Abstract
Introduction
Dukes A stages of colorectal cancer are rarely reported to metastasize. Subcutaneous or skin metastases from colon cancer are rare events and usually indicate widespread disease.
Case presentation
We present the case of a 72-year-old Caucasian woman with Dukes A colorectal cancer at diagnosis and, three years later, a single secondary subcutaneous involvement with no other metastatic sites. The description of this case is supported by critical analysis of its clinical, radiological and pathological features. Our report illustrates that diagnosis can be difficult and controversial when relapse occurs in early stage patients and at uncommon sites.
Conclusion
The unusual and aggressive course of the reported disease stresses the importance of intensive follow-up in colorectal cancer patients with good prognostic factors.
Similar content being viewed by others
Introduction
Colorectal carcinoma most often metastasizes to liver and lung, while subcutaneous or skin metastases are rare [1, 2], accounting for only 5% of such cases [3]. The most common malignancies reported to metastasize to the skin, both in men and women, are lung and breast cancers [4].
Usually, for almost all cancers, skin involvement is synonymous with extensive disease and frequently implies a poor prognosis [5, 6]. In colorectal cancer, this event occurs mostly on the incision scars, but is also seen on the skin of the extremities, head and neck, and penis [7–9]. Some authors, such as Kaufmann et al., have suggested two hypotheses for this metastatic involvement: the first one implies a lymphatic and hematogenous spread of disease, while the second one speculates on an implantation during surgery [10].
Ulceration, nodules, bullae or fibrotic processes are the most common signs of cutaneous metastases.
In stage Dukes A, colorectal cancer involves only the innermost lining of the colon or rectum, with minimal invasiveness in the muscular layer.
In patients with this stage of cancer, relapse is very rare [11]. Here we describe the case of a 72-year-old woman with Dukes A colorectal cancer at diagnosis, and three years later, a single secondary involvement of the subcutaneous tissue of the left paravertebral dorsal region.
Case presentation
A 72-year-old Caucasian woman underwent a right hemicolectomy for a Dukes A colon cancer in August 2008 (staging: pT2, pN0-0/27nodes, G2). Computed tomography (CT) of her abdomen, pelvis, and chest did not show any distant metastases, so she was not treated further. Follow-up examinations were negative until August 2009 when mammography showed a suspicious lesion of the left breast. In September 2009 a left superior and external quadrantectomy was performed. Histological examination revealed breast intraductal carcinoma (staging: pTis, p N0). For this new pathology, the patient was only treated with radiotherapy. She continued her follow-up examinations for colorectal cancer. She remained asymptomatic until May 2011, with no clinical or radiological signs of recurrence. In June 2011, she presented with a painless swelling, affecting the skin of the left paravertebral dorsal region. Serum tumor markers were not increased and colonoscopy did not show any local disease relapse. A chest X-ray excluded pulmonary metastasis and an abdominal ultrasound did not detect either liver metastases or peritoneal dissemination. Therefore, an ultrasound scan of the dorsal tumefaction was performed, showing a suspected heterogeneous, solid and vascularized lesion. She underwent a radical en-bloc resection of the dorsal swelling. Histological analysis of the excised specimen revealed a metastatic poorly differentiated adenocarcinoma, most likely originating from the large bowel, which infiltrated the skin and the subcutaneous tissue.
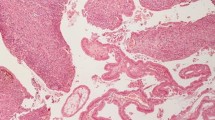
Macroscopically, the surgical specimen consisted of a radical en-bloc resection of subcutaneous tissue (soft-tissue) of 4x2.5x2cm which contained a nodular lesion of 3.2cm diameter. The cut surface was white to yellowish white and showed areas of necrosis and hemorrhage. The excised specimen was fixed in 10% buffered formalin and embedded in paraffin. Sections of 4μm were prepared and routinely stained with hematoxylin and eosin. Further sections were examined immunohistochemically using a streptavidin-biotin complex technique (DAKO). Prediluted antibodies against the following antigens were used: keratin 20 protein (monoclonal, 1:50; Zymed®), keratin 7 (monoclonal, 1:50; Zymed®), Thyroid transcription factor 1 (TTF-1) (monoclonal, 1:100; Zymed®), anti-estrogen receptor (monoclonal, 1:50; DAKO), and anti-progesterone receptor (monoclonal, 1:50; DAKO).
Microscopically, the tumor was characterized by nests and islands of epithelial cells with only scattered abortive glands. The cells had atypical nuclei, with evidence of nucleoli, abundant eosinophilic cytoplasm without sharply defined outlines. The inflammatory infiltrate was marked and there were hemorrhagic foci and areas of necrosis. The mitosis was either frequently or sometimes infrequently atypical (sFigure 1). The cells were focally positive for keratin 20 (Figure 2). Keratin 7, TTF1, estrogen and progesterone receptors were negative. The morphologic aspects and the immunohistochemical results were considered specific for a colonic origin. In this setting, the neoplasia was also evaluated for K-ras mutation and the molecular analysis showed the absence of mutation on codon 12 and 13 (wild type). The total body CT revealed no evidence of visceral distant metastases but showed suspicious abdominal colliquative lymphadenopathy. The patient is being treated with FOLFIRI ( leucovorin (folinic acid), fluorouracil, irinotecan hydrochloride) + bevacizumab and she remains asymptomatic.
Discussion
Colorectal cancer is one of the most frequent oncological diseases. This clinical history shows a rare pattern of colon cancer metastasis. In patients with Dukes A, colon carcinoma relapse is rare [11]. Cutaneous or subcutaneous metastases are uncommon in colorectal cancer [1, 2], as well as in carcinomas that have originated elsewhere [5, 6, 12, 13].
The identification of this type of metastasis in many types of cancer is indicative of a poor prognosis with the presence of disseminated disease [5, 6]. The study by Schoenlaub et al. reviewed 200 cases of cancers with cutaneous or subcutaneous metastasis and reported that among these, patients with colorectal cancer had a median survival of 4.4 months [5]. On the other hand, a retrospective study by Lookingbill et al. showed a median survival of 18 months in patients with the same characteristics [6].
A finding of isolated subcutaneous metastases of colorectal cancer without other metastatic sites is extremely rare and may delay the diagnosis by several months [14].
In our case, the rarity of this event caused many difficulties in the correct diagnosis and in the right therapeutic approach.
From a biological perspective, this case outlines the plural-phenotypic nature of cancer: the course of disease that we report here is clearly determined by a peculiar cancer cell population with specific biology and homing features.
Conclusion
Despite the Dukes A staging, G2 grading and the absence of an increase in serum tumor markers, the characteristics of this cancer phenotype appear to be rather aggressive. Studies in molecular biology are strongly warranted to distinguish patients with a peculiar clinical course and prognosis. Intensive follow-up is also indicated in patients with good prognostic factors at diagnosis.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
Llaguna OH, Desai P, Fender AB, Zedek DC, Meyers MO, O’Neil BH, Diaz LA, Calvo BF: Subcutaneous metastatic adenocarcinoma: an unusual presentation of colon cancer- case report and literature review. Case Rep Oncol. 2010, 3: 386-390. 10.1159/000321948.
Gupta SS, Singh O: Carcinoma colon presenting as cutaneous metastasis to an old operative scar of hysterectomy. J Canc Res Ther. 2010, 6: 316-317. 10.4103/0973-1482.73334.
Horiuchi A, Nozawa K, Akahane T, Shimada R, Shibuya H, Aoyagi Y, Nakamura K, Hayama T, Yamada H, Ishihara S, Matsuda K, Watanabe T: Skin metastasis from sigmoid colon cancer. Int Surg. 2011, 96: 135-138.
Kaplan RP: Specific cutaneous manifestations of internal malignancy. Adv Dermatol. 1986, 1: 3-42.
Schoenlaub P, Sarraux A, Grosshans E, Heide E, Cribier B: Survival after cutaneous metastasis: a study of 200 cases (in French). Ann Dermatol Venereol. 2001, 128: 1310-1315.
Lookingbill DP, Spangler N, Helm KF: Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patients. J Am Acad Dermatol. 1993, 29: 228-236. 10.1016/0190-9622(93)70173-Q.
Stavrianos SD, McLean NR, Kelly CG, Fellows S: Cutaneous metastasis to the head and neck from colonic carcinoma. Eur J Surg Oncol. 2000, 26: 518-519. 10.1053/ejso.1999.0935.
Camci C, Türk HM, Büyükberber S, Karakök M, Koruk M, Beyazity Y, Inalöz HS: Colon carcinoma with synchronous subcutaneous and osseous metastasis: a case report. J Dermatol. 2002, 29: 362-365.
Banerjee GK, Lim KP, Cohen NP: Penile metastasis: an unusual presentation of metastatic colonic cancer. J R Coll Surg Edinb. 2002, 47: 763-764.
Kauffman LC, Sina B: Metastatic inflammatory carcinoma of the rectum: tumour spread by three routes. Am J Dermatopathol. 1997, 19: 528-532. 10.1097/00000372-199710000-00107.
Andreoni B, Chiappa A, Bertani E, Bellomi M, Orecchia R, Zampino M, Fazio N, Venturino M, Orsi F, Sonzogni A, Pace U, Monfardini L: Surgical outcomes for colon and rectal cancer over a decade: results from a consecutive monocentric experience in 902 unselected patients. World J Surg Oncol. 2007, 5: 73-10.1186/1477-7819-5-73.
Krathen RA, Orengo IF, Rosen T: Cutaneous metastasis: a meta-analysis of data. South Med J. 2003, 96: 164-167. 10.1097/01.SMJ.0000053676.73249.E5.
Hu SC, Chen GS, Wu CS, Chai CY, Chen WT, Lan CC: Rates of cutaneous metastases from different internal malignancies: experience from a Taiwanese medical center. J Am Acad Dermatol. 2009, 60: 379-387. 10.1016/j.jaad.2008.10.007.
Gmitter TL, Dhawan SS, Phillips MG, Wiszniak J: Cutaneous metastases of colonic adenocarcinoma. Cutis. 1990, 46: 66-68.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
GPS, FA, GLR, EM and ST designed the study, interpreted the study results and drafted the manuscript. FB contributed to the pathologic analysis. LC, VS, NP, SS and MS contributed to the work. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lo Russo, G., Accarpio, F., Spinelli, G.P. et al. Subcutaneous metastases from colon cancer: a case report. J Med Case Reports 6, 212 (2012). https://doi.org/10.1186/1752-1947-6-212
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1752-1947-6-212