Abstract
Currently, a comprehensive assessment of the relationship between ideal cardiovascular health (CVH) indicators and cataract risk is lacking. Life’s Essential 8 (LE8) is the latest concept proposed by the American Heart Association to comprehensively reflect CVH status. LE8 includes four health behaviors (diet, physical activity, smoking, and sleep) and four health factors (blood lipid, blood sugar, blood pressure, and body mass index). This study tried to evaluate the association between LE8 and cataract using data from National Health and Nutrition Examination Survey (NHANES) 2005–2008, a continuous research program which aims to monitor and evaluate the health and nutrition status of the US population. A cross-sectional study of 2720 non-cataract participants and 602 cataract participants. All participants were assigned to the poor, intermediate, and ideal CVH status groups based on LE8 score. Weighted multiple logistic regression was used to investigate the correlation between the LE8 score and cataract, as well as the correlation between each of the eight subitems and cataract, with potential confounding variables being adjusted. Then, restricted cubic spline analysis was used to further explore whether there was a nonlinear relationship between LE8 score and cataract. The proportion of cataract participants was 14.1%, 18.2%, and 20.6% in the ideal, intermediate, and poor CVH groups, respectively (P < 0.05). LE8 score was inversely associated with cataract risk, with each 10-point increase in LE8 score associated with a 14% reduction in cataract risk [odds ratio (OR) = 0.86, 95% confidence interval (CI): 0.79–0.93, P < 0.01]. Among all the LE8 subitems, physical activity, sleep, and blood glucose were significantly associated with cataract risk (all P < 0.05). Better CVH, defined by a higher LE8 score, is associated with a lower cataract risk. Efforts to improve LE8 score (especially when it comes to physical activity, sleep, and blood glucose) may serve as a novel strategy to help reduce the risk of cataract.
Similar content being viewed by others
Introduction
Cataract is a degenerative disease of the lens that is related to multiple factors such as age, environment, and metabolism1,2,3. In recent years, under the influence of the aging global population, the prevalence of cataracts has increased significantly4. In 2000, there were 20.5 million cataract patients in the United States, and this number is projected to increase to 38.7 million by 20305,6. The harm caused by cataracts is mainly visual impairment, which can even lead to blindness in severe cases. According to the Global Burden of Disease Study, cataract is the leading cause of blindness in people aged over 50 years and the second leading global cause of moderate and severe vision impairment (MSVI) in the general population7. At present, surgery is still the only effective and recognized treatment option for cataracts. Modern cataract surgery, which includes removing the affected lens and implanting an artificial lens, has been shown to improve the patient's visual acuity and quality of life in a safe and quick manner. However, cataract surgery is not without surgical complications and has posed a considerable economic burden on healthcare systems8. In the United States, direct ophthalmic medical costs for cataract surgery in both eyes were $5052 per person9.
In 2010, the American Heart Association (AHA) introduced the concept of Life’s Simple 7 (LS7) as a tool for assessing cardiovascular health (CVH)14. This finding suggests that actively cultivating healthy habits in accordance with the LS7 framework in life, is expected to reduce the probability of develo** eye diseases such as diabetic retinopathy.
With the continuous accumulation and updating of empirical evidence, the AHA revised and reinforced the “LS7” framework in June 2022. This revision primarily incorporated sleep health into the framework, giving rise to the concept of “Life’s Essential 8 (LE8)”15. Each LE8 subitems has its own scoring criteria, and the final LE8 score is the average score of each subitem, ranging from 0 to 100. The higher the LE8 score, the better the CVH. Similar to LE7, higher LE8 scores are associated with a protective effect against stroke and CVD16,17. It has long been thought that certain CVD risk factors may also be associated with cataract risk, such as diabetes and obesity, both of which belong to the LE8 healthy factors. Meanwhile, sleep and PA, among the LE8 healthy behaviors, have received increasing attention in recent years as possible factors affecting cataract risk18,19. Thus, using LE8 factors as a metric to examine the relationship between these health variables and cataracts may provide valuable insights for cataract prevention20,21. However, to date, there is no published study concerning the correlation of the LE8 with cataracts. Given that surgery remains the only recognized effective treatment option for cataracts, it remains important to explore the modifiable risk factors for cataracts, which may provide new intervention strategies to delay or prevent the onset of cataracts, and finally to reduce the burden of this prevailing disease.
In this study, we conducted an analysis of the correlation between LE8 and cataracts employing data from the US National Health and Nutrition Examination Survey (NHANES) between 2005 and 2008, hopefully to provide healthy lifestyle guidance for cataract patients and high-risk groups.
Materials and methods
Research design and population
NHANES is a government-sponsored continuous research program administered by the National Center for Health Statistics (NCHS), which aims to monitor and evaluate the health and nutrition status of the US population. The study protocol was approved by the Research Ethics Review Board of NCHS, and all methods were performed in accordance with the relevant guidelines and regulations. This survey adopts the method of multi-stage random sampling, which selects the residents of representative states in the US, and conducts personal interviews, physical measurements, laboratory examinations, and nutrition surveys, thus providing a large amount of data for the formulation of nutrition and health policies. In order to clarify the relationship between the LE8 and cataracts, the data of the NHANES database from 2005 to 2008 were selected in this study, with the specific exclusion criteria being as follows: (1) Age < 49 (n = 14,509); (2) lack of complete LE8 information (n = 1320); (3) lack of in-formation on cataract assessment (n = 513); (4) lack of information on other covariates, including gender, race, education level, household income level, and alcohol consumption (n = 830). Finally, 3322 participants with complete information comprised the study population, which included 2720 non-cataract participants and 602 cataract patients. Figure 1 shows the specific process for the inclusion of the study population.
Definition of cataract
This study referred to other studies using self-reported history of cataract surgery as the diagnostic criteria22,23. Considering that the US has a coverage and low threshold for cataract surgery, self-reported cataract surgery could be used as a surrogate for clinically significant cataracts22. When participants completed a questionnaire that asked “Have you previously undergone cataract surgery?”. A positive response to this question was considered an indication of the presence of cataracts.
Definition of LE8
The LE8 considers the impact of both health behaviors and health factors on CVH15. Healthy behaviors include diet, PA, smoking (nicotine exposure), and sleep health, while healthy factors include blood lipid (non-high-density lipoprotein cholesterol [non-HDL cholesterol]), blood sugar, blood pressure, and BMI. The specific distribution scores of each subitem are shown in Supplementary Table 1 and Table 215. The average of the scores of the 8 subitems is the final LE8 score, which ranges between 0 and 100. As per the AHA, a score of 80–100 indicates high CVH, while a score of 50–79 suggests moderate CVH, and a score of 0–49 indicates low CVH15. In addition, we also divided each of the eight subitems into three levels: Ideal, Intermediate, and Poor. Classification criteria are listed in Table 1.
Definition of covariates
According to relevant studies14,24, we adjusted for some risk factors that might have affected the outcome as covariates. These factors mainly included: (1) age; (2) gender (male and female); (3) race (white, black, Mexican American, and other races); (4) education level (below high school, high school, and more than high school); (5) household income level, which was used household in-come-to-poverty line ratio (< 1.3, 1.3–3.5, and > 3.5); (6) alcohol consumption (never, former, moderate, mild, and heavy). Since some factors such as blood pressure, BMI, blood lipid, and diabetes were included in the estimates of the LE8 score, we did not make additional adjustments for these factors.
Statistical analysis
To ensure that the data are representative of the whole US population, our analysis was weighted according to the weights recommended by the NCHS25. In the initial phase, the data were comprehensively summarized and expounded upon based on the presence or absence of cataract. For categorical variables (expressed as percentages), the comparison between the two groups was conducted utilizing Chi-square tests, whereas continuous variables (reported as mean ± standard deviation) were subjected to one-way analysis of variance for between-group comparisons. We employed weighted multiple logistic regression to investigate the correlation between the overall LE8 score and cataract, as well as the link between each of the eight subitems and cataract. Subsequently, we adjusted for several potential confounding variables (age, gender, race, education level, household income level, and alcohol consumption) to enhance the robustness of the findings. In addition, restricted cubic spline (RCS) analysis was used to further explore whether there was a nonlinear relationship between LE8 score and cataract.
All analyses were based on survey and rms packages in R software (version 4.2.3), where P < 0.05 was considered statistically significant.
Ethics approval and consent to participate
The NCHS Institutional Review Board has approved NHANES's investigative, and all participants have provided written informed consent.
Results
Population baseline characteristics
The survey-weighted characteristics of the study population are summarized in Table 2 according to the CVH status of the participants. Overall, the mean age of all participants was 65.37 years, among whom 49.8% were females. A total of 602 cataract patients were included. The LE8 score of all participants was 62.86 ± 13.64, whereas the poor, intermediate, and ideal CVH groups had scores of 41.46 ± 6.22, 64.32 ± 8.15, and 85.06 ± 4.15, respectively (P < 0.01). The proportion of cataract participants was 14.1%, 18.2%, and 20.6% in the ideal, intermediate, and poor CVH group, respectively (P < 0.05). No significant difference in age was found among the three groups (P > 0.05). There were significant differences among the three groups in terms of household income level, gender, race, educational level, and alcohol consumption (all P < 0.05).
Relationship between LE8 score and cataract
In Table 3, after adjusting for covariates (age, gender, and race; Model 1), the presented odds ratio (OR) showed that every 10-point increase in the LE8 score was associated with a 15% decrease in the risk of having cataract (OR = 0.85, 95% CI: 0.79–0.92, P < 0.01). Even after continuing to adjust for education level, household income level, and alcohol consumption (Model 2), the result remained stable (OR = 0.86, 95% CI: 0.79–0.93, P < 0.01). When classified according to the CVH status recommended by the AHA, in Model 1, individuals with moderate to high CVH levels exhibited a reduced risk of cataract in comparison to those with low CVH levels (moderate CVH: OR = 0.71, 95% CI: 0.54–0.93, P < 0.001; High CVH: OR = 0.52, 95% CI: 0.34–0.79, P < 0.01). However, in Model 2, only highly cardiovascular-healthy individuals had a lower risk of cataract (OR = 0.56, 95% CI: 0.36–0.85, P < 0.01).
We further performed subgroup analysis and RCS analysis to determine whether the protective effect of LE8 score on cataract differs among different populations. Subgroup analysis showed that LE8 scores were more protective for individuals aged ≥ 65 years than those aged < 65 years, and were more protective for Caucasians and Mexican Americans than for African Americans and other races (Supplementary Table 3). The RCS showed a linear negative relationship between the LE8 score and cataract risk, i.e., the higher the LE8 score, the lower the risk of cataract, and this trend remained consistent across genders and age groups (Supplementary Fig. 1).
Relationship between health behaviors/factors and cataract
We further analyzed the relationship between each LE8 subitem and cataract (Table 4).
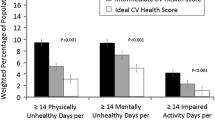
Among the four healthy behaviors, ideal sleep was negatively correlated with the risk of cataract [Model 1: OR = 0.70, 95% CI: 0.53–0.92, P < 0.05; Model 2: OR = 0.72, 95% CI: 0.55–0.96, P < 0.05]. Both intermediate PA [Model 1: OR = 0.62, 95% CI: 0.47–0.81, P < 0.01; Model 2: OR = 0.65, 95% CI: 0.49–0.85, P < 0.01] and ideal PA [Model 1: OR = 0.68, 95% CI: 0.54–0.86, P < 0.01; Model 2: OR = 0.71, 95% CI: 0.56–0.90, P < 0.01] significantly reduced the risk of cataract. Notably, ideal diet had a protective effect against cataracts in Model 1, whereas this protective effect was absent in model 2 [Model 1: OR = 0.67, 95% CI: 0.45–0.97, P < 0.05; Model 2: OR = 0.68, 95% CI: 0.46–1.00, P > 0.05]. Besides, we observed no significant effect of smoking on cataracts.
As for the four healthy factors, we observed that only intermediate blood glucose status [Model 1: OR = 0.42, 95% CI: 0.32–0.57, P < 0.01; Model 2: OR = 0.43, 95% CI: 0.32–0.58, P < 0.01] and ideal blood glucose status [Model 1: OR = 0.45, 95% CI: 0.35–0.59, P < 0.01; Model 2: OR = 0.46, 95% CI: 0.35–0.60, P < 0.01] were negatively associated with cataract risk.
Discussion
This study, to our knowledge, is the first to analyze the correlation between LE8 score (as well as each LE8 subitem) and the risk of cataracts. We found that the LE8 score was inversely associated with cataract risk. Among all the LE8 subitems, sleep duration, physical activity, and blood glucose were significantly associated with cataract risk. Our findings provide new insight into the strategy to reduce cataract and its accompanying disease burden.
Currently, a comprehensive assessment of the relationship between ideal CVH indicators and cataract risk is lacking, although some previous studies have observed associations between some LE8 subitems (such as blood glucose and diet) and cataracts26,27. Therefore, we first analyzed the correlation between LE8, an overall measure of CVH, and cataracts. We found that the better the CVH status, the lower the proportion of cataract patients, and every 10-point increase in the LE8 score was associated with a 14% reduction in cataract risk, both of which suggest that better CVH is associated with lower cataract risk. To better describe whether there is a non-linear relationship between LE8 scores and cataracts, we then performed an RCS analysis. In the RCS analysis, the LE8 score was negatively correlated with cataract risk with a cut-off LE8 score of 63, that is, people with this score have the same risk of cataracts as the general population, whereas those with a score higher than 63 have a relatively lower risk. These findings suggest that efforts to improve CVH (reflected in a higher LE8 score) can serve as a novel strategy to help reduce the risk of cataracts.
Considering that all the eight subitems of LE8 score could be controlled by lifestyle modification or medical treatment, we conducted further analyses to determine which subitems have the most significant impact on cataract risk. We found that intermediate-to-ideal-intensity PA, ideal sleep, and intermediate-to-ideal blood glucose status were associated with a reduced risk of cataracts.
The direct cause of cataract development is unknown, but oxidative damage is thought to play an important role in its pathogenesis28. Reactive oxygen species (ROS) can induce damage to the lens cell via different ways, thus causing opacification of the lens, namely cataracts29. PA may reduce oxidative stress levels by increasing endogenous antioxidant defenses30. A large meta-analysis involving 6 cohort studies also found that increased PA is negatively related to cataract risk in a dose-responsive manner18. This relationship is plausible given the beneficial effects of physical activity on oxidative stress.
Previous studies indicate that individuals with inadequate sleep duration are more prone to cataracts, potentially due to reduced resilience to oxidative stress, prolonged exposure to ultraviolet (UV) rays, and an increased likelihood of diabetes or hypertension, all of which are established risk factors for cataracts19,31,32,33. However, there are currently limited studies evaluating the relationship between sleep and cataracts, so more research is needed.
Of note, it has been noticed that there is an interaction between screen time and sleep duration, sleep quality, as well as PA34,35,36. Specifically, prolonged screen time correlates with shortened sleep duration, diminished sleep quality, and reduced PA. Conversely, increased PA and sufficient sleep would naturally allocate individuals less time for screen usage. From this perspective, excessive screen time might indirectly elevate the risk of cataracts by impacting both sleep patterns and PA levels. Furthermore, exposure to blue light from LED (light-emitting diode) screens may have a direct promoting effect on cataracts37,38. In this era of escalating screen use, the relationship between screen time and cataracts merits in-depth exploration through large-scale cohort studies.High blood sugar level (including diabetes) has long been recognized as an important risk factor for cataract occurrence and progression26. The pathogenesis of diabetic cataracts is complex and involves many factors. Long-term experimental studies and clinical observations have put forward a variety of different hypotheses on its pathogenesis. At present, the mainstream theories mainly include three theories. First is the polyol pathway. Aldose reductase is a key enzyme in diabetic cataracts, as it plays an important role in the polyol pathway40. When glucose in aqueous humor reaches saturation, aldose reductase is activated, converting glucose into sorbitol and fructose. Sorbitol can increase the osmotic pressure in the lens after accumulation, causing excessive water to enter the lens, resulting in cataracts41,42. The second is oxidative stress. Lens epithelial cells maintain the stability and transparency of the lens. ROS, however, induces apoptosis of lens epithelial cells, causing diabetic cataract43. The third is non-enzymatic glycation. In the physiological state, only a small amount of glycosylation products (AGE) exists in the lens, but in hyperglycemic environment, AGE increases and accumulates in large quantities, which promotes cataract formation through various pathways44,45.
Notably, in Model 1, we found that ideal dietary status was significantly associated with a lower risk of cataract. In LE8, “diet” refers specifically to the HEI-2015 (Healthy Eating Index-2015) diet, a healthy eating pattern proposed by Dietary Guidelines for Americans. A large cohort study in the UK showed that there was a strong relationship between cataract risk and diet patterns, with a gradual reduction in cataract risk among high meat eaters to low meat eaters, fish eaters (participants who ate fish instead of meat), and vegetarians27. Zhou et al.46 also found that adherence to the healthy eating patterns advocated by HEI-2015 was associated with a reduced risk of age-related cataracts. However, in Model 2, diet was not statistically associated with cataract risk. Considering that the relationship between diet and health is extremely complex, its correlation with cataract needs to be further verified.There are two most notable strengths in this study. One is the novelty (the first to provide a comprehensive assessment of the relationship between LE8 and cataract). The other is that we have identified three modifiable behaviors and factors (PA, sleep, and blood glucose), which have guiding effects on reducing the risk of cataracts for the public.
This study has some limitations. First, LE8 is a comprehensive indicator of cardiovascular health, and its effect on cataracts may be caused by the combination of the eight subitems it contains. Therefore, although we found that the ideal state of the three subitems had a statistically significant protective effect on cataract, this does not necessarily mean that the other subitems do not have an effect on cataract. Second, in this study, diagnosis of cataract is based on self-reported cataract surgeries. While this approach has been reported as a good indicator of the presence of clinically significant cataract, it may underestimate the burden of cataract. Third, due to the limitations of the NHANES database, we did not exclude individuals with other eye diseases, and we call for more well-designed studies to address this issue in the future.
Conclusions
Better CVH is associated with a lower cataract risk. Adhering to the healthy lifestyle recommended by LE8 (especially when it comes to PA, sleep, and blood glucose) may reduce the occurrence of cataracts. Our findings suggest that interventions to prevent cardiovascular diseases hold promise for reducing the disease burden of cataract.
Data availability
The datasets for this study can be found in the National Health and Nutrition Examination Surveys database (https://www.cdc.gov/nchs/nhanes/index.htm).
References
Klein, B. E., Klein, R., Lee, K. E. & Gangnon, R. E. Incidence of age-related cataract over a 15-year interval the Beaver Dam Eye Study. Ophthalmology 115, 477–482. https://doi.org/10.1016/j.ophtha.2007.11.024 (2008).
Modenese, A. & Gobba, F. Cataract frequency and subtypes involved in workers assessed for their solar radiation exposure: A systematic review. Acta Ophthalmol. 96, 779–788. https://doi.org/10.1111/aos.13734 (2018).
Kiziltoprak, H., Tekin, K., Inanc, M. & Goker, Y. S. Cataract in diabetes mellitus. World J. Diabetes 10, 140–153. https://doi.org/10.4239/wjd.v10.i3.140 (2019).
Fang, R. et al. Global, regional, national burden and gender disparity of cataract: Findings from the global burden of disease study 2019. BMC Public Health 22, 2068. https://doi.org/10.1186/s12889-022-14491-0 (2022).
Blindness, G. B. D., Vision Impairment, C., Vision Loss Expert Group of the Global Burden of Disease, S. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: The Right to Sight: An analysis for the Global Burden of Disease Study. Lancet Glob Health 9, e144–e160. https://doi.org/10.1016/S2214-109X(20)30489-7 (2021).
Wang, W. et al. Cataract surgical rate and socioeconomics: A global study. Invest. Ophthalmol. Vis. Sci. 57, 5872–5881. https://doi.org/10.1167/iovs.16-19894 (2016).
Lloyd-Jones, D. M. et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 121, 586–613. https://doi.org/10.1161/CIRCULATIONAHA.109.192703 (2010).
Younus, A. et al. A Systematic review of the prevalence and outcomes of ideal cardiovascular health in US and Non-US populations. Mayo Clin. Proc. 91, 649–670. https://doi.org/10.1016/j.mayocp.2016.01.019 (2016).
Gao, B., Song, S. & Guo, J. Associations between life’s simple 7 and incident depression among adults aged 50 years and older: A 15-year cohort study. Psychiatry Res. 320, 115046. https://doi.org/10.1016/j.psychres.2022.115046 (2023).
**a, X. et al. The age-dependent association of Life’s Simple 7 with transitions across cognitive states after age 60. J. Intern. Med. 294, 191–202. https://doi.org/10.1111/joim.13657 (2023).
De-La-Cruz, N., Shabaneh, O. & Appiah, D. The association of ideal cardiovascular health and ocular diseases among US adults. Am. J. Med. 134, 252–259. https://doi.org/10.1016/j.amjmed.2020.06.004 (2021).
Lloyd-Jones, D. M. et al. Life’s Essential 8: Updating and enhancing the american heart association’s construct of cardiovascular health: A Presidential Advisory From the American Heart Association. Circulation 146, e18–e43. https://doi.org/10.1161/CIR.0000000000001078 (2022).
Li, X., Ma, H., Wang, X., Feng, H. & Qi, L. Life’s Essential 8, genetic susceptibility, and incident cardiovascular disease: A prospective study. Arterioscler. Thromb. Vasc. Biol. 43, 1324–1333. https://doi.org/10.1161/ATVBAHA.123.319290 (2023).
Zhang, J. et al. Relation of Life’s Essential 8 to the genetic predisposition for cardiovascular outcomes and all-cause mortality: Results from a national prospective cohort. Eur. J. Prev. Cardiol. https://doi.org/10.1093/eurjpc/zwad179 (2023).
Nemet, A. Y., Vinker, S., Levartovsky, S. & Kaiserman, I. Is cataract associated with cardiovascular morbidity?. Eye (Lond.) 24, 1352–1358. https://doi.org/10.1038/eye.2010.34 (2010).
Ang, M. J. & Afshari, N. A. Cataract and systemic disease: A review. Clin. Exp. Ophthalmol. 49, 118–127. https://doi.org/10.1111/ceo.13892 (2021).
Zhu, Z. et al. Visual impairment and major eye diseases in chronic kidney disease: The National Health and Nutrition Examination Survey, 2005–2008. Am. J. Ophthalmol. 213, 24–33. https://doi.org/10.1016/j.ajo.2020.01.002 (2020).
Deng, R. et al. Evaluation of systemic medications associated with surgically treated cataract among US adults. Am. J. Ophthalmol. 249, 126–136. https://doi.org/10.1016/j.ajo.2023.01.005 (2023).
Drinkwater, J. J., Davis, W. A. & Davis, T. M. E. A systematic review of risk factors for cataract in type 2 diabetes. Diabetes Metab. Res. Rev. 35, e3073. https://doi.org/10.1002/dmrr.3073 (2019).
Appleby, P. N., Allen, N. E. & Key, T. J. Diet, vegetarianism, and cataract risk. Am. J. Clin. Nutr. 93, 1128–1135. https://doi.org/10.3945/ajcn.110.004028 (2011).
Sacks, F. M. et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N. Engl. J. Med. 344, 3–10. https://doi.org/10.1056/NEJM200101043440101 (2001).
Kisic, B., Miric, D., Zoric, L., Ilic, A. & Dragojevic, I. Antioxidant capacity of lenses with age-related cataract. Oxid. Med. Cell Longev. 2012, 467130. https://doi.org/10.1155/2012/467130 (2012).
Babizhayev, M. A. & Yegorov, Y. E. Reactive oxygen species and the aging eye: Specific role of metabolically active mitochondria in maintaining lens function and in the initiation of the oxidation-induced maturity onset cataract–a novel platform of mitochondria-targeted antioxidants with broad therapeutic potential for redox regulation and detoxification of oxidants in eye diseases. Am. J. Ther. 23, e98-117. https://doi.org/10.1097/MJT.0b013e3181ea31ff (2016).
Sui, X. et al. Influence of cardiorespiratory fitness on lung cancer mortality. Med. Sci. Sports Exerc. 42, 872–878. https://doi.org/10.1249/MSS.0b013e3181c47b65 (2010).
Jiang, H. et al. Physical activity and risk of age-related cataract. Int. J. Ophthalmol. 13, 643–649. https://doi.org/10.18240/ijo.2020.04.18 (2020).
Rim, T. H., Kim, D. W., Kim, S. E. & Kim, S. S. Factors associated with cataract in Korea: A Community Health Survey 2008–2012. Yonsei Med. J. 56, 1663–1670. https://doi.org/10.3349/ymj.2015.56.6.1663 (2015).
Zhou, M., Li, D. L., Kai, J. Y., Zhang, X. F. & Pan, C. W. Sleep duration and the risk of major eye disorders: A systematic review and meta-analysis. Eye (Lond.) 37, 2707–2715. https://doi.org/10.1038/s41433-023-02403-4 (2023).
Leproult, R., Holmback, U. & Van Cauter, E. Circadian misalignment augments markers of insulin resistance and inflammation, independently of sleep loss. Diabetes 63, 1860–1869. https://doi.org/10.2337/db13-1546 (2014).
Parise, B. K. et al. Sleep irregularity and the association with hypertension and blood pressure levels: The ELSA-Brasil study. J. Hypertens. 41, 670–677. https://doi.org/10.1097/HJH.0000000000003392 (2023).
Kanthan, G. L., Mitchell, P., Burlutsky, G. & Wang, J. J. Fasting blood glucose levels and the long-term incidence and progression of cataract—the Blue Mountains Eye Study. Acta Ophthalmol. 89, e434-438. https://doi.org/10.1111/j.1755-3768.2011.02149.x (2011).
Zatechka, D. S. Jr., Kador, P. F., Garcia-Castineiras, S. & Lou, M. F. Diabetes can alter the signal transduction pathways in the lens of rats. Diabetes 52, 1014–1022. https://doi.org/10.2337/diabetes.52.4.1014 (2003).
Kador, P. F., Wyman, M. & Oates, P. J. Aldose reductase, ocular diabetic complications and the development of topical Kinostat((R)). Prog. Retin Eye Res. 54, 1–29. https://doi.org/10.1016/j.preteyeres.2016.04.006 (2016).
Chitra, P. S. et al. Status of oxidative stress markers, advanced glycation index, and polyol pathway in age-related cataract subjects with and without diabetes. Exp. Eye Res. 200, 108230. https://doi.org/10.1016/j.exer.2020.108230 (2020).
Gong, W., Zhu, G., Li, J. & Yang, X. LncRNA MALAT1 promotes the apoptosis and oxidative stress of human lens epithelial cells via p38MAPK pathway in diabetic cataract. Diabetes Res. Clin. Pract. 144, 314–321. https://doi.org/10.1016/j.diabres.2018.06.020 (2018).
Bejarano, E. & Taylor, A. Too sweet: Problems of protein glycation in the eye. Exp. Eye Res. 178, 255–262. https://doi.org/10.1016/j.exer.2018.08.017 (2019).
Kandarakis, S. A., Piperi, C., Topouzis, F. & Papavassiliou, A. G. Emerging role of advanced glycation-end products (AGEs) in the pathobiology of eye diseases. Prog. Retin. Eye Res. 42, 85–102. https://doi.org/10.1016/j.preteyeres.2014.05.002 (2014).
Acknowledgements
We want to acknowledge the participants and investigators of the National Health and Nutrition Examination Surveys.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, Y.M., Z.T. and L.L.; methodology, Z.T., Y.M., L.L. and C.C.; software, Z.T.; validation, Y.M., Z.T. and C.C.; formal analysis, Z.T.; investigation, Y.M. and A.S.; resources, L.L. and C.C.; data curation, Z.T. Y.M. and A.S.; writing—original draft preparation, Z.T. and Y.M.; writing—review and editing, L.L. and C.C.; visualization, Y.M. and Z.T.; supervision, L.L. and C.C.; project administration, Z.T., Y.M. and A.S. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Meng, Y., Tan, Z., Sawut, A. et al. Association between Life’s Essential 8 and cataract among US adults. Sci Rep 14, 13101 (2024). https://doi.org/10.1038/s41598-024-63973-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-63973-1
- Springer Nature Limited