpol.2018.07.041.
Martinez GS, Spadaro JV, Chapizanis D, Kendrovski V, Kochubovski M, Mudu P. Health impacts and economic costs of air pollution in the metropolitan area of skopje. Int J Environ Res Public Health. 2018;15(4):626. https://doi.org/10.3390/ijerph15040626.
Muindi K, Egondi T, Kimani-Murage E, Rocklov J, Ng N. “We are used to this”: a qualitative assessment of the perceptions of and attitudes towards air pollution amongst slum residents in Nairobi. BMC Public Health. 2014;14:226. https://doi.org/10.1186/1471-2458-14-226.
Nelson DE, Kreps GL, Hesse BW, Croyle RT, Willis G, Arora NK, Alden S. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004;9(5):443–60. https://doi.org/10.1080/10810730490504233 discussion 481–444.
Nwanaji-Enwerem JC, Allen JG, Beamer PI. Another invisible enemy indoors: COVID-19, human health, the home, and United States indoor air policy. J Expo Sci Environ Epidemiol. 2020;30(5):773–5. https://doi.org/10.1038/s41370-020-0247-x.
O’Neill MS, Kinney PL, Cohen AJ. Environmental equity in air quality management: local and international implications for human health and climate change. J Toxicol Environ Health A. 2008;71(9–10):570–7. https://doi.org/10.1080/15287390801997625.
Oltra C, Sala R, Boso A, Asensio SL. Public engagement on urban air pollution: an exploratory study of two interventions. Environ Monit Assess. 2017;189(6):296. https://doi.org/10.1007/s10661-017-6011-6.
Omanga E, Ulmer L, Berhane Z, Gatari M. Industrial air pollution in rural Kenya: community awareness, risk perception and associations between risk variables. BMC Public Health. 2014;14:377. https://doi.org/10.1186/1471-2458-14-377.
Orru K, Nordin S, Harzia H, Orru H. The role of perceived air pollution and health risk perception in health symptoms and disease: a population-based study combined with modelled levels of PM10. Int Arch Occup Environ Health. 2018;91(5):581–9. https://doi.org/10.1007/s00420-018-1303-x.
Pedersen M, Stafoggia M, Weinmayr G, Andersen ZJ, Galassi C, Sommar J, Raaschou-Nielsen O. Is there an association between ambient air pollution and bladder cancer incidence? analysis of 15 european cohorts. Eur Urol Focus. 2018;4(1):113–20. https://doi.org/10.1016/j.euf.2016.11.008.
Quintana PJE, Khalighi M, Castillo Quiñones JE, Patel Z, Guerrero Garcia J, Martinez Vergara P, Mantz A. Traffic pollutants measured inside vehicles waiting in line at a major US-Mexico port of entry. Sci Total Environ. 2018;622–623:236–43. https://doi.org/10.1016/j.scitotenv.2017.11.319.
Raaschou-Nielsen O, Andersen ZJ, Beelen R, Samoli E, Stafoggia M, Weinmayr G, Hoek G. Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE). Lancet Oncol. 2013;14(9):813–22. https://doi.org/10.1016/s1470-2045(13)70279-1.
RajagopalanBrauerBhatnagarBhattBrookHuang SMADLJRW, et al. Personal-level protective actions against particulate matter air pollution exposure: a scientific statement from the American Heart Association. Circulation. 2020;142(23):e411–31. https://doi.org/10.1161/CIR.0000000000000931.
Ramirez AS, Ramondt S, Van Bogart K, Perez-Zuniga R. Public awareness of air pollution and health threats: challenges and opportunities for communication strategies to improve environmental health literacy. J Health Commun. 2019;24(1):75–83. https://doi.org/10.1080/10810730.2019.1574320.
Ross K, Chmiel JF, Ferkol T. The impact of the clean air act. J Pediatr. 2012;161(5):781–6. https://doi.org/10.1016/j.jpeds.2012.06.064.
Schmidt CW. Air pollution and breast cancer in postmenopausal women: evidence across cohorts. Environ Health Perspect. 2018;126(3):034001. https://doi.org/10.1289/ehp3200.
Seguel JM, Merrill R, Seguel D, Campagna AC. Indoor air quality. Am J Lifestyle Med. 2017;11(4):284–95. https://doi.org/10.1177/1559827616653343.
Shmuel S, White AJ, Sandler DP. Residential exposure to vehicular traffic-related air pollution during childhood and breast cancer risk. Environ Res. 2017;159:257–63. https://doi.org/10.1016/j.envres.2017.08.015.
Sircar K, Clower J, Shin MK, Bailey C, King M, Yip F. Carbon monoxide poisoning deaths in the United States, 1999 to 2012. Am J Emerg Med. 2015;33(9):1140–5. https://doi.org/10.1016/j.ajem.2015.05.002.
Turner MC, Krewski D, Diver WR, Pope CA 3rd, Burnett RT, Jerrett M, Gapstur SM. Ambient air pollution and cancer mortality in the cancer prevention study II. Environ Health Perspect. 2017;125(8):087013. https://doi.org/10.1289/EHP1249.
Vanderpool RC, Huang B. Cancer risk perceptions, beliefs, and physician avoidance in Appalachia: results from the 2008 HINTS Survey. J Health Commun. 2010;15(Suppl 3):78–91. https://doi.org/10.1080/10810730.2010.522696.
Vermeulen R, Downward GS, Zhang J, Hu W, Portengen L, Bassig BA, Lan Q. Constituents of household air pollution and risk of lung cancer among never-smoking women in Xuanwei and Fuyuan China. Environ Health Perspect. 2019;127(9):97001. https://doi.org/10.1289/EHP4913.
Viehmann A, Hertel S, Fuks K, Eisele L, Moebus S, Möhlenkamp S, Hoffmann B. Long-term residential exposure to urban air pollution, and repeated measures of systemic blood markers of inflammation and coagulation. Occup Environ Med. 2015;72(9):656. https://doi.org/10.1136/oemed-2014-102800.
Westat. Health Information National Trends Survey 4 (HINTS 4) Cycle 2 Methodology Report Retrieved from 2015.
Zahnd WE, Goldfarb J, Scaife SL, Francis ML. Rural-urban differences in behaviors to prevent skin cancer: an analysis of the Health Information National Trends Survey. J Am Acad Dermatol. 2010;62(6):950–6. https://doi.org/10.1016/j.jaad.2009.08.058.
Zhang L, Yuan Z, Maddock JE, Zhang P, Jiang Z, Lee T, Lu Y. Air quality and environmental protection concerns among residents in Nanchang, China. Air Qual Atmos Health. 2014;7(4):441–8. https://doi.org/10.1007/s11869-014-0255-x.
Acknowledgements
This research was presented as a poster by Hayley Aja, MPH at the International Society for Environmental Epidemiology, Seattle, WA, August 2014. Citation: Aja H, Ghazarian AA, Reid BC, Ellison GL. Characteristics associated with worry of harm from indoor air pollution in the United States.
Funding
Open Access funding provided by the National Institutes of Health (NIH). This research received no external funding.
Author information
Authors and Affiliations
Contributions
This study was conducted by a team of researchers with each contributing in a significant way towards the development of the manuscript. SA, HA, and GLE conceived the study. SA worked on the methodology, data analysis, and writing the original draft. AAG, GYL, and GLE worked on the data validation and assisted with visualization of the tables. GYL, AAG, and GLE worked on the reviewing and editing. GLE supervised the project. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval and participant consent was not necessary as this study involved the use of a de-identified database. The data used in the study are publicly available.
Consent for publication
Not Applicable.
Competing interests
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table 1. Unadjusted Regression Analysis of IAP and OAP.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ammons, S., Aja, H., Ghazarian, A.A. et al. Perception of worry of harm from air pollution: results from the Health Information National Trends Survey (HINTS). BMC Public Health 22, 1254 (2022). https://doi.org/10.1186/s12889-022-13450-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-13450-z