Abstract
N-terminal prohormone of brain natriuretic peptide (NT-proBNP) is an established biomarker for diagnosis of heart failure. The study aims to explore whether known cardiovascular risk factors, including education and income as indicators of socioeconomic position (SEP), may interact with the genetic effect of NT-proBNP-related single nucleotide polymorphisms (SNP) to influence plasma levels of NT-proBNP in a population-based study sample. Information on effect alleles of three SNPs previously reported to be related to NT-proBNP was combined individually for 4,520 participants of the Heinz Nixdorf Recall Study to calculate a genetic risk allele sum score (GRSNT-proBNP). Linear Regression models were used to examine the association of cardiovascular risk factors and GRSNT-proBNP with log-transformed NT-proBNP levels, as well as cardiovascular risk factor by GRSNT-proBNP interactions. The GRSNT-proBNP was associated with NT-proBNP showing 1.13-fold (95% CI 1.10–1.16) higher plasma levels per additional effect allele. Interaction terms included in the regression models gave some indication for interaction of the GRSNT-proBNP with the SEP indicator income as well as with C-reactive protein. In regression models stratified by income quartiles the strongest genetic effect was observed in the third income quartile showing 1.18-fold (95% CI 1.12–1.25) higher average NT-proBNP levels per additional allele compared to the lowest income quartile with 1.08-fold (95% CI 1.01–1.15) higher NT-proBNP levels. The results of the present study indicate that genetic effects of NT-proBNP increasing alleles are stronger in higher SEP groups. This may be due to a stronger influence of non-genetic cardiovascular risk on NT-proBNP in low SEP groups.
Similar content being viewed by others
Introduction
The biological inactive N-terminal prohormone of brain natriuretic peptide (NT-proBNP) and the biological active counterpart brain natriuretic peptide (BNP), initially discovered in brain tissue, are both products of the precursor peptide pro brain natriuretic peptide (proBNP) in cardiomyocytes. They are secreted under mechanical stress conditions (i.e. high ventricular volume) in a 1:1 ratio1. NT-proBNP is established in clinical routine for the diagnosis and evaluation of prognosis in patients with heart failure2. Different etiologies, for instance coronary artery disease, can cause heart failure, resulting in ventricular overload and thereby increasing NT-proBNP blood levels. Therefore, NT-proBNP has also been suggested for cardiovascular risk assessment3 and used to monitor pharmacological treatment success4. Moreover, NT-proBNP has been proposed as a biomarker for other diseases such as bronchopulmonary dysplasia after birth5, protein energy wasting in hemodialysis6 and cancer7,8.
However, NT-proBNP levels are influenced by risk factors, such as gender, age, antihypertensive medication (i.e., beta-blockers), renal insufficiency, obesity and testosterone levels9,10,11,12,13. Furthermore, indicators of socioeconomic position (SEP) (e.g., education, income, area deprivation) have been identified to be inversely associated with NT-proBNP levels14,15, yet there is limited research in this area. These clinical and social aspects have to be taken into account when interpreting NT-proBNP blood levels.
Recent genome-wide association studies have identified three single nucleotide polymorphism (SNP) alleles associated with increased NT-proBNP levels16. Like other common polygenetic risks for complex traits, main effects of the individual SNP alleles on NT-proBNP have been quite small16, indicating possible gene by environment interactions. It is assumed that SEP influences cardiovascular risk via its impact on the distribution of cardiovascular risk factors (CRF), meaning that SEP indicators can serve as proxy markers describing overall risk-related environments. It may then be hypothesized that SEP affects NT-proBNP by having an impact on the expression of NT-proBNP-related genes via its influence on CRFs17,18.
The aim of the present study was to explore whether a genetic risk allele sum score of NT-proBNP increasing alleles (GRSNT-proBNP) may interact with indicators of SEP (i.e., education, household income) and traditional CRFs (i.e., total cholesterol, high-density lipoprotein, low-density lipoprotein, triglycerides, C-reactive protein, serum glucose, HBA1C, body mass index, blood pressure, physical activity, diabetes mellitus, smoking status and coronary artery calcification) to influence plasma levels of NT-proBNP in a population-based study sample.
Methods
Study population
Baseline data of the Heinz Nixdorf Recall Study was used. Details of the study have been described elsewhere19. In brief, this ongoing population-based cohort study, starting in December 2000, included 4814 men and women from the German cities Essen, Bochum und Mülheim, aged 45 to 75 years. Participants were selected randomly by drawing a sample of the local resident registries, yielding a baseline response proportion of 55.8%20.
Data acquisition
NT-proBNP was measured from frozen blood plasma, obtained from blood samples taken at study baseline, which were centrifuged and aliquoted for storage at -80 °C. Roche Modular E170 Assay (Roche Diagnostics, Mannheim, Germany) was used with the lowest analytical sensitivity reached at 5 pg/ml21,22.
Education and income were used as indicators of SEP at study baseline. Education was defined using the International Standard Classification of Education (ISCED-97)23 and then categorized into three education groups (≤ 10 years, 11–13 years, ≥ 14 years of education) using the lowest education groups as reference for statistical analysis. Income was measured as the monthly household equivalent income in Euro calculated by dividing the total household net income by a weighting factor for each household member according to the OECD scale24. Calculations were performed using sex-specific income quartiles using the lowest quartile as reference.
Total cholesterol, high density lipoprotein (HDL) cholesterol and triglycerides in blood serum samples were determined using standard enzymatic assays. Low density lipoprotein (LDL) cholesterol was assessed via direct measurement and calculation using the Friedewald equation. Body Mass Index (BMI) was calculated by dividing measured baseline weight by squared baseline height. Blood glucose was determined by hexokinase reaction. High sensitivity C-reactive protein (CRP) and HbA1C were measured by nephelometry (BN-II System, Dade-Behring Inc.). Blood pressure was assessed using the mean of the second and third of three measurements. Oscillometric blood pressure measurements were performed with an Omron HEM-705CP on sitting participants. Physical activity was assessed in computer-assisted face-to-face interviews and dichotomized as weekly physical exercise versus no weekly physical exercise. Smoking status was assessed in computer-assisted face-to-face interviews and dichotomized into current and former smokers versus never-smokers. Coronary artery calcification (CAC) was measured using EB-CT (electron beam computed tomography) with a GE Imatron scanner and the Agaston score was then computed as a measure of total CAC defined as the sum of the area (in mm2) of each detectable focus in the epicardial coronary system multiplied by its computed tomography density25. Glomerular filtration rate (GFR) was calculated using the modification of diet and renal disease formula (MDRD). Diabetes mellitus was defined as having blood glucose levels ≥ 200 mg/dl, fasting glucose > 125 mg/dl, or reported diabetes mellitus diagnosis or medication. Prevalent stroke and coronary heart disease at study baseline were assessed in computer-assisted face-to-face interviews.
Genetic data
Selection of SNPs was based on the genome-wide association study of Johansson et al.16, in which three SNPs (rs198389 near NPPB; rs13107325 near SLC39A8; rs10858894 near POC1B/GALNT4) were robustly associated with NT-proBNP blood levels (Table 1).
Lymphocyte DNA of Heinz Nixdorf Recall Study participants was isolated from EDTA anti-coagulated venous blood using the Chemagic Magnetic Separation Module I (Chemagen, Baesweiler, Germany). Genoty** was performed using the Infinium Global Screening Array (GSA chip) by Illumina. For SNP rs11105306, originally reported by Johannson et al.16, the proxy SNP rs10858894 in perfect linkage disequilibrium (r2 = 1.0; 1000 Genomes CEU population) was used for statistical analysis. An unweighted genetic risk allele sum score (GRSNT-proBNP) was calculated for each participant by adding the number of NT-proBNP increasing effect alleles. No deviation from Hardy–Weinberg equilibrium (p > 0.001) was detected using an exact two-sided test.
Statistical analyses
Genetic data and information on NT-proBNP were available for 4520 participants of the Heinz Nixdorf Recall Study (Fig. 1). Participants with missing data on SEP indicators and other CRFs were only excluded from the respective analyses.
To normalize the distribution of NT-proBNP a log-transformation was applied. Effect size estimates were presented back-transformed (exp[β]). Main effects of the three SNP effect alleles, the GRSNT-proBNP, SEP indicators and CRFs on NT-proBNP were assessed by fitting age- and sex-adjusted linear regression models separately for each variable. Interaction was explored by additionally including GRSNT-proBNP*SEP/CRF interaction terms and SEP indicator/CRF main effects in age- and sex-adjusted linear regression models separately for each SEP indicators and CRF (i.e., log(NT-proBNP) = age + sex + GRSNT-proBNP + SEP/CRF + GRSNT-proBNP*SEP/CRF). SEP indicators were included as dummy variables in the regression models with the first income quartile and lowest education group as reference category, respectively. The GRSNT-proBNP effect was also calculated stratified by groups of SEP indicators and those CRFs showing indication for interaction. Sensitivity analysis was performed by including only participants without stroke and coronary artery disease at baseline and with a GFR of > 30 ml/min/1.73m2. All statistical analyses were performed using the statistical software package R, version 3.5.326.
Ethics approval and consent to participate
Written informed consent was retrieved from all participants and the study was approved by the ethics committee of the University Duisburg-Essen. The study complies with the quality management system DIN ISO 9001:2000. The study was conducted according to the guidelines and recommendations for ensuring Good Epidemiological Practice (https://www.dgepi.de/assets/Leitlinien-und-Empfehlungen/Recommendations-for-good-Epidemiologic-Practice.pdf).
Results
Median NT-proBNP plasma levels of 2263 male and 2257 female participants, mean aged 60 years, were 70.0 pg/ml, with women having higher median NT-proBNP levels (86.0 pg/ml, IQR 52.0–147.0) than men (54.0 pg/ml, IQR 31.0–109.0) in the study population (Table 2). Indicators of SEP showed sex-differences with women having a lower median income compared to men (1313€ vs. 1520€) and on average less years of education. The mean number of GRSNT-proBNP effect alleles did not differ between women and men (2.6 ± 1.0 vs. 2.5 ± 1.0) in the study population.
Per additional effect allele of the GRSNT-proBNP the average NT-proBNP level was 1.13-fold (95% CI 1.10–1.16) higher (Table 3). Each effect allele of the three selected SNPs showed directional consistent effects as previously reported. The strongest effect was observed for rs13107325 with an exp(β) of 1.21 (95% CI 1.12–1.30) per additional effect allele. Using the first income quartile as reference, NT-proBNP levels decreased with increasing income (Table 3). In the fourth quartile the effect strength of income showed an exp(β) of 0.90 (95% CI 0.83–0.97) compared to the first income quartile. No association between education and NT-proBNP was observed. Positive associations with NT-proBNP were observed for CRP, systolic blood pressure, no physical activity, diabetes mellitus, smoking and coronary artery calcification. Negative associations were observed for total cholesterol and LDL.
Results of the interaction analysis including GRSNT-proBNP by SEP/CRF interaction terms gave some indication for a positive interaction between GRSNT-proBNP and income for comparing the first and the third income quartile (exp(βGRSxIncome) = 1.10, 95% CI 1.01–1.19) as well as between GRSNT-proBNP and CRP (exp(βGRSxCRP) = 1.03, 95% CI 1.01–1.06) on NT-proBNP (Table 4). However, after including income and the related income interaction terms in the regression model containing CRP and the GRSNT-proBNP by CRP interaction term, the effect size estimate of the observed GRSNT-proBNP by CRP interaction term dropped to 1.00 (95% CI 0.96–1.04), while the effect size for GRSNT-proBNP by income interaction terms remained virtually the same.
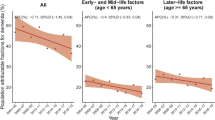
The effect of the GRSNT-proBNP stratified by income quartiles showed an increase of the genetic effect on NT-proBNP with increasing income quartiles, except for the fourth income quartile (Fig. 2). The strongest effect of GRSNT-proBNP was observed in the third income quartile showing an exp(β) of 1.18 (95% CI 1.12–1.25) compared to an exp(β) of 1.08 (95% CI 1.01–1.15) in the first income quartile. The effect of the GRSNT-proBNP stratified by education groups also showed an increase in the strength of the genetic effect with increasing years of education (Fig. 2). However, compared to the stratified analysis using income quartiles, differences in the genetic effect size estimates between education groups were less strong. After calculating the effect of the GRSNT-proBNP on NT-proBNP stratified by CRP quartiles, only small differences in effect size were observed lacking a general trend of effects across CRP strata (Fig. 2). However, the effect size estimate of rs13107325 effect alleles on NT-proBNP show an increasing trend across CRP quartiles in the single SNP analyses (Fig. S1). Single SNP effects on NT-proBNP stratified by income and education showed that for income the effect of all three SNPs was again strongest in the third quartile with the strongest effect across all SNPs for rs13107325 (exp(β) of 1.35 [95% CI 1.14–1.60]), while for education again smaller differences in the genetic effect were observed between groups compared to income quartiles (Fig. S1).
After including only participants without stroke, coronary artery disease and a GFR > 30 ml/min/1.73 m2 in a sensitivity analysis of the main results, only small changes in effect size estimates were observed for the association of SEP indicators and CRFs with NT-proBNP (Table 5). Effect size estimates for the GRSNT-proBNP by SEP and GRSNT-proBNP by CRP interaction effect were slightly smaller compared to the main analyses population (Table 6). In a single SNP analysis, the strongest indication for interaction was observed for rs13107325 interaction with CRP (Table S1).
Discussion
The present study aimed to explore the impact of established CRFs and SEP indicators on the effect of a GRSNT-proBNP in a population-based cohort, including three SNPs previously reported to be associated with NT-proBNP blood levels. The observed association between the GRSNT-proBNP and NT-proBNP levels was directionally consistent, replicating the findings of Johansson et al.16, as the cumulative and individual effects of the selected SNPs on NT-proBNP were demonstrated in an independent study sample with rs13107325 reaching genome-wide significance. However, there was heterogeneity of the effect strength across groups of different household income used as SEP indicator. Groups with higher SEP experienced stronger genetic effects compared to groups with lower SEP. Indication for a positive GRSNT-proBNP by CRP interaction was also observed suggesting stronger genetic effects with increasing CRP. However, after adjustment for confounding by income, the GRSNT-proBNP by CRP interaction disappeared, while the GRSNT-proBNP by income interaction was still present. Overall, results were not strongly affected by prevalent cardiovascular disease or GFR.
In a previous study, social inequality in NT-proBNP levels has already been reported15, which may be explained by a higher prevalence of NT-proBNP-related health risks in lower SEP groups. In a twin study by Johnson and Krueger17,27 it has been observed that the genetic influence on overall measures of physical health decreased with increasing income. This may be interpreted as an impact of non-genetic risk factors associated with SEP on the expression of adverse effects of health-related genetic variants. However, the direction of this effect modification is not in line with the results of the study presented here and stronger genetic effects on NT-proBNP in groups of high SEP have to be explained by a different mechanism. One possible explanation may be that the effect of the selected SNPs on NT-proBNP becomes negligible in the presence of much stronger effects of non-genetic risk factors associated with SEP, while in high SEP groups with lower rates of health risks a greater direct influence of genetic factors on NT-proBNP can be observed. As proposed in previous studies, cardiovascular diseases are more prevalent in lower SEP groups28. It is hypothesized that absolute NT-proBNP levels may compensate cardiovascular risk due to a mechanism that regulates cardiac preload, as NT-proBNP reduces blood pressure and preload via natriuresis29,30. Smaller genetic effects on NT-proBNP in groups of low SEP might be a result of CRFs inducing a regulatory NT-proBNP increase that outweighs the genetic effect on NT-proBNP. Thus, groups of high SEP may experience stronger genetic effects on NT-proBNP, because cardiovascular risks are less prevalent in those groups. Moreover, it may be speculated that people with genetically incremented NT-proBNP levels might experience a protective factor against certain cardiovascular diseases, for instance heart failure31.
Strengths of the current study are the population-based design and the use of a range of established CRFs for analysis. However, the cross-sectional study design is a limitation as individuals who already experienced a fatal cardiovascular event could not be included in the analyses population. Another limitation is that the study results may not be transferable to other ethnic groups as participants are mainly of Caucasian origin.
In conclusion, the results of the present study indicate that genetic effects of NT-proBNP increasing alleles are stronger in higher SEP groups. This may be due to a stronger influence of non-genetic cardiovascular risk on NT-proBNP in low SEP groups. Any interactions between NT-proBNP genetic effects and traditional CRFs may be confounded by SEP interactions.
Data availability
Due to data security reasons (i.e., data contain potentially participant identifying information), the Heinz Nixdorf Recall Study does not allow sharing data as a public use file. However, others can access the data used upon request, which is the same way the authors of the present paper obtained the data. Data requests can be addressed to: recall@uk-essen.de.
References
Semenov, A. G. et al. Processing of pro-B-type natriuretic peptide: Furin and corin as candidate convertases2. Clin. Chem. 56(7), 1166–1176 (2010).
Lemos, J. A. D., Omland, T. & Hall, C. The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N. Engl. J. Med. 8, 1–10 (2001).
Willeit, P. et al. Natriuretic peptides and integrated risk assessment for cardiovascular disease: An individual-participant-data meta-analysis. Lancet Diabetes Endocrinol. 4(10), 840–849 (2016).
Savarese, G. et al. Natriuretic peptide-guided therapy in chronic heart failure: A meta-analysis of 2,686 patients in 12 randomized trials. PLoS ONE 8(3), e58287 (2013).
Sellmer, A. et al. N-terminal Pro-B type natriuretic peptide as a marker of bronchopulmonary dysplasia or death in very preterm neonates: A cohort study. PLoS ONE 10, 10 (2015).
Ikeda, M., Honda, H., Takahashi, K., Shishido, K. & Shibata, T. N-terminal pro-B-type natriuretic peptide as a biomarker for loss of muscle mass in prevalent hemodialysis patients. PLoS ONE 11(11), e0166804 (2016).
Ohsaki, Y., Gross, A. J., Le, P. T., Oie, H. & Johnson, B. Human small cell lung cancer cells produce brain natriuretic peptide. OCL. 56(2), 155–159 (1999).
Popat, J., Rivero, A., Pratap, P. & Guglin, M. What is causing extremely elevated amino terminal brain natriuretic peptide in cancer patients?. Congest. Heart Fail. 19(3), 143–148 (2013).
Luchner, A. et al. Long-term pattern of brain natriuretic peptide and N-terminal pro brain natriuretic peptide and its determinants in the general population: contribution of age, gender, and cardiac and extra-cardiac factors. Eur. J. Heart Fail. 15(8), 859–867 (2013).
Tsai, Y.-C. et al. The interaction between N-terminal pro-brain natriuretic peptide and fluid status in adverse clinical outcomes of late stages of chronic kidney disease. PLoS ONE 13(8), e0202733 (2018).
Zheng, L. et al. Impact of body mass index on plasma N-terminal ProB-type natriuretic peptides in chinese atrial fibrillation patients without heart failure. PLoS ONE 9(8), e105249 (2014).
Wirth, J. et al. Relationship between N-terminal pro-brain natriuretic peptide, obesity and the risk of heart failure in middle-aged German adults. PLoS ONE 9(11), e113710 (2014).
Saenger, A. K., Dalenberg, D. A., Bryant, S. C., Grebe, S. K. & Jaffe, A. S. Pediatric brain natriuretic peptide concentrations vary with age and sex and appear to be modulated by testosterone. Clin Chem. 55(10), 1869–1875 (2009).
Vart, P. et al. SES, heart failure, and N-terminal Pro-b-type natriuretic peptide: The atherosclerosis risk in communities study. Am. J. Prev. Med. 54(2), 229–236 (2018).
Rudman, M. et al. Socioeconomic position is associated with N-terminal pro brain natriuretic peptide (NT proBNP): Results of the population based Heinz Nixdorf recall study. PLoS ONE 16(8), e0255786 (2021).
Johansson, Å. et al. Genome-wide association and Mendelian randomization study of NT-proBNP in patients with acute coronary syndrome. Hum. Mol. Genet. 25(7), 1447–1456 (2016).
Johnson, W. et al. Education reduces the effects of genetic susceptibilities to poor physical health. Int. J. Epidemiol. 39(2), 406–414 (2010).
Börge, S. et al. Socioeconomic status interacts with the genetic effect of a chromosome 9p21.3 common variant to influence coronary artery calcification and incident coronary events in the Heinz Nixdorf recall study (risk factors, evaluation of coronary calcium, and lifestyle). Circ. Cardiovasc. Genet. 10(2), e001441 (2017).
Schmermund, A. et al. Assessment of clinically silent atherosclerotic disease and established and novel risk factors for predicting myocardial infarction and cardiac death in healthy middle-aged subjects: Rationale and design of the Heinz Nixdorf RECALL Study. Am. Heart J. 144(2), 212–218 (2002).
Stang, A. et al. Baseline recruitment and analyses of nonresponse of the Heinz Nixdorf Recall Study: Identifiability of phone numbers as the major determinant of response. Eur. J. Epidemiol. 20(6), 489–496 (2005).
Kara, K. et al. B-type natriuretic peptide: Distribution in the general population and the association with major cardiovascular and coronary events: The Heinz Nixdorf Recall Study. Clin. Res. Cardiol. 103(2), 125–132 (2014).
Kara, K. et al. NT-proBNP is superior to BNP for predicting first cardiovascular events in the general population: The Heinz Nixdorf Recall Study. Int. J. Cardiol. 183, 155–161 (2015).
UNESCO Institute for Statistics. International Standard Classification of Education ISCED 1997 (UNESCO-UIS, 2006).
Hagenaars, A., de Vos, K. & Zaidi, M. A. Poverty Statistics in the Late 1980s (Office for Official Publications of the European Communities, 1994).
Agatston, A. S. et al. Quantification of coronary artery calcium using ultrafast computed tomography. J. Am. Coll. Cardiol. 15(4), 827–832 (1990).
R FAQ. https://cran.r-project.org/doc/FAQ/R-FAQ.html#Citing-R. Accessed 16 Oct 2020.
Johnson, W. & Krueger, R. F. Genetic effects on physical health: Lower at higher income levels. Behav. Genet. 35(5), 579–590 (2005).
Raimund, E. et al. Subclinical coronary atherosclerosis predicts cardiovascular risk in different stages of hypertension. Hypertension 59(1), 44–53 (2012).
Chow, S. L. et al. Role of biomarkers for the prevention, assessment, and management of heart failure: A scientific statement from the American Heart Association. Circulation 135(22), e1054–e1091 (2017).
Del Greco, M. F. et al. Genome-wide association analysis and fine map** of NT-proBNP level provide novel insight into the role of the MTHFR-CLCN6-NPPA-NPPB gene cluster. Hum. Mol. Genet. 20(8), 1660–1671 (2011).
van der Ende, M. Y., Said, M. A., van Veldhuisen, D. J., Verweij, N. & van der Harst, P. Genome-wide studies of heart failure and endophenotypes: Lessons learned and future directions. Cardiovasc. Res. 114(9), 1209–1225 (2018).
Acknowledgements
We are indebted to all study participants and to both the dedicated personnel of the study center of the Heinz Nixdorf Recall study and to the investigative group, in particular to U. Slomiany, U. Roggenbuck, E. M. Beck, A. Öffner, S. Münkel, R. Peter, and H. Hirche. Advisory Board: Meinertz T., Hamburg, Germany (Chair); Bode C., Freiburg, Germany; deFeyter P. J., Rotterdam, Netherlands; Güntert B, Halli, Austria; Gutzwiller F., Bern, Switzerland; Heinen H., Bonn, Germany; Hess O., Bern, Switzerland; Klein B., Essen, Germany; Löwel H., Neuherberg, Germany; Reiser M., Munich, Germany; Schmidt G., Essen, Germany; Schwaiger M., Munich, Germany; Steinmüller C., Bonn, Germany; Theorell T., Stockholm, Sweden; Willich S. N., Berlin, Germany.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors thank the Heinz Nixdorf Foundation [Chairman: Martin Nixdorf; Past Chairman: Dr jur. Gerhard Schmidt (†)], for their generous support of this study. Parts of the study were also supported by the German Research Council (DFG) [DFG project: EI 969/2-3, ER 155/6-1;6-2, HO 3314/2-1;2-2;2-3;4-3, INST 58219/32-1, JO 170/8-1, KN 885/3-1, PE 2309/2-1, SI 236/8-1;9-1;10-1,], the German Ministry of Education and Science [BMBF project: 01EG0401, 01GI0856, 01GI0860, 01GS0820_WB2-C, 01ER1001D, 01GI0205].
Author information
Authors and Affiliations
Contributions
B.S. formed the study concept. K.K., A.A.M., N.D., R.E., and K.H.J. contributed to data acquisition. E.M., M.F. and B.S. performed the statistical analysis. E.M. and B.S. drafted the manuscript. All authors contributed to the interpretation of results, revised the paper draft and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Matusch, E., Frank, M., Kara, K. et al. Impact of socioeconomic and cardiovascular risk factors on the effect of genetic variants associated with NT-proBNP. Sci Rep 12, 15560 (2022). https://doi.org/10.1038/s41598-022-19821-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-19821-1
- Springer Nature Limited