Abstract
COVID-19 is characterized by a severe course in approximately 5‒10% of patients, who require admittance to the intensive care unit and mechanical ventilation, which is associated with a very high risk of a poor prognosis. At present, in real clinical practice, in managing severe patients with COVID-19, noninvasive ventilation (NIV) is widely used (in some countries, up to 60% of all methods of respiratory support). In most studies on the effectiveness of NIV in hypoxemic acute respiratory failure in patients with COVID-19, the need for tracheal intubation and hospital mortality with the use of NIV averaged 20–30%, which suggests the rather high efficiency of this method. The COVID-19 pandemic has given a powerful impetus to the widespread use of prone positioning among nonintubated patients with acute respiratory failure caused by COVID-19. Several studies have shown that prone positioning can reduce the need for mechanical ventilation and hospital mortality. Medications that have proven effective in severe forms of COVID-19 include remdesivir, systemic glucocorticoids, tocilizumab, baricitinib, and anticoagulants. Among the new promising areas of drug therapy, noteworthy is the use of thiol-containing drugs (N-acetylcysteine), inhaled surfactant, and inhaled prostacyclin analogues.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
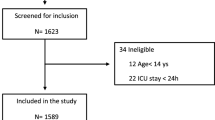
Multicenter studies have shown that 5 to 32% of patients hospitalized for COVID-19 require admittance to an intensive care unit (ICU), mostly for hypoxemic acute respiratory failure (ARF). Indeed, acute respiratory distress syndrome (ARDS) is diagnosed in 40–96% of patients in critical care resuscitation units and intensive care units, and 30–88% of them require invasive mechanical ventilation [1]. Most severe and critically ill patients in intensive care units are elderly people with obesity, hypertension, cardiovascular disease, and diabetes. The registered mortality in these units ranges from 16 to 78%, and in patients receiving mechanical ventilation, it is consistently higher, up to 88%. Several large multicenter studies in a large cohort of patients have demonstrated that older age, male gender, obesity, a history of diabetes mellitus, chronic lung disease, along with the need for mechanical ventilation, are independent predictors of mortality in intensive care units.
As was shown in the LUNG-SAFE study, in acute respiratory distress syndrome associated with COVID-19, the duration of mechanical ventilation is significantly longer than in the absence of this background: 26 (13–43) days and 14 (7–23) days, respectively.
This review is dedicated to the methods of respiratory support and drug therapy that have demonstrated their effectiveness in the treatment of patients with severe and critical forms of COVID-19.
Respiratory support. Traditionally, it was assumed that in ARDS, early intubation (insertion of an endotracheal tube into the trachea to secure the airway) and mechanical ventilation improve patient survival. However, given the poor prognosis of mechanical ventilation in patients with COVID-19, increasingly more attention is being paid to methods of noninvasive respiratory support, which include high-flow oxygen therapy and noninvasive lung ventilation (NIV).
Noninvasive lung ventilation is a method of respiratory support in which the main interface—a mask or helmet—is easily applied and detached from the patient’s airways [2]. Unlike traditional mechanical ventilation, artificial airways (intubation tube, tracheostomy) are not required, swallowing and eating functions are preserved, the need for sedatives is reduced, and, most importantly, the risk of direct damage to the respiratory tract and nosocomial infections is significantly decreased.
Since the onset of the pandemic, the role of NIV in hypoxemic acute respiratory failure in patients with COVID-19 has been the subject of heated debate and discussion. The joint guidance issued in Britain by the Intensive Care Society, the Association of Anesthesiologists, and the Royal College of Anesthetists in early 2020 stated that the use of NIV or similar devices should be avoided, noting that there is no survival advantage over conventional oxygen therapy, and the risk of contracting the virus may be higher. The World Health Organization in 2020 recommended the use of NIV only in individual patients with hypoxemic respiratory failure. However, just a few months after the start of the pandemic, NIV was considered as the first line of respiratory support in the recommendations of the UK National Health Service for hypoxemic acute respiratory failure in patients with COVID-19 [3]. A similar approach was also soon supported in Italy, Russia, and other countries [4, 5].
NIV helps to recruit collapsed alveoli and reduces the work of breathing [5, 6]. Randomized clinical trials and guidelines support the use of NIV as a first-line therapy for exacerbations of chronic obstructive pulmonary disease (COPD) with respiratory acidosis and acute heart failure [2, 7, 8]. However, the evaluation of the effectiveness of the method in acute hypoxemic respiratory failure is quite controversial.
In hypoxemic ARF, the main goals are to improve oxygenation, reduce the work of breathing (the work to overcome all types of resistance performed by the respiratory muscles during ventilation), and decrease shortness of breath. The first goal can usually be achieved by using higher levels of positive end-expiratory pressure to recruit unventilated or poorly ventilated alveoli into the process of ventilation [6], which leads to an increase in the functional residual lung capacity, a decrease in ventilation‒perfusion (V/Q) mismatch and shunt, and therefore improved oxygenation. In addition, the use of higher levels of positive pressure stabilizes the airways, reduces the inhomogeneity of the distribution of lung volumes, and decreases the load on the respiratory muscles.
A meta-analysis including 25 studies involving 3804 patients with hypoxemic ARF has shown that, compared with standard oxygen therapy, noninvasive ventilation with helmets (risk ratioFootnote 1 is 0.26) and face masks (RR 0.76) reduces the need for tracheal intubation [9]. NIV using both interfaces—a helmet (RR 0.40) and face masks (RR 0.83)—reduces the risk of death.
To date, more than 50 studies have been published on the effectiveness of NIV in hypoxemic acute respiratory failure in patients with COVID-19; most of them are open and observational, and only a few are randomized controlled. Both the former and the latter included patients with severe hypoxemic ARF, whose condition corresponded to the manifestations of severe or moderate acute respiratory distress syndrome according to the Berlin classification: the average initial values of the PaO2/FiO2 ratio varied from ~75 to 200 mm Hg; that is, according to the classical canons, these patients had indications for mechanical ventilation [10, 11]. The rather high efficacy of NIV in hypoxemic acute respiratory failure in patients with COVID-19 is evidenced by data on the proportion of intubated and deceased patients. Of course, the results presented are quite heterogeneous—the lethality of patients varied from 0 to 74%, and the need for tracheal intubation, from 22 to 38%. According to most studies, the need for tracheal intubation and the hospital mortality rates averaged 20–30% [11].
In a population-based study conducted in Italy with the participation of 1400 hospital patients, 520 people with symptoms of ARF due to COVID-19 were studied [12]. Of the 520 patients, 408 (78.5%) received only oxygen therapy, 46 (8.8%) received only NIV, 25 (4.8%) received invasive ventilation after NIV, and 41 (7.9%) received only invasive ventilation. After 60 days, mortality did not increase with mechanical ventilation after NIV (32.0%) compared with only invasive mechanical ventilation (36.6%) [12], which suggests the safety of noninvasive ventilation in patients with ARF against the background of COVID-19.
Air leakage, discomfort, and skin damage limit the tolerability of NIV with a face mask and make long-term therapy with certain settings (for example, high positive airway pressure at the end of expiration) difficult. The use of a helmet, which is a transparent cap that covers the entire head and is fixed with a soft collar on the patient’s neck, largely eliminates these shortcomings of therapy and can serve as an alternative when prescribing NIV [13].
In an open randomized controlled trial, which included 109 patients with ARF due to COVID-19 (the ratio PaO2/FiO2Footnote 2 is less than 200 mm Hg), the effects of high-flow oxygen therapy and NIV using a helmet were compared [13]. The latter did not lead to a significant improvement in the main result (number of days without respiratory support), but significantly reduced the frequency of tracheal intubation. NIV with a helmet may be the preferred strategy to improve outcomes in patients with COVID-19.
In a multicenter three-group open adaptive randomized controlled trial [14], hospitalized patients with ARF caused by COVID-19 were randomly assigned to CPAP (Constant Positive Airway Pressure) therapy groups—mechanical ventilation using constant positive pressure, high-flow oxygen therapy, and conventional oxygen therapy. The primary endpoint of the trial was a combination of tracheal intubation or mortality within 30 days. Over 13 months, 1272 participants were randomized and included in the analysis: 380 patients received CPAP therapy (29.9%); 417 patients, high-flow oxygen therapy (32.8%); and 475 patients, traditional oxygen therapy (37.3%). The need for tracheal intubation or mortality within 30 days were lower in the CPAP group. There was no difference between high-flow oxygen therapy and conventional oxygen therapy. Thus, CPAP compared with conventional oxygen therapy reduced the combined outcome of intubation or death within 30 days of randomization in hospitalized adults with ARF due to COVID-19.
Prone positioning for nonintubated patients. From its first description in the 1970s to the COVID-19 pandemic, the prone position was used only for severe hypoxemic acute respiratory failure requiring mechanical ventilation. The proposed mechanisms for improving oxygenation include a better V/QFootnote 3 match, redistribution of blood flow, and changes in the lung volume and compliance of the chest wall. According to the results of several randomized controlled trials, prone positioning in patients with severe acute respiratory distress syndrome on invasive ventilation improves survival.
We know today that prone positioning can effectively improve oxygenation and reduce the inspiratory effort in nonintubated patients with acute respiratory failure without the use of any additional resources. One of the first studies in such patients treated with oxygen or high-flow oxygen therapy/NIV for moderate to severe ARF reported an improvement in oxygenation, but this was not sustained after resupination (turning) of the patients [15].
The COVID-19 pandemic has given a powerful impetus to the widespread use of prone positioning for nonintubated patients with ARF due to COVID-19. According to an international survey conducted in 40 countries with 502 respondents, prone positioning was used in 46.2% of treatment centers [16], but despite the great interest in it on the part of the medical community, evidence for its effectiveness is still limited.
In a multicenter retrospective comparative study of 827 nonintubated patients with severe COVID-19, prone positioning was associated with less need for mechanical ventilation (23.6 vs. 40.4%) and lower in-hospital mortality (20 vs. 37.9%) [17].
A prospective metastudy using data from six open randomized controlled trials included 1126 patients with hypoxemic ARF due to COVID-19 who required respiratory support with high-flow oxygen therapy. They were randomly assigned to two groups: with prone positioning and standard care [18]. A positive effect was observed in 223 (40%) of 564 patients who were assigned to prone positioning while awake, and in 257 (46%) of 557 patients who underwent standard treatment. On the 28th day of therapy, when comparing prone positioning with standard treatment, the risk ratio was 0.75 for intubation and 0.87 for mortality. In patients with hypoxemic ARF due to COVID-19, prone positioning reduced treatment failure and the need for intubation.
On the other hand, some trials have shown negative results. A large retrospective observational study including 166 cases of ARF with COVID-19 requiring oxygen supplementation (>3 L/min) and tachypnea (>24 breaths per minute) showed no difference in the intubation rates in prone positioning (58%) and routine therapy (49%) [19]. Thus, the benefits of prone positioning for patients with acute respiratory failure due to COVID-19 have yet to be confirmed.
Note adverse events. Side effects of the prone position include discomfort, nosebleeds, chest pain, back pain, and bedsores. Abdominal distention, gastroesophageal reflux, vomiting, and accidental loss of oxygen support can also occur when lying on the stomach.
There is no consensus thus far regarding the characteristics a patient should meet to recommend prone positioning. Most studies have applied awake prone positioning to patients with mild to moderate hypoxic ARF. Those requiring urgent intubation or patients with altered mental status, hemodynamic instability, trauma, or intraabdominal hypertension were not eligible for prone positioning. There is no consensus on the optimal duration and frequency of the procedure. The duration of prone positioning for each session varied from <1 to >18 h; sessions were repeated throughout the day.
A multicenter prospective cohort study of 335 patients evaluated the effect of the duration of the prone position on the risk of tracheal intubation and hospital mortality in patients with COVID-19-related ARF [20]. One hundred and eighty-seven (56%) of them were in the prone position for 12 (95%) h/day, and 148 (44%) served as controls. After adjusting for other confounding factors, the odds ratio (OR)Footnote 4 for tracheal intubation in the prone positioning group was 0.36, decreasing gradually as the duration of the sessions increased. The adjusted OR of hospital mortality in the prone position ≥6 h/day group was 0.47. Exposure to the prone position ≥8 h/day resulted in a further decrease in OR (0.37). Thus, in the study population, prone positioning for ≥6 h/day reduced the risk of tracheal intubation, and exposure for ≥8 h/day reduced the risk of in-hospital mortality.
It is recognized that prone positioning is not effective in all cases; it is very difficult to predict its lasting effect on oxygenation. In a study performed by my colleagues and myself, changes in lung aeration were evaluated using ultrasound as a possible way to predict the response from oxygenation in the prone position [21]. A significant increase in PaO2/FiO2 (more than 20 mm Hg) was noted in 72.7% of patients. In those who responded to the prone position, the initial disturbances in aeration in the posterior sections of the lungs were more pronounced (p = 0.006) (p is the probability of error in rejecting the null hypothesis). The decrease in the total score on the lung ultrasound assessment scale and the ultrasound score of the posterior sections was significantly higher in responders (p < 0.001). Thus, in patients with severe COVID-19, the response to prone positioning is likely to depend on the extent and location of lung tissue changes. Aeration changes assessed by lung ultrasound may be useful in predicting the oxygenation response to prone positioning in awake, nonintubated patients with COVID-19-associated ARF.
Accepted approaches to medical therapy for COVID-19. In accordance with the biphasic pattern of COVID-19, it is expected that antiviral therapy will have the greatest benefit in the early stages of the disease, while targeting the patient’s immune response will have a positive impact later. This division is more clearly distinguishable from the point of view of the conditions of care (outpatient, inpatient, intensive care).
Data from noncritically ill hospitalized patients suggest the benefit of drug treatment that targets both the virus and the systemic inflammation caused by the infection. Among the drugs of this kind, we note remdesivir, an inhibitor of viral RNA polymerase; it is approved by the US Food and Drug Administration for the treatment of hospitalized patients with COVID-19. In a multicenter randomized control trial of 1062 hospitalized patients with COVID-19 pneumonia, those treated with remdesivir had a faster recovery compared to placebo (median 10 vs. 15 days, p < 0.001) [22]. However, a multicenter open-label study evaluating remdesivir along with three other repurposed antivirals for the treatment of COVID-19 found no mortality benefit for remdesivir compared with controls [23].
In a pragmatic randomized open-label study involving 6425 patients in 176 UK hospitals, treatment with dexamethasone (6 mg for 10 days) was associated with a reduction in 28-day mortality among patients hospitalized with COVID-19 [24]. A meta-analysis of other small studies examining the effectiveness of systemic glucocorticoids (GCS) in COVID-19 was consistent with the results of this study. The reduction in mortality appeared to be limited to inpatients receiving supplemental oxygen, including high-flow oxygen therapy and mechanical ventilation. Unfortunately, the authors did not distinguish between conventional oxygen therapy and high-flow oxygen therapy; so, the effect of treatment in noncritical patients is not clear.
Since inhibition of interleukin-6 (IL-6) is effective in cytokine release syndrome, which may have some similarities with the critical course of COVID-19, studies have been conducted to evaluate the effectiveness of IL-6 receptor inhibitors: tocilizumab and sarilumab. While the overall results appear to be mixed, multiple trials point to the potential benefit of tocilizumab in some subgroups of more severely ill patients, especially when given within 24 h of admission to the intensive care unit in patients requiring high-flow oxygen therapy, NIV, or mechanical ventilation [25].
Baricitinib serves as a selective inhibitor of Janus kinases 1 and 2. In a randomized control trial, this drug, in combination with remdesivir, reduced the time to recovery compared with remdesivir alone, with the strongest effect in acute respiratory distress syndrome [26]. However, it remains unclear whether baricitinib provides additional benefit to patients already receiving glucocorticoids.
Due to the proven association of COVID-19 and vascular thrombosis, a coalition of three multicenter randomized open-label trials compared the therapeutic dose of heparins with the standard prophylactic dose in hospitalized patients with COVID-19 [27]. The published results suggest a reduction in organ failure in noncritically ill patients receiving a full dose of anticoagulants but no benefit from a high dose in critically ill patients.
Promising approaches to drug therapy for COVID-19: Thiol-containing preparations. At present, there is a lot of discussion about the possible role of oxidative stress in the pathogenesis of COVID-19. Among hospitalized patients, a strong relationship has been demonstrated between biomarkers of oxidative stress and the severity of the disease. High stress levels and lower antioxidant indices may exacerbate the severity of COVID-19 [28]. Excessive oxidative stress may lead to alveolar damage, thrombosis, and erythrocyte dysregulation observed in COVID-19.
The accumulated data suggest that N-acetylcysteine (NAC) and erdosteine, which are also classified as mucolytic agents, being thiol drugs, exhibit multiple pharmacological activities relevant to the treatment of some respiratory diseases, including chronic obstructive pulmonary disease (COPD) and idiopathic pulmonary fibrosis (IPF) [28]. In addition to powerful antioxidant and anti-inflammatory properties, these drugs exhibit antibacterial and antiviral activity and can affect bronchial tone. Thiol-containing drugs can modulate inflammation and oxidative stress by acting through NF-kB (inhibitor of the pathway). Given the importance of oxidative stress in COVID-19 and the pharmacological properties of thiol-based drugs, the possible role of thiols in the treatment of COVID-19 can be speculated. Oral and intravenous glutathione, as well as its precursors such as N-acetylcysteine (NAC) and erdosteine, may form the basis of a new treatment approach and be used to block NF-kB and eliminate cytokine storm syndrome and the respiratory distress observed in patients with COVID-19 [28].
A two-center retrospective cohort study in Greece, which included 82 patients with viral pneumonia caused by COVID-19, reported a lower rate of progression of severe respiratory failure, a decrease in the need for mechanical ventilation, and a decrease in the risk of death when patients received NAC at a dose of 1200 mg/day [29].
In a Russian case-control study, 24 patients with confirmed SARS-CoV-2 infection and radiological findings consistent with severe pneumonia caused by COVID-19 received NAC at a daily dose of 1200‒1800 mg intravenously, and 22 patients were included in the study as a control group [30]. NAC therapy provided a significant improvement in oxygenation parameters and a decrease in the level of C-reactive protein as a marker of inflammation, the number of scores on the NEWS-2 scale, and the duration of hospitalization. In addition, in the intake group, according to computed tomography, there was a more rapid decrease in the levels of C-reactive protein and the volume of lung parenchyma damage, as well as the restoration of oxygenation parameters [31].
However, in a Brazilian study, in which 67 patients with severe COVID-19 were randomized to receive NAC at a dose of 21 g (approximately 300 mg/kg) for 20 hours and 68 patients were assigned to the control group, no differences between the two groups regarding the need for invasive mechanical ventilation were identified [32]. No differences were found in secondary endpoints (mortality, ICU hospitalization, invasive ventilation time).
Despite conflicting clinical data, the pharmacology of thiol-containing drugs suggests that they should be considered as adjunctive therapy in patients with pneumonia and other complications of COVID-19 and as an adjunct to standard care in patients discharged from the hospital after COVID-19. Several clinical randomized control trials are currently underway to investigate the effects of N-acetylcysteine in COVID-19.
Inhalation surfactant. The use of an exogenous surfactant (a mixture of surfactants lining the lung alveoli and bronchial tree from the inside) may be a promising treatment for patients with acute respiratory distress syndrome associated with COVID-19. Pulmonary surfactant is produced by type II alveolocytes; its main function is to reduce the surface tension in the alveoli and thereby prevent lung collapse and maintain gas exchange. In addition, pulmonary surfactant participates in the barrier and protective function of the lungs, influencing the innate and adaptive types of the immune response. The surfactant also has anti-inflammatory properties; reduces the production of tumor necrosis factor alpha, IL-1, and IL-6; and, thus, can effectively promote the recovery of damaged alveoli in ARDS associated with COVID-19 [33].
SARS-CoV-2 predominantly attacks type II alveolocytes; the release of the virus, followed by replication, leads to apoptosis and ultimately to the death of the patient. Damage to type II alveolocytes dramatically reduces the production of pulmonary surfactant and its secretion into the alveolar space, which leads to alveolar collapse and inflammation, increased capillary permeability, edema, and microvascular thrombosis.
Exogenous surfactant therapy has been used safely and successfully for the treatment of neonatal respiratory distress syndrome (RDS), but its efficacy in adult patients with ARDS has not yet been proven. Several randomized controlled trials failed to confirm the effectiveness of surfactant therapy in ARDS in adults, probably because of some methodological limitations, such as inadequacy of the timing, doses, and methods of delivery of surfactant and the heterogeneity of groups of patients with ARDS.
To date, several small studies have been published on the possibility of using exogenous surfactant in ARDS associated with COVID-19 [33, 34]. In two of them (including five and seven patients), the drug was administered during bronchoscopy in intubated patients. The first results were very promising: the exogenous surfactant led to an improvement in the oxygenation parameters and an increase in the static compliance of the lungs; in addition, a positive trend towards a decrease in mortality was found in one of the studies [34].
It is quite likely that early initiation of exogenous surfactant therapy, before tracheal intubation and mechanical ventilation, may be even more effective. Theoretically, such therapy will reduce the risk of disease progression, decrease the need for tracheal intubation and mechanical ventilation, and possibly reduce mortality. One of the currently available delivery methods for surfactant is inhalation. Advances in technology have led in recent years to the widespread introduction of vibrating mesh nebulizers into clinical practice, which have improved pulmonary drug deposition and reduced procedure time. It is important that, when using new generation inhalers, the ultrastructure and integrity of the surfactant and its characteristics do not change. In animal models, nebulized surfactant therapy was associated with a lower incidence of adverse hemodynamic effects compared to bolus administration, resulting in improved uniformity of drug distribution. Note that in Russia an original surfactant-BL was developed more than 20 years ago; it is based on the lungs of cattle and is as close as possible in its composition to human lung surfactant.
The first published study (involving 122 patients) on the effectiveness of inhaled surfactant in the complex treatment of severe forms of COVID-19 was performed at Sechenov University and the Almazov National Medical Research Center (St. Petersburg) [35]. Fifty-six patients received inhaled surfactant-BL at a dose of 1 mg/kg 2‒3 times/day, and 66 patients were in the control group. Among those who received surfactant therapy, 14.3% died, while among those who did not receive it, 41% did (p = 0.001). Thus, judging by the results of this pilot study, inhaled surfactant therapy can improve the prognosis of severe SARS-CoV-2 pneumonia.
The author of this article and my colleagues used inhaled surfactant-BL at a daily dose of 150‒300 mg as an additional option for patients treated with NIV in COVID-19 associated with ARDS [36]. Inhalations were carried out using a mesh nebulizer placed in the breathing circuit. On the fifth day of therapy, the PaO2/FiO2 ratio in patients improved significantly compared to the control group (184 (155–212) mm Hg vs. 150 (91–173) mm Hg, p = 0.02). Inhaled surfactant significantly reduced the need for transfer of patients to the intensive care unit (24.2 vs. 46.9%, p = 0.05) and invasive mechanical ventilation (18.2 vs. 40.6%, p = 0.04). The duration of NIV and hospitalization were significantly shorter in the surfactant group compared to the control group.
These preliminary data suggest that patients with ARDS-associated COVID-19 on NIV may benefit from the use of nebulized surfactant. However, data from larger clinical trials, including randomized controlled ones, are urgently needed today. In this context, a number of larger trials of inhaled surfactant therapy for COVID-19 associated with ARDS are underway.
Inhaled analogues of prostacyclin. Acute respiratory distress syndrome is characterized by diffuse alveolar damage leading to edema and atelectasis. In ARDS, an imbalance of vasoconstriction in well-ventilated areas and vasodilatation in poorly ventilated areas leads to a redistribution of the blood flow from well-ventilated to poorly ventilated alveoli and V/Q mismatch, which in turn causes hypoxemia. Other factors contributing to decreased perfusion of well-ventilated alveoli are vascular obstruction due to edema, inflammation, and (micro)thrombosis. Morphological studies have shown that pulmonary endotheliitis and microangiopathy are significantly more common with COVID-19 compared with other viral respiratory diseases.
The use of pulmonary vasodilators (drugs that dilate blood vessels) can reduce vasoconstriction, increase pulmonary vascular perfusion, and improve oxygenation. In ARDS, inhaled nitric oxide (NO) and inhaled prostacyclin analogues—epoprostenol, iloprost, and treprostinil—were considered as drugs that promote a selective increase in blood flow to partially ventilated alveoli. Inhaled vasodilators have the potential advantage of delivering the drug only to ventilated areas of the lungs.
Prostacyclin analogues have a potent vasodilating effect; pulmonary vasodilation is achieved by increasing the concentration of cyclic adenosine monophosphate in smooth muscle cells, drug interaction with prostacyclin receptors, and opening of potassium channels, possibly, by antagonism with endothelin. In addition, prostacyclin analogues have antithrombotic, anti-inflammatory, and antiproliferative effects, exerting these effects by inhibiting platelet activation and suppressing the production of IL-6 and tumor necrosis factor alpha. Important therapeutic effects of prostacyclin in the treatment of COVID-19 are the modulation of the expression of adhesion molecules and the interaction between macrophages and the activated endothelium. Prostacyclin analogues also reduce pulmonary sequestration of leukocytes and platelets, which is an important mechanism in the development of ARDS.
Prior to the COVID-19 pandemic, inhaled iloprost was shown to lead to a significant improvement in the PaO2/FiO2 ratio and PaO2 without adversely affecting lung mechanics or systemic hemodynamics in patients with ARDS and pulmonary hypertension. To date, several clinical studies have been published on the efficacy of inhaled prostacyclin analogues in severe forms of COVID-19.
The efficacy and safety of inhaled epoprostenol (iEpo) and inhaled NO in 38 mechanically ventilated patients with ARDS associated with COVID-19 and refractory hypoxemia were studied by DeGrado et al. [37]. All patients received inhaled epoprostenol as the initial pulmonary vasodilator. Sixteen patients (42%) were classified as responders (>10% increase in PaO2/FiO2) to iEpo with a mean increase in PaO2/FiO2 of 34.1 (24.3–53.9) mm Hg. No factors have been found to predict which patients with refractory hypoxemia may benefit from pulmonary vasodilator therapy.
In a retrospective single-center cohort study, the authors found that the combined use of inhaled iEpo and prone positioning improved oxygenation (84.0 ± 25.6 vs. 124.7 ± 62.7 mm Hg; p < 0.001) in 43 intubated COVID-19 patients with refractory hypoxemia, including those that did not respond to prone positioning or iEpo alone [38]. Epoprostenol was delivered by continuous nebulization using a mesh nebulizer. In 27 patients (63%), PaO2/FiO2 improved by more than 20% with a combination of inhaled epoprostenol and prone positioning; survival was higher among responders compared to nonresponders (52 vs. 81%; p = 0.025).
The first and thus far only study of the efficacy of inhaled prostacyclin analogues in nonintubated patients with COVID-19-associated ARDS was a case-control study [39]. A total of 23 patients received at least one iloprost inhalation, and 22 were included in the control group. Iloprost was administered with a mesh nebulizer 4 times a day for 5 days. Prior to this, 7 patients received NIV, and 16 required additional oxygen therapy. On the fifth day, the therapy resulted in a more significant improvement in PaO2/FiO2 values compared to the control group. The study suggested that inhaled iloprost may be a possible therapeutic option to improve oxygenation in nonintubated patients with COVID-19-associated ARDS.
To the best of the author’s knowledge, there are no published randomized controlled trials of the efficacy of inhaled prostacyclin analogues in ARDS associated with COVID-19; however, several such trials are currently underway.
٭ ٭ ٭
COVID-19 is characterized by a severe course in approximately 5‒10% of patients with the need for their admittance to the intensive care unit and mechanical ventilation, which is associated with a very high risk of a poor prognosis. Currently, in real clinical practice, in the management of severe patients with COVID-19, noninvasive lung ventilation (NIV) is widely used (in some countries, up to 60% of all methods of respiratory support). In most studies on the effectiveness of NIV in hypoxemic ARF in patients with COVID-19, the need for tracheal intubation and hospital mortality with the use of NIV averaged 20–30%, which suggests a fairly high efficacy of the method. The COVID-19 pandemic has given a powerful impetus to the widespread use of prone positioning in nonintubated patients with ARF due to COVID-19. A number of studies have shown that prone positioning can reduce the need for mechanical ventilation and hospital mortality. Medications that have proven effective in severe forms of COVID-19 include remdesivir, systemic glucocorticoids, tocilizumab, baricitinib, and anticoagulants. Among the new promising areas of drug therapy, noteworthy is the use of thiol-containing drugs (N-acetylcysteine), inhaled surfactant, and inhaled prostacyclin analogues.
Notes
The risk ratio (RR) is the measure most often used to assess changes in survival. An RR of 0.5 means that the risk of death in the intervention group is two times lower than in the control group.
PaO2/FiO2 is the oxygenation index, PaO2 is the partial pressure of oxygen, and FiO2 is the fractional concentration of oxygen in the inhaled air.
V/Q is the amount of air that reaches the alveoli divided by the amount of blood flow in the capillaries of the lungs.
The odds ratio (OR) is a characteristic used in mathematical statistics to describe quantitatively the closeness of the relationship between trait A and B in a certain statistical population.
REFERENCES
G. Grasselli, M. Greco, A. Zanella, et al., “Risk factors associated with mortality among patients with COVID-19 in Intensive Care Units in Lombardy, Italy,” JAMA Intern. Med. 180 (10), 1345–1355 (2020). https://doi.org/10.1001/jamainternmed.2020.3539
S. N. Avdeev, “Noninvasive lung ventilation in acute respiratory failure: From clinical guidelines to real clinical practice,” Pul’monologiya, No. 1, 32–35 (2018).
NHS. Guidance for the role and use of non-invasive respiratory support in adult patients with COVID-19 (confirmed or suspected), April 6, 2020, Version 3. https://amhp.org.uk/app/uploads/2020/03/Guidance- Respiratory-Support.pdf
M. Vitacca, S. Nava, P. Santus, and S. Harari, “Early consensus management for non-ICU ARF SARS-CoV-2 emergency in Italy: From ward to trenches,” Eur. Respir. J. 55, 2000632 (2020).
S. N. Avdeev, N. A. Tsareva, Z. M. Merzhoeva, et al., “Practical recommendations for oxygen therapy and respiratory support for patients with COVID-19 in the preresuscitation stage,” Pul’monologiya, No. 2, 151–163 (2020).
E. L’Her, N. Deye, F. Lellouche, et al., “Physiologic effects of noninvasive ventilation during acute lung injury,” Am. J. Respir. Crit. Care Med, No. 9, 1112–1118 (2005).
S. N. Avdeev, “Noninvasive lung ventilation in patients with chronic obstructive pulmonary disease in hospital and at home,” Pul’monologiya, No. 2, 232–249 (2017).
S. N. Avdeev, A. V. Tret’iakov, R. A. Grigor’iants, et al., “Study of the use of noninvasive ventilation of the lungs in acute respiratory insufficiency due to exacerbation of chronic obstructive pulmonary disease,” Anesteziol. Reanimatol., No. 3, 45–51 (1998).
B. L. Ferreyro, F. Angriman, L. Munshi, et al., “Association of noninvasive oxygenation strategies with all-cause mortality in adults with acute hypoxemic respiratory failure. A systematic review and meta-analysis,” JAMA 324 (1), 57–67 (2020).
S. Avdeev, A. Yaroshetskiy, N. Tsareva, et al., “Noninvasive ventilation for acute hypoxemic respiratory failure in patients with COVID-19,” Amer. J. Emerg. Med. 39, 154–157 (2021). https://doi.org/10.1016/j.ajem.2020.09.075
S. N. Avdeev, “Noninvasive ventilation of the lungs with a new coronavirus infection COVID-19,” Pul’monologiya, No. 5, 679–687 (2020).
A. Potalivo, J. Montomoli, F. Facondini, et al., “Sixty-day mortality among 520 Italian hospitalized COVID-19 patients according to the adopted ventilatory strategy in the context of an integrated multidisciplinary clinical organization: A population-based cohort study,” Clin. Epidemiol. 12, 1421–1431 (2020).
D. L. Grieco, L. S. Menga, M. Cesarano, et al., “Effect of helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: The HENIVOT randomized clinical trial,” JAMA 325 (17),1731–1743 (2021).
G. D. Perkins, C. Ji, B. A. Connolly, et al., “An adaptive randomized controlled trial of non-invasive respiratory strategies in acute respiratory failure patients with COVID-19,” MedRxiv, 2022. https://doi.org/10.1101/2021.08.02.21261379
V. Scaravilli, G. Grasselli, L. Castagna, et al., “Prone positioning improves oxygenation in spontaneously breathing nonintubated patients with hypoxemic acute respiratory failure: a retrospective study,” J. Crit. Care 30 (6), 1390–1394 (2015).
J. S. Alqahtani, R. G. Mendes, A. Aldhahir, et al., “Global current practices of ventilatory support management in COVID-19 patients: An international survey,” J. Multidiscip. Healthc., No. 13, 1635–1648 (2020).
O. R. Perez-Nieto, D. Escarraman-Martinez, M. A. Guerrero-Gutierrez, et al., “Awake prone positioning and oxygen therapy in patients with COVID-19: The APRONOX study,” Eur. Respir. J. 59 (2), 2100265 (2022).
S. Ehrmann, J. Li, M. Ibarra-Estrada, Y. Perez, et al., “Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: a randomised, controlled, multinational, open-label meta-trial,” Lancet Respir. Med. 9 (12), 1387–1395 (2021).
E. M. H. Padrao, F. S. Valente, B. A. M. P. Besen, et al., “Awake prone positioning in COVID-19 hypoxemic respiratory failure: Exploratory findings in a single-center retrospective cohort study,” Acad. Emerg. Med. 27 (12), 1249–1259 (2020).
M. Esperatti, M. Busico, N. A. Fuentes, et al., “Impact of exposure time in awake prone positioning on clinical outcomes of patients with COVID-19-related acute respiratory failure treated with high-flow nasal oxygen: A multicenter cohort study,” Crit. Care. 26 (1), 16 (2022).
S. N. Avdeev, G. V. Nekludova, N. V. Trushenko, et al., “Lung ultrasound can predict response to the prone position in awake non-intubated patients with COVID‑19 associated acute respiratory distress syndrome,” Crit. Care 25 (1), 35 (2021).
J. H. Beigel, K. M. Tomashek, L. E. Dodd, et al., “Remdesivir for the treatment of Covid-19: Final report,” New Engl. J. Med. 383, 1813–1826 (2020).
WHO Solidarity Trial Consortium. H. Pan, R. Peto, A. M. Henao-Restrepo, et al., “Repurposed antiviral drugs for Covid-19: Interim WHO Solidarity Trial results,” N. Engl. J. Med. 384 (6), 497–511 (2021).
RECOVERY Collaborative Group. P. Horby, W. S. Lim, J. R. Emberson, et al., “Dexamethasone in hospitalized patients with Covid-19,” New Engl. J. Med. 384 (8), 693–704 (2021).
RECOVERY Collaborative Group, “Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial,” Lancet 397 (10285), 1637–1645 (2021).
A. C. Kalil, T. F. Patterson, A. K. Mehta, et al., “Baricitinib plus remdesivir for hospitalized adults with Covid-19,” New Engl. J. Med. 384 (9), 795–807 (2021).
ATTACC Investigators; ACTIV-4a Investigators; REMAP-CAP Investigators. P. R. Lawler, E. C. Goligher, J. S. Berger, et al., “Therapeutic anticoagulation with heparin in noncritically ill patients with Covid-19,” New Engl. J. Med. 385 (9), 790–802 (2021).
M. Cazzola, P. Rogliani, S. S. Salvi, et al., “Use of thiols in the treatment of COVID-19: Current evidence,” Lung. 199 (4), 335–343 (2021).
S. F. Assimakopoulos, D. Aretha, D. Komninos, et al., “N-acetyl-cysteine reduces the risk for mechanical ventilation and mortality in patients with COVID-19 pneumonia: A two-center retrospective cohort study,” Infect. Dis. (London) 53 (11), 847–854 (2021).
S. N. Avdeev, V. V. Gaynitdinova, Z. M. Merzhoeva, Z. G. Berikkhanov, “N-acetylcysteine for the treatment of COVID-19 among hospitalized patients,” J. Infect. 84 (1), 94–118 (2022).
V. V. Gainitdinova, S. N. Avdeev, Z. M. Merzhoeva, et al., “Experience in the use of N-acetylcysteine in the complex treatment of moderate COVID-associated pneumonia,” Pul’monologiya, No. 1, 21–29 (2021).
J. C. G. de Alencar, C. L. Moreira, A. D. Muller, et al., “Double-blind randomized placebo-controlled with N-acetylcysteine for treatment of severe acute respiratory syndrome caused by coronavirus disease 2019 (COVID-19),” Clin. Infect. Dis. 72 (11), e736–741 (2021).
S. Busani, L. Dall’Ara, R. Tonelli, et al., “Surfactant replacement might help recovery of low-compliance lung in severe COVID-19 pneumonia,” Ther. Adv. Respir. Dis. 14, 1–6 (2020).
S. Piva, R. M. DiBlasi, A. E. Slee, et al., “Surfactant therapy for COVID‑19 related ARDS: A retrospective case-control pilot study,” Respir. Res. 22, 20 (2021). https://doi.org/10.1186/s12931-020-01603-w
A. E. Bautin, S. N. Avdeev, A. A. Seiliev, et al., “Surfactant inhalation therapy in the integrated treatment of severe COVID-19 pneumonia,” Tuberkulez Bolezni Legkikh, No. 9, 6–12 (2020). https://doi.org/10.21292/2075-1230-2020-98-9-6-12
S. N. Avdeev, N. V. Trushenko, S. Y. Chikina, et al., “Beneficial effects of inhaled surfactant in patients with COVID-19-associated acute respiratory distress syndrome,” Respir. Med. 185, 106489 (2021).
J. R. DeGrado, P. M. Szumita, B. R. Schuler, et al., “Evaluation of the efficacy and safety of inhaled epoprostenol and inhaled nitric oxide for refractory hypoxemia in patients with coronavirus disease 2019,” Crit. Care Explor. 2 (10), e0259 (2020).
J. Li, J. B. Fink, A. E. Augustynovich, S. Mirza, et al., “Effects of inhaled epoprostenol and prone positioning in intubated coronavirus disease 2019 patients with refractory hypoxemia,” Crit. Care Explor. 2 (12), e0307 (2020).
N. A. Tsareva, S. N. Avdeev, D. Kosanovic, et al., “Inhaled iloprost improves gas exchange in patients with COVID-19 and acute respiratory distress syndrome,” Crit. Care 25 (1), Article no. 258 (2021).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The author declares that he has no conflicts of interest.
Additional information
Translated by B. Alekseev
RAS Academician Sergei Nikolaevich Avdeev is Head of the Department of Pulmonology at the Institute of Clinical Medicine of Sechenov University, Head of the Clinical Department at the Pulmonology Research Institute of the Federal Medical‒Biological Agency (FMBA) of Russia, and Chief Pulmonologist of the Ministry of Health of Russia.
Rights and permissions
About this article
Cite this article
Avdeev, S.N. COVID-19: Opportunities to Improve Prognosis. Her. Russ. Acad. Sci. 92, 404–411 (2022). https://doi.org/10.1134/S1019331622040025
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S1019331622040025