Abstract
Background
The northern regions of the Nordic countries have common challenges of sparsely populated areas, long distances, and an arctic climate. The aim of this study was to compare the cause and rate of fatal injuries in the northernmost area of the Nordic countries over a 5-year period.
Methods
In this retrospective cohort, we used the Cause of Death Registries to collate all deaths from 2007 to 2011 due to an external cause of death. The study area was the three northernmost counties in Norway, the four northernmost counties in Finland and Sweden, and the whole of Iceland.
Results
A total of 4308 deaths were included in the analysis. Low energy trauma comprised 24% of deaths and high energy trauma 76% of deaths. Northern Finland had the highest incidence of both high and low energy trauma deaths. Iceland had the lowest incidence of high and low energy trauma deaths. Iceland had the lowest prehospital share of deaths (74%) and the lowest incidence of injuries leading to death in a rural location. The incidence rates for high energy trauma death were 36.1/100000/year in Northern Finland, 15.6/100000/year in Iceland, 27.0/100000/year in Northern Norway, and 23.0/100000/year in Northern Sweden.
Conclusion
We found unexpected differences in the epidemiology of trauma death between the countries. The differences suggest that a comparison of the trauma care systems and preventive strategies in the four countries is required.
Similar content being viewed by others
Introduction
Annually, injuries kill 5.8 million people worldwide. Injuries are one of the top three leading causes of death for people aged 15 to 49 years, resulting in a significant impact on life years lost [1]. However, an increase in knowledge, preventive measures, efficiency and technology in emergency medicine, and implementation of trauma systems has contributed to increasing survival from serious injuries over the past few years [1, 2].
The burden of injury is not evenly distributed. Rural areas, with sparse population and long distances, have higher death rates from injuries than urban [3,4,5,6]. Urban-rural differences has been attributed to longer response and transport distances, behavioural differences and differences in socio-economic status [4].
The northern subarctic areas of the Nordic countries are, in a European context, characterised by large areas with low population density. Epidemiological findings from other rural areas are not necessarily applicable or transferable. The majority of trauma research in rural areas is from the USA, Canada, and Australia, countries with areas that have considerably longer transport distances, but also other societal differences. Differences in climate, politics, and demographics, necessitate local studies.
The northernmost areas of the Nordic countries have common challenges to trauma care, with regards to distance, rurality, and climate. Although some structural societal differences between the Nordic countries are likely as well, they are relatively homogenous, with small differences in socioeconomic status on a national level. Therefore, we believe that a head-to-head comparison of trauma epidemiology between these northern regions, may disclose areas where these Nordic neighbours can learn from one another. While the differences in overall epidemiology must be expected to be small, any differences may point to areas where the otherwise similar regions can look to the others for ways to improvement. In addition, though formalised trauma systems have been implemented in the Nordic countries, insight into the local epidemiology of trauma may help adjust these systems to local needs [7].
The aims of the present study were to describe and compare the rates of fatal injuries in the northern regions of the Nordic countries between the countries, and to describe and compare the injury mechanisms and places of death.
Materials and methods
Study design
A registry based retrospective cohort study.
Study area
The study area comprised the northernmost university hospital and its catchment area, for the Nordic countries. Thus, the study area included Iceland in its entirety, the three northernmost counties in Norway, and the four northernmost counties in both Finland and Sweden. The area covers approximately 730,000 km2 and had a population of nearly 2.4 million in 2011.
The four northernmost counties in Finland are Kainuu, Lapland, Middle Ostrobothnia, and Northern Ostrobothnia. Together these counties cover approximately 166,000 km2, 731,000 inhabitants (14% of Finland’s population), and had one trauma centre (analogue to a level II hospital according to the American College of Surgeon’s Trauma Centre Classification System, with all relevant specialties available, but not fulfilling the required volume of a level I hospital) and four local hospitals with trauma function (analogue to level III hospitals, with capability to initially manage the majority of injured patients but with transfer agreements with a higher level trauma centre) in 2011 [8]. Iceland covers approximately 103,000 km2 and 418,000 inhabitants, and had one Level II and one Level III hospital [9]. The three northernmost counties in Norway were Finnmark, Nordland and Troms, which cover approximately 177,000 km2, 470,000 inhabitants (10% of Norway’s population), and had one Level II and nine Level III hospitals in 2011 [10]. The four northernmost counties in Sweden are, Norrbotten, Västerbotten, Jämtland and Västernorrland. These counties cover approximately 225,000 km2, 877,000 inhabitants (9% of Sweden’s population), and had one Level II and 11 Level III hospitals in 2011 [11].
Inclusion and exclusion criteria
We identified from the national Cause of Death Registries and recorded all individuals who died from external causes (ICD-10 codes V01-Y98) in the northern regions of the Scandinavian Peninsula, and Iceland (Fig. 1) for the 5-year period from 2007 through 2011 [12].
We excluded all individuals with iatrogenic injuries (ICD-10 codes Y40-Y84) and all deaths occurring more than 90 days after injury. We also excluded cases in which key information was lacking, such as cases with an injury in an undetermined municipality. We excluded all accidental poisonings, except carbon monoxide poisoning where fire was the mechanism (Fig. 2). In addition, cases with too much information missing to register in the database, no hospital record found, no personal identification number found, were also excluded. These constituted 194 patients: 50 patients from Norway, 61 from Iceland, 23 from Finland, in addition to 60 patients with low energy trauma from Sweden.
Flowchart of case inclusion and exclusion. High energy trauma deaths include traumatic suicides. aOther reasons include cases with too much information missing to register in the database, no hospital record found, no personal identification number found, ICD-code(s) not matching inclusion criteria, and incompatible differences in the method of gathering LE data in Sweden (n = 60)
Data collection and analysis
We gathered data from the Cause of Death Registries (CDRs) in Finland, Iceland, and Norway, and from the Unit of Forensic Medicine in Umeå of the National Board of Forensic Medicine in Sweden. The method for data gathering in Sweden omitted many cases, particularly low energy trauma, because deaths due to ground level falls are not routinely autopsied. Because of this, Swedish data were exempt from the low energy comparison. Researchers from each country gathered their own data. We anonymised the data by assigning each case an identifier and removed personal identification numbers, kee** the key for reversal and the data separate. The anonymised data were transferred to a common database for analysis. The data could still be identified indirectly as single data points, but not when summarised as rates and proportions.
Age, sex, date of death, municipality of residence, municipality of injury, ICD-10 codes for the cause of death, and how the cause of death was determined were collected from the CDRs and Unit of Forensic Medicine [12]. The intention, mechanism, and dominating type of injury and site of death, or place of death if not on site, were obtained from the CDRs, hospital records, and autopsy reports. In Finland and Sweden, we used insurance records and police reports, respectively, to supplement the information required by the study.
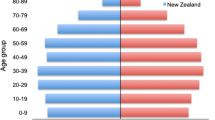
We analysed all high energy trauma deaths (including trauma suicides), and low energy trauma deaths separately. The proportions given below are the proportions of collated deaths. Incidence rates were calculated using the 2011 population size as denominator, and municipality of injury as numerator. Population size was obtained from the national statistics provider from each country (Statistics Norway, Statistics Finland, StatIce, and Statistics Sweden) [8,9,10,11]. The OECD standard population of 1980 was used for age and sex standardisation [13]. All rates are given in number of deaths/100000/year (95% confidence interval [CI]).
Definitions
We categorised the municipalities into four levels of rurality based on the municipality’s population density. Level 1 (most rural) was defined as < 18.15 inhabitants/km2, level 2 as 18.15–76.9 inhabitants/km2, level 3 as 77.0–442.7 inhabitants/km2, and level 4 (most urban) as > 442.7 inhabitants/km2 [14]. We assigned an “urban” (level 3) category to the municipalities with a university hospital, even if this municipality had a lower category based on population density, and levels 3 and 4 were grouped together as “urban” during the analysis.
We divided the manner of death into the main categories of unintentional (accidental), intentional by self (suicidal), intentional by other (homicidal), other, and unknown. We defined low energy trauma as ground level falls, whereas the remaining trauma cases were regarded as high energy trauma.
We used the American College of Surgeon’s Trauma Centre Classification System to define university hospitals with a neurosurgery department as trauma centres (Level II), and smaller hospitals equipped to deal with traumatic injuries as local hospitals with trauma function (Level III) [15]. If the hospital did not admit trauma patients according to the national trauma system, the hospital was left out of the registration.
Ethics
According to Swedish law, register studies of deceased individuals do not require ethical approval. The study was approved by ethics committees in each of the other countries: Regional Ethics Committee, Finland (98/2013); The National Bioethics Committee, Vísindasiðanefnd, Iceland (VSNb201410013/03.11); The Norwegian Ethics Board (REK) (No. 2013/1470/REK Nord); and Patient Data Security Officer at University Hospital of Northern Norway (2014/0418).
Statistical analysis
Statistical analyses were performed using SPSS (IBM SPSS Statistics for Windows, Version 25.0, Armonk, NY, USA). We present the results using medians with interquartile range (IQR), percentages with 95% CIs, and crude incidence rates of 100,000/year with 95% CIs. We used 95% CIs to determine if there were any differences between the countries and between the crude rates of subgroups.
Results
We collated a total of 5190 cases, with 4641 cases remaining after exclusion (Fig. 2). Low energy trauma deaths accounted for 1100 cases, whereas 3208 cases were high energy trauma deaths.
Low energy (LE) trauma comprised 24% of all included cases. Victims of low energy trauma were older (median age 84 years), and with a more equal sex distribution (male sex in 51% of cases) compared to victims of high energy trauma, and death mostly occurred in-hospital (in-hospital death in 88.5% of cases). Comparison of LE trauma deaths between the study areas can be found in Table 1. Iceland had a significantly lower incidence of LE trauma compared to the other areas.
High energy (HE) trauma comprised 76% of all included cases. Blunt force trauma was the most prevalent type of injury, followed by asphyxia and penetrating injuries. Most HE trauma deaths occurred in the prehospital phase in all study areas. Median age was 50 years, and males constituted 80% of HE deaths. A comparison of HE trauma deaths between the study areas can be found in Table 2. Finland had the highest incidence rate of HE trauma, followed by Norway, Sweden, and Iceland. Age and sex standardisation (Table 3) did change the absolute rates, but not their internal order among the countries.
Suicide was the most common manner of death, comprising 40% of all high energy trauma deaths, followed by accidental deaths in traffic. A comparison of mechanism of injury for high energy trauma between the study areas can be found in Table 4. The distribution was fairly similar internally in each area, with Finland significantly higher for several mechanisms. The difference between areas was greatest for suicide where Finland had an incidence rate of 15.6 per 100.000 compared to 9.3 per 100.000 in Northern Sweden, which had the second highest incidence rate for suicide.
Discussion
The aims of the present study were to describe and compare the rates of fatal injuries in the northern regions of the Nordic countries, and to describe and compare the injury mechanisms and places of death. The areas differed in the overall incidence rate of high energy trauma, with some accompanying differences in the manner and external cause of death. Northern Finland had the highest incidence, primarily driven by a high suicide rate. Deaths from high energy trauma were mostly prehospital (74–92%) in all areas; Iceland had the lowest share of prehospital high energy trauma deaths but was also the area with the lowest incidence of rural deaths. Autopsy rates were high (92–100%), except in Northern Norway (36%). The pattern of low energy trauma was more homogenous between the areas. Low energy trauma deaths occurred in older individuals, predominantly during primary admission or after being discharged, and with a more equal balance between the sexes than high energy trauma deaths.
The northern part of the Scandinavian peninsula and Iceland face similar challenges in trauma care, with sparsely populated areas, long transport distances and prehospital times in a European perspective. Differences in incidence of trauma fatalities between the northern areas, and the denser southern areas have been shown in previous studies [6, 16, 17]. The present study had injury fatality rates that exceeded those reported in studies from the southern parts of the Nordic countries [6, 18]. Despite these similar challenges for the northern areas of the Nordic countries, the present study reveals that there are marked differences between the study areas.
Iceland had a lower incidence of high energy trauma death, and a lower share of prehospital deaths. Rural areas have a higher rate of fatal injuries than urban areas, and typically a higher share of prehospital deaths [4, 19, 20]. A more urban settlement pattern in Iceland could explain Iceland’s deviant profile. Interestingly, Iceland also had a lower incidence of fatalities caused by low energy trauma, where previous studies have shown less tendency to urban-rural disparity, or even increased urban incidence rates [5, 21, 22].
There were also some differences between the other areas; Northern Finland, Northern Sweden, and Northern Norway. These areas have more similar settlement patterns, with the majority of the population living in non-urban areas, yet Northern Finland had a significantly higher incidence rate of fatal trauma, both for high energy and low energy trauma deaths [10, 11, 23]. Their incidence rates were comparatively high for most injury mechanisms overall, but particularly for suicides and homicides. The suicide rate was the main driver for the overall difference in high energy trauma death incidence between northern Finland and its neighbours.
When considering suicide, it is important to keep in mind that poisoning is a common method [24]. In trauma studies where poisonings are excluded a perceived difference in suicide rates may reflect a difference in the choice of method, and not a real difference in suicide rates. Indeed, if poisonings are considered when comparing suicide rates between the study areas of this study, only Northern Finland has a significantly different suicide rate compared to the other areas (unpublished data). Therefore, this may be a point of attack for reduction of the Finnish excessive incidence of fatal trauma, in the form of preventive strategies.
In addition to a markedly elevated suicide rate compared to the other study areas, northern Finland also had the highest incidence rate for several other mechanisms. Lower socioeconomic status and comorbidity are known risk factors for trauma related death, as well as high ethanol consumption or an unfavourable drinking pattern [4, 25, 26]. As Finland has a comparatively similar settlement pattern as its neighbours, these would be areas for further study to find explanations for the higher mortality rates. Another area to look into would be the structure and capacities of the trauma health care systems in the study areas.
Autopsy rates was another area of considerable difference. Northern Norway had a markedly lower autopsy rate compared to the other areas. Epidemiological data from a population with a higher autopsy rate are likely more reliable, and autopsies are useful in determining the correct cause of death and to assess whether deaths are preventable. In Finland and Iceland, an autopsy was performed in almost all deaths, which suggests that this also should be feasible in Norway and is an area for improvement.
Considering the northern parts of the Nordic countries as one area, the overall age and sex adjusted annual rate of injury-related deaths in the present study was 31.1/100000 (24.0 for high energy trauma deaths and 7.1 for low energy trauma deaths). This is well below the mortality rates Mack et al. has reported for the USA, more in line with, and slightly lower than their findings from Canada and Australia overall [27]. However, the incidence rate was not as high as the more rural areas of both Australia and Canada [28, 29].
Limitations
This study has several limitations. First, it is retrospective and includes only fatalities; therefore, we could not assess survivability, which would be of great interest to compare between the regions. The Swedish data were collated from the Unit of Forensic Medicine and not from the CDR. This constitutes a problem for the analysis of Swedish low energy cases, and these were exempt from comparison to the other areas. Autopsy rates for high energy trauma in Sweden have been reported to be quite high, and the inclusion through the Unit of Forensic Medicine should capture most cases [30, 31]. Even so, the Swedish high energy trauma deaths should be interpreted with care. The varying autopsy rates aggravate a comparison of injury severity scores, which could be useful in analysing differences in mortality rates. This also makes it impossible to accurately describe the mechanism of death beyond the external cause of death.
Conclusion
The northern regions of the Nordic countries have an overall rural injury pattern with relatively high rates of trauma deaths and predominantly prehospital fatalities. Northern Finland has a high injury death rate compared to its neighbours, a difference that is largely driven by a high rate of suicide. Iceland has a comparatively lower injury death rate. Given the differences in regions that would be expected to be relatively similar, further studies should investigate social differences and different approaches to health care.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CDR:
-
Cause of Death Registry
- LE:
-
Low energy
- HE:
-
High energy
- CI:
-
Confidence interval
References
World Health Organization. Injuries, Violence, The Facts: The magnitude and causes of injuries. http://www.who.int/violence_injury_prevention/media/news/2015/Injury_violence_facts_2014/en/ (2014). Accessed 11 Oct 2019.
Utter GH, Maier RV, Rivara FP, Mock CN, Jurkovich GJ, Nathens AB, et al. Inclusive trauma systems: do they improve triage or outcomes of the severely injured? J Trauma Inj Infect Crit Care. 2006;60(3):529–35. https://doi.org/10.1097/01.ta.0000204022.36214.9e.
McDermott KM, Brearley MB, Hudson SM, Ward L, Read DJ. Characteristics of trauma mortality in the Northern Territory, Australia. Inj Epidemiol. 2017;4(1):15. https://doi.org/10.1186/s40621-017-0111-1.
Peek-Asa C, Zwerling C, Stallones L. Acute traumatic injuries in rural populations. Am J Public Health. 2004;94(10):1689–93. https://doi.org/10.2105/AJPH.94.10.1689.
Raatiniemi L, Steinvik T, Liisanantti J, Ohtonen P, Martikainen M, Alahuhta S, et al. Fatal injuries in rural and urban areas in northern Finland: a 5-year retrospective study. Acta Anaesthesiol Scand. 2016;60(5):668–76. https://doi.org/10.1111/aas.12682.
Bakke HK, Schrøder Hansen I, Bakkane Bendixen A, Morild I, Lilleng PK, Wisborg T. Fatal injury as a function of rurality-a tale of two Norwegian counties. Scand J Trauma Resusc Emerg Med. 2013;21:14. https://doi.org/10.1186/1757-7241-21-14.
Kristiansen T, Søreide K, Ringdal KG, Rehn M, Krüger AJ, Reite A, et al. Trauma systems and early management of severe injuries in Scandinavia: review of the current state. Injury. 2010;41(5):444–52. https://doi.org/10.1016/j.injury.2009.05.027.
Official Statistics of Finland (OSF).http://www.stat.fi/til/ksyyt/2014/ksyyt_2014_2015-12-30_tau_001_en.html (2014) Accessed 11 Oct 2019.
Iceland Statistics. Statistics 2012. www.statice.is.(2012) Accessed 11 Oct 2019.
Statistics Norway. Folkemengde ved folketellingene i 2001 og 2011 i fylker og kommuner. https://www.ssb.no/a/kortnavn/fobhoved/tab-2012-06-21-03.html (2012) Accessed 11 Oct 2019.
SCB. Statistikdatabsen: Län och kommuner 2012. http://www.statistikdatabasen.scb.se (2012) Accessed 11 Oct 2019.
WHO ICD-10. International statistical classification of diseases and related health problems, 10th revision (ICD-10). 2016.
Federal Health Monitoring. Standard Populations. https://www.gbe-bund.de (2021). Accessed 8 June 2021.
Kristiansen T, Rehn M, Gravseth HM, Lossius HM, Kristensen P. Paediatric trauma mortality in Norway: a population-based study of injury characteristics and urban-rural differences. Injury. 2012;43(11):1865–72. https://doi.org/10.1016/j.injury.2011.08.011.
ACS Committee on Trauma. RESOURCES FOR OPTIMAL CARE OF THE INJURED PATIENT. American College of Surgeons; 2014.
Bagher A, Wangefjord S, Andersson L, Wingren CJ, Ottosson A, Acosta S. Socio-economic status and major trauma in a Scandinavian urban city: a population-based case-control study. Scand J Public Health. 2016;44(2):217–23. https://doi.org/10.1177/1403494815616302.
Finland Ministry of Social Affairs and Health. Target Programme for the Prevention of Home and Leisure. http://urn.fi/URN:ISBN:978-952-00-3473-3 (2014) Accessed 11 Oct 2019.
Søreide K, Krüger AJ, Vårdal AL, Ellingsen CL, Søreide E, Lossius HM. Epidemiology and contemporary patterns of trauma deaths: changing place, similar pace, older face. World J Surg. 2007;31(11):2092–103. https://doi.org/10.1007/s00268-007-9226-9.
Mitchell RJ, Chong S. Comparison of injury-related hospitalised morbidity and mortality in urban and rural areas in Australia. Rural Remote Health. 2010;10(1):1326.
Kristiansen T, Lossius HM, Rehn M, Kristensen P, Gravseth HM, Røislien J, et al. Epidemiology of trauma: a population-based study of geographical risk factors for injury deaths in the working-age population of Norway. Injury. 2014;45(1):23–30. https://doi.org/10.1016/j.injury.2013.07.007.
Dilsen G, Aydin R, Oral A, Sepici V, Alparsan B, Berker C, et al. Regional differences in hip fracture risk in Turkey. Bone. 1993;14(Suppl 1):S65–8. https://doi.org/10.1016/8756-3282(93)90352-b.
Chevalley T, Herrmann FR, Delmi M, Stern R, Hoffmeyer P, Rapin CH, et al. Evaluation of the age-adjusted incidence of hip fractures between urban and rural areas: the difference is not related to the prevalence of institutions for the elderly. Osteoporos Int. 2002;13(2):113–8. https://doi.org/10.1007/s001980200002.
Official Statistics of Finland (OSF). Population structure [e-publication]. http://www.stat.fi/til/vaerak/tau_en.html (2012) Accessed 11 Oct 2019.
Koskela L, Raatiniemi L, Bakke HK, Ala-Kokko T, Liisanantti J. Fatal poisonings in northern Finland: causes, incidence, and rural-urban differences. Scand J Trauma Resusc Emerg Med. 2017;25(1):90. https://doi.org/10.1186/s13049-017-0431-8.
Brattström O, Eriksson M, Larsson E, Oldner A. Socio-economic status and co-morbidity as risk factors for trauma. Eur J Epidemiol. 2015;30(2):151–7. https://doi.org/10.1007/s10654-014-9969-1.
Griswold MG, Fullman N, Hawley C, Arian N, Zimsen SRM, Tymeson HD, et al. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2018;392(10152):1015–35. https://doi.org/10.1016/S0140-6736(18)31310-2.
Mack KA, Clapperton AJ, Macpherson A, Sleet D, Newton D, Murdoch J, et al. Trends in the leading causes of injury mortality, Australia, Canada and the United States, 2000–2014. Can J Public Health. 2017;108(2):e185–91. https://doi.org/10.17269/cjph.108.5695.
Simons R, Brasher P, Taulu T, Lakha N, Molnar N, Caron N, et al. A population-based analysis of injury-related deaths and access to trauma care in rural-remote Northwest British Columbia. J Trauma Inj Infect Crit Care. 2010;69(1):11–9. https://doi.org/10.1097/TA.0b013e3181e17b39.
Fatovich DM, Jacobs IG. The relationship between remoteness and trauma deaths in Western Australia. J Trauma Inj Infect Crit Care. 2009;67(5):910–4. https://doi.org/10.1097/TA.0b013e3181815a26.
Pettersson G, Eriksson A. Onaturliga dödsfall måste utredas bättre – risk att brott missas: Granskning av polisens och sjukvårdens dödsfallshandläggning i tre län. Läkartidningen. 2014;111(48):2160–2.
Brooke HL, Talbäck M, Hörnblad J, Johansson LA, Ludvigsson JF, Druid H, et al. The Swedish cause of death register. Eur J Epidemiol. 2017;32(9):765–73. https://doi.org/10.1007/s10654-017-0316-1.
Acknowledgements
We would like to thank Rod Wolstenholme at The University of Tromsø for the artwork contribution.
Funding
The study was conducted with funding from the Finnmarkssykehuset Health Trust, The University of Tromsø, and Northern Norway Regional Health Authority.
Author information
Authors and Affiliations
Contributions
TS planned the study, collected data in Norway, and coordinated overall data collection, performed the analysis, interpreted data, and wrote the manuscript. LR contributed to planning, collected data in Finland, contributed to analysis and interpretation of data, and wrote the manuscript. BM contributed to planning, collected data in Iceland, contributed to interpretation of data and writing the manuscript. GBS collected data in Iceland, contributed to interpretation of data and writing the manuscript. TB contributed to planning, collected data in Sweden, contributed to analysis and interpretation of data, and writing the manuscript. AE contributed to planning, collected data in Sweden, contributed to interpretation of data and writing the manuscript. TD contributed to planning, contributed to and supervised analysis of data, contributed to interpretation of data, and writing the manuscript. TW conceived of the study, contributed to planning, facilitated data collection, contributed to interpretation of data, and writing the manuscript. HKB contributed to planning, supervised data collection, supervised data analysis, contributed to interpretation of data, and co-wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
According to Swedish law, register studies of deceased individuals do not require ethical approval. The study was approved by ethics committees in each of the other countries: Regional Ethics Committee, Finland (98/2013); The National Bioethics Committee, Vísindasiðanefnd, Iceland (VSNb201410013/03.11); The Norwegian Ethics Board (REK) (No. 2013/1470/REK Nord); and Patient Data Security Officer at University Hospital of Northern Norway (2014/0418). Consent to participate was not applicable.
Consent for publication
Not applicable.
Competing interests
None of the authors have any conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Steinvik, T., Raatiniemi, L., Mogensen, B. et al. Epidemiology of trauma in the subarctic regions of the Nordic countries. BMC Emerg Med 22, 7 (2022). https://doi.org/10.1186/s12873-021-00559-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-021-00559-4