Abstract
Purpose
To explore the mediating effect of hope in the relationships between social support and self-esteem with psychological resilience among patients with stroke survivors in early rehabilitation.
Methods
A cross-sectional study design was adopted. Data from a cross-sectional survey of 210 patients undergoing early stroke rehabilitation were analyzed using structural equation modeling. The variables of interest were measured using the Connor Davidson Resilience Scale, the Social Support Rating Scale, the Herth Hope Index, and the Self-Esteem Scale. This article reports according to the STROBE checklist.
Results
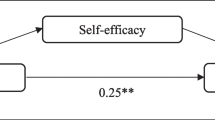
A positive relationship was found between social support and psychological resilience (β1 = 0.548), which was mediated by hope (β2 = 0.114), and social support had significant direct effect on resilience (β3 = 0.434). A positive relationship was also found between self-esteem and psychological resilience (β4 = 0.380), which was mediated by hope (β5 = 0.200), and self-esteem had significant direct effect on resilience (β6 = 0.179).
Conclusion
According to the results of this study, some strategies can be incorporated into the rehabilitation process to enhance psychological resilience, such as cultivating individual personality characteristics and improving patients’ social relationships. In the future, we need to explore methods for improving psychological resilience among patients with stroke in combination with their risk factors to improve their quality of life and reduce the incidence of post-stroke depression.
Similar content being viewed by others
Introduction
The significance of stroke is likely to increase in the future due to the aging populations in develo** countries [1]. China has the highest lifelong risk of stroke worldwide [2], and one of the burdens is post-stroke depression, the most common non-cognitive neuropsychiatric complication of stroke [3], characterized by patients’ reduced participation in rehabilitation and increased rates of recurrence and mortality [4]. The evidence for specific therapies of stroke has been separated into two periods: early rehabilitation (< 6 months post-stroke) versus late rehabilitation (> 6 months post-stroke) treatment [5]. Post-stroke depression usually occurs within the first months after a stroke, then gradually increases, and eventually peaks within six months [6]. Therefore, methods to reduce the incidence of depression within 6 months (early rehabilitation) after stroke are important. A longitudinal study showed that resilience is a protective factor against post-stroke depression [7], and the rate of depression among patients with a high level of psychological resilience decreases over time. Resilience is defined as ‘the dynamic process of adapting well to trauma, adversity, threat, tragedy, or major sources of stress’ [8]. A positive outlook is an effective component of psychological resilience, which protects resilient people from depression and helps them obtain psychological resources [9]. Psychological resilience is also an independently related factor of quality of life in patients with first ischemic stroke [10]. A higher level of psychological resilience is related to a lower level of emotional distress and a higher quality of life [9]. From what is mentioned above, we can know that psychological resilience is an important outcome for stroke patients in early rehabilitation. Determining the key factors that affect the level of resilience after a stroke is important for planning and evaluating interventions for rehabilitation.
Hope, a dynamic and multi-level psychological process, is believed to be important in recovery and the perception of recovery from illness or injury. Qualitative and quantitative studies have shown that hope plays an important role in early post-stroke recovery [11,12,13] and is necessary for optimal recovery [14]. These studies have explored the important role of hope in post-stroke recovery, but have not explained the specific path of action.
Psychological resilience
The psychological resilience of patients over the first 6 months following a first stroke is much worse than that of the general population [15, 16] and healthy older population [17]. Few conditions demand resilience more than stroke does [18]. Psychological resilience can greatly affect the recovery and adjustment process of patients with stroke, and it may be an important determinant of their future living arrangements. Changes in psychological resilience may be due to a combination of environmental and personal factors. Resilience is a continuous process, not necessarily a characteristic that a person has or does not have. For example, a person may cope very well in one situation but show low psychological resilience in another one [19]. Therefore, resilience has dynamic properties, and it can be learned and enhanced. A review summarized the factors that contribute significantly to psychological resilience, including biological factors (such as brain structure and function and neurobiological systems), personal factors (such as optimism, self-esteem, and hope), and environmental-systemic factors (such as social support) [20].
Social support
Social support in this study refers to the spiritual and material help perceived, obtained, and used by patients with stroke, such as love and respect from others or groups, which can reduce stress. The research literature shows that a social support system is an important protective factor for individuals experiencing stressful events, and protective factors are necessary for the recovery process. Therefore, social support may be closely related to psychological resilience [21, 22]. Price et al. [23] found several prominent characteristics of stroke survivors with psychological resilience, one of which was the use of social support. Some researchers have developed group-based peer support interventions to improve the psychological resilience of patients with stroke, and the results have been positive [24]. However, few studies have been published on the relationship between psychological resilience and social support in convalescing patients with stroke; thus, it is necessary to further explore the relationship between them.
Self-esteem
Self-esteem reflects people’s feelings about themselves and is a multifaceted construct related to other psychological constructs, such as self-image, self-concept, self-perception, self-confidence, self-acceptance, self-esteem, and self-worth [25]. For a long time, self-esteem has been a variable of interest in mental health research and has become an important variable in the health care. In recent years, the impact of self-esteem on stroke rehabilitation has received more attention in the literature with focusing on patients with acute stroke in the rehabilitation [26,27,28,29]. Self-esteem is considered to be an important factor affecting the emotional and functional outcomes of patients with chronic diseases (such as stroke) [28]. However, stroke survivors reported low self-esteem [30, 31]. Studies have explored the antecedents of self-esteem of stroke patients [32, 33), and others have shown that self-esteem and social support jointly affect the practice of self-care behaviour of stroke patients [34]. However, there is still a lack of research on the psychological impact of self-esteem after brain injury. People who have low self-esteem following acquired brain injury (including stroke) may be less able to utilize co** strategies and manage the physical, cognitive, psychological and psychosocial consequences of the injury if they are less able to focus on competence over limitations, or to maintain a sense of self-worth over feelings of hopelessness [35]. People with high self-esteem are more likely to attempt to increase their feelings of self-worth, whereas people with low or fragile self-esteem may be more unconsciously concerned with protecting the limited self-esteem resources they have, therefore becoming more reluctant to risk failure or rejection [36]. Therefore, we try to broaden our understanding of self-esteem by studying the impact of self-esteem on psychological resilience.
Hope and its relationship with social support, self-esteem, and psychological resilience
Hope is a complex and multidimensional concept. Based on the findings of concept analysis, a multidimensional model of hope for people after stroke is proposed [37]. The key features depicted in the model include: (1) Hope being developed through a range of factors: internal (attitude, sense of self, previous experience), stroke-related (progress to date, severity), and external (family and friends, spiritual beliefs, staff); (2) Hope having 3 attributes - an inner state, an outcome-oriented attribute, and an active process; (3) Hope yielding positive outcomes that affect a person’s internal state (perseverance, motivation, co**, mood modulation) and recovery (increased participation, ongoing recovery, improved quality of life). There were 3 crucial factors in maintaining hope according to the model: a supportive environment (interconnectedness), a sense of belief in one’s self (positive attitude towards temporality and the future), and a belief that ongoing progress is possible (positive readiness and expectancy) [38].
Although hope can theoretically explain how social support and self-esteem affect patients’ psychological resilience after stroke, empirical studies are still in their infancy. Empirical studies from patients with other chronic diseases provided support for the relationship between these variables. Snyder’s theory of hope [39] shows that hope is a positive motivational state, which involves the evaluation of a person’s ability to achieve goals successfully, and may be affected by self-esteem. Specifically, self-esteem is an important motivator in the pursuit of self-worth. It can encourage individuals to use effective strategies to overcome difficulties, achieve goals, and have greater hope for the future [40]. Therefore, self-esteem is likely to play a positive role in improving hope. A narrative review [41] found that social support from friends and family members could be a potential factor in generating hope in stroke patients. In particular, social support can be a source of motivation and encouragement during the rehabilitation process, hel** to foster or maintain a sense of hope among stroke survivors. A study on adolescents after an earthquake found that hope mediated social support and post-traumatic growth [42]. Snyder et al. suggested that social support could improve the level of personal hope by establishing and expanding personal resources [43]. In addition, the results of empirical research support the positive effect of social support on hope [44]. Therefore, we believe that social support can increase levels of psychological resilience among patients after stroke by increasing hope.
In summary, the first 6 months following a first stroke is the key period of rehabilitation, during which the patient’s psychological resilience plays an important role. In the multidimensional model of hope for people after stroke, psychological resilience is an important positive result of hope. This model explains the internal antecedents, external antecedents, and positive results of hope, but lacks the support of empirical research. Therefore, this study focused on internal antecedent - self-esteem, external antecedent - social support, and consequence - psychological resilience (Fig. 1). The aim of this study is to explore the mediating effect of hope in the relationships between social support and self-esteem with psychological resilience among patients with stroke survivors in early rehabilitation. Based on the above analysis and the multidimensional model of hope after stroke proposed by Bright et al. [38], the following research hypotheses are put forward:
Hypothesis 1
Social support, hope and self-esteem of patients with stroke in early rehabilitation have a positive impact on their psychological resilience;
Hypothesis 2
Social support and self-esteem of patients with stroke in early rehabilitation have a positive impact on hope;
Hypothesis 3
The hope of patients with stroke in early rehabilitation is a mediator variable between social support and psychological resilience;
Hypothesis 4
The hope of patients with stroke in early rehabilitation is a mediator variable between self-esteem and psychological resilience.
Methods
Study design
A cross-sectional study design was used in this study.
Settings, samples and data collection
This cross-sectional study was conducted from October 2020 to May 2021 in the rehabilitation center of a tertiary hospital in Liaoning Province. Due to the requirement of a sample size of at least 200 for structural equation modeling [45] and the principle that the sample size should be 10 times for each variable according to regression analysis [46], a total of 210 inpatients stroke patients were finally recruited by convenience sampling method to participate in the study.
The criteria for the inclusion of patients were as follows: (1) met the diagnostic criteria of the Chinese Society of Neurology and Chinese Stroke Society 2018; and were diagnosed with stroke using cranial CT, DSA or MRI; (2) age ≥ 18 years; (3) had clear thought processes; (4) gave informed consent to participate voluntarily; and (5) a course of disease ≥ 2 weeks and ≤ 6 months. The exclusion criteria were as follows: (1) patients with transient ischemic attack; (2) those with major organ failure; (3) those unable to communicate using words; and (4) those diagnosed with a mental disorder before experiencing a stroke.
A paper questionnaire was used for the study’s survey from October 2020 to May 2021. Prior to distributing the survey, the researcher communicated with the participants, answered their questions in detail, and guided them to complete it by themselves. Rehabilitation physicians uniformly assessed patients’ level of functioning and disability using the Barthel Index rating scale [47]. As the researcher guided the participants to fill in the questionnaire one-on-one, the recovery rate and effectiveness rate of the questionnaire reached 100%. The patients participated in this study voluntarily and did not receive any compensation for filling in the questionnaire. Participants signed written consent forms before data collection and the data collected are only available to researchers and the Ethics Review Committee. This article reports according to the STROBE checklist.
Ethical consideration
The study was approved by the Ethics Committee of Sheng**g Hospital of China medical university (approval number: 2020PS737K). The study conforms to Declaration of Helsinki.
Measurements
Demographic data
Sociodemographic and disease-related data of patients with stroke were collected during the rehabilitation period, including patients’ gender, age, religious beliefs, marital status, residential area, educational level, medical insurance type, employment status, family per capita monthly income, stroke type, first or not first onset, and number of sequelae. The sequelae mainly included hemiplegia, speech disorder, sensory disorder, and swallowing disorder.
Psychological resilience
The Connor-Davidson Resilience Scale (CD-RISC), which was developed by Connor & Davidson [16], was used to measure the psychological resilience of patients with stroke. The Chinese version of CD-RISC has 25 items that are divided into three dimensions [48]: self-improvement (8 items), tenacity (13 items), and optimism (4 items). Each item is rated on a 5-point scale (0–4 points), and the total possible score ranges from 0 to 100. A higher score indicates greater psychological resilience. The internal consistency of the scale was 0.910, and Cronbach’s α for the three dimensions ranged from 0.600 to 0.880, and for the entire scale was 0.920. This instrument has acceptable concurrent validity; the total score correlates positively with hardiness (r = 0.83) and social support (r = 0.36) and negatively with perceived stress (r = -0.76) and stress vulnerability (r = -0.32).
Social support
Social support was measured using the Social Support Rating Scale (SSRS), which was developed by ** obstacles in the face of such frustrating events. Stroke patients with high education have a higher level of psychological resilience. Educational intervention also played a positive role in reducing helplessness and discomfort in other studies [58]. Therefore, during hospitalization, health providers should regularly popularize disease-related knowledge for stroke convalescent patients so that patients can become deeply familiar with the reason and treatment of stroke, which will help patients better understand the disease and receive treatment in the hospital, community, and family. Furthermore, the more sequelae, the lower the level of psychological resilience of stroke patients. The sequelae of stroke, such as hemiplegia, speech inability, sensory, and swallowing disorders, can bring great psychological pressure to patients, resulting in lower psychological resilience.
The above results on the influencing factors in the general characteristics of psychological resilience of stroke patients were basically consistent with other studies in patients with stroke. What caregivers can do is to use different focus care methods according to different characteristics of patients. Appropriate intervention and treatment measures are also needed to reduce the sequelae of stroke. At the same time, the author also found that the research on psychological resilience of stroke patients is relatively small. Considering the important role of psychological resilience in post-stroke depression and the characteristics of post-stroke depression, it is necessary to strengthen research on psychological resilience in the early rehabilitation after stroke.
The mediating role of hope in the relationships of social support and self-esteem with psychological resilience
Research shows that the first 6 months after a stroke are the period of physical and mental recovery [59]. Psychological resilience is an independent predictor of post-stroke depression and quality of life [60], and post-stroke depression can be alleviated by improving psychological resilience [61]. Using a cross-sectional survey, this study explored the roles of social support, self-esteem, and hope as predictors of psychological resilience in patients with stroke. This study found that social support and self-esteem were predictors of psychological resilience. When hope was included in a model of the relationship between social support and self-esteem with psychological resilience, the direct effects of social support and self-esteem were reduced, due to the mediating effect of hope.
The social support of patients with stroke during the early rehabilitation stage can indirectly affect their resilience levels, which is consistent with the results of other studies: A study of patients with breast cancer undergoing treatment found that hope played a complete mediating role between social support and resilience [62]. A study on patients with prostate cancer also showed that hope played a mediating role in the relationship between social support and psychological state [63]. Perceived social support can improve an individual’s overall level of happiness and promote the establishment of positive qualities, including hope [Limitations First, this cross-sectional study investigated only the level of psychological resilience of patients with stroke during the early stroke rehabilitation stage; however, psychological resilience is a dynamic process. We should investigate the level of psychological resilience of patients with stroke in different stages of the illness (i.e., the acute, recovery, and sequelae stages), and explore the status and the factors influencing the level of psychological resilience in in the different stages. Second, the Psychological Resilience Scale currently used is a universal scale. The specificity of the information yielded on the psychological resilience of patients with stroke in the convalescent stage needs to be improved. Develo** a psychological resilience scale suitable for this population is a necessary research direction, which should provide a reference for the prevention of, and solutions for psychological distress among patients with stroke and for implementing mental-health nursing interventions. Third, we explored the protective factors of psychological resilience, and the Multi-System Model of Resilience proposed by Liu, Reed, & Fung [77] showed that psychological resilience is also affected by risk factors (such as exposure to stress and adversity). Therefore, we need to explore methods for improving psychological resilience among patients with stroke in combination with their risk factors to improve their quality of life and reduce the incidence of post-stroke depression. Fourth, this study is a cross-sectional study, which hinders the causal inference between variables. In the future, longitudinal study design or experimental study can be considered to verify the cross-sectional study results and better explore the causal relationship. Therefore, the current cross-sectional study can provide preliminary support for the mediation process described. Finally, there are communalities in what is measured in resilience, social support and hope scales, given that resilience and social support are measured by the Hope scale to some extent. In the future, study should carefully examine the specific items within each scale to identify any potential redundancies or shared variance among the constructs, and provide a more comprehensive discussion on the potential interrelations among resilience, social support, and hope, highlighting the nuances and complexities of these constructs.
Conclusion
Despite some limitations, this study provides preliminary support for explaining and elucidating the mediating role of hope in the relationship between social support, self-esteem, and psychological resilience in in patients with stroke during the early rehabilitation stage. Psychological resilience is very important for improving a patients’ quality of life and alleviating post-stroke depression. Therefore, in future studies, the personality characteristics of patients with stroke should be evaluated as soon as possible to predict their level of psychological resilience and improve their social support system, as indicated during early stroke rehabilitation.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. The author confirmed that we didn’t use AI tools to analyse and draw insights from data as part of the research process. This manuscript has not been published or presented elsewhere in part or entirety and is not under consideration by another journal.
References
Kao CC, Chiang HT, Chen CY, Hung CT, Chen YC, Su LH, et al. National bundle care program implementation to reduce ventilator-associated pneumonia in intensive care units in Taiwan. Journal of microbiology, immunology, and infection. J Microbiol Immunol Infect. 2019;52(4):592–7. https://doi.org/10.1016/j.jmii.2017.11.001. Epub 2017/12/05.
Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2019;394(10204):1145–58. https://doi.org/10.1016/s0140-6736(19)30427-1.
Villa RF, Ferrari F, Moretti A. Post-stroke depression: mechanisms and pharmacological treatment. Pharmacol Ther. 2018;184:131–44. https://doi.org/10.1016/j.pharmthera.2017.11.005.
Medeiros GC, Roy D, Kontos N, Beach SR. Post-stroke depression: a 2020 updated review. Gen Hosp Psychiatry 2020 Sep-Oct;66:70–80. https://doi.org/10.1016/j.genhosppsych.2020.06.011. Epub 2020 Jun 27.
Hebert D, Lindsay MP, McIntyre A, Kirton A, Rumney PG, Bagg S, et al. Canadian stroke best practice recommendations: stroke rehabilitation practice guidelines, update 2015. Int J Stroke. 2016;11(4):459–84. https://doi.org/10.1177/1747493016643553.
Grabowska-Fudala B, Jaracz K, Gorna K, Miechowicz I, Wojtasz I, Jaracz J, et al. Depressive symptoms in stroke patients treated and non-treated with intravenous thrombolytic therapy: a 1-year follow-up study. J Neurol. 2018;265(8):1891–9. https://doi.org/10.1007/s00415-018-8938-0.
Zhou X, Liu Z, Zhang W, Zhou L. Resilience is associated with post-stoke depression in Chinese stroke survivors: a longitudinal study (273, pg 402, 2020). J Affect Disord. 2020;274:1232. https://doi.org/10.1016/j.jad.2020.06.024.
American Psychological Association. The road to resilience. 2017. Retrieved from https://www.apa.org/helpcenter/road-resilience.
Kim M, Kim K, Kim J-S. Impact of resilience on the health-related quality of life of adolescents with a chronic health problem: a structural equation approach. J Adv Nurs. 2019;75(4):801–11. https://doi.org/10.1111/jan.13888.
Liu ZH, Zhou X, Zhang W, Zhou LZ. Resilience is an independent correlate of the course of quality of life in patients with first-ever ischemic stroke. Int Psychogeriatr. 2021;33(6):567–75. https://doi.org/10.1017/S1041610220000587.
Burton CR. Living with stroke: a phenomenological study. J Adv Nurs. 2000;32(2):301–9. https://doi.org/10.1046/j.1365-2648.2000.01477.x.
Cross A, Schneider M. A preliminary qualitative analysis of the impact of hope on stroke recovery in women. Top Stroke Rehabil. 2010 Nov-Dec;17(6):484–95. https://doi.org/10.1310/tsr1706-484.
Nilsson I, Jansson L, Norberg A. To meet with a stroke: patients’ experiences and aspects seen through a screen of crises. J Adv Nurs. 1997;25(5):953–63. https://doi.org/10.1046/j.1365-2648.1997.1997025953.x.
Popovich JM, Fox PG, Burns KR. Hope in the recovery from stroke in the U.S. Int J Psychiatr Nurs Res. 2003;8(2):905–20.
Zhang W, Liu Z, Zhou X, Zhou L. Resilience among stroke survivors: a cohort study of the first 6 months. J Adv Nurs. 2020;76(2):504–13. https://doi.org/10.1111/jan.14247.
Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. https://doi.org/10.1002/da.10113.
Lim ML, Lim D, Gwee X, Nyunt MSZ, Kumar R, Ng TP. Resilience, stressful life events, and depressive symptomatology among older Chinese adults. Aging Ment Health. 2015;19(11):1005–14. https://doi.org/10.1080/13607863.2014.995591.
Michael K. Call to Action Enhancing Poststroke Resilience. Top Geriatr Rehabil. 2014;30(3):195–8. https://doi.org/10.1097/tgr.0000000000000018.
Wild K, Wiles JL, Allen RES. Resilience: thoughts on the value of the concept for critical gerontology. Ageing Soc. 2013;33:137–58. https://doi.org/10.1017/s0144686x11001073.
Herrman H, Stewart DE, Diaz-Granados N, Berger EL, Jackson B, Yuen T. What is resilience? Can J Psychiatry. 2011;56(5):258–65. https://doi.org/10.1177/070674371105600504.
Krueger EA, Upchurch DM. Sexual orientation, social support, and mental health resilience in a U.S. national sample of adults. Behav Med (Washington DC). 2020;1–9. https://doi.org/10.1080/08964289.2020.1825922. Epub 2020/10/15.
Lok N, Bademli K. The Relationship between the Perceived Social Support and Psychological Resilience in caregivers of patients with Schizophrenia. Community Ment Health J. 2021;57(2):387–91. https://doi.org/10.1007/s10597-020-00665-w.
Price P, Kinghorn J, Patrick R, Cardell B. Still there is beauty: one man’s resilient adaptation to stroke. Scand J Occup Ther. 2012;19(2):111–7. https://doi.org/10.3109/11038128.2010.519402.
Sadler E, Sarre S, Tinker A, Bhalla A, McKevitt C. Develo** a novel peer support intervention to promote resilience after stroke. Health Soc Care Community. 2017;25(5):1590–600. https://doi.org/10.1111/hsc.12336.
Fukuya Y, Fujiwara T, Isumi A, Doi S, Ochi M. Association of Birth Order with Mental Health Problems, Self-Esteem, Resilience, and happiness among children: results from A-CHILD study. Front Psychiatry. 2021;12. https://doi.org/10.3389/fpsyt.2021.638088.
Chen S, Lewthwaite R, Schweighofer N, Winstein CJ. Discriminant validity of a new measure of self-efficacy for reaching movements after stroke-induced hemiparesis. J Hand Ther. 2013 Apr-Jun;26(2):116– 22; quiz 123. https://doi.org/10.1016/j.jht.2012.09.002.
Vickery CD, Sepehri A, Evans CC. Self-esteem in an acute stroke rehabilitation sample: a control group comparison. Clin Rehabil. 2008;22(2):179–87. https://doi.org/10.1177/0269215507080142.
Vickery CD, Sepehri A, Evans CC, Lee JE. The association of level and stability of self-esteem and depressive symptoms in the acute inpatient stroke rehabilitation setting. Rehabil Psychol. 2008;53:171–9. https://doi.org/10.1037/0090-5550.53.2.171.
Vickery CD, Sherer M, Evans CC, Gontkovsky ST, Lee JE. The relationship between self-esteem and functional outcome in the acute stroke-rehabilitation setting. Rehabil Psychol. 2008;53:101–9. https://doi.org/10.1037/0090-5550.53.1.101.
Ellis-Hill CS, Horn S. Change in identity and self-concept: a new theoretical approach to recovery following a stroke. Clin Rehabil. 2000;14(3):279–87. https://doi.org/10.1191/026921500671231410.
Penninx BW, van Tilburg T, Boeke AJ, Deeg DJ, Kriegsman DM, van Eijk JT. Effects of social support and personal co** resources on depressive symptoms: different for various chronic diseases? Health Psychol. 1998;17(6):551–8. https://doi.org/10.1037//0278-6133.17.6.551.
Park EY, Kim JH. An analysis of self-esteem in stroke survivors: the interaction between gender, income, and the presence of a spouse. J Ment Health. 2016;25(2):159–64. https://doi.org/10.3109/09638237.2015.1101430.
Shida J, Sugawara K, Goto J, Sekito Y. Relationship between self-esteem and living conditions among stroke survivors at home. Jpn J Nurs Sci. 2014;11(4):229–40. https://doi.org/10.1111/jjns.12024. Epub 2013 Jul 16.
Muhlenkamp AF, Sayles JA. Self-esteem, social support, and positive health practices. Nurs Res. 1986 Nov-Dec;35(6):334–8.
Kendall E, Terry DJ. Psychosocial adjustment following closed head injury: a model for understanding individual differences and predicting outcome. Neuropsychological Rehabilitation. 1996;6:101–32. https://doi.org/10.1080/713755502.
Zeigler-Hill V. The connections between self-esteem and psychopathology. J Contemp Psychother. 2011;41(3):157–64. https://doi.org/10.1007/s10879-010-9167-8.
Bright FA, Kayes NM, McCann CM, McPherson KM. Understanding hope after stroke: a systematic review of the literature using concept analysis. Top Stroke Rehabil. 2011 Sep-Oct;18(5):490–508. https://doi.org/10.1310/tsr1805-490.
Cross A, Schneider M. A preliminary qualitative analysis of the impact of hope on stroke recovery in women. Top Stroke Rehabil. 2010;17(6):484–95. https://doi.org/10.1310/tsr1706-484.
Snyder CR. Hope theory: rainbows in the mind. Psychol Inq. 2002;13(4):249–75. https://doi.org/10.1207/s15327965pli1304_01.
Setliff AE, Marmurek HHC. The mood regulatory function of autobiographical recall is moderated by self-esteem. Pers Individ Dif. 2002;32(4):761–71. https://doi.org/10.1016/s0191-8869(01)00078-2.
Soundy A, Stubbs B, Freeman P, Coffee P, Roskell C. Factors influencing patients’ hope in stroke and spinal cord injury: a narrative review. Int J Therapy Rehabilitation. 2014;21(5):210–8. https://doi.org/10.12968/ijtr.2014.21.5.210.
Zhou X, Wu X, Zhen R. Self-esteem and hope mediate the relations between social support and post-traumatic stress disorder and growth in adolescents following the Ya’an earthquake. Anxiety Stress Co**. 2018;31(1):32–45. https://doi.org/10.1080/10615806.2017.1374376.
Snyder CR, Michael ST, Cheavens JS. Hope as a psychotherapeutic foundation of common factors, placebos, and expectancies. The heart and soul of change: what works in therapy. Washington, DC, US: American Psychological Association; 1999. pp. 179–200.
Yadav S. Perceived social support, hope, and quality of life of persons living with HIV/AIDS: a case study from Nepal. Qual Life Res. 2010;19(2):157–66. https://doi.org/10.1007/s11136-009-9574-z. Epub 2010/01/05.
Lambert LSJORM. Beyond significance testing: Reforming Data Analysis methods in behavioral research. Am J Psychiatry. 2007;10(4):713–6. https://doi.org/10.1176/appi.ajp.162.3.643-a.
Riley RD, Ensor J, Snell K, Harrell FE, Martin GP, Reitsma JB, et al. Calculating the sample size required for develo** a clinical prediction model. BMJ. 2020;368m441. https://doi.org/10.1136/bmj.m441.
Mahoney FI. DW Barthel 1965 FUNCTIONAL EVALUATION: THE BARTHEL INDEX. Maryland State Med J 14 61–5.
Yu X, Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Social Behav Personality: Int J. 2007;35(1):19–30. https://doi.org/10.2224/sbp.2007.35.1.19.
**ao SY. Theoretical basis and application of social support rating scale. J Clin Psychol Med. 1994; (2):98–100.
GuoYu Y, ZhengZhi F, BenLi XIA. The reliability, validity and National Norm of Social Support Scale in Servicemen. Chin Mental Health J. 2006;20(5):309–12.
Herth K. Abbreviated instrument to measure hope-development and psychometric evaluation. J Adv Nurs. 1992;17(10):1251–9. https://doi.org/10.1111/j.1365-2648.1992.tb01843.x.
Rosenberg M. Society and the adolescent self-image. Princeton: Princeton University Press; 1965.
Vispoel WP, Boo J, Bleiler T. Computerized and paper-and-pencil versions of the Rosenberg Self-Esteem Scale: a comparison of psychometric features and respondent preferences. Educ Psychol Meas. 2001;61(3):461–74. https://doi.org/10.1177/00131640121971329.
Diana S. The Basics of Structural Equation Modeling. University of Northern Colorado. https://www.lexjansen.com/wuss/2006/tutorials/TUT-Suhr.pdf.
Fradelos EC, Latsou D, Mitsi D, Tsaras K, Lekka D, Lavdaniti M, et al. Assessment of the relation between religiosity, mental health, and psychological resilience in breast cancer patients. Contemp Oncol (Pozn). 2018;22(3):172–7. https://doi.org/10.5114/wo.2018.78947.
Chen YY, Koenig HG. Traumatic stress and religion: is there a relationship? A review of empirical findings. J Relig Health. 2006;45(3):371–81. https://doi.org/10.1007/s10943-006-9040-y.
Liu X. The Resilience Affecting Factors of Chronic Patients and Medical Social Worker’s Strategy [Master’s degree]. Chongqing University, China; 2019.
Fawzy FI, Fawzy NW, Arndt LA, Pasnau RO. Critical-review of psychological interventions in cancer care. Arch Gen Psychiatry. 1995;52(2):100–13. https://doi.org/10.1001/archpsyc.1995.03950140018003.
Mahendran N, Kuys SS, Brauer SG. Recovery of ambulation activity across the first six months post-stroke. Gait Posture. 2016;49:271–76. https://doi.org/10.1016/j.gaitpost.2016.06.038.
Mahendran N, Kuys SS, Brauer SG. Recovery of ambulation activity across the first six months post-stroke. Gait Posture. 2016;49:271–6. https://doi.org/10.1016/j.gaitpost.2016.06.038. Epub 2016/07/31.
de Lemos CM, Moraes DW, Pellanda LC. Resilience in patients with ischemic heart disease. Arq Bras Cardiol. 2016;106(2):130–5. https://doi.org/10.5935/abc.20160012. Epub 2016/01/28.
Hsu H-T, Juan C-H, Chen J-L, Hsieh H-F. Mediator roles of Social Support and Hope in the relationship between body image distress and resilience in breast Cancer patients undergoing treatment: a modeling analysis. Front Psychol. 2021;12. https://doi.org/10.3389/fpsyg.2021.695682.
Zhao X, Sun M, Yang Y. Effects of social support, hope and resilience on depressive symptoms within 18 months after diagnosis of prostate cancer. Health Qual Life Outcomes. 2021;19(1). https://doi.org/10.1186/s12955-020-01660-1.
**ang G, Teng Z, Li Q, Chen H, Guo C. The influence of perceived social support on hope: a longitudinal study of older-aged adolescents in China. Child Youth Serv Rev. 2020;119(c):105616. https://doi.org/10.1016/j.childyouth.2020.105616.
Kemer G, Atik G. Hope and social support in high school students from urban and rural areas of Ankara, Turkey. J Happiness Stud. 2012;13(5):901–11. https://doi.org/10.1007/s10902-011-9297-z.
Morley CA, Kohrt BA. Impact of peer support on PTSD, hope, and functional impairment: a mixed-methods study of child soldiers in Nepal. J Aggress Maltreatment Trauma. 2013;22(7):714–34. https://doi.org/10.1080/10926771.2013.813882.
Simmons BL, Gooty J, Nelson DL, Little LM. Secure attachment: implications for hope, trust, burnout, and performance. J Organizational Behavior: Int J Industrial Occup Organizational Psychol Behav. 2009;30(2):233–47. https://doi.org/10.1002/job.585.
Li Z, Yin X. How social support influences hope in college students: the mediating roles of self-esteem and self-efficacy. Psychol Dev Educ. 2015;31(5):610–7. https://doi.org/10.16187/j.cnki.issn1001-4918.2015.05.13.
Ong AD, Edwards LM, Bergeman CS. Hope as a source of resilience in later adulthood. Pers Indiv Differ. 2006;41(7):1263–73. https://doi.org/10.1016/j.paid.2006.03.028.
Kirmani MN, Sharma P, Anas M, Sanam R. Hope, resilience and subjective well-being among college going adolescent girls. Int J Humanit Social Sci Stud. 2015;2(1):262–70.
Mullin A. Children’s hope, resilience and autonomy. Ethics Social Welf. 2019;13(3):230–43. https://doi.org/10.1080/17496535.2019.1588907.
Satici SA. Psychological vulnerability, resilience, and subjective well-being: the mediating role of hope. Pers Indiv Differ. 2016;102:68–73. https://doi.org/10.1016/j.paid.2016.06.057.
Granek L, Barrera M, Shaheed J, Nicholas D, Beaune L, D’agostino N, Antle B. Trajectory of parental hope when a child has difficult-to-treat cancer: a prospective qualitative study. Psycho-oncology. 2013;22(11):2436–44. https://doi.org/10.1002/pon.3305.
Condly SJ. Resilience in children: a review of literature with implications for education. Urban Educ. 2006;41(3):211–36. https://doi.org/10.1177/0042085906287902.
Mashiach-Eizenberg M, Hasson-Ohayon I, Yanos PT, Lysaker PH, Roe D. Internalized stigma and quality of life among persons with severe mental illness: the mediating roles of self-esteem and hope. Psychiatry Res. 2013;208(1):15–20. https://doi.org/10.1016/j.psychres.2013.03.013.
Cotter VT, Gonzalez EW, Fisher K, Richards KC. Influence of hope, social support, and self-esteem in early-stage dementia. Dement (London). 2018;17(2):214–24. https://doi.org/10.1177/1471301217741744.
Liu JJW, Reed M, Fung KP. Advancements to the Multi-system Model of Resilience: updates from empirical evidence. Heliyon. 2020;6(9). https://doi.org/10.1016/j.heliyon.2020.e04831.
Acknowledgements
Thank you to all clinical patients who participated in this study from 2020 to 2022 for providing us with research data. Thank you also to the doctoral supervisors of the school for their guidance on this study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conception and design: Boru SUN; Nan WANG; Fengjiao ZHANG; Acquisition of data: Nan WANG; Ke LI; Yan YANGAnalysis and interpretation of data: Boru SUN; Yan YANGDrafting the manuscript: Boru SUN; Nan WANG; Yan YANGFinal approval of the version to be published: Boru SUN; Nan WANG; Fengjiao ZHANG; Ke LI; Yan YANGAgreed to be accountable for all aspects of the work: Boru SUN; Nan WANG; Fengjiao ZHANG; Ke LI; Yan YANG.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
All study participants provided informed consent, and the study design was approved by the appropriate ethics review board(Sheng**g hospital of China medical university 2020PS737K). Participants signed written informed consent forms before data collection and the data collected are only available to researchers and the Ethics Review Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, B., Wang, N., Li, K. et al. The mediating effects of hope on the relationships of social support and self-esteem with psychological resilience in patients with stroke. BMC Psychiatry 24, 340 (2024). https://doi.org/10.1186/s12888-024-05744-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05744-w