Abstract
Background
Microalbuminuria and subsequent progression to proteinuria and nephropathy is associated with increased oxidative stress, increased inflammatory cytokines and increased cardiovascular (CVD) risk. The common functional IL-6 -174G>C gene variant is also associated with elevated levels of inflammatory cytokines and CVD risk.
Methods
The aim of this study was to examine the association between the IL-6 -174G>C gene variant with plasma total antioxidant status (TAOS) in 552 subjects with type 2 diabetes in relation to urinary protein excretion.
Results
In subjects free from CVD, there was a significant interaction between urinary protein excretion (normoalbuminuria/ microalbuminuria/proteinuria) and the -174C allele (compared to -174GG) in determining plasma TAOS (p value for interaction = 0.03). In the -174C allele carriers there was a significant association between plasma TAOS and urinary protein excretion: normalbuminuria v microalbuminuria v proteinuria: 44.30% ± 11.32 vs. 39.74% ± 14.83 vs. 37.93% ± 16.42, ANOVA p = 0.025. In those with CVD, no interaction or association was observed with the -174C allele (p = 0.246).
Conclusion
The IL-6 -174G>C gene variant is associated with differences in plasma oxidative stress in response to altered protein excretion in subjects with type 2 diabetes.
Similar content being viewed by others
Background
Interleukin-6 (IL-6) is a multifunctional inflammatory cytokine expressed in many tissues [1, 2]. The IL-6 -174G>C functional gene variant has previously been studied in relation to the risk of coronary heart disease (CHD) [3], juvenile onset chronic arthritis [4] and primary Sjogren's syndrome [5]. The promoter region of this gene contains many functional sites including a multiple response element (-173 to -145), which is responsive to interleukin-1, tumour necrosis factor-α, nuclear factor-κB (NFκ-B) and glucocorticoids [6]. In addition there is a variable run of A and T bases (-257 to -276) which may affect promoter strength [4, 6]. Increased IL-6 is associated with numerous adverse effects on the cardiovascular system, including increased synthesis of reactive oxygen species (ROS) via NADPH oxidase [7], and hence increased oxidative stress. Previous studies have shown the -174C allele to be associated with prospective CHD risk and hypertension [3], and in an environment of increased stress is associated with elevated plasma IL-6 levels [8, 9].
Microalbuminuria is a marker of vascular dysfunction in subjects with type 2 diabetes mellitus (Type 2 DM), however whether it plays a causal role in cardiovascular disease (CVD) remains to be clarified [10–12]. Microalbuminuria and subsequent progression to proteinuria and nephropathy is associated with increased oxidative stress [13], inflammatory cytokines [14] and increased CVD risk [12]. Previous studies have also shown that functional gene variants in the IL-6 gene may influence progression from microalbuminuria to overt proteinuria and subsequent renal failure [15], where CVD is the major cause of mortality [16]. In vitro studies have shown that IL-6 stimulates mesangial cell proliferation and matrix production, two of the core features of diabetic glomerulosclerosis [17, 18]. Moreover, urinary levels of IL-6 are elevated in patients with diabetic nephropathy [19].
Therefore IL-6, urinary protein excretion and oxidative stress appear to be closely associated in their common outcome of CVD and within this cluster of phenotypes there may be important genotypic-phenotypic (gene-environment) interactions. From the above studies we would hypothesis that the -174C allele would be associated with higher oxidative stress and to modulate urine protein excretion. The aim of this study was to examine the association and potential interaction between the IL-6 -174G>C functional gene variant and urinary protein excretion, with oxidative stress in subjects with Type 2 DM. Since oxidative stress is increased in the presence of atherosclerosis [7], we reasoned that it would also be essential to study the association after grou** the subjects by CVD status.
Methods
Subject population
Patients were recruited from the University College Diabetes and Cardiovascular Study (UDACS). This comprises of 1020 consecutive subjects recruited from the diabetes clinic at University College London Hospitals NHS Trust (UCLH) between the years 2001–2. All patients had diabetes according to WHO criteria [20]. No subjects requiring renal dialysis were recruited. Analyses was confined to Caucasian subjects with Type 2 DM (605, of whom 569 were successfully genotyped for the IL-6 -174G>C gene variant and 552 had plasma total antioxidant status (TAOS) and urine protein excretion measured). Analysis was therefore confined to 552 subjects. Ethical approval was obtained from UCL/UCLH ethics committee.
Identification and classification of endpoints
Microalbuminuria was defined as an albumin:creatinine ratio (ACR) of greater than 2.5 mg/mmol in men and 3.5 mg/mmol in women. Proteinuria was defined as an ACR > 30 mg/mmol.
Subjects were categorised by the presence/absence of clinically manifest CVD. CVD was recorded if a patient had one or more of CHD, peripheral vascular disease (PVD) or cerebrovascular disease (CbVD). The presence of CHD was recorded if any patient had positive coronary angiography or angioplasty, coronary artery bypass, a positive cardiac thallium scan or exercise tolerance test, documented evidence of myocardial infarction or symptomatic/treated angina. The presence of PVD was recorded in any patient with absent peripheral pulses and abnormal lower limb doppler pressures or an abnormal lower limb angiogram, previous angioplasty or limb by-pass graft. CbVD was recorded if a patient had been investigated for symptoms or signs consistent with a cerebrovascular accident and had a brain CT showing any evidence of infarction (diffuse/localised) or haemorrhage. Those with either CHD or PVD or CbVD were designated as having CVD. Subjects who were asymptomatic for CHD/CbVD/PVD or had negative investigations were categorised as having no CVD.
Measurement of plasma TAOS
Plasma TAOS was measured by a photometric microassay previously described by Sampson et al [21]. The TAOS of plasma was determined by its capacity to inhibit the peroxidase-mediated formation of the 2,2-azino-bis-3-ethylbensthiazoline-6-sulfonic acid (ABTS+) radical. In the assay, the relative inhibition of ABTS+ formation in the presence of plasma is proportional to the antioxidant capacity of the sample. Therefore, there are two arms to the assay, a control arm and test arm. In the control arm phosphate buffered saline (PBS) is used instead of plasma. The assay is performed in a 96 well ELISA plate using 2.5 μl of plasma. The difference in absorbance (control absorbance minus test absorbance) divided by the control absorbance (expressed as a percentage) was used to represent the percentage inhibition of the reaction. Plasma TAOS is therefore inversely related to oxidative stress (the higher the oxidative stress, the lower the TAOS). The inter assay coefficient of variation (CV) was 14.1%, and the intra assay CV was 4.3%.
IL-6 -174G>C genoty**
Genomic leukocyte DNA was extracted by salting out from 5 ml EDTA blood samples. Genotypes were determined using polymerase chain reaction amplification (PCR) with published primers and conditions [3, 22]. Digest products were resolved by micro-titre array diagonal gel electrophoresis (MADGE) [23] and confirmed by two independent technicians blind to subject outcome, with discrepancies resolved by repeat genoty**.
Statistical analysis
Analysis was performed using SPSS (version 10.1, SPSS Inc., Chicago). Data are reported for those individuals amongst whom high-throughput genoty**, plasma TAOS and urine protein excretion measurement was successful. Results are presented as mean ± standard deviation or median (interquartile range). Deviations from Hardy-Weinberg equilibrium were considered using chi-squared tests. Deviations from Hardy-Weinberg equilibrium were considered using chi-squared tests. Hardy-Weinberg equilibrium gives the expected genotype distribution based on the observed frequency of the rare allele (q) and common allele (p) as p2+2pq+q2, where p2 is the predicted frequency for homozygosity of the common allele, q2 is the predicted frequency for homozygosity of the rare allele and 2pq, the heterozygotes. These frequencies are expected provided the sample is drawn from a population with random mating and no strong selection. Deviations from the expected frequencies may suggest selection bias.
Allele frequencies are shown with the 95% confidence interval. To assess the differences between CVD and no CVD patients, two-sided T-tests were performed on normally distributed data or after appropriate transformation (log or square root). Analysis of variance (ANOVA) was used to assess the association between genotypes /urinary protein excretion and plasma TAOS, followed by a comparison made after combining the GC and CC groups as the C allele has previously been shown to have a dominant effect on CVD risk [3, 9, 24] and plasma IL-6 [8]. This provided an ANOVA p-value between groups and a p-value for the linear relationship between groups. The relationships between baseline parameters and plasma TAOS were tested by Spearman rank correlation co-efficient. An ANOVA was also performed to test the association between genotype and TAOS after adjustment for the potential confounders using multiple regression analysis to obtain a residual. For the analysis of the combined effect of genotype and urinary protein excretion on plasma TAOS, subjects were grouped by genotype (GG and GC/CC). ANOVA was then performed separately within each genotype group with urinary protein excretion (normoalbuminuria/ microalbuminuria/proteinuria) as the independent and plasma TAOS as the dependent variable. The interaction between genotype and urinary protein excretion in determining plasma TAOS was performed using linear regression were the combined effects were compared to the individual effects of these variables. In all cases a P value of less than 0.05 was considered statistically significant.
Results
The baseline characteristics of the subjects grouped by CVD status are summarized in table 1. Of the 552 subjects, 188 had CVD (141 CHD, 45 PVD and 37 CbVD) and 364 no CVD. The genotype distribution was in Hardy-Weinberg equilibrium (χ2 = 0.019, p = 0.998) with a G allele frequency of 0.652 [0.62–0.68] and C allele frequency of 0.348 [0.32–0.38]. In the whole group, no significant association was seen between genotype and plasma TAOS (GG: 42.26% [13.20] v GC: 41.91% [13.15] v CC: 43.39% [13.70], ANOVA p = 0.720), and urinary protein excretion (normoalbuminuria/microalbuminuria/proteinuria p = 0.558) and CVD status, p = 0.985.
Plasma TAOS was independent of pharmacotherapy, but correlated positively with plasma HDL-cholesterol, and negatively with triglyceride, glucose and HbA1c (correlation co-efficient r = 0.12, -0.15, -0.11 and -0.10 respectively; all P < 0.05). After adjustment for these variables, the above results remained unchanged (for genotype and plasma TAOS, p = 0.704). No association was observed between genotype and baseline lipid measures, blood pressure, C-reactive protein and modes of therapy (antihypertensive, oral hypoglycaemic, statin and aspirin).
Subjects without CVD
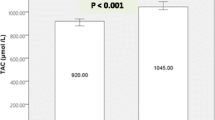
In subjects without CVD, no association was seen between genotype and plasma TAOS (GG: 43.23% [12.40] v GC 41.79% [13.30] v CC 42.59% [14.14], ANOVA p = 0.614, after adjustment p = 0.645) or between urinary protein excretion and TAOS (normoalbuminuria 43.55% [11.92] v microalbuminuria 41.54% [14.03] v proteinuria 40.00% [14.82], ANOVA p = 0.194, after adjustment p = 0.284). However in those with the -174C allele, as shown in figure 1, there was a significant association between higher urinary protein excretion and lower plasma TAOS (ANOVA p = 0.025, linearity between groups, p = 0.008). This remained significant after adjustment for age, triglyceride, HDL-C, glucose and HbA1c (ANOVA p = 0.031). No such differences were observed in those subjects homozygous for the -174G allele. The interaction between urinary protein excretion and genotype on plasma TAOS was statistically significant, p = 0.032 (after adjustment p = 0.029).
Plasma TAOS by genotype and urinary protein excretion in subjects free from CVD. Footnote: Mean (± standard error) shown. Numbers of subjects are shown at the base of each column. In those without CVD, the interaction between genotype (GG v GC/CC) and urinary protein excretion in determining plasma TAOS was significant (p = 0.032). *In the GC/CC subjects, there was a significant difference in plasma TAOS by urinary protein excretion (normoalbuminuria/ microalbuminuria/proteinuria), ANOVA between groups p = 0.025 (as expected the linear association in TAOS between these groups was significant p = 0.008 with normoalbuminuric subjects having the highest TAOS and those with proteinuria the lowest). In GG Subjects no such difference was observed, (ANOVA between groups, p = 0.399)
When subjects with normoalbuminuria were compared to those with microalbuminuria and/or proteinuria, the -174C allele was still associated with variation in plasma TAOS (p interaction = 0.02, after adjustment p = 0.016). When subjects with frank proteinuria were excluded from the analysis, those subjects with the -174C allele and microalbuminuria still had the lowest plasma TAOS (p value for interaction = 0.01, after adjustment p = 0.023).
Subjects with CVD
In subjects with CVD, no association was seen between genotype and plasma TAOS (GG: 40.39% [14.50] v GC 42.37% [12.84] v CC 44.91% [12.98], ANOVA p = 0.332, after adjustment p = 0.319) or between urinary protein excretion and TAOS (normoalbuminuria 42.73% [12.84] v microalbuminuria 41.84% [13.53] v proteinuria 39.36% [15.87], ANOVA p = 0.510, after adjustment p = 0.615). In contrast to those without CVD, no interaction was seen between genotype and urinary protein excretion or plasma TAOS by genotype (p = 0.246, after adjustment p = 0.303).
Conclusion
Although there was no overall significant influence of the IL-6 -174G>C variant on plasma TAOS or on urinary protein excretion, this study provides evidence of an impact of this common variant in the IL-6 gene, on the relationships between an intermediate phenotype (urinary protein excretion) and oxidative stress. Carriage of the -174C allele increased the likelihood of a nephropathy-associated increase in oxidative stress in subjects with Type 2 DM. This effect was confined to subjects free from clinically manifest CVD and no such interaction was observed in those subjects with CVD. This may be explained by the fact that in the presence of established CVD, ROS formation is increased as a result of the atherosclerotic process [7] and this overwhelms the modest effect of genotype. Plasma TAOS was not however significantly different between subjects with and without CVD in our study, possibly due to the fact that those with CVD are being treated with agents such as statins and aspirin, which may be overwhelming the genotype effect.
The -174C allele has been associated with increased plasma IL-6 under conditions of stress and with CHD risk [3, 8, 9]. High levels of plasma IL-6 have also been shown to be an independent predictor of mortality in patients with renal impairment, prior to starting dialysis treatment [25]. We did not observe a decrease in plasma TAOS associated with the -174C allele, but rather an interaction with urinary protein excretion.
Glomerular basement thickening, increased accumulation of extracellular matrix and expanded mesangium are common features of diabetic nephropathy [17, 18]. Previous in vitro studies have shown that IL-6 may stimulate mesangial cell proliferation. High levels of urinary IL-6 have also been noted in patients with diabetic nephropathy [19]. As described, increased oxidative stress and CVD risk is associated with nephropathy, renal failure [12] and elevated plasma IL-6. Therefore in a patient with the -174C allele and early/established nephropathy, the additive effects may be to increase plasma IL-6 and subsequent ROS generation. Interestingly, ROS may also promote IL-6 gene expression by activating the NFκ-B binding site, 100 base pairs downstream from the -174G>C variant [26].
This study provides an example of a genotypic-phenotypic (gene-environment) interaction. 'Genotype-phenotype interaction' implies that in combination, the risk associated with a particular gene variant in a particular environment is more than the effects of each independently. From a mechanistic viewpoint, interaction suggests that at the molecular level, the effect or by product of the phenotypic insult modifies the molecular function of the gene product under observation or vice-versa. In this study we provide evidence that a common gene variant in the IL-6 -174 gene increases the likelihood of a nephropathy-associated increase in oxidative stress in subjects with Type 2 DM. The study of common 'genotype-phenotype' or 'gene-environment interactions' not only provides a useful means to improve our understanding of disease at the molecular level but also allows specific targeting of advice and therapies to high risk individuals (those with high-risk genotype in a high-risk environment). From the results described, this might involve targeting microalbuminuria and proteinuria more aggressively in those patients who carry the -174C allele, for example with anti-inflammatory agents.
Abbreviations
CVD = Cardiovascular disease
CHD = Coronary heart disease
PVD = Peripheral vascular disease
CbVD = Cerebrovascular disease
TAOS = Total antioxidant status
IL-6 = Interleukin-6
Type 2 DM = Type 2 diabetes
ANOVA = Analysis of variance
UDACS = University College London diabetes and cardiovascular disease study
UCL = University College London
WHO = World Health Organisation
CV = Co-efficient of variation
MADGE = Microtitre array diagonal gel electrophoresis
ROS = Reactive oxygen species
CRP = C-reactive protein
ACEI = Angiotensin converting-1 enzyme inhibitor
HbA1c = Glycated haemoglobin
References
Hirano T, Akira S, Taga T, Kishimoto T: Biological and clinical aspects of interleukin 6. Immunol Today. 1990, 11: 443-449. 10.1016/0167-5699(90)90173-7.
Horii Y, Iwano M, Hirata E, Shiiki M, Fujii Y, Dohi K, Ishikawa H: Role of interleukin-6 in the progression of mesangial proliferative glomerulonephritis. Kidney Int Suppl. 1993, 39: S71-5.
Humphries SE, Luong LA, Ogg MS, Hawe E, Miller GJ: The interleukin-6 -174 G/C promoter polymorphism is associated with risk of coronary heart disease and systolic blood pressure in healthy men. Eur Heart J. 2001, 22: 2243-2252. 10.1053/euhj.2001.2678.
Fishman D, Faulds G, Jeffery R, Mohamed-Ali V, Yudkin JS, Humphries S, Woo P: The effect of novel polymorphisms in the interleukin-6 (IL-6) gene on IL-6 transcription and plasma IL-6 levels, and an association with systemic-onset juvenile chronic arthritis. J Clin Invest. 1998, 102: 1369-1376.
Hulkkonen J, Pertovaara M, Antonen J, Pasternack A, Hurme M: Elevated interleukin-6 plasma levels are regulated by the promoter region polymorphism of the IL6 gene in primary Sjogren's syndrome and correlate with the clinical manifestations of the disease. Rheumatology (Oxford). 2001, 40: 656-661. 10.1093/rheumatology/40.6.656.
Terry CF, Loukaci V, Green FR: Cooperative influence of genetic polymorphisms on interleukin 6 transcriptional regulation. J Biol Chem. 2000, 275: 18138-18144. 10.1074/jbc.M000379200.
Harrison D, Griendling KK, Landmesser U, Hornig B, Drexler H: Role of oxidative stress in atherosclerosis. Am J Cardiol. 2003, 91: 7A-11A. 10.1016/S0002-9149(02)03144-2.
Brull DJ, Montgomery HE, Sanders J, Dhamrait S, Luong L, Rumley A, Lowe GD, Humphries SE: Interleukin-6 gene -174g>c and -572g>c promoter polymorphisms are strong predictors of plasma interleukin-6 levels after coronary artery bypass surgery. Arterioscler Thromb Vasc Biol. 2001, 21: 1458-1463.
Jones KG, Brull DJ, Brown LC, Sian M, Greenhalgh RM, Humphries SE, Powell JT: Interleukin-6 (IL-6) and the prognosis of abdominal aortic aneurysms. Circulation. 2001, 103: 2260-2265.
Jarrett RJ, Viberti GC, Argyropoulos A, Hill RD, Mahmud U, Murrells TJ: Microalbuminuria predicts mortality in non-insulin-dependent diabetics. Diabet Med. 1984, 1: 17-19.
Mogensen CE: Microalbuminuria predicts clinical proteinuria and early mortality in maturity-onset diabetes. N Engl J Med. 1984, 310: 356-360.
Mattock MB, Barnes DJ, Viberti G, Keen H, Burt D, Hughes JM, Fitzgerald AP, Sandhu B, Jackson PG: Microalbuminuria and coronary heart disease in NIDDM: an incidence study. Diabetes. 1998, 47: 1786-1792.
Mehrotra S, Ling KL, Bekele Y, Gerbino E, Earle KA: Lipid hydroperoxide and markers of renal disease susceptibility in African-Caribbean and Caucasian patients with Type 2 diabetes mellitus. Diabet Med. 2001, 18: 109-115. 10.1046/j.1464-5491.2001.00416.x.
Stehouwer CD, Gall MA, Twisk JW, Knudsen E, Emeis JJ, Parving HH: Increased urinary albumin excretion, endothelial dysfunction, and chronic low-grade inflammation in type 2 diabetes: progressive, interrelated, and independently associated with risk of death. Diabetes. 2002, 51: 1157-1165.
Kitamura A, Hasegawa G, Obayashi H, Kamiuchi K, Ishii M, Yano M, Tanaka T, Yamaguchi M, Shigeta H, Ogata M, Nakamura N, Yoshikawa T: Interleukin-6 polymorphism (-634C/G) in the promotor region and the progression of diabetic nephropathy in type 2 diabetes. Diabet Med. 2002, 19: 1000-1005. 10.1046/j.1464-5491.2002.00844.x.
Clermont G, Lecour S, Lahet J, Siohan P, Vergely C, Chevet D, Rifle G, Rochette L: Alteration in plasma antioxidant capacities in chronic renal failure and hemodialysis patients: a possible explanation for the increased cardiovascular risk in these patients. Cardiovasc Res. 2000, 47: 618-623. 10.1016/S0008-6363(00)00117-6.
Coleman DL, Ruef C: Interleukin-6: an autocrine regulator of mesangial cell growth. Kidney Int. 1992, 41: 604-606.
Ruef C, Budde K, Lacy J, Northemann W, Baumann M, Sterzel RB, Coleman DL: Interleukin 6 is an autocrine growth factor for mesangial cells. Kidney Int. 1990, 38: 249-257.
Shikano M, Sobajima H, Yoshikawa H, Toba T, Kushimoto H, Katsumata H, Tomita M, Kawashima S: Usefulness of a highly sensitive urinary and serum IL-6 assay in patients with diabetic nephropathy. Nephron. 2000, 85: 81-85. 10.1159/000045634.
Alberti KG, Zimmet PZ: New diagnostic criteria and classification of diabetes--again?. Diabet Med. 1998, 15: 535-536. 10.1002/(SICI)1096-9136(199807)15:7<535::AID-DIA670>3.3.CO;2-H.
Sampson MJ, Gopaul N, Davies IR, Hughes DA, Carrier MJ: Plasma F2 isoprostanes: direct evidence of increased free radical damage during acute hyperglycemia in type 2 diabetes. Diabetes Care. 2002, 25: 537-541.
Stephens JW: A long-range PCR method for genoty** promoter variants in the interleukin-6 gene. Thromb Haemost. 2003, 89: 765-767.
Day IN, Humphries SE: Electrophoresis for genoty**: microtiter array diagonal gel electrophoresis on horizontal polyacrylamide gels, hydrolink, or agarose. Anal Biochem. 1994, 222: 389-395. 10.1006/abio.1994.1507.
Jenny NS, Tracy RP, Ogg MS, Luong le A, Kuller LH, Arnold AM, Sharrett AR, Humphries SE: In the elderly, interleukin-6 plasma levels and the -174G>C polymorphism are associated with the development of cardiovascular disease. Arterioscler Thromb Vasc Biol. 2002, 22: 2066-2071. 10.1161/01.ATV.0000040224.49362.60.
Pecoits-Filho R, Barany P, Lindholm B, Heimburger O, Stenvinkel P: Interleukin-6 is an independent predictor of mortality in patients starting dialysis treatment. Nephrol Dial Transplant. 2002, 17: 1684-1688. 10.1093/ndt/17.9.1684.
Zhang J, Johnston G, Stebler B, Keller ET: Hydrogen peroxide activates NFkappaB and the interleukin-6 promoter through NFkappaB-inducing kinase. Antioxid Redox Signal. 2001, 3: 493-504. 10.1089/15230860152409121.
Acknowledgements
JWS is supported by a clinical training fellowship from Diabetes UK (BDA: RD01/0001357). SEH is supported by grants from the British Heart Foundation (RG2000015). We should also like to thank the medical staff and patients who contributed to the UDAC studies.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
JWS, SJH and SEH are the lead investigators of the UDAC study. Subject recruitment was performed by JWS and SJH. JA is the curator of the study DNA. DNA extraction and preparation was performed by JWS and JA. Genoty** and plasma TAOS measurements were performed by JWS. Data analysis was performed by JWS, SJH and SEH.
All authors have read and approved the manuscript for publication
Competing interests
None declared.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Stephens, J.W., Hurel, S.J., Acharya, J. et al. An interaction between the interleukin-6 -174G>C gene variant and urinary protein excretion influences plasma oxidative stress in subjects with type 2 diabetes. Cardiovasc Diabetol 3, 2 (2004). https://doi.org/10.1186/1475-2840-3-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2840-3-2