Abstract
Purpose
Previous randomized studies have shown a survival benefit of using regorafenib but a high rate of adverse events in unresectable colorectal cancer patients. To reduce these adverse events and improve the tolerability, we examined the appropriate dose of regorafenib based on body weight.
Methods
We used a nationwide claims database in Japan and examined the efficacy and safety of regorafenib for patients with metastatic colorectal cancer between groups divided by body weight (60 kg) and median average dose (120 mg) between 2013 and 2018. We also assessed overall survival (OS) and adverse events between these groups.
Results
We identified 2530 Japanese patients (heavy weight/high dose: 513, light weight/low dose: 921, heavy weight/low dose: 452, and light weight/high dose: 644). There was no significant difference in the adverse events and OS after inverse probability treatment weighting (IPTW) adjustment between heavy weight/high dose group and light weight/low dose group (hazard ratio, HR=0.97). Among the light-weight patients, higher average dose was associated with shorter OS (IPTW adjusted HR=1.21, 95% CI 1.05 – 1.39, Table 3) while among the heavy-weight patients, there was no significant difference in OS between high and low dose groups (IPTW adjusted HR=1.14, 95% CI 0.95 – 1.37).
Conclusion
The findings suggest that a low dose of regorafenib for light-weight patients may be as safe and effective as high doses for heavy-weight patients. Further studies should be conducted to identify an appropriate dose based on each patient's physique and condition.
Similar content being viewed by others
Introduction
Regorafenib is an oral multi-kinase inhibitor that inhibits the protein kinase activities via antiangiogensis, oncogenesis, and tumor microenvironment. Regorafenib is approved as a single agent for treatment of patients with metastatic colorectal cancer (CRC), who failed previous therapies at an initial dose of 160 mg once daily on days 1-21 of each 28-day cycle [1, 2]. Previous randomized trials (CORRECT and CONCUR) have shown some efficacy of regorafenib, compared with that of placebo [3, 4]. However, various treatment-related adverse events, such as hand-foot skin reaction, fatigue, and rash, have been reported. The most common adverse events of grade 3-5 were hand-foot skin reaction (17%), fatigue (10%), diarrhoea (7%), hypertension (7%), and rash or desquamation (6%) [3, 4]. The incidence of serious adverse events was 9%.3
Studies in the real-world setting also showed high proportions of adverse events. There were many initial dose reductions, dose reductions during treatment, and discontinuations due to adverse events [5,6,7]. The selection of an appropriate regorafenib dose should require simultaneous consideration of anti-tumor effects. For reducing occurrence of adverse effects, several studies have tried to adjust the initial dose reduction [8,9,10,11]. For example, Suzuki T. et al. conducted a phase II study of regorafenib with a starting dose of 120 mg/day, and then the dosage was increased to 160 mg/day on day 15; however, the disease control rate was lower than the statistically expected rate.10 A randomized multicenter, open-label, phase II study (ReDOS) conducted a dose-escalation strategy (a starting dose 80 mg/day with a weekly escalation, per 40 mg increment, to 160 mg/day), which showed a comparable effect activity and a lower incidence of adverse events than general scheme.11 However, there is still no study focusing on personalized regorafenib dose modification.
The establishment of personalized regorafenib dose usage is imperative for clinical guidance, because it is helpful to optimize the anti-tumor effect and to enhance the life quality of patients. Multiple approaches should be explored to develop alternative strategies for identifying an optimal dose based on patients’ characteristics. Post hoc analysis of the CORRECT trial suggests regorafenib (160 mg once daily) has comparable efficacy in Japanese and non-Japanese subpopulations, but regorafenib-associated adverse events occurred more frequently in the Japanese subpopulation than in the non-Japanese one [12].
Japanese and non-Japanese groups were significantly different in body weight, with a difference of about 10 kg. Body weight is a possible factor to affect the anti-tumor affect and treatment-related adverse events for regorafenib treatment. Therefore, personalized regorafenib dose modification based on body weight is a promising research direction.
In the present study using a nationwide claims database in Japan, we hypothesized that low dose of regorafenib in CRC patients with low body weight would achieve similar survival benefit and incidences of adverse events as high dose in patients with high body weight.
Methods
The present study was conducted according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [13]. The study was approved by the Ethics Committee of the Graduate School and Faculty of Medicine, Kyoto University (approval number: R2719, November 18, 2020), which waived the requirement for an informed consent due to the anonymous nature of the data.
Data sources
This study used the medical claims database maintained by Medical Data Vision Co, Ltd., (MDV; Tokyo, Japan). This database contains patient-level information on demographic characteristics; diagnoses coded according to the International Classification of Diseases, 10th revision (ICD-10); outcome at discharge; and prescription information, such as dose, number of days of supply, and quantity. The database comprises data of inpatient and outpatient medical care from 269 hospitals in different regions throughout Japan and covers approximately 17% of Japanese acute care hospitals. The distributions of age and sex in the source population were similar to those in the Japanese census, and several studies using this database have been reported [14,15,16].
Study cohort
We selected data for CRC patients aged over 20 years who were diagnosed between June 2013 (the time when regorafenib was launched in Japan) and September 2018 by using ICD-10 codes in the database. We included the patients who received regorafenib and did not have a diagnosis of metastases but in whom the tumor at the primary site was considered unresectable. We excluded (1) regorafenib-treated patients with diseases other than CRC, such as a gastrointestinal stromal tumor, small intestine cancer, and liver cancer; (2) patients who had no body weight data; (3) patients who received an inappropriate initial dose (less than 80 mg or more than 160 mg); (4) patients who received other chemotherapy simultaneously with regorafenib; (5) patients who received repeated administration of regorafenib; and (6) patients who had less than 1 year follow-up period. We set the cutoff point as 60 kg body weight and median average dose across the whole follow-up period (120 mg). The cutoff value of 60 kg was close to the median body weight (56.7 kg) and was set for easy understanding. By using the average dose, we investigated not only the appropriate initial dose but also the appropriate maintenance dose. The high average dose group (>120 mg) includes many patients starting 160 mg initial dose and patients starting reduced initial dose of 120 mg and later increasing to 160 mg. We divided the patients into four groups based on different weight and dose combinations: heavy weight/low average dose group (heavy/low group), heavy weight/high average dose group (heavy/high group), light weight/high average dose group (light/high group), light weight/low average dose group (light/low group).
Outcome measures
The primary outcome of this study was overall survival (OS) between heavy/high group and light/low group adjusted by inverse probability of treatment weighting (IPTW). OS was defined as the time from regorafenib initiation until death from any cause. Patients who lost to follow-up or survived until September 2018 were censored at the date of the last visit. We also retrieved the following patient information from the database: age, body weight, body mass index (BMI), comorbidities, the primary site of disease, metastatic sites, previous systemic anticancer agents administered, doctor’s department, and subsequent anticancer agents administered. We utilized data on comorbidities registered before the first prescription of regorafenib by using ICD-10 codes.
Statistical analysis
Demographics, disease characteristics, and cancer history of heavy/high and light/low groups are displayed. Descriptive summaries of continuous data present the group mean and standard deviation. Descriptive summaries of categorical data present the category counts as frequencies and percentages. To compare the drug exposure, adverse events, and use of subsequent anticancer agents between the heavy/high and light/low groups, we used two-sample t-test or Mann-Whitney U test for continuous variables and Fisher’s exact test for categorical variables.
To account for selection bias, the observed difference in patient characteristics were adjusted by using inverse probability of treatment weighting (IPTW) method. Specifically, we first estimated the propensity score which reflecting the probability of being in heavy/high vs. light/low groups, using a logistic regression. The following patient characteristics and clinical risk factors were included in the models: age, sex, the primary site of disease, comorbidities, previous systemic anticancer agents, and doctor’s department. When comparing heavy/high group vs. heavy/low group or light/high group vs. light/low group, body weight was also included in the logistic regression as a confounding factor. The propensity scores were then used to weight each patient with the aim of balancing the characteristics between two groups (e.g., heavy/high vs. light/low). The imbalance of baseline characteristics between groups were assessed using standardized differences (SD) [17] in the original (unweighted) study population and the weighted population, respectively. A SD less than 0.1 was considered indicative of a negligible imbalance between groups.
The adjusted Kaplan–Meier curves and log-rank tests based on IPTW were computed to compare OS between different groups. Moreover, an inverse probability weighted Cox proportional hazards regression model with dose group as the sole predictor was used to determine the relative change in hazards (i.e., the IPTW-adjusted hazards ratio [HR]) associated with high dose or low dose. To check the robustness of the results in the present study, we performed sensitivity analysis by setting the median body weight (56.7 kg) of all patients as the cut-off. We further performed subgroup analysis to investigate the IPTW-adjusted HR of high vs. low dose within the light and high body weight subgroups. A nominal P < 0.05 (two-sided) was considered statistically significant. Statistical analyses were performed using SAS (Version 9.4; SAS Institute, Cary, NC) and R statistical software version 4.03 (https://www.r-project.org/).
Results
Patients
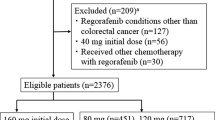
The number of patients who received regorafenib was 4205, of whom we excluded 1675 patients based on the exclusion criteria. The patient number of heavy/high group was 513, light/low group was 921, heavy/low group was 579, and light/high group was 577. The flow diagram for the present study is shown in Fig 1. Table 1 displays demographics, disease characteristics, and cancer history of heavy/high and light/low groups, in addition to the comparisons of unadjusted and adjusted standardized difference between these two groups. Compared with the heavy/high group, patients in light/low group were more likely to be older, be treated by doctors from Department of Surgery, more female sex, less likely to have diabetes mellitus, to be administered systemic anticancer agents of fluorouracil, tegafur/gimeracil/oteracil, and irinotecan. After IPTW adjustment, the characteristics in the weighted population for heavy/high and light/low groups are comparable (SD for most variables was < 0.1).
Effectiveness
There was no significant difference in OS between the heavy/high group and the light/ low group after IPTW adjustment (HR=0.97; 95% CI 0.79 – 1.20, p=0.81)) (Fig 2). Comparison of drug exposure, adverse events, and subsequent anticancer agents between these two groups was shown in Table 2. Treatment duration was longer (51 days vs. 49 days, p=0.043) and total dosage was higher (5600 mg vs. 3160 mg, p < 0.001) in heavy/high group. There were no significant differences in the adverse events. Sensitivity analysis based on median body weight (56.7 kg) showed no significant difference in OS (IPTW adjusted HR=0.89; 95% CI 0.73 – 1.08, p=0.19) (Fig 3). In the subgroup of light-weight patients, higher average dose was associated with shorter OS (IPTW adjusted HR=1.21, 95% CI 1.05 – 1.39, , p=0.01) (Table 3) while among the heavy-weight patients, there was no significant difference in OS between high and low dose groups(IPTW adjusted HR=1.14, 95% CI 0.95 – 1.37, p=0.17) (Table 3). Comparison of drug exposure, adverse events, and subsequent anticancer agents in the subgroup of light-weight patients was shown in Supplemental Table 1. Mean time of treatment duration was longer in light/low group and some adverse events rates (oral mucositis, rash/desquamation, and hepatotoxicity) were higher in light/high group.
Discussion
Using a nationwide claims database, this study firstly investigated the appropriate dose of regorafenib based on body weight to improve survival. The present study showed that light-weight CRC patients who received reduced average dose may have no significant improvement/difference in survival or adverse event as heavy-weight patients who received high average dose. High average dose use among light-weight patients was associated with shorter OS. Among the heavy-weight patients, dose reduction of regorafenib had similar efficacy as the standard dose 160 mg once daily.
In CRC patients, previous randomized trials of regorafenib demonstrated not only a good efficacy but also a high proportion of adverse events [3, 4]. Since adverse events were observed mainly within the first cycles of treatment, [4, 5] several studies have been conducted focusing on the initial dose reduction [8,9,10,11]. These studies reported that the reduced initial dose groups experienced lower treatment-related toxicity and comparable effect, compared with the 160 mg initial dose groups. However, there were few discussions of reducing the maintenance dose.
The adequate initial and maintenance dose of cytotoxic anticancer agents is determined based on the results of the Phase I study. Because these agents show a typical dose-toxicity relationship, an adequate dose would be maximum tolerated dose (MTD). On the other hand, most oral targeted anticancer agents including regorafenib have an extensive interindividual pharmacokinetic variability and a narrow therapeutic window [18]. Therefore, an initial and maintenance dose finding of new oral targeted therapies should be determined based on individual patient’s characteristics [19]. Regorafenib would be given later in the series of treatments, and given the patient’s quality of life, setting a minimum dose as the initial or maintenance dose with satisfying anti-tumor effect and less adverse events may be the most appropriate treatment strategy. However, the initial dose of regorafenib was set as MTD from a traditional Phase I trial, and it can be sub-optimal [2, 20, 21]. Ideally, the dose should be personalized based on patients’ predictive bio-markers and/or blood drug concentrations, but currently there is no definite available method [22]. In the main analysis, the median duration of treatment was within two months, and a certain proportion of patients were considered to be discontinued due to adverse events. The proportion of adverse events and treatment duration were not different between the heavy/high group and the light/low group. On the other hand, the total dosage was significantly higher in the heavy/high group. In subgroup analysis with light-weight patients, the light/low group showed a longer treatment duration. This result might be due to the tendency of the lower adverse events in the light/low group. Therefore, a reduced-dose administration for both initial dose and average dose should be done more aggressively, especially for light-weight patients.
Due to the nature of the database, the present study had some limitations. First, several pieces of information were missing (e.g., performance status, grades of adverse events, KRAS mutation, reasons for treatment discontinuation, and therapeutic evaluation). We could not determine progression-free survival and disease control rates from the database. Second, there were many censored cases in the OS analysis. If patients changed hospitals or decided to opt for the end-of-life care at other places such as own home or hospice, it is impossible to follow-up patient outcomes. Finally, since most of the patients were Japanese, the patients in our study were not representative of the general population in the world. In a previous Japanese study, the patients were older and thinner and had more adverse events [12]. Thus, similar studies based on population from more geographically diverse regions are needed.
Conclusion
We firstly performed a comparative analysis of heavy-weight CRC patients treated with high average regorafenib dose and light-weight CRC patients treated with low average regorafenib dose using a large nationwide cohort of patients with CRC. There was no significant difference in survival, and reduced doses of regorafenib were considered appropriate for light-weight patients. Moreover, heavy-weight CRC patients may achieve similar survival benefit with reduced doses as compared to the standard dose. The results of this study are helpful in providing appropriate guidance about regorafenib dose to CRC patients.
Availability of data and materials
The data that support the findings of this study are available from Medical Data Vision Co, Ltd. But restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the corresponding authors upon reasonable request and with permission of Medical Data Vision Co, Ltd.
Abbreviations
- BMI:
-
Body mass index
- CRC:
-
Colorectal cancer
- IPTW:
-
Inverse probability of treatment weighting
- MTD:
-
Maximum tolerated dose
- OS:
-
Overall survival
- SD:
-
Standardized differences
References
Schmieder R, Hoffmann J, Becker M, Bhargava A, Müller T, Kahmann N, et al. Regorafenib (BAY 73–4506): antitumor and antimetastatic activities in preclinical models of colorectal cancer. Int J Cancer. 2014;135(6):1487–96.
Strumberg D, Scheulen ME, Schultheis B, Richly H, Frost A, Büchert M, et al. Regorafenib (BAY 73–4506) in advanced colorectal cancer: a phase I study. Br J Cancer. 2012;106(11):1722–7.
Li J, Qin S, Xu R, Yau TC, Ma B, Pan H, et al. Regorafenib plus best supportive care versus placebo plus best supportive care in Asian patients with previously treated metastatic colorectal cancer (CONCUR): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2015;16(6):619–29.
Grothey A, Van Cutsem E, Sobrero A, Siena S, Falcone A, Ychou M, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381(9863):303–12.
Yamaguchi K, Komatsu Y, Satoh T, Uetake H, Yoshino T, Nishida T, et al. Large-Scale, prospective observational study of regorafenib in Japanese patients with metastatic colorectal cancer in a real-world clinical setting. Oncologist. 2019;24(7):e450–7.
Ducreux M, Petersen LN, Öhler L, Bergamo F, Metges JP, de Groot JW, et al. Safety and effectiveness of regorafenib in patients with metastatic colorectal cancer in routine clinical practice in the prospective, observational CORRELATE study. Eur J Cancer. 2019;123:146–54.
Nakashima M, Ide K, Kawakami K. Comparison of Standard Initial Dose and Reduced Initial Dose Regorafenib for Colorectal Cancer Patients: A Retrospective Cohort Study. Target Oncol. 2019;14(3):295–306.
Osawa H. Response to regorafenib at an initial dose of 120 mg as salvage therapy for metastatic colorectal cancer. Mol Clin Oncol. 2017;6(3):365–72.
Tabchi S, Ghosn M. Regorafenib: start low and go slow. Target Oncol. 2015;10(3):445–7.
Suzuki T, Sukawa Y, Imamura CK, Masuishi T, Satake H, Kumekawa Y, et al. A Phase II study of regorafenib with a lower starting dose in patients with metastatic colorectal cancer: exposure-toxicity analysis of unbound regorafenib and its active metabolites (RESET Trial). Clin Colorectal Cancer. 2020;19(1):13-21.e3.
Bekaii-Saab TS, Ou FS, Ahn DH, Boland PM, Ciombor KK, Heying EN, et al. Regorafenib dose-optimisation in patients with refractory metastatic colorectal cancer (ReDOS): a randomised, multicentre, open-label, phase 2 study. Lancet Oncol. 2019;20(8):1070–82.
Yoshino T, Komatsu Y, Yamada Y, Yamazaki K, Tsuji A, Ura T, et al. Randomized phase III trial of regorafenib in metastatic colorectal cancer: analysis of the CORRECT Japanese and non-Japanese subpopulations. Invest New Drugs. 2015;33(3):740–50.
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18(6):805–35.
Joo WJ, Ide K, Kawasaki Y, Takeda C, Seki T, Usui T, Kawakami K. Effectiveness and safety of early enteral nutrition for patients who received targeted temperature management after out-of-hospital cardiac arrest. Resuscitation. 2019;135:191–6.
Tanaka S, Seto K, Kawakami K. Pharmacoepidemiology in Japan: medical databases and research achievements. J Pharm Health Care Sci. 2015;1:16.
Shinkawa K, Yoshida S, Seki T, Yanagita M, Kawakami K. Risk factors of venous thromboembolism in patients with nephrotic syndrome: a retrospective cohort study. Nephrol Dial Transplant. 2020;36(7):1199–206.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–107.
Sparreboom A, Verweij J. Advances in cancer therapeutics. Clin Pharmacol Ther. 2009;85(2):113–7.
Groenland SL, Mathijssen RHJ, Beijnen JH, Huitema ADR, Steeghs N. Individualized dosing of oral targeted therapies in oncology is crucial in the era of precision medicine. Eur J Clin Pharmacol. 2019;75(9):1309–18.
Sunakawa Y, Furuse J, Okusaka T, Ikeda M, Nagashima F, Ueno H, et al. Regorafenib in Japanese patients with solid tumors: phase I study of safety, efficacy, and pharmacokinetics. Invest New Drugs. 2014;32(1):104–12.
Mross K, Frost A, Steinbild S, Hedbom S, Büchert M, Fasol U, et al. A phase I dose-escalation study of regorafenib (BAY 73–4506), an inhibitor of oncogenic, angiogenic, and stromal kinases, in patients with advanced solid tumors. Clin Cancer Res. 2012;18(9):2658–67.
Callebout E, Ribeiro SM, Laurent S, De Man M, Ferdinande L, Claes KBM, et al. Long term response on Regorafenib in non-V600E BRAF mutated colon cancer: a case report. BMC Cancer. 2019;19(1):567.
Acknowledgements
Not applicable.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Masayuki Nakashima, Kan Li, Sheng Luo, and Hong Zhao. The first draft of the manuscript was written by Masayuki Nakashima, Kan Li, Sheng Luo, and Hong Zhao, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. The Ethics Committee of the Graduate School and Faculty of Medicine, Kyoto University approved the study (November 18, 2020, approval number: R2719) , and waived the requirement for an informed consent due to the anonymous nature of the data.
Consent for publication
Not applicable.
Competing interests
K.K. received an advisory fee from Shin Nippon Biomedical Laboratories, Ltd., JMDC Inc., AGREE Inc.; research funds from Sumitomo Dainippon Pharma Co, Ltd., Pfizer Inc., Stella Pharma Corporation, CMIC Co., Ltd., Suntory Beverage & Food Ltd., Medical Platform Co., Ltd., and Real World Data, Co., Ltd.; and holds stocks in Real World Data, Co., Ltd. There are no patent products under development or marketed products to declare relevant to these companies. Other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Table 1.
Comparison of drug exposure, adverse events, and subsequent anticancer agents.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nakashima, M., Li, K., Chen, Q. et al. Appropriate dose of regorafenib based on body weight of colorectal cancer patients: a retrospective cohort study. BMC Cancer 23, 1268 (2023). https://doi.org/10.1186/s12885-023-11720-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11720-6