Abstract
Background
Cytomegalovirus (CMV) retinitis is a common opportunistic infection in patients with acquired immunodeficiency syndrome. The common funduscopic manifestations are haemorrhagic necrotising variety and granular variety. Frosted branch angiitis (FBA), as a special form, when it occurred after antiretroviral therapy(ART), could possibly be associated with immune reconstitution. We report a case of FBA secondary to CMV infection-associated unmasking immune reconstitution inflammatory syndrome (IRIS).
Case presentation
A 27-year-old man with human immunodeficiency virus infection developed FBA after 35 days of ART. The left Aqueous humour (AqH) tested positive for CMV DNA, and the patient was diagnosed with CMV retinitis. The degree of intraocular inflammation was reflected by increased levels of interleukin (IL)-6 and IL-8 in AqH. After anti-CMV treatment and continuous ART for several months, his FBA and vision significantly improved. CMV DNA became undetectable in the left AqH, and the IL-6 and IL-8 levels in AqH decreased.
Conclusion
FBA could be a sign of CMV-associated unmasking IRIS. Anti-CMV treatment alone or combination with steroid treatment may be administered, depending on the changes in CMV DNA load and immunologic profile of AqH.
Similar content being viewed by others
Background
Frosted branch angiitis (FBA) is a special form of vasculitis, affecting the entire retina. The funduscopic findings of FBA include bilateral widespread retinal vasculitis with severe sheathing of the retinal vessels, resembling frosted branches of a tree, especially at the periphery, and mild to moderate iritis or vitritis. In this article, we reported a case of FBA secondary to cytomegalovirus (CMV) infection-associated unmasking immune reconstitution inflammatory syndrome (IRIS).
Case presentation
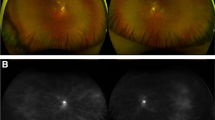
A 27-year-old young man, who previously had sexual contact with other men, was diagnosed with human immunodeficiency virus(HIV) infection 2 months ago. His CD4 + T cell count was 33 cells/μL. His serum anti-cytomegalovirus immunoglobulin M (IgM) was 23.6 U/mL (normal range: 0–18 U/mL), and CMV IgG was 139.0 U/mL (normal range:0–12 U/mL). His serum CMV DNA load was 4.54 × 103 copies/mL. The patient had no ocular symptoms and signs. No abnormalities were found on funduscopic screening examination (Fig. 1A). The preemptive anti-CMV treatment was not performed. His acid-fast smear of sputum, interferon-gamma release assay for Mycobacterium tuberculosis, and tuberculin skin test were negative. The IgM antibodies of rubella virus, herpes simplex virus(HSV), varicella-zoster virus(VZV), and Epstein-Barr virus(EBV) were all negative. The IgM and IgG antibodies of toxoplasma gondii, mycoplasma, and legionnella were all negative. The specific antibody of syphilis was negative. The blood sugar level was normal. Abdominal ultrasound screening, chest computed tomography, and brain magnetic resonance imaging were normal. Then, the patient received antiretroviral therapy (ART), including tenofovir, lamivudine, and efavirenz as well as oral co-trimoxazole, two tablets daily, for primary prophylaxis of Pneumocystis jirovecii pneumonia.
Changes observed in the patient’s eye examination. A Normal bilateral eyes appearance before antiretroviral therapy (ART). B After 5 weeks of ART, the left eye showed sheathing of the retinal vessels appearing like frosted branches of a tree without haemorrhages, necrosis, and occlusion. C Eye ultrasound revealed mild vitreous haze in the left eye after 5 weeks of ART. D No oedema in the macular area by optical coherence tomography were seen after 5 weeks of ART. E After 6 weeks of anti-CMV treatment, frosted branch angiitis in the left eye had significantly improved. F After 6 months of anti-CMV treatment, the retinal perivenous exudate in the left eye had resolved
On the 35th day of ART, the patient complained of floaters and blurred vision in the left eye and was admitted to our hospital due to worsening of eyesight. No other systemic abnormal symptoms and signs had been found, such as fever, rashes, cough, watering nose, sneeze, sore throat, parotid enlargement, mouth ulcer, diarrhoea, and bloody stool, etc. His CD4 + T cell count rapidly increased to 172 cells/μL. The HIV RNA load was 1.80 × 103 copies/mL. The left and right eyes were not red and swollen. His visual acuity was 20/20 in the right eye and 20/30 in the left eye. Bilateral intraocular pressures were normal. Slit-lamp examination showed diffuse punctate keratic precipitates and positive aqueous flare in the left eye. The size of the pupils and the light response were normal. The lens was transparent. Fundal examination revealed extensive retinal perivenous exudate, forming frosted branch vascular sheathing in the left eye (Fig. 1B). At the lower border of the right eye, peripheral retinitis, characterized by white granular exudates with minimal haemorrhage, was detected. Eye ultrasound revealed a slightly vitreous haze (Fig. 1C). Optical coherence tomography did not reveal macular oedema (Fig. 1D). The serum CMV DNA became negative (< 1.0 × 103 copies/mL). The level of C-reactive protein was 5.60 mg/L (normal range:0.00–5.00 mg/L). The levels of antistreptolysin O and rheumatoid factor were normal. Blood screening results of autoantibodies were all negative. A 100 μL sample of Aqueous humour (AqH), collected by anterior chamber puncture, was sent to Bei**g Zhi De medical laboratory science finite company. CMV DNA in the left AqH was 6.54 × 105copies/mL. Using BD-Pharmingen cytometric bead array, the interleukin (IL)-6 and IL-8 levels in the AqH were 2845.0 pg/mL (normal range: 1–50 pg/mL) and 967.8 pg/mL (normal range: 0–20 pg/mL), respectively. The DNA of HSV, EBV, and VZV were all negative in the left AqH. He was treated with intravitreal ganciclovir (2 mg twice a week for a total of four times) and intravenous ganciclovir (5 mg/kg twice daily for 2 weeks, followed by 5 mg/kg/day for 1 month). No non-steroidal anti-inflammatory drug was prescribed for the patient. His previous ART regimen was continued. Oral co-trimoxazole, two tablets daily, was continued. His FBA significantly improved (Fig. 1E). Thereafter, he had to switch to foscarnet at 180 mg/day because of leukopenia. Subsequently, foscarnet was replaced with oral ganciclovir (3 g/day). During the sixth-month follow-up, the peripheral granular lesion in his right eye subsided, and the vascular sheath-like exudates in the left eye resolved (Fig. 1F). His visual acuity became 20/25 in the left eye. His serum CMV DNA was undetectable. CMV DNA in the left AqH was also negative (< 1.0 × 103 copies/mL), and the levels of IL-6 and IL-8 in the left AqH decreased to 28.5 pg/mL and 5.6 pg/mL, respectively. His CD4 + T cell count was 131 cells/μL, and HIV RNA load was 30.3 copies/mL. His serum CMV IgM was negative, and CMV IgG exceeded 180.0 U/mL.
Discussion and conclusion
This was the first case that met the criteria for diagnosing early unmasking IRIS-FBA [1]. His condition was classified as a re-activation of a latent CMV infection. Short-term ART decreased the CMV DNA in his blood to undetectable levels [2]. However, subacute visual loss and floaters developed in his left eye. Detectable CMV DNA in the intraocular fluid is crucial for CMV retinitis diagnosis and differentiation from primary FBA or other infections. The elevated levels of IL-8 and IL-6 (principal cellular sources from monocytes and macrophages) in the AqH, as an indicator of active retinitis, obviously decreased following the anti-CMV treatment [3,4,5]. In this case, anti-CMV treatment monotherapy decreased the CMV DNA load as well as IL-8 and IL-6 levels in the AqH. Along with this, the patient’s eyesight improved, and perivascular exudation regressed. Thus, systemic steroid treatment was not required.
CMV retinitis is an important cause of blindness in individuals with advanced HIV infection and is characterized by intraretinal haemorrhages, white zones of retinitis, retinal oedema, and vasculitis. FBA is a special form of retinal vasculitis. This may be primary FBA or secondary to ocular infectious diseases, such as CMV, syphilis, HSV, VZV, tuberculosis, toxoplasmosis, and non-infectious diseases, such as autoimmune diseases and haematological malignancies in the non-HIV-infected population [6]. Antigen-antibody complex deposition and direct CMV infection of the vessel wall are the underlying pathogeneses [7, 8]. In the setting of HIV infection, FBA is an uncommon sign. Apart from the syphilis-related case [9], reported cases were exclusively associated with CMV retinitis [7, 8, 10,11,12,13,14,15,16] (summarised in Table 1). Currently, only two cases of FBA were associated with paradoxical IRIS [10, 12]. The time from ART initiation to IRIS development was 7 days [12] and 6 months [10], respectively. Anti-CMV treatment without steroid treatment was beneficial in ART-naive HIV-infected patients [7, 16]. However, some individuals responded well to steroid treatment, especially in the presence of CMV-associated IRIS [12, 13].
In conclusion, FBA could be a sign of CMV-associated unmasking IRIS. In HIV-infected patients with asymptomatic CMV viremia, preemptive anti-CMV therapy was not recommended by the guideline. However, some trials assessing preemptive anti-CMV therapy in advanced HIV-infected patients documented its efficacy [17, 18]. CMV retinitis can be prevented by taking early ART and maintaining a CD4 + T cell count > 100 cells/mm3. Recognising the early manifestations of the disease and initiating proper therapy are crucial. Anti-CMV treatment with or without steroid treatment can be administered for FBA depending on the changes in CMV DNA load and immunologic profile of the AqH. In patients with no response to anti-CMV medications, systemic corticosteroids are recommended.
Availability of data and materials
Not applicable (no datasets were generated or analyzed during the current study).
Abbreviations
- AqH:
-
Aqueous humour
- ART:
-
Antiretroviral therapy
- CMV:
-
Cytomegalovirus
- EBV:
-
Epstein-Barr virus
- FBA:
-
Frosted branch angiitis
- HIV:
-
Human immunodeficiency virus
- HSV:
-
Herpes simplex virus
- Ig:
-
Immunoglobulin
- IL:
-
Interleukin
- IRIS:
-
Immune reconstitution inflammatory syndrome
- VZV:
-
Varicella-zoster virus
References
Manzardo C, Guardo AC, Letang E, Plana M, Gatell JM, Miro JM. Opportunistic infections and immune reconstitution inflammatory syndrome in HIV-1-infected adults in the combined antiretroviral therapy era: a comprehensive review. Expert Rev Anti-Infect Ther. 2015;13(6):751–67. https://doi.org/10.1586/14787210.2015.1029917.
Mihăilescu R, Arama V, Paraschiv S, Streinu-Cercel A, Oţelea D, Munteanu D, et al. Impact of highly active antiretroviral therapy on cytomegalovirus viraemia in the absence of specific anti-cytomegalovirus therapy. Rom J Intern Med. 2008;46(4):305–11.
Ruiz-Cruz M, Ávila-Rios S, Ormsby CE, Ablanedo-Terrazas Y, la Barrera C A-d, Kuri-Cervantes L, et al. Cytokine Profiles in Aqueous Humor and Plasma of HIV-infected Individuals with Ocular Syphilis or Cytomegalovirus Retinitis. Ocul Immunol Inflamm. 2018;26(1):74–81.
Wang B, Tian B, Tao Y, Hou J, Zhao X-T, Li X-X. Continued decline of aqueous interleukin-8 after multiple intravitreal injections of ganciclovir for cytomegalovirus retinitis. J Ocul Pharmacol Ther. 2014;30(7):587–92. https://doi.org/10.1089/jop.2013.0241.
Schrier RD, Song M-K, Smith IL, Karavellas MP, Bartsch D-U, Torriani FJ, et al. Intraocular viral and immune pathogenesis of immune recovery uveitis in patients with healed cytomegalovirus retinitis. Retina. 2006;26(2):165–9.
Walker S, Iguchi A, Jones NP. Frosted branch angiitis: a review. Eye (Lond). 2004;18(5):527–33. https://doi.org/10.1038/sj.eye.6700712.
Mansour AM, Li HK. Frosted retinal periphlebitis in the acquired immunodeficiency syndrome. Ophthalmologica. 1993;207(4):182–6. https://doi.org/10.1159/000310430.
Spaide RF, Vitale AT, Toth IR, Oliver JM. Frosted branch angiitis associated with cytomegalovirus retinitis. Am J Ophthalmol. 1992;113(5):522–8. https://doi.org/10.1016/S0002-9394(14)74723-3.
Anderson AM, Bergstrom CS. Syphilitic frosted branch angiitis with anterior uveitis in a patient with a new HIV diagnosis. Lancet Infect Dis. 2009;9(7):453.
Alp MN, Baykam N, Kural G. Immune recovery uveitis associated with highly active antiretroviral therapy in a patient with CMV retinitis and AIDS despite a low CD4+ T cell count: case report and a review of the literature. Int Ophthalmol. 2010;30(2):183–9. https://doi.org/10.1007/s10792-009-9303-1.
Aguilar Lozano LA, Gonzalez DA. Frosted Branch Angiitis Associated with Cytomegalovirus Retinitis. Ophthalmology. 2016;123(3):645.
Leeamornsiri S, Choopong P, Tesavibul N. Frosted branch angiitis as a result of immune recovery uveitis in a patient with cytomegalovirus retinitis. J Ophthalmic Inflamm Infect. 2013;3(1):52. https://doi.org/10.1186/1869-5760-3-52.
Fine HF, Smith JA, Murante BL, Nussenblatt RB, Robinson MR. Frosted branch angiitis in a child with HIV infection. Am J Ophthalmol. 2001;131(3):394–6. https://doi.org/10.1016/S0002-9394(00)00792-3.
Biswas J, Raizada S, Gopal L, Kumarasamy N, Solomon S. Bilateral frosted branch angiitis and cytomegalovirus retinitis in acquired immunodeficiency syndrome. Indian J Ophthalmol. 1999;47(3):195–7.
Geier SA, Nasemann J, Klauss V, Kronawitter U, Goebel FD. Frosted branch angiitis in a patient with the acquired immunodeficiency syndrome. Am J Ophthalmol. 1992;113(2):203–5. https://doi.org/10.1016/S0002-9394(14)71536-3.
Mao F, Wu J, Sun H, You Q, Li D. Frosted branch angiitis in an AIDS patient with cytomegalovirus retinitis. Int J Infect Dis. 2016;52:9–11. https://doi.org/10.1016/j.ijid.2016.09.003.
Mattioni S, Pavie J, Porcher R, Scieux C, Denis B, De Castro N, et al. Assessment of the efficacy and safety of pre-emptive anti-cytomegalovirus (CMV) therapy in HIV-infected patients with CMV viraemia. Int J STD AIDS. 2015 Apr;26(5):306–12. https://doi.org/10.1177/0956462414536146.
Bigliano P, Calcagno A, Lucchini A, Audagnotto S, Montrucchio C, Marinaro L, et al. The outcome of HIV-positive late presenters according to detectable CMV DNA and anti-CMV treatment. Antivir Ther. 2018;23(5):451–6. https://doi.org/10.3851/IMP3221.
Acknowledgements
None.
Funding
This work was supported by “double first class” university and discipline construction funds of China Medical University(3110119068 to W.Y.). The funder had no role in writing the manuscript or in the decision to publish the results.
Author information
Authors and Affiliations
Contributions
TS and WY participated in the drafting of the manuscript. ZN participated in the management of the patient. All authors revised the article critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The informed consent for being written and published was provided by the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tang, S., Zhao, N., Wang, L.Y. et al. Frosted branch angiitis due to cytomegalovirus-associated unmasking immune reconstitution inflammatory syndrome: a case report and literature review. BMC Infect Dis 21, 613 (2021). https://doi.org/10.1186/s12879-021-06311-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-021-06311-4