Abstract
Growing evidence supports the hypothesis that type 2 diabetes (T2D) increases the risk of develo** dementia. Experimental evidence from mouse models demonstrates that the induction of T2D/insulin resistance (IR) can promote the accumulation of Alzheimer’s disease (AD) pathological features. However, the association of T2D with pathological and clinical phenotypes in humans is unclear. Here we investigate the relationship of indices of IR (HOMA-IR) and pancreatic β-cell function (HOMA-B) with cognitive performance across several domains (Verbal/Visual Episodic Memory, Executive Function, Language and a measure of Global cognition) and AD biomarkers (CSF Aβ42, T-tau/P-tau, hippocampal volume and neocortical Aβ-amyloid burden). We reveal that HOMA-IR (p < 0.001) incrementally increases across diagnostic groups, becoming significantly elevated in the AD group compared with cognitively normal (CN) adults. In CN adults, higher HOMA-IR was associated with poorer performance on measures of verbal episodic memory (p = 0.010), executive function (p = 0.046) and global cognition (p = 0.007), as well as with higher CSF T-tau (p = 0.008) and P-tau (p = 0.014) levels. No association was observed with CSF Aβ or imaging modalities. Together our data suggest that IR may contribute to reduced cognitive performance and the accumulation of CSF tau biomarkers in cognitively normal adults.
Similar content being viewed by others
Introduction
Epidemiological studies indicate that Type 2 diabetes (T2D) is associated with an increased risk of dementia1,2,3,4,5. Clinical studies using cross-sectional designs support this association by showing that cognition is worse in patients with T2D as compared to matched controls without T2D6, 7. Furthermore, studies of structural magnetic resonance imaging (MRI) show that in T2D cognitive impairment is associated with greater levels of vascular lesions as well as with brain atrophy6,7,8,9,10. Prospective MRI studies also show that in T2D brain atrophy occurs at faster rates than in normal ageing11, 12, suggesting that T2D accelerates neurodegeneration.
Animal studies provide additional evidence to show that inducing T2D/insulin resistance (IR) can promote the pathological changes characteristic of Alzheimer’s disease (AD), specifically accumulation of amyloid-beta (Aβ) and tau (see review ref. 13). These studies also implicate common inflammatory or oxidative stress pathways that link these two chronic diseases of ageing (see review ref. 14). However, the association between cognition and AD pathology in human studies and the stage of AD progression where IR has greater impact remains unclear. Evidence to date using Positron emission tomography (PET) studies have so far been inconclusive.
In AD, PET studies of cerebral glucose metabolism (18F-deoxyglucose PET: FDG-PET) and Aβ deposition (e.g. C11-Pittsburg compound B-PET: PiB-PET) show that reduced neuronal glucose metabolism and increased levels of neocortical Aβ accumulation are features that occur early in the disease (see review ref. 15). A small number of cohort studies have investigated the relationship between these imaging markers of AD and T2D. A cross-sectional study in the population-based Mayo Clinic Study of Ageing assessed cerebral glucose metabolism (FDG-PET) and Aβ deposition (PiB-PET) in healthy older and cognitively normal (CN) adults and older people with T2D. The study showed that compared to the controls, those with T2D displayed cerebral hypometabolism, particularly in those regions severely affected in AD, but no differences in neocortical amyloid load16. In the Baltimore, longitudinal study of Ageing (BLSA), no association was observed between measures of peripheral IR or glucose tolerance and neocortical Aβ load (in a PiB-PET scanned cohort) or other pathological features of AD in post-mortem brain17. More recently in the Alzheimer’s Disease Neuroimaging Initiative (ADNI) study, no association was shown betweenT2D and accumulation of neocortical Aβ load (PiB-PET) or increases in CSF Aβ4210. Instead, T2D was associated with lower cortical thickness an increase in CSF total tau (T-Tau) and phosphorylated tau (P-tau). Together, these findings suggest that IR/T2D is not associated with cerebral accumulation of Aβ but with other hallmarks of the disease. However, in a recent cross-sectional study, Aβ deposition was associated with a higher Homeostatic Model Assessment of IR (HOMA-IR) in late-middle aged, normoglycaemic cognitively normal participants18. The conflicting results in the current literature may be in part due to demographic differences in populations (e.g. age, clinical staging of disease and disease progression) and study design. Further, recent meta-analyses suggest that sex can also mediate T2D associations with dementias and associated co-morbidities, such as stroke19,20,21. Thus, the relationship between IR and clinical and pathological features of the early stages of AD, and sex specific effects, requires further study, particularly in normoglycaemic individuals and prior to the onset of cognitive impairment.
In addition to IR, β-cell hyperactivity and dysfunction and subsequent hyperinsulinemia also contribute to hyperglycaemia and T2D (see review ref. 22). Further, recent evidence indicates β-cell dysfunction in AD rodent models23, 24 and that Aβ and Tau have been shown to accumulate in human post-mortem pancreatic tissue in T2D25, possibly contributing to β-cell dysfunction. Despite this evidence, there is a lack of literature investigating pancreatic β-cell activity (HOMA-B) on cognition and AD related pathology.
The overall aim of this study was to investigate if assessments of IR (HOMA-IR) or pancreatic β-cell function (HOMA-B) are altered across diagnostic groups and ascertain their associations with pathological and clinical expressions of AD in the well characterised Australian Imaging Biomarker and Lifestyle (AIBL) study. We hypothesised that HOMA-IR and HOMA-B are altered across diagnostic groups and are associated with poorer cognitive performance and higher burdens of neuroimaging/CSF biomarker load in cognitively normal participants.
Results
Clinical and cognitive descriptive data for the diagnostic groups [cognitively normal adults (CN), mild cognitive impairment (MCI) and AD] are presented in Tables 1 and 2, respectively. A significant difference in age and frequency of the Apolipoprotein E (APOE) ε4 allele was observed across all diagnostic groups (Table 1), with AD and MCI being older and having a significantly higher APOE ε4 frequency compared to CN (p < 0.001). Significant differences between groups for pathological features and cognitive measures confirmed a clear differentiation between diagnostic groups (Table 2).
Relationships between T2D markers and clinical diagnosis
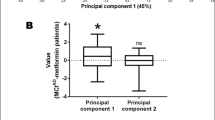
Serum glucose levels were increased significantly in AD and MCI compared with CN (p = 0.014) (AD > MCI > CN), and a non-significant trend was observed for serum insulin HOMA-IR, but not for HOMA-B (Table 1). These group differences in the HOMA indices became statistically significant after co-varying for BMI, sex, diabetes, use of diabetes medication, smoking, age and APOE genotype. HOMA-IR (Fig. 1A) was significantly increased across diagnostic groups (ANCOVA, F = 8.656, p < 0.001) with post-hoc analysis showing a significant increase in HOMA-IR in the AD group (Bonferroni p < 0.001) compared to CN. A clinical group difference was also observed for HOMA-B (Fig. 1B; F = 4.564, p = 0.011), though between the MCI and CN groups (Bonferroni p = 0.028). In both cases, significant differences were only observed in females (HOMA-IR, F = 6.989 p = 0.001; HOMA-B, F = 5.575 p = 0.004) but not males (HOMA-IR, F = 2.603 p = 0.075; HOMA-B, F = 0.911 p = 0.403). In females HOMA-IR was still only observed to be different in the AD group (Bonferroni p = 0.001) compared to CN, whilst HOMA-B, was significantly lower in CN compared to both the MCI (Bonferroni p = 0.041) and AD (Bonferroni p = 0.017) groups.
HOMA-IR (A) and HOMA-B (B) at baseline within the clinical classifications of AIBL: *HOMA-IR and HOMA-B represented as Estimated Marginal Means ( ± SEM) of Box-Cox transformed raw data. Univariate analysis was performed covarying for BMI, sex, %diabetes, %diabetes medication, %hypertension, smoking, age and APOE ε4 (HOMA-IR, F = 8.656, p < 0.001; HOMA-B, F = 4.564, p = 0.011). Presented p-values are calculated using Post-hoc Bonferoni analysis.
HOMA-IR is associated with cognitive performance and CSF biomarkers
A significant inverse relationships were observed (Table 3) between HOMA-IR and the cognitive composites, verbal episodic memory (β = −0.65, p = 0.010), executive functioning (β = −0.48, p = 0.046) and global composite (β = −0.68, p = 0.007). Significant positive relationships were also observed with CSF T-tau (β = 830.2, p = 0.008) and P-tau (β = 95.9, p = 0.014). Increases in HOMA-B were only observed to be associated with reductions in executive functioning (β = −0.095, p = 0.044) and the global composite (β = −0.011, p = 0.043). Stratification by sex (Table 4, female; Table 5
, male) revealed that prior significant associations held between HOMA-IR and verbal episodic memory (β = −0.63, p = 0.046), executive function (β = −0.61, p = 0.042), the global cognitive composite (β = −0.79, p = 0.014) and both CSF T-tau (β = 639.5, p = 0.048) and P-Tau (β = 93.4, p = 0.031) in females. No significant associations were observed for either HOMA-IR or HOMA-B in males.
Discussion
Our findings demonstrate modest yet significant differences, in both HOMA-IR and HOMA-B, between the clinical classifications of AD, MCI and CN within the AIBL cohort, after covarying for potential confounding variables. Within clinical classifications, compared to the CN group, the AD group had higher HOMA-IR. These findings are consistent with previous reports showing that the prevalence of IR is greater in MCI/AD patients than controls26,27,28. However, in the current study HOMA-B was increased only in the MCI group, suggesting an increase in β-cell function/insulin secretion in this group, an observation consistent with the observed trend towards increasing absolute insulin levels across groups. This may represent a response to control increasing glucose levels during disease progression29, which was also observed in this study. Overall, these initial findings suggested that increased β -cell function/insulin secretion is associated with cognitive impairment, at least in non-demented adults. However, in the absence of overt cognitive impairment (i.e. CN group), compared to HOMA-IR, HOMA-B had no or weak associations with functioning of cognitive domains. This suggests that changes in insulin sensitivity is the stronger, earlier contributor to impairments in cognition. Longitudinal analysis in the cognitively normal that do or do not show clinical disease progression may provide further support for this notion.
We also observed sex differences in levels of HOMA-IR and HOMA-B between diagnostic groups, where upon stratification by sex, the increases observed in the MCI or AD groups were only observed in females. These findings are consistent with outcomes from meta-analyses which indicate women with T2D are at higher risk of stroke and dementia compared to men with T2D19,20,21 and may be a consequence of several factors. For example, studies in different ethnic groups have suggested that age related increases in the prevalence of metabolic syndrome are greater in women then in men (see review ref. 30). Similarly, impaired glucose tolerance has been reported to be more prevalent in older women than men, although impaired fasting glycaemia more prevalent in men31. Further, changes in hormonal status also contribute to an age-associated increased prevalence of metabolic syndrome in women32 and may be driven by androgen/oestrogen imbalances during the peri-menopausal period68. As part of the clinical pathology assessment, fasting plasma insulin (FPI) and fasting plasma glucose levels (FPG) were assessed. The stated reference ranges are the ranges established in the clinical pathology laboratory in accordance with the national guidelines (http://www.nata.asn.au/, http://www.health.gov.au/npaac). The FPI and FPG were used to calculate values of Homeostatic modelling assessment (HOMA). The HOMA model is often used in cross-sectional and longitudinal studies to estimate insulin sensitivity and pancreatic β-cell functioning as alternatives to more direct assessments such as glucose clam** or acute insulin response, which are not practical in large cohort studies (see review ref. 70). Initially, comparisons of two methods of HOMA was performed; the HOMA1 (“original method”) using equations developed by Mathews and colleagues71 and the HOMA2 “the computer model”) developed by Levy and colleagues72. These models and the differences between them have been extensively discussed elsewhere70. HOMA1 was calculated using the following: HOMA-IR = (FPI x FPG)/22.5; HOMA-B (%) = (20x FPI)/(FPG = 3.5) to estimate IR and β-cell functioning respectively. HOMA2 was calculated from a Microsoft Excel macro accessed via the Oxford University website (www.dtu.ox.ac.uk/homacalculator/). Pearson’s correlation analysis of the data generated from HOMA1 and HOMA2 analysis revealed a strong significant correlation between these indices (HOMA1-IR vs HOMA2-IR, r = 0.976, p < 0.001; HOMA1-B vs HOMA2 B, r = 0.717, p < 0.0001), indicating suitability of both methods for this data set. However, HOMA1 was utilised as it is the most commonly used method in large cohort cross-sectional or longitudinal studies. All reference to HOMA in this report reflects HOMA1 calculated indices.
DNA was extracted and APOE genotype determined previously described73. Briefly, QIAamp DNA Blood Maxi Kits (Qiagen, Hilden, Germany) were used per manufacturer’s instructions to extract from whole blood. APOE genotype was determined from two separate TaqMan® (Thermo Fisher Scientific, Waltham, MA) genoty** assays for the single nucleotide polymoprhisms rs7412 (assay ID: C____904973_10) and rs429358 (assay ID: C___3084793_20). TaqMan® genoty** assays were performed on a QuantStudio 12 K Flex™ Real-Time-PCR systems (Thermo Fisher Scientific, Waltham, MA) using the TaqMan® GTXpress™ Master Mix (Thermo Fisher Scientific, Waltham, MA) methodology as per manufacturer instructions. APOE carrier status was defined by the presence (1 or 2 copies; ε4 + ) or absence (0 copies; ε4−) of the APOE ε4 allele.
CSF collection and Aβ42, T-tau, and P-tau181P quantitation were performed as previously described74. Briefly, approximately 10–14 ml of CSF was collected in the morning by routine lumbar puncture after overnight fasting directly into one 15 ml polypropylene tube (Greiner Bio-One188271), employing a protocol like that recommended by the Alzheimer’s Biomarkers Standardization Initiative75. All CSF samples for analysis were taken from aliquots prepared and stored as previously described74 and thawed at time of assay. All CSF samples were analyzed in duplicate using the enzyme-linked immunosorbent assay (ELISA): INNOTEST Aβ-amyloid (1–42; Aβ42), INNOTEST hTAU Ag (T-tau), and INNOTEST Phospho-tau (P-tau; 181 P; P-tau181P) (Innogenetics, Ghent, Belgium) per published standard methods. Mean intra-assay coefficients of variation for these assays are as previously published74. This study reports on data from 66 study participants from whom CSF was taken at the baseline time point of the AIBL study.
Brain Imaging
Data was available at baseline from a total of 379 AIBL participants (262 CN, 69 MCI, 48 AD) who underwent Aβ-amyloid imaging with positron emission tomography using either 11C-Pittsburgh Compound B (PiB), 18F-florebetapir or 18F-Flutemetamol as described elsewhere76,77,78. PET standardized uptake value ratios (SUVR) were determined for all tracers using CapAIBL, a web based freely availably MR-less methodology79. Briefly, SUVs were summed and normalized to either the cerebellar cortex SUV (PiB), whole cerebellum SUV (florbetapir, FBP) or pons SUV (flutemetamol, FLUTE) to yield the target-region to reference-region SUVR. To allow for the analysis of tracer specific SUVRs as a single continuous variable, a linear regression transformation, termed the “Before the Centiloid Kernel Transformation” (BeCKeT) scale, was applied to FBP and FLUTE SUVR to generate PiB-like SUVR units80.
Hippocampal Volume data was available for 319 (229 CN, 52 MCI, 38 AD) participants at baseline. Hippocampal volumes were determined through MRI, parameters of which have been previously described81. Briefly, participants underwent T1 weighted MRI using the ADNI 3-dimensional (3D) Magnetization Prepared Rapid Gradient Echo (MPRAGE) sequence on 1.5 T or 3 T scanners. Hippocampal volume was calculated after correcting for age in years and intracranial volume (sum of grey matter, white matter and cerebrospinal fluid volumes), as previously described82.
Statistical analysis
All statistical analysis was conducted using IBM SPSS Statistics (version 23; IBM Corp, Armonk, NY, USA) with the level of significance set to α = 0.05 (two-tailed). All variables were assessed for conformation to a normal distribution. Box-Cox transformations was used to correct variables departing from a normal distribution83. For all variables, except HOMA indices, the calculated lambda (λ) equated to no transformation. HOMA indices underwent transformations (T(Y)) prior to analysis, specifically: T(Y) = ((Y + 1)−0.079−1)/−0.079 and T(Y) = (Y0.04−1)/0.04 for HOMA-IR and HOMA-B, respectively (with Y representing the HOMA index). Analysis of demographic variables was undertaken using a One-way Analysis of Variance (ANOVA) to determine differences in continuous variables across clinical classifications differences in categorical variables determined using the χ2-test. Differences in HOMA indices between clinical classifications were assessed using an analysis of covariance (ANCOVA) via a General Linear Model (GLM) with Bonferroni correction. Associations between HOMA indices and cognitive composites and pathological brain changes in CN were assessed using linear regression analysis. Both ANCOVA and linear regression analyses, for all dependent variables, covaried for body mass index (BMI), diabetes (yes/no), diabetes medication (yes/no), hypertension (yes/no), smoking (yes/no), and APOE genotype (ε4+/ε4−), with sex and age only covaried for with biomarker dependent variables.
Data availability
All data and samples used in this study are derived from the Australian Imaging, Biomarkers and Lifestyle (AIBL) Study of Ageing. All AIBL data, and that specific to this study, is publically accessible to all interested parties through an Expression of Interest procedure and is governed by the AIBL Data Use Agreement, for more information please see https://aibl.csiro.au/awd/.
References
Leibson, C. L. et al. The risk of dementia among persons with diabetes mellitus: a population-based cohort study. Ann NY Acad Sci 826, 422–427 (1997).
Arvanitakis, Z. et al. Diabetes mellitus and progression of rigidity and gait disturbance in older persons. Neurology 63, 996–1001 (2004).
Ott, A. et al. Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology 53, 1937–1942 (1999).
Peila, R., Rodriguez, B. L., Launer, L. J. & Honolulu-Asia Aging, S. Type 2 diabetes, APOE gene, and the risk for dementia and related pathologies: The Honolulu-Asia Aging Study. Diabetes 51, 1256–1262 (2002).
Xu, W. L., Qiu, C. X., Wahlin, A., Winblad, B. & Fratiglioni, L. Diabetes mellitus and risk of dementia in the Kungsholmen project: a 6-year follow-up study. Neurology 63, 1181–1186 (2004).
Manschot, S. M. et al. Brain magnetic resonance imaging correlates of impaired cognition in patients with type 2 diabetes. Diabetes 55, 1106–1113 (2006).
van Harten, B., Oosterman, J. M., Potter van Loon, B. J., Scheltens, P. & Weinstein, H. C. Brain lesions on MRI in elderly patients with type 2 diabetes mellitus. Eur Neurol 57, 70–74, doi:10.1159/000098054 (2007).
Moran, C. et al. Brain atrophy in type 2 diabetes: regional distribution and influence on cognition. Diabetes Care 36, 4036–4042, doi:10.2337/dc13-0143 (2013).
Biessels, G. J. & Reijmer, Y. D. Brain changes underlying cognitive dysfunction in diabetes: what can we learn from MRI? Diabetes 63, 2244–2252, doi:10.2337/db14-0348 (2014).
Moran, C. et al. Type 2 diabetes, skin autofluorescence, and brain atrophy. Diabetes 64, 279–283, doi:10.2337/db14-0506 (2015).
Kooistra, M. et al. Diabetes mellitus and progression of vascular brain lesions and brain atrophy in patients with symptomatic atherosclerotic disease. The SMART-MR study. J Neurol Sci 332, 69–74, doi:10.1016/j.jns.2013.06.019 (2013).
van Elderen, S. G. et al. Progression of brain atrophy and cognitive decline in diabetes mellitus: a 3-year follow-up. Neurology 75, 997–1002, doi:10.1212/WNL.0b013e3181f25f06 (2010).
Verdile, G., Fuller, S. J. & Martins, R. N. The role of type 2 diabetes in neurodegeneration. Neurobiol Dis 84, 22–38, doi:10.1016/j.nbd.2015.04.008 (2015).
Verdile, G. et al. Inflammation and Oxidative Stress: The Molecular Connectivity between Insulin Resistance, Obesity, and Alzheimer’s Disease. Mediators Inflamm 2015, 105828, doi:10.1155/2015/105828 (2015).
Cohen, A. D. & Klunk, W. E. Early detection of Alzheimer’s disease using PiB and FDG PET. Neurobiol Dis 72 Pt A, 117–122, doi:10.1016/j.nbd.2014.05.001 (2014).
Roberts, R. O. et al. Diabetes and elevated hemoglobin A1c levels are associated with brain hypometabolism but not amyloid accumulation. J Nucl Med 55, 759–764, doi:10.2967/jnumed.113.132647 (2014).
Thambisetty, M. et al. Glucose intolerance, insulin resistance, and pathological features of Alzheimer disease in the Baltimore Longitudinal Study of Aging. JAMA Neurol 70, 1167–1172, doi:10.1001/jamaneurol.2013.284 (2013).
Willette, A. A. et al. Insulin resistance predicts brain amyloid deposition in late middle-aged adults. Alzheimers Dement 11, 504–510, e501, doi:10.1016/j.jalz.2014.03.011 (2015).
Huxley, R., Barzi, F. & Woodward, M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ 332, 73–78, doi:10.1136/bmj.38678.389583.7C (2006).
Chatterjee, S. et al. Type 2 Diabetes as a Risk Factor for Dementia in Women Compared With Men: A Pooled Analysis of 2.3 Million People Comprising More Than 100,000 Cases of Dementia. Diabetes Care 39, 300–307, doi:10.2337/dc15-1588 (2016).
Peters, S. A., Huxley, R. R. & Woodward, M. Diabetes as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 64 cohorts, including 775,385 individuals and 12,539 strokes. Lancet 383, 1973–1980, doi:10.1016/S0140-6736(14)60040-4 (2014).
Keane, K. N., Cruzat, V. F., Carlessi, R., de Bittencourt, P. I. Jr. & Newsholme, P. Molecular Events Linking Oxidative Stress and Inflammation to Insulin Resistance and beta-Cell Dysfunction. Oxid Med Cell Longev 2015, 181643, doi:10.1155/2015/181643 (2015).
Vandal, M. et al. Insulin reverses the high-fat diet-induced increase in brain Abeta and improves memory in an animal model of Alzheimer disease. Diabetes 63, 4291–4301, doi:10.2337/db14-0375 (2014).
Park, S., Kim, D. S., Kang, S. & Moon, N. R. beta-Amyloid-induced cognitive dysfunction impairs glucose homeostasis by increasing insulin resistance and decreasing beta-cell mass in non-diabetic and diabetic rats. Metabolism 62, 1749–1760, doi:10.1016/j.metabol.2013.08.007 (2013).
Miklossy, J. et al. Beta amyloid and hyperphosphorylated tau deposits in the pancreas in type 2 diabetes. Neurobiol Aging 31, 1503–1515, doi:10.1016/j.neurobiolaging.2008.08.019 (2010).
Craft, S. et al. Memory improvement following induced hyperinsulinemia in Alzheimer’s disease. Neurobiol Aging 17, 123–130 (1996).
Craft, S. et al. Cerebrospinal fluid and plasma insulin levels in Alzheimer’s disease: relationship to severity of dementia and apolipoprotein E genotype. Neurology 50, 164–168 (1998).
Reger, M. A. et al. Intranasal insulin administration dose-dependently modulates verbal memory and plasma amyloid-beta in memory-impaired older adults. J Alzheimers Dis 13, 323–331 (2008).
Morris, J. K., Vidoni, E. D., Honea, R. A. & Burns, J. M. & Alzheimer’s Disease Neuroimaging, I. Impaired glycemia increases disease progression in mild cognitive impairment. Neurobiol Aging 35, 585–589, doi:10.1016/j.neurobiolaging.2013.09.033 (2014).
Pucci, G. et al. Sex- and gender-related prevalence, cardiovascular risk and therapeutic approach in metabolic syndrome: A review of the literature. Pharmacol Res 120, 34–42, doi:10.1016/j.phrs.2017.03.008 (2017).
Unwin, N., Shaw, J., Zimmet, P. & Alberti, K. G. Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. Diabet Med 19, 708–723 (2002).
Janssen, I., Powell, L. H., Crawford, S., Lasley, B. & Sutton-Tyrrell, K. Menopause and the metabolic syndrome: the Study of Women’s Health Across the Nation. Arch Intern Med 168, 1568–1575, doi:10.1001/archinte.168.14.1568 (2008).
Lovejoy, J. C., Champagne, C. M., de Jonge, L., **e, H. & Smith, S. R. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes (Lond) 32, 949–958, doi:10.1038/ijo.2008.25 (2008).
Pike, C. J. Sex and the development of Alzheimer’s disease. J Neurosci Res 95, 671–680, doi:10.1002/jnr.23827 (2017).
Benedict, C. et al. Impaired insulin sensitivity as indexed by the HOMA score is associated with deficits in verbal fluency and temporal lobe gray matter volume in the elderly. Diabetes Care 35, 488–494, doi:10.2337/dc11-2075 (2012).
Ekblad, L. L. et al. Insulin resistance is associated with poorer verbal fluency performance in women. Diabetologia 58, 2545–2553, doi:10.1007/s00125-015-3715-4 (2015).
Schuur, M. et al. Insulin-resistance and metabolic syndrome are related to executive function in women in a large family-based study. Eur J Epidemiol 25, 561–568, doi:10.1007/s10654-010-9476-y (2010).
Elias, M. F. et al. The preclinical phase of alzheimer disease: A 22-year prospective study of the Framingham Cohort. Arch Neurol 57, 808–813 (2000).
Grober, E. et al. Memory impairment, executive dysfunction, and intellectual decline in preclinical Alzheimer’s disease. J Int Neuropsychol Soc 14, 266–278, doi:10.1017/S1355617708080302 (2008).
Derby, C. A. et al. Screening for predementia AD: time-dependent operating characteristics of episodic memory tests. Neurology 80, 1307–1314, doi:10.1212/WNL.0b013e31828ab2c9 (2013).
Palta, P., Schneider, A. L., Biessels, G. J., Touradji, P. & Hill-Briggs, F. Magnitude of cognitive dysfunction in adults with type 2 diabetes: a meta-analysis of six cognitive domains and the most frequently reported neuropsychological tests within domains. J Int Neuropsychol Soc 20, 278–291, doi:10.1017/S1355617713001483 (2014).
Vincent, C. & Hall, P. A. Executive Function in Adults With Type 2 Diabetes: A Meta-Analytic Review. Psychosom Med 77, 631–642, doi:10.1097/PSY.0000000000000103 (2015).
Mehla, J., Chauhan, B. C. & Chauhan, N. B. Experimental induction of type 2 diabetes in aging-accelerated mice triggered Alzheimer-like pathology and memory deficits. J Alzheimers Dis 39, 145–162, doi:10.3233/JAD-131238 (2014).
Knight, E. M., Martins, I. V., Gumusgoz, S., Allan, S. M. & Lawrence, C. B. High-fat diet-induced memory impairment in triple-transgenic Alzheimer’s disease (3xTgAD) mice is independent of changes in amyloid and tau pathology. Neurobiol Aging 35, 1821–1832, doi:10.1016/j.neurobiolaging.2014.02.010 (2014).
Takeda, S. et al. Diabetes-accelerated memory dysfunction via cerebrovascular inflammation and Abeta deposition in an Alzheimer mouse model with diabetes. Proc Natl Acad Sci USA 107, 7036–7041, doi:10.1073/pnas.1000645107 (2010).
Wang, Y. et al. Synergistic exacerbation of mitochondrial and synaptic dysfunction and resultant learning and memory deficit in a mouse model of diabetic Alzheimer’s disease. J Alzheimers Dis 43, 451–463, doi:10.3233/JAD-140972 (2015).
Ho, L. et al. Diet-induced insulin resistance promotes amyloidosis in a transgenic mouse model of Alzheimer’s disease. FASEB J 18, 902–904, doi:10.1096/fj.03-0978fje (2004).
Hoscheidt, S. M. et al. Insulin Resistance is Associated with Increased Levels of Cerebrospinal Fluid Biomarkers of Alzheimer’s Disease and Reduced Memory Function in At-Risk Healthy Middle-Aged Adults. J Alzheimers Dis 52, 1373–1383, doi:10.3233/JAD-160110 (2016).
Hoscheidt, S. M. et al. Insulin resistance is associated with lower arterial blood flow and reduced cortical perfusion in cognitively asymptomatic middle-aged adults. J Cereb Blood Flow Metab. doi:10.1177/0271678X16663214 (2016).
Reiman, E. M. et al. Fibrillar amyloid-beta burden in cognitively normal people at 3 levels of genetic risk for Alzheimer’s disease. Proc Natl Acad Sci USA 106, 6820–6825, doi:10.1073/pnas.0900345106 (2009).
Castellano, J. M. et al. Human apoE isoforms differentially regulate brain amyloid-beta peptide clearance. Sci Transl Med 3, 89ra57, doi:10.1126/scitranslmed.3002156 (2011).
Bales, K. R. et al. Human APOE isoform-dependent effects on brain beta-amyloid levels in PDAPP transgenic mice. J Neurosci 29, 6771–6779, doi:10.1523/JNEUROSCI.0887-09.2009 (2009).
Morris, J. C. et al. APOE predicts amyloid-beta but not tau Alzheimer pathology in cognitively normal aging. Ann Neurol 67, 122–131, doi:10.1002/ana.21843 (2010).
Lim, Y. Y. et al. Abeta amyloid, cognition, and APOE genotype in healthy older adults. Alzheimer’s & dementia: the journal of the Alzheimer’s Association 9, 538–545, doi:10.1016/j.jalz.2012.07.004 (2013).
Lim, Y. Y. et al. APOE epsilon4 moderates amyloid-related memory decline in preclinical Alzheimer’s disease. Neurobiol Aging 36, 1239–1244, doi:10.1016/j.neurobiolaging.2014.12.008 (2015).
LaDu, M. J. et al. Isoform-specific binding of apolipoprotein E to beta-amyloid. J Biol Chem 269, 23403–23406 (1994).
Yang, D. S. et al. Apolipoprotein E promotes the binding and uptake of beta-amyloid into Chinese hamster ovary cells in an isoform-specific manner. Neuroscience 90, 1217–1226 (1999).
Hone, E. et al. Alzheimer’s disease amyloid-beta peptide modulates apolipoprotein E isoform specific receptor binding. J Alzheimers Dis 7, 303–314 (2005).
Deane, R. et al. apoE isoform-specific disruption of amyloid beta peptide clearance from mouse brain. J Clin Invest 118, 4002–4013, doi:10.1172/JCI36663 (2008).
Sharman, M. J. et al. APOE genotype results in differential effects on the peripheral clearance of amyloid-beta42 in APOE knock-in and knock-out mice. J Alzheimers Dis 21, 403–409, doi:10.3233/JAD-2010-100141 (2010).
Irizarry, M. C. et al. Apolipoprotein E modulates gamma-secretase cleavage of the amyloid precursor protein. J Neurochem 90, 1132–1143, doi:10.1111/j.1471-4159.2004.02581.x (2004).
Hass, S., Weidemann, A., Utermann, G. & Baier, G. Intracellular apolipoprotein E affects Amyloid Precursor Protein processing and amyloid Abeta production in COS-1 cells. Mol Genet Genomics 265, 791–800 (2001).
Ishii, M. & Iadecola, C. Metabolic and Non-Cognitive Manifestations of Alzheimer’s Disease: The Hypothalamus as Both Culprit and Target of Pathology. Cell Metab 22, 761–776, doi:10.1016/j.cmet.2015.08.016 (2015).
Bharadwaj, P. et al. The Link between Type 2 Diabetes and Neurodegeneration: Roles for Amyloid-beta, Amylin, and Tau Proteins. J Alzheimers Dis, doi:10.3233/JAD-161192 (2017).
Nestor, P. J., Fryer, T. D., Smielewski, P. & Hodges, J. R. Limbic hypometabolism in Alzheimer’s disease and mild cognitive impairment. Ann Neurol 54, 343–351, doi:10.1002/ana.10669 (2003).
Cross, D. J. et al. Loss of olfactory tract integrity affects cortical metabolism in the brain and olfactory regions in aging and mild cognitive impairment. J Nucl Med 54, 1278–1284, doi:10.2967/jnumed.112.116558 (2013).
Macesic, M. et al. Impaired Insulin Sensitivity And Secretion In Patients With Alzheimer’s Disease: The Relationship With Other Atherosclerosis Risk Factors. Curr Vasc Pharmacol (2016).
Ellis, K. A. et al. The Australian Imaging, Biomarkers and Lifestyle (AIBL) study of aging: methodology and baseline characteristics of 1112 individuals recruited for a longitudinal study of Alzheimer’s disease. Int Psychogeriatr 21, 672–687, doi:10.1017/S1041610209009405 (2009).
Burnham, S. C. et al. Novel Statistically-Derived Composite Measures for Assessing the Efficacy of Disease-Modifying Therapies in Prodromal Alzheimer’s Disease Trials: An AIBL Study. J Alzheimers Dis 46, 1079–1089, doi:10.3233/JAD-143015 (2015).
Wallace, T. M., Levy, J. C. & Matthews, D. R. Use and abuse of HOMA modeling. Diabetes Care 27, 1487–1495 (2004).
Matthews, D. R. et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985).
Levy, J. C., Matthews, D. R. & Hermans, M. P. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care 21, 2191–2192 (1998).
Brown, B. M. et al. Influence of BDNF Val66Met on the relationship between physical activity and brain volume. Neurology 83, 1345–1352, doi:10.1212/WNL.0000000000000867 (2014).
Li, Q. X. et al. Alzheimer’s Disease Normative Cerebrospinal Fluid Biomarkers Validated in PET Amyloid-beta Characterized Subjects from the Australian Imaging, Biomarkers and Lifestyle (AIBL) study. J Alzheimers Dis 48, 175–187, doi:10.3233/JAD-150247 (2015).
Vanderstichele, H. et al. Standardization of preanalytical aspects of cerebrospinal fluid biomarker testing for Alzheimer’s disease diagnosis: a consensus paper from the Alzheimer’s Biomarkers Standardization Initiative. Alzheimers Dement 8, 65–73, doi:10.1016/j.jalz.2011.07.004 (2012).
Rowe, C. C. et al. Amyloid imaging results from the Australian Imaging, Biomarkers and Lifestyle (AIBL) study of aging. Neurobiol Aging 31, 1275–1283, doi:10.1016/j.neurobiolaging.2010.04.007 (2010).
Clark, C. M. et al. Use of florbetapir-PET for imaging beta-amyloid pathology. JAMA 305, 275–283, doi:10.1001/jama.2010.2008 (2011).
Vandenberghe, R. et al. 18F-flutemetamol amyloid imaging in Alzheimer disease and mild cognitive impairment: a phase 2 trial. Ann Neurol 68, 319–329, doi:10.1002/ana.22068 (2010).
Bourgeat, P. et al. Comparison of MR-less PiB SUVR quantification methods. Neurobiol Aging 36(Suppl 1), S159–166, doi:10.1016/j.neurobiolaging.2014.04.033 (2015).
Villemagne, V. et al. En Attendant Centiloid. Advances in Research 2, 723–729 (2014).
Bourgeat, P. et al. Beta-amyloid burden in the temporal neocortex is related to hippocampal atrophy in elderly subjects without dementia. Neurology 74, 121–127, doi:10.1212/WNL.0b013e3181c918b5 (2010).
Dore, V. et al. Cross-sectional and longitudinal analysis of the relationship between Abeta deposition, cortical thickness, and memory in cognitively unimpaired individuals and in Alzheimer disease. JAMA Neurol 70, 903–911, doi:10.1001/jamaneurol.2013.1062 (2013).
Box, G. E. P. & Cox, D. R. An Analysis of Transformations. J Roy Stat Soc B 26, 211–252 (1964).
Acknowledgements
Funding for the AIBL study was provided in part by the study partners [Commonwealth Scientific Industrial and research Organization (CSIRO), Edith Cowan University (ECU), Mental Health Research institute (MHRI), National Ageing Research Institute (NARI), Austin Health, CogState Ltd.]. The AIBL study has also received support from the National Health and Medical Research Council (NHMRC) and the Dementia Collaborative Research Centres program (DCRC2), as well as funding from the Science and Industry Endowment Fund (SIEF) and the Cooperative Research Centre (CRC) for Mental Health – funded through the CRC Program (Grant ID:20100104), an Australian Government Initiative. GV is supported by the Curtin Senior Resarch Fellowship (CRF140196), West Australian Department of Health Merit Award and the National Health and Medical Research Council (APP1105698) awarded to G.V, P.N., P.F. and R.M. We thank all those who took part as subjects in the study for their commitment and dedication to hel** advance research into the early detection and causation of AD. We kindly thank all AIBL Research Group members (http://aibl.csiro.au/about/aibl-research-team/).
Author information
Authors and Affiliations
Contributions
S.M.L., G.V. designed the study, collated, analysed and interpreted data and drafted the manuscript; S.G., A.W. helped collate data and draft the manuscript; T.P., V.D., Q.X.L., helped collate data and reviewed the manuscript; S.B. provided data analysis and interpretation and reviewed the manuscript; V.L.V. helped collate data, interpret analysis and reviewed the manuscript; V.S., D.B., P.F., P.N., N.W., P.M., C.L.M., S.R.S., C.C.R., O.S. and R.N.M. reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing Interests
CLM is an advisor to Prana Biotechnology Ltd and a consultant to Eli Lilly. PM is a full-time employee of Cogstate Ltd. DA has served on scientific advisory boards for Novartis, Eli Lilly, Janssen, and Pfizer Inc. RNM is a consultant to Alzhyme. SML has previously been a paid consultant to Alzhyme. CCR has served on scientific advisory boards for Bayer Pharma, Elan Corporation, GE Healthcare and AstraZeneca; has received speaker honoraria from Bayer Pharma and GE Healthcare; and has received research support from Bayer Pharma, GE Healthcare, Piramal Lifesciences and Avid Radiopharmaceuticals. VLV served as a consultant for Bayer Pharma; and received research support from a NEDO grant from Japan. All other authors have nothing to disclose.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Laws, S.M., Gaskin, S., Woodfield, A. et al. Insulin resistance is associated with reductions in specific cognitive domains and increases in CSF tau in cognitively normal adults. Sci Rep 7, 9766 (2017). https://doi.org/10.1038/s41598-017-09577-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-09577-4
- Springer Nature Limited
This article is cited by
-
The relationship of insulin resistance and diabetes to tau PET SUVR in middle-aged to older adults
Alzheimer's Research & Therapy (2023)
-
Intranasal insulin modulates cerebrospinal fluid markers of neuroinflammation in mild cognitive impairment and Alzheimer’s disease: a randomized trial
Scientific Reports (2022)
-
Network activity changes in the pathophysiology of Alzheimer’s disease: the role of aging and early entorhinal cortex dysfunction
Metabolic Brain Disease (2022)
-
Intranasal Insulin for Alzheimer’s Disease
CNS Drugs (2021)
-
A Phase II, Single-Center, Randomized, Double-Blind, Placebo-Controlled Study of the Safety and Therapeutic Efficacy of Intranasal Glulisine in Amnestic Mild Cognitive Impairment and Probable Mild Alzheimer’s Disease
Drugs & Aging (2021)