Abstract
Background
Bone tumors account for approximately 6% of all cancers in children. Malignant bone tumors, commonly occurring in children and adolescents, are associated with high mortality and morbidity. The overall survival of children with primary malignant bone tumors is affected by the stage of disease, time of diagnosis, and treatment response. Despite advanced treatment modalities with chemotherapy, surgery, and radiotherapy, bone tumor is the third leading cause of death in children with malignancy. Patients with metastatic disease at diagnosis have poor outcomes compared to localized disease at presentation. The 5-year Overall Survival and event-free survival in children with primary malignant bone tumors were 85.2% and 69.2%. The study aimed to assess the clinicopathological profile and treatment outcomes of children with primary malignant bone tumors in our setup.
Materials and methods
A hospital-based cross-sectional study was conducted on 95 children who met the inclusion criteria through structured questionnaire. The collected data were analyzed using a statistical package for social sciences (SPSS) version 25. P-value < 0.05 was considered to be statistically significant. Kaplan Meier survival estimate was used for overall and event-free survival analysis.
Results
A total of ninety-five patients met the study inclusion criteria and the median age at diagnosis with primary malignant bone tumors was 10 years, with an interquartile range of 8–12 years. The duration of the illness from the onset of symptoms to the oncologic treatment center ranges from three weeks to 2 years with a mean duration of five months. Swelling was the commonest presenting symptom accounting for 95.8% (n = 91). Lower extremity was the commonest primary site of involvement accounting for 55.8% (n = 53) of children with primary malignant bone tumors. Osteosarcoma was the commonest malignant bone tumor constituted 66.3% (n = 63), followed by Ewing sarcoma at 33.7% (n = 32).
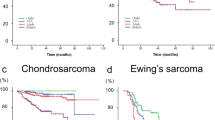
About 41.2% (n = 39) of children had metastatic disease at presentation and the lung was the commonest site of distant metastasis. The Kaplan Meier survival estimate analysis showed the 1-year and 5-year overall survival probabilities for all pediatric primary malignant bone tumor patients were 65% (95% CI: 0.3–0.56) and 38% (95% CI:0.19–0.47) respectively. The 1-year and 5-year event-free survival probabilities were 55% (95% CI: 0.32–0.73) and 33% (95% CI: 0.10–0.59). The stage of the disease at presentation had a significant association with the outcome (p = 0.023).
Conclusion
Our study showed the mean duration of the illness from the onset of symptoms to the oncologic treatment center was 5 months ranging from 3 weeks to 2 years. More than one-third of the presented with metastatic disease at presentation. The 1-year and 5-year overall survival (OS) probabilities of children with primary malignant bone tumors were low in our setup compared to other studies.
Similar content being viewed by others
Introduction
Bone tumors arise from bone and closely related structures in the skeletal system [1, 2]. Primary malignant bone tumors are more common in children and young adolescents than in the adult population, constitute approximately 6% of all cancers in children, and are highly associated with high mortality and morbidity [3,4,5]. Osteosarcoma is the most common malignant bone tumor in childhood followed by Ewing sarcoma, boys are slightly more affected than girls (1.5: 1) and the peak incidence is in the second decade of life [6,7,8]. A study done in Germany from 1987–2011 showed the median age of occurrence of primary bone tumors was 10–14 years old with an average age of 12 years. The incidence rates of specific bone sarcomas are age-related; the first well-defined peak occurs during the second decade of life. Up to 56% of malignant bone tumors will arise around the knee in the distal femur and tibial bone in those under the age of 20 years. The other most common site is the pelvis, which is numerically the most common site of presentation for both Ewing sarcoma and chondrosarcoma [4, 9].
About 80% of osteosarcomas occur in the extremities; the distal femur, proximal tibia, and proximal humerus are the commonest sites of occurrence. Whereas, Ewing sarcoma family tumors are evenly distributed between the axial and appendicular skeleton [7, 10,11,12]. In a review of the histopathological pattern of primary bone tumors and tumor-like lesions in Ile-Ife, Nigeria; Osteosarcoma was the most common primary malignant bone tumor accounting for 42%. About 42.86% occurred in the distal third of the femur, 14.28% in the distal tibia, 14.28% in the proximal tibia, 9.52% in the mandible, and the proximal third of the femur, the maxilla, humerus, and calcaneus 4.76% each.
In a pathology review of 335 patients with bone tumors in Ethiopia; 158 (47%) had benign tumors and 177 (53%) had malignant tumors. Osteochondroma was the most common benign bone tumor and osteosarcoma constituted 62% of all primary malignant bone neoplasms, followed by Ewing sarcoma, and chondrosarcoma. The most common age groups affected by primary bone tumors were 10–29 years and the most common locations of presentation for primary malignant bone tumors were the distal femur and proximal tibia [13, 14].
Genetic factors; such as Li-Fraumeni syndrome, RB gene mutation, environmental factors, and previous radiation therapy may increase the risks of develo** primary bone tumors [15].
Bone tumors in children were the third leading death of malignancy and the trend of survival rate was increasing with an overall survival rate of 79% with a significant impact on the quality of life with high mortality and morbidity [16, 17]. The mean survival times for patients with osteosarcoma, and Ewing sarcoma were approximately 54.9 and 58.1 months respectively [18,19,20]. Despite the advanced combined treatment modalities using chemotherapy, surgery, and radiotherapy, malignant bone tumors affect the quality of life of children and contribute significantly to childhood cancer morbidity and mortality. The five-year survival rate and event-free survival for localized malignant bone tumors were 81% and 68% respectively, whereas the overall survival for metastatic bone tumors was 42% [21,22,23,24].
Based on Estimates of Cancer Incidence in Ethiopia in 2015 [25], bone and cartilage tumors accounted for 7% of all childhood cancers. However, there was no well-documented data about primary bone tumor patterns and survivals in our setup. Thus, this study aimed to provide an overview of the histopathological pattern of primary bone tumors, describing the anatomic sites, and assessing the outcomes of the primary bone tumors treated at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia.
Methodology
Study setting
The study was conducted at the Department of Pediatrics and Child Health, Haemato-Oncology Unit, Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Tikur Anbessa Specialized Hospital is the largest tertiary hospital in the country established in 1974, and administered by Addis Ababa University. Tikur Anbessa Specialized Hospital is one of the largest pediatric haemato-oncology treatment centers in the county, and a separate unit for children with cancer began in March 2013 with initiatives taken by the International Network for Cancer Treatment and Research, USA (INCTR-USA) in collaboration with George Town University Hospital. The pediatric haemato-oncology wards have 42 inpatient beds dedicated to pediatric cancer patients and the unit gives both inpatient and outpatient services for more than 800 patients every month.
Sampling
All radiologically and pathologically confirmed primary bone tumors in children under the age of 15 years from January 1, 2014, to June 30, 2022, were included. Children with secondary metastatic bone tumors, tissue biopsies revealing benign bone tumors, and patients with incomplete records were excluded. A total of ninety-five (n = 95) patients met the inclusion criteria and were included in our study. A hospital-based cross-sectional study was carried out through a self-administered structured questionnaire. Data were collected from July 1, 2022, to September 30, 2022.
Data collection and data analysis
Data were collected by the principal investigator and trained General Practitioners using structured self-administered questionnaires. The study questionnaires had four parts: Part I was about the socio-demographic characteristics of the study participants, Part II was about the clinical profile of patients at presentation, Part III was about the diagnosis and diagnostic investigations, and Part IV was about the treatment profiles and outcomes of primary malignant bone tumors in children treated at Tikur Anbessa Specialized Hospital.
After selecting the study cases, the data was collected from the registration log book, the patient card, and the follow-up chart by the data collectors. The administered questionnaire encompasses the socio-demography profile, clinical profile, and outcome. ODK version 2022.3.3 software was used to collect the data along with the Kobo Toolbox server to store the collected data. Data was entered into Epi data version 3.1 and exported to SPSS version 25 for analysis. P-value < 0.05 was considered to be statistically significant. The Kaplan Meier survival was used to estimate the first, and fifth year overall and event-free survival analysis.
Overall survival (OS) represents the time from the date of first diagnosis to the date of last follow-up or death from any cause.
Event-free survival is the time duration after treatment completion for a primary bone tumor that the patient remains free of any events.
Events include treatment abandonment, relapse, and death.
Data quality control and management
To ensure the quality of data, the structured questionnaire checklists were tested on 5% of the sample. Problems highlighted during the pre-test were corrected before the start of the data collection. Each question was properly coded; continuous cross-checking was done both during the pre-test and data collection period by the principal investigator. The collected data were checked for completeness and consistency on each day of data collection.
Ethical approval
Ethical approval was obtained from the Research and Publication Committee of Pediatrics and Child Health Department (DRCP), School of Medicine, College of Health Sciences, Addis Ababa University. Confidentiality was fully maintained during data collection and analysis. Participants would be anonymous during the dissemination of results.
Results
Socio-demographic characteristics of patients
During the study period, a total of ninety-five patients met the study inclusion criteria and were included in the study. Our study showed that 52.6% (n = 50) were males and 47.4% (n = 45) were females with male to female ratio of 1.1: 1. The median age at diagnosis was 10 years, with an interquartile range of 8–12 years. Nearly half of the children, 48.4% (n = 46) were between the ages of 5 and 10 years and 45.2% (n = 43) were between 11- 15 years. Most of the children; 87.4% (n = 83) came from out of Addis Ababa, the capital city of the country (Table 1).
Clinical profile of children with primary bone tumors at Tikur Anbessa Specialized Hospital
The duration of the illness from the onset of symptoms to the oncologic treatment center ranges from three weeks to 2 years with a mean duration of 5 months. The average duration of a delay from the primary referring institute to the oncologic treatment center was 5.8 ± 8.2 SD days and the average time of treatment initiation after visiting the treatment center was more than 1 month (35.7 days).
Swelling was the commonest presenting symptom accounting for 95.8% (n = 91). The commonest primary site of involvement was the lower extremity accounting for 55.8% (Fig. 1). Anthropometric nutritional assessment showed that 14.7% (n = 14) were severely acutely malnourished and 25.3% (n = 24) were moderately malnourished at presentation (Table 2).
Diagnosis and diagnostic work-up
Our study showed, that 58.1% (n = 54) of the patients had localized disease, and 41.2% (n = 39) of the patients presented with metastatic disease at presentation commonly to the lungs. More than one-third of patients; 40.5% (n = 32) had chest metastases on the Chest CT scan, 17.9% (n = 10) had chest metastases on Chest X-ray, 29.2% (n = 7) had abdominal-pelvic metastases and 21.7% (n = 5) of Ewing sarcoma had bone marrow involvement. Sixty-three (66.3%) patients were diagnosed with Osteosarcoma and 32 (33.6%) patients were diagnosed with Ewing sarcoma (Table 3). Only 75.8% (n = 72) had a histologic diagnosis of bone tumors. Histologic diagnosis was confirmed for 68% (n = 49) and 32% (n = 23) of osteosarcoma and Ewing sarcoma respectively (Fig. 2). The commonest histologic sub-type of Osteosarcoma in our study was chondroblastic osteosarcoma accounting for 44.9% (n = 22) of patients (Fig. 3).
Treatment profile of children with primary bone tumors
Sixty-eight of the patients (71.6%) started treatment; 64.7% (n = 44) with curative intent and 35.3% (n = 24) with palliative treatment intent. Chemotherapy was the most common type of treatment modality offered for 98.5% (n = 67) of patients, whereas surgical treatment was done for 30.5% (n = 29) and 9.4% (n = 3) of Ewing sarcoma patients received radiotherapy. Chemotherapy was administered as first-line treatment for 82.4% (n = 56) patients, whereas surgical treatment was offered as first-line therapy for 17.6% (n = 12). More than half of the patients, 62.7% (n = 42), received the Osteosarcoma chemotherapy protocol. Ewing sarcoma patients were treated with VCD/IE, VCD, and other (VAC, Metronomic) protocols; 22.4% (n = 15), 5.9% (n = 4), and 10.3% (n = 7) respectively. Nearly half of the patients, 32 (47.1%) completed the chemotherapy. Among the surgically treated patients, 79.3% (n = 23) were amputated, and debulking of the mass was done for two (6.9%) patients (Table 4).
Treatment outcomes of children with primary bone tumors
During the study period, the survival status showed that 46.3% (n=44) were died, 27.4% (n=26) were alive and for 26.3% (n=25) the status was unknown. After completion of chemotherapy, 46.9% (n=15) had no new event, 43.8% (n=14) had relapsed, and for 9.3% (n=3) the status was unknown, lost to follow-up. Kaplan Meier analysis showed that the median overall survival time for all pediatric patients who had primary malignant bone tumors was around 1 year (95%CI: 0.8-3.12). The 1-year and 5-year overall survival probabilities for all pediatric primary malignant bone tumor patients were 65% (95%CI:0.3-0.56) and 38% (95%CI:0.19-0.47) respectively (Fig. 4). The 1-year and 5-year event-free survival probabilities were 55 % (95 CI: 0.32-0.73) and 33% (95% CI: 0.10-0.59) (Fig. 5).
Factors affecting treatment outcomes
To identify the associated factors with survival status, a chi-square test of independence was performed. Statistical significance was considered at a level of significance of 5%. Our finding revealed that survival status was independent of age, sex, duration of illness, and primary site of occurrence (p = 0.6, 0.78, 0.39, and 0.07) respectively, whereas it was dependent on the stage of the disease at diagnosis (p = 0.023), and the histology of the tumor; either osteosarcoma or Ewing sarcoma (P = 0.05) (Table 5).
A log-rank test was calculated to see if there was a difference between those treatments completed and those treatments not completed or started in terms of the distribution of time to survival and death occurrence and showed that there is a significant difference in groups in terms of the distribution of time survival (P ≤ 0.015). Those children who completed the chemotherapy had better survival than those who didn’t complete or started at all (Fig. 6).
Discussion
Primary malignant bone tumors are one of the common malignant solid tumors in childhood and adolescence age, but the clinical profile and outcome status were not well studied in Low and Middle-Income Countries (LMICs). Most studies revealed that the median age of diagnosis was 10–14 years, with males slightly more affected than females with a 1.5:1 ratio [9, 24, 26].
Our study showed that the median age of diagnosis of primary malignant bone tumor was 10 years with an interquartile range of 8–12 years, which showed slight occurrence at an earlier age compared to another study done in Germany, which showed a median age of 10–14 years [9]. The difference might be due to the participants in our study being under 15 years old.
The duration of illness from the onset of symptoms to the oncologic treatment center ranges from 3 weeks to years with a mean duration of 5 months. In our study, the major clinical presentation was swelling (95.8%), followed by pain (53.7%), whereas pain was the most common presentation in a study done in India [2]. The site of occurrence is similar to other studies but variation of clinical presentation may be due to age differences and benign lesions were also included in the other studies [2, 26,27,28].
In our study, 41.9% (n = 39) were diagnosed with advanced (Metastatic) disease, and 58.1% (n = 54) with localized disease at presentation. An institution-based retrospective study done at St. Jude Children’s Research Hospital Studies showed 71% of bone tumor patients had localized disease and 29% had metastasis at the diagnosis. The high incidence of metastatic presentation at diagnosis in our setup might be due to a lack of awareness of cancer, delayed seeking of medical care (delayed presentation), delayed referral, and delayed diagnosis.
Osteosarcoma was the commonest primary malignant bone tumor accounting for 66.3% (n = 63) followed by Ewing sarcoma 33.7%) in our study, similar results were found in the study done in Ethiopia; Osteosarcoma accounts for 62%, followed by Ewing sarcoma; 15.2% [13] and in South Iran, which was done among 100 patients; 57 patients were diagnosed with Osteosarcoma and 43 patients with Ewing sarcoma [29].
The lower extremity was the most common primary site of involvement (55.8%) followed by the upper extremity (12.6%) which was similar to the prospective study in Lebanon which revealed the lower extremity as the commonest site of occurrence in 89.5% of patients [23].
Effective adjuvant or neoadjuvant regimens of chemotherapy with timely local control with surgery have dramatically improved the prognosis of patients with localized osteosarcoma evidenced by many studies reaching the five-year amore th [27, 28, 30, 31]. The 5-year overall survival with a combination of surgery with chemotherapy for localized primary malignant bone tumors has increased to 60–70% in better setup [6, 29, 32]. The five-year survival rate and event-free survival for localized malignant bone tumors in developed countries even improved to 81% and 68% respectively, whereas the overall survival for metastatic bone tumors was dismal [21,22,23,24].
In our study, the 1-year and 5-year overall survival probabilities for all pediatric primary malignant bone tumor patients were 65% 95% CI:0.3–0.56) and 38% (95% CI:0.19–0.47) respectively. The 1-year and 5-year event-free survival probabilities were 55% (95% CI: 0.32–0.73) and 33% (95% CI: 0.10–0.59), which was lower than other studies [33]. The overall survival in our setup was lower than in the other studies; this might be due to the delayed presentation, treatment abandonment, fewer surgical interventions, and limited radiotherapy services.
Previous reviews on primary metastatic osteosarcoma treated with cooperative osteosarcoma study group protocols showed that the overall survival of osteosarcoma was significantly correlated with patient age, site of the primary tumor, number and location of metastases, number of involved organ systems, and histologic response of the primary tumor to preoperative chemotherapy [32, 34, 35]. Our finding revealed that survival status was dependent on the stage of the disease at diagnosis (p = 0.023), and the histology of the tumor; either osteosarcoma or Ewing sarcoma (P = 0.050. However, the survival status was independent of age, duration of illness, and primary site of occurrence. These findings are supported by similar findings in South Iran [33]. Our study revealed that children who completed the chemotherapy had better survival than those who didn’t complete or started treatment (P ≤ 0.015).
In this study, the survival status was unknown for one-fourth of the patients (26.3%); those patients were lost to follow-up, and addressing their status with a phone call was attempted, but the registered phones were not working or picked up during the time of data collection.
Strengths and limitations of the study
The study was done in one of the biggest tertiary referral hospitals, serving as the only center for pediatric cancer patients till recently, and our study reports patterns and outcomes of primary bone tumors in children. Our study focused on the overall picture of survival status and determinants of outcomes of primary malignant bone tumors rather than delineating and analyzing separately based on the types of primary malignant bone tumors, which might need a large cohort to study the outcomes and determinants of each type of primary malignant bone tumor. The other limitation of this research is that this study didn’t specifically investigate the effects of local control measures on the overall survival rates of children with primary bone tumors, which needs to be addressed in future studies as local control measures such as surgery or radiotherapy may play a significant role in the survival of children with solid cancers.
Conclusion
In our study, most bone tumor patients seek medical care after an average of five months, and more than one-third of the patients presented with advanced stage (Metastatic disease). The 1-year and 5-year overall survival and event-free survival probabilities for all pediatric primary malignant bone tumor patients were low and emphasis has to be given to improving childhood cancer survival in Low and Middle-Income Countries (LMICs). Future research should identify barriers and psycho-social issues for late presentation, loss to follow-up, and treatment abandonment in children and adolescents diagnosed with primary bone tumors.
Availability of data and materials
The datasets used and analyzed are available upon reasonable request from the corresponding author.
References
Bamanikar S, Pagaro P, Kaur P, et al. Histopathological study of primary bone tumors and tumor-like lesions in a medical teaching hospital. JKIMSU. 2015;4:46.
Kokode DN, Wilkinson A. A clinicopathological study of lesions of bone. Int J Clin Diagn Pathol. 2018;1(1):17–22. https://www.patholjournal.com/articles/30/2-1-8-587.pdf.
Malawer MM, Sternheim A. Operative techniques in orthopedic surgical oncology. In: Philadelphia. 2012. p. 418. https://shop.lww.com/Operative-Techniques-in-Orthopaedic-Surgical-Oncology/p/9781975174071.
Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F. WHO classification of tumors of tumors of soft tissue and bone. 2013. https://publications.iarc.fr/Book-And-Report-Series/Who-Classification-Of-Tumours/WHO-Classification-Of-Tumours-Of-Soft-Tissue-And-Bone-2013.
Johnson LC. A general theory of bone tumors. Bull N Y Acad Med. 1953;29(2):164–71 PMID: 13009398; PMCID: PMC1877293.
Picci P. Osteosarcoma (Osteogenic sarcoma). Orphanet J Rare Dis. 2007;2:6. https://doi.org/10.1186/1750-1172-2-6.
Caudill JS, Arndt CA. Diagnosis and management of bone malignancy in adolescence. Adolescent Med. 2007;18:62–78.
Hartford CM, Wodowski KS, Rao BN, et al. Osteosarcoma among children aged 5 years or younger. PediatrHematol Oncol. 2006;28:43–7.
Kaatsch P, Strothotte J, Becker C, et al. Pediatric bone tumors in Germany from 1987 to 2011: incidence rates, time trends, and survival. Acta Oncol. 2016;55(9–10):1145–51.
Stiller CA, Bielack SS, Jundt G, et al. Bone tumors in European children and adolescents. 2006;42(13):2124–35.
Grier HE. The Ewing’s family of tumors. Ewing’s sarcoma and primitive neuroectodermal tumors. Pediatr Clin North Am. 1997;44:991–1004.
Obata H, Ueda T, Kawai A, et al. Clinical outcome of patients with Ewing sarcoma family of tumors of bone in Japan. Cancer. 2007;109:767–7752.
Weyessa TG, Kindie EA, Yefter ET. Histopathological pattern of primary bone tumours at the Black Lion Specialized Hospital, Addis Ababa, Ethiopia: a retrospective cross-sectional, 2015-2019. Pan Afr Med J. 2022;41:62. https://doi.org/10.11604/pamj.2022.41.62.27905.
Rodríguez-Galindo C, Liu T, Krasin MJ, Wu J, Billups CA, Daw NC, Spunt SL, Rao BN, Santana VM, Navid F. Analysis of prognostic factors in ewing sarcoma family of tumors: review of St Jude Children’s Research Hospital studies. Cancer. 2007;110(2):375–84. https://doi.org/10.1002/cncr.22821. PMID: 17569105.
Heare T, Hensley MA, Dell’Orfano S. Bone tumors: osteosarcoma and Ewing’s sarcoma. Curr Opin Pediatr. 2009;21:365–72.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63(1):11–30.
i Tortajada JF, Tornero OB, García JO, Claudio-Morales L, i Castell JG, Perales VM, Casas LM . Factores de riesgo para los tumores óseos malignos pediátricos [Risk factors for pediatric malignant bone tumors]. A Pediatr (Barc). 2005;63(6):537–47. Spanish. https://doi.org/10.1016/s1695-4033(05)70254-x. PMID: 16324620.
Brown HK, Schiavone K, Gouin F, et al. Biology of bone sarcomas and new therapeutic developments. Calcif Tissue Int. 2018;102(2):174–95.
Siclari VA, Qin L. Targeting the osteosarcoma cancer stem cell. J Orthop Surg Res. 2010;5(1):78.
Xu G, Wu H, Xu Y, et al. Homogenous and heterogenous prognostic factors for patients with bone sarcoma. Orthop Surg. 2021;13(1):134–44.
Meazza C, Scanagatta P. Metastatic osteosarcoma: a challenging multidisciplinary treatment. Expert Rev Anticancer Ther. 2016;16(5):543–56.
Geraci M, Birch JM, Alston RD, Moran A, Eden TO. Cancer mortality in 13 to 29-year-olds in England and Wales, 1981–2005. Br J Cancer. 2007;97(11):1588–94.
Abou Ali B, Salman M, Ghanem KM, Boulos F, Haidar R, Saghieh S, et al. Clinical Prognostic Factors and Outcome in Pediatric Osteosarcoma: Effect of Delay in Local Control and Degree of Necrosis in a Multidisciplinary Setting in Lebanon. J Glob Oncol. 2019;5:1–8. https://doi.org/10.1200/JGO.17.00241.
Ries L, Smith M, Gurney J, et al. Cancer incidence and survival among children and adolescents: United States SEER program 1975–1995. Bethesda: National Institutes of Health; 1999. p. 99–4659.
Memirie ST. Estimates of cancer incidence in Ethiopia in 2015 using population-based registry data. Addis Ababa University. 2018.
Aina OJ, Adelusola KA, Orimolade AE, Akinmade A. Histopathological pattern of primary bone tumors and tumor-like lesions in Ile-Ife, Nigeria. Pan Afr Med J. 2018;29:193.
Provisor AJ, Ettinger LJ, Nachman JB, et al. Treatment of nonmetastatic osteosarcoma of the extremity with preoperative and postoperative chemotherapy: a report from the Children’s Cancer Group. J Clin Oncol. 1997;15(1):76–84.
Meyers PA, Heller G, Healey J, et al. Chemotherapy for nonmetastatic osteogenic sarcoma: the Memorial Sloan-Kettering experience. J Clin Oncol. 1992;10(1):5–15.
Fuchs N, Bielack SS, Epler D, et al. Long-term results of the co-operative German Austrian-Swiss osteosarcoma study group’s protocol COSS86 of intensive multidrug chemotherapy and surgery for osteosarcoma of the limbs. Ann Oncol. 1998;9(8):893–9.
Bacci G, Briccoli A, Rocca M, et al. Neoadjuvant chemotherapy for osteosarcoma of the extremities with metastases at presentation: recent experience at the Rizzoli Institute in 57 patients treated with cisplatin, doxorubicin, and a high dose of methotrexate and ifosfamide. Ann Oncol. 2003;14(7):1126–34.
Kager L, Zoubek A, Potschger U, Cooperative German-Austrian-Swiss Osteosarcoma Study Group, et al. Primary metastatic osteosarcoma: presentation and outcome of patients treated on neoadjuvant Cooperative Osteosarcoma Study Group protocols. J Clin Oncol. 2003;21(10):2011–8.
Womer RB, West DC, Krailo MD, Dickman PS, Pawel BR, Grier HE, et al. Randomized controlled trial of interval-compressed chemotherapy for the treatment of localized Ewing sarcoma: a report from the Children’s Oncology Group. J Clin Oncol. 2012;30(33):4148–54. https://doi.org/10.1200/JCO.2011.41.5703.
Bordbar M, Sarfaraz A, Haghpanah S, Zekavat O, Zareifar S, Zarei T. The Outcome of Children With Malignant Bone Tumors: A Single-Center Experience. Glob Pediatr Health. 2021;8:2333794X211042238. https://doi.org/10.1177/2333794X211042238.
Nesbit ME Jr, Gehan EA, Burgert EO Jr, et al. Multimodal therapy for the management of primary, nonmetastatic Ewing’s sarcoma of bone: a long-term follow-up of the First Intergroup study. J Clin Oncol. 1990;8:1664–74.
Grier HE, Krailo M, Tarbell N, et al. Addition of ifosfamide and etoposide to standard chemotherapy for Ewing’s sarcoma and primitive neuroectodermal tumor of bone. N Engl J Med. 2003;348:694–701.
Acknowledgements
We would like to thank the Department of Pediatrics and Child Health for giving us this chance to do the research. We express our deep sense of gratitude and respect to the patients and their attendants who passed through challenges in their treatment course and disease state.
Funding
This research has no funding source.
Author information
Authors and Affiliations
Contributions
T.L.: Inception of the idea, data collection, data analysis, write up; S.Y.: Data analysis, review of the manuscript, and prepared tables 1-5; A.M: Data analysis, review of the manuscript, prepared figures 1-6; G.A.: Data analysis, review of the manuscript, and write-up. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval for the present study was obtained from the Research and Publication Committee of the Pediatrics and Child Health Department (DRCP), School of Medicine, College of Health Sciences, Addis Ababa University, and the College Institutional Review Board (IRB). The requirement for informed consent was waived because of the anonymous nature of the data.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lingerih, T., Yeshiwas, S., Mohamedsaid, A. et al. Patterns and treatment outcomes of primary bone tumors in children treated at tertiary referral hospital, Ethiopia. BMC Cancer 24, 394 (2024). https://doi.org/10.1186/s12885-024-12169-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12169-x