Abstract
Influenza virus infections pose a significant threat to global health. Vaccination is the main countermeasure against influenza virus spread, however, the effectiveness of vaccines is variable. Current seasonal influenza virus vaccines mostly rely on the immunodominant hemagglutinin (HA) glycoprotein on the viral surface, which usually leads to a narrow and strain-specific immune response. The HA undergoes constant antigenic drift, which can lead to a dramatic loss in vaccine effectiveness, requiring the annual reformulation and readministration of influenza virus vaccines. Recently, it has been demonstrated that the subdominant glycoprotein, neuraminidase (NA), is an attractive target for vaccine development. Here, we tested a newly developed recombinant influenza virus N1 neuraminidase vaccine candidate, named N1-MPP, adjuvanted with CpG 1018, a TLR9 agonist. Additionally, N2-MPP and B-NA-MPP vaccine constructs have been generated to cover the range of influenza viruses that are seasonally circulating in humans. These constructs have been characterized in vitro and in vivo regarding their functionality and protective potential. Furthermore, a trivalent NA-MPP mix was tested. No antigenic competition between the individual NA constructs was detected. By adjuvating the recombinant protein constructs with CpG 1018 it was possible to induce a strong and robust immune response against the NA, which provided full protection against morbidity and mortality after high lethal challenges in vivo. This study provides important insights for the development of a broadly protective NA-based influenza virus vaccine candidate.
Similar content being viewed by others
Introduction
Influenza viruses can cause severe respiratory infections in humans and pose a significant threat to global health. According to the World Health Organization, seasonal influenza viruses cause up to five million cases of severe influenza virus infection, including up to 650,000 deaths each year globally. The influenza virus contains two glycoproteins on its viral surface, which include the immunodominant hemagglutinin (HA) and the immunosubdominant neuraminidase (NA). Current available seasonal influenza virus vaccines mostly target the HA as the NA content in the vaccines is not standardized and can vary significantly. While the HA of the influenza virus is known to induce a strong neutralizing antibody response in humans, it is more susceptible to antigenic drift. This can lead to a mismatch between vaccine strains and circulating strains, resulting in a significant loss of effectiveness of the annual vaccines.
Over the past few years, the NA has emerged as an attractive target for vaccine development since it is less prone to undergo antigenic drift and therefore is antigenically more stable. In addition, it has been demonstrated in animal models as well as in humans that anti-NA immunity correlates with protection and reduces viral shedding1,2,3,4,5. The main obstacles to using NA as a vaccine antigen are its lack of standardization in seasonal vaccine preparations as well as its fragile stability. Indeed, the amount of NA in seasonal vaccines usually varies in quality and quantity6 and it is likely that the structural integrity in current vaccine formulations is suboptimal. Additionally, it has been hypothesized that antigenic competition occurs between HA and NA in vaccine formulations, making the NA immunosubdominant7. The anti-NA immunity acquired after vaccination with live attenuated or inactivated vaccines is mediocre at best8. Stable, recombinant NA protein has been shown to be immunogenic and protective in animal models5,6,9 and may enhance NA-based immunity in humans by standalone administration or as an admixture to seasonal influenza virus vaccines. Recently, we have developed a recombinant NA vaccine candidate, named N1-MPP10. This vaccine candidate utilized the tetramerization domain of the phosphoprotein of the measles virus to multimerize and stabilize the NA protein. N1-MPP can form fully enzymatically active NA tetramers which are highly protective in vivo in a mouse model and induce high titers of neuraminidase inhibiting (NI) antibodies after vaccination. The tetramerization of the protein is a crucial factor in generating an NA-based vaccine since it has been previously shown that only multimeric but not monomeric protein confers protection in vivo11,12.
In general, the efficiency of a vaccine depends on the magnitude, duration, and quality of the immune response that is induced. However, recombinant protein vaccines usually tend to induce a lower immune response compared to whole virus vaccines due to the lack of molecules that engage innate immune receptors. Here, we tested N1-MPP—as well as novel N2-MPP and B-NA-MPP constructs in a trivalent formulation—adjuvanted with the GMP-produced TLR9 agonist CpG 1018 (ODN1018) in the mouse model. CpG 1018 is currently used in the licensed hepatitis B virus vaccine HEPLISAV-B®13,14. The work described here was performed in preparation for the clinical testing of N1-MPP with CpG 1018.
Results
A prime-boost regimen with N1-MPP is required to achieve full protection in a naive mouse model
To assess the adjuvant effect of CpG 1018 on the N1-MPP antigen in a prime-only or prime-boost vaccination regimen, naive female 6–8 week old BALB/c mice (n = 5 per group) were either vaccinated once with 3 μg N1-MPP, 3 μg N1-MPP + 3 μg CpG 1018, or 3 μg of an irrelevant protein, or twice with the same formulations in a 3-week interval (Fig. 1A). Three weeks post boost, mice were then challenged with 10 x the 50% mouse lethal dose (mLD50) of A/Singapore/GP1908/15 H1N1 (IVR-180, this virus is antigenically equivalent to A/Michigan/45/15) virus, and weight loss and survival were monitored over a 14-day period. As shown in Fig. 1B, mice that only received one vaccination with non-adjuvanted N1-MPP or irrelevant protein all succumbed to infection around day 8 post challenge. Mice vaccinated once with N1-MPP + CpG 1018 experienced high weight loss (approximately 20%) and 4 out of 5 mice succumbed to infection around day 10 post challenge. Nevertheless, mice vaccinated with the adjuvanted formulation survived significantly longer (p = 0.0143). However, groups of mice that received two vaccinations of N1-MPP or N1-MPP + CpG 1018 did not experience any weight loss and all animals in these groups survived the challenge. All mice in the negative control group succumbed to infection around day 8 (Fig. 1B, C). To assess serological characteristics of the serum antibodies induced after vaccination, the serum was tested via an enzyme-linked immunosorbent assay (ELISA) against recombinant Mich15 N1-VASP protein. This protein containing a different tetramerization domain was used to avoid the detection of antibodies induced against the MPP tetramerization domain. After the prime, only a low antibody response against the NA was detectable, with slightly higher levels in the N1-MPP + CpG 1018 group (Fig. 1D). Serum from mice vaccinated with the prime-boost regimen showed a strong increase in N1-specific antibodies, with N1-MPP + CpG 1018 performing the best (Fig. 1D). The same trend was observed in a NI assay using an H7N1Mich15 virus, which contains an irrelevant HA and the N1 of A/Michigan/45/15. Mice vaccinated with the prime-boost regimen showed high levels of NI active antibodies in their serum with the N1-MPP + CpG 1018 group performing best (geometric mean 50% inhibitory dilution (ID50) = 7046) indicating that the CpG 1018 adjuvant leads to a more robust immune response to the antigen (Fig. 1E). The NI results also indicated a statistically significant difference between adjuvanted and non-adjuvanted groups in the prime-boost regimen.
A Mice (n = 5 per group, except for Neg. Contr. 2× Vacc where n = 3) were vaccinated either once (prime) or twice (prime-boost) with 3 μg of N1-MPP, 3 μg N1-MPP + ODN1018 or irrelevant protein following a challenge with 10xmLD50 of A/Singapore/GP1908/15 H1N1 (IVR-180). Weight loss and survival were monitored over a 14-day time period. Mice were bled on day 21 and 42 post prime for serological analysis. B Weight loss curve (mean plus standard deviation) and C survival after challenge with 10xmLD50 of A/Singapore/GP1908/15 H1N1 (IVR-180) are shown. Differences in survival between the vaccine groups and respective control groups as well as between matched prime-only and prime-boost groups were analyzed using a Mantel–Cox log-rank test. N1-MPP + ODN1018 1× Vacc vs. Neg. Contr. 1× Vacc p = 0.0298; N1-MPP 1× Vacc vs. N1-MPP + ODN1018 1× Vacc p = 0.0143; N1-MPP 2× Vacc vs Neg. Contr. 2× Vacc p = 0.0067; N1-MPP + ODN1018 2× Vacc vs. Neg. Contr. 2× Vacc p = 0.0067; N1-MPP 1× Vacc vs. N1-MPP 2× Vacc p = 0.0027; N1-MPP + ODN1018 1× Vacc vs. N1-MPP + ODN1018 2× Vacc p = 0.0494. The difference between the remaining curves were not statistically significant p > 0.05 or they were not compared. D ELISA titers in serum pre-challenge are shown (mean plus standard deviation). E NI titers 42 days post prime using H7N1Mich15 virus (geometric mean plus standard deviation of the geometric mean). Statistical analysis in E was performed using a one-way ANOVA corrected for multiple comparisons.
Passive serum transfer from vaccinated to naive mice protects from lethal challenge
Serum obtained from mice vaccinated with the prime-boost regimen with N1-MPP, N1-MPP + 3 μg CpG 1018 or an irrelevant protein was used to perform a passive serum transfer into 6–8 week old naive BALB/c mice (n = 5 per group) followed by a challenge with 5xmLD50 of A/Singapore/GP1908/15 H1N1 (IVR-180). Weight loss and survival were monitored over a 14-day period. Mice which received N1-MPP serum showed ~10% weight loss, with one mouse succumbing to infection on day 6 post challenge. Mice that received N1-MPP + CpG 1018 experienced slightly less weight loss than the N1-MPP group and experienced no mortality (Fig. 2A, B). The negative control group succumbed to infection by day 8 post challenge.
BALB/c mice (n = 5 per group) received a passive serum transfer intraperitoneally and were challenged with 5xmLD50 of A/Singapore/GP1908/15 H1N1 (IVR-180). Weight loss A was monitored over a 14-day period (shown is mean plus standard deviation) and the survival B of each group is also shown. Differences in survival were analyzed using a Mantel–Cox log-rank test. N1-MPP vs Neg. Ctrl. p = 0.0419, N1-MPP + ODN1018 vs Neg. Ctrl. p = 0.0034, the remaining differences were not statistically significant (p > 0.05).
CpG 1018 adjuvantation partially breaks the immunodominance of HA over NA in a QIV + rNA formulation in terms of anti-NA antibody titers
We have previously shown, that – while recombinant NA on its own is immunogenic—admixture to QIV leads to reduced immunogenicity, likely due to the immunodominance of HA over NA10. To test if CpG 1018 would improve NA immunogenicity, even in a mixture with QIV, naive female 6–8 week old BALB/c mice (n = 5 per group) were vaccinated IM in a prime-boost regimen. Mice received either 3 µg of N1-MPP, 3 µg N1-MPP + 3 μg CpG 1018, QIV (matched with the challenge virus), QIV + 3 μg CpG 1018, 3 µg N1-MPP admixed with QIV, 3 µg N1-MPP admixed with QIV and 3 μg CpG 1018, 3 µg of N1-MPP given in the right leg and QIV at the same time in the left leg (N1-MPP (r) + QIV (l)), 3 µg of N1-MPP + 3 μg CpG 1018 given in the right leg and QIV + 3 μg CpG 1018 given in the left leg at the same time (N1-MPP + 3 μg CpG 1018 (r) + QIV + 3 μg CpG 1018 (l)) or 3 µg of irrelevant protein (Fig. 3A). Following vaccination, mice were challenged with 25xmLD50 of A/Singapore/GP1908/2015 H1N1 (IVR-180). Weight loss and survival was monitored over a 14-day period. The non-adjuvanted N1-MPP group showed the highest post challenge weight loss of ~10% and one mouse in the group succumbed to infection on day 6 post infection. All mice in the negative control group succumbed to infection on day 6 post infection. The remaining groups did not experience any morbidity or mortality (Fig. 3B, C).
A Vaccination scheme, mice (n = 5 per group) were vaccinated in a prime/boost regimen and then challenged either with 25xmLD50 of A/Singapore/GP1908/15 H1N1 (IVR-180) to monitor weight loss and survival over a 14-day period or with 1xmLD50 of A/Singapore/GP1908/15 H1N1 (IVR-180) to determine viral lung titers. B Weight loss curve (mean plus standard deviation) and C survival after viral challenge are shown. Differences in survival were analyzed using a Mantel–Cox log-rank test. N1-MPP vs Neg. Ctrl. p = 0.0404, all other groups vs. Neg. Ctrl. p = 0.0082, all other comparisons were not statistically significant (p > 0.05). D Viral lung titers obtained on day 3 (n = 3 per group) and E day 6 (n = 3 per group) post challenge. Statistical analysis in D and E was performed using an one-way ANOVA corrected for multiple comparisons, shown is mean plus standard deviation.
To observe the effect of CpG 1018 on the reduction of viral load in the lungs, a subset of mice was infected with a lower challenge dose of 1xmLD50 A/Singapore/GP1908/15 H1N1 (IVR-180). Lungs were extracted on day 3 (Fig. 3D) and day 6 (Fig. 3E) post infection and the viral titers were determined. On day 3, the negative control group showed the highest viral titer (7.8 × 105 pfu/ml), followed by the N1-MPP group (5.1 × 104 pfu/ml), the N1-MPP + CpG 1018 (5.0 × 103 pfu/ml) and the QIV groups (1.0 × 103 pfu/ml). In the remaining groups, no virus was detectable. On day 6, the virus cleared out in the N1-MPP + CpG 1018 group as well as in the QIV group. The viral titer remained detectible in the N1-MPP group (8.5 × 103 pfu/ml) but was lower than in the negative control group (2.4 × 105 pfu/ml).
Since it is known that high titers of NI active antibodies correlate with reduction of viral replication as well as a less severe disease outcome, we wanted to assess the level of NI active antibodies induced after vaccination with N1-MPP and QIV in combination with CpG 1018. NI assays were performed with H7N1Mich15 virus, which contains the matching NA component to the vaccine antigen, and with H7N1Cal09 virus to observe if cross-reactive NI antibodies can be induced. Against H7N1Mich15, N1-MPP + CpG 1018 induced the highest level of NI antibodies (ID50 = 62309), followed by N1-MPP + CpG 1018 (r) and QIV + CpG 1018 (l) (ID50 = 17602), N1-MPP + QIV + CpG 1018 admixed (ID50 = 15954) and unadjuvanted N1-MPP (ID50 = 15409) (Fig. 4A). Of note, the N1-MPP + CpG 1018, N1-MPP + CpG 1018 (r) and QIV + CpG 1018 (l) and N1-MPP + QIV + CpG 1018 group NI activity were not significantly different suggesting that both administration of HA and NA containing vaccine in different limbs as well as co-administration in the presence of adjuvant may induce similar immune responses while this is not the case when recombinant NA is admixed with QIV without adjuvant. In case of the heterologous H7N1Cal09 virus, N1-MPP + CpG 1018 had the highest NI inhibition potential (ID50 = 4585), followed by the unadjuvanted N1-MPP group (ID50 = 1479) (Fig. 4B).
A NI using a reassortant H7N1Mich15 virus containing the N1 of A/Michigan/45/2015 or B containing the N1 of A/California/04/09. Geometric mean plus standard deviation is shown. Statistical analysis in A and B was performed using an one-way ANOVA corrected for multiple comparisons, shown is mean plus standard deviation. ELISA crossreactivity testing against C Mich15 N1-VASP protein, D NC99 N1-VASP protein, E PR8 N1-VASP protein, F Cal09 N1-VASP protein, G Bris18 N1-VASP protein, and H Vn04 N1-VASP protein. For C to H, mean and standard deviation are shown. N = 5 per group.
We also wanted to test if antibodies induced through vaccination with N1-MPP would induce N1 subtype cross-reactive antibodies. The serum was tested in ELISAs against recombinant Mich15 N1-VASP protein (Fig. 4C) matching the vaccine antigen strain, and against NC99 N1 (pre-pandemic N1, Fig. 4D), PR8 N1 (prototype N1, Fig. 4E), Cal09 N1 (Fig. 4F), Bris18 N1 (Fig. 4G) and Vn04 N1 (avian N1, Fig. 4H). Overall, the same trend was seen as in the NI assay, with N1-MPP + CpG 1018 performing the best, followed by N1-MPP + ODN1018 (r) and QIV + CpG 1018 (l) and N1-MPP + QIV + CpG 1018 admixed. This underscores that CpG 1018 is beneficial in inducing a strong and robust antibody response, which appears to be cross-reactive within the N1 subgroup. N1-MPP + QIV admixed induced only a low N1-specific antibody response as well as lower titers of NI active antibodies, underlining the antigenic competition between HA and NA.
Antigen dose de-escalation shows a clear adjuvant effect of CpG 1018
In the previous animal experiments described above, a standard amount of 3 μg N1-MPP protein per vaccine dose was used in a prime-boost regimen. Using this quantity of NA protein, it was observed that mice vaccinated with unadjuvanted N1-MPP, experienced approximately 10% weight loss (Fig. 5A), with one mouse which succumbing to infection on day 7 post challenge (Fig. 5B). However, mice which received N1-MPP + CpG 1018 did not experience any significant morbidity or mortality. To assess if this trend could be maintained with a reduced amount of N1-MPP, we performed a dose de-escalation study. Mice (n = 4–5 per group) were vaccinated IM in a prime/boost regimen with different amounts of antigen and challenged three weeks after the boost with 25xmLD50 of A/Singapore/GP1908/15 H1N1 (IVR-180). Mice were vaccinated with 1 µg, 0.3 µg, or 0.1 µg of N1-MPP, N1-MPP + CpG 1018 or an irrelevant protein. Mice which received 1 μg of N1-MPP experienced around 20% weight loss (Fig. 5C), with two mice succumbing to infection on day 6 and 7 post challenge (Fig. 5D). However, the 1 μg N1-MPP + CpG 1018 group experienced only 5% weight loss and showed full protection. When vaccinated with 0.3 μg of non-adjuvanted N1-MPP, all mice succumbed to infection by day 7 similar to the negative control group (Fig. 5E, F). The 0.3 μg N1-MPP + CpG 1018 group experienced high weight loss of almost 20% and three mice succumbed to infection by day 8. Vaccination with 0.1 μg of antigen, no matter if adjuvanted or non-adjuvanted, failed to protect mice against viral challenge and all mice succumbed to infection by day 7 (Fig. 5G, H). In terms of serological responses, there was a high level of N1-specific antibodies detectable via ELISA (against Mich15 N1-VASP protein) in mice which received 3 μg (Fig. 5C) and 1 μg (Fig. 5G) of antigen. Even though vaccination with 0.3 μg (Fig. 5K) and 0.1 μg (Fig. 5J) failed to induce protection in vivo, serological analysis revealed that there was still an N1 antibody response detectable, albeit only at low levels. In terms of NI activity, there were bigger differences detected between individual dose groups than in ELISA. After vaccination with 3 μg of N1-MPP + CpG 1018, the ID50 was 5000 (geometric mean) (Fig. 5I). Once the dose was reduced to 1 µg, the ID50 dropped to 324 for the N1-MPP + CpG 1018 group and to 119 for the non-adjuvanted N1-MPP group (Fig. 5I). For mice that received 0.3 μg of antigen, the N1-MPP + CpG 1018 group showed an ID50 of 113 (Fig. 5I). In the case of the 0.1 μg group, the ID50 level decreased to below the limit of detection (Fig. 5I). In general, while binding antibodies were present, these antibodies had little to no NI activity in groups which received low amounts of NA protein.
Mice (n = 4–5 per group) were vaccinated in a prime/boost regimen with different doses of antigen (3 µg, 1 µg, 0.3 µg, 0.1 µg) and then challenged with 25xmLD50 of A/Singapore/GP1908/15 H1N1 (IVR-180). Weight loss (mean plus standard deviation) and survival were monitored over a 14-day period. Blood was obtained 42 days after prime and serological testing via ELISA and an NI assay was performed. A, C, E, G Weight loss and B, D, F, H survival curves for the respective dose groups. Differences in survival were analyzed using a Mantel–Cox log-rank test. 3 µg N1-MPP vs 3 µg Neg. Ctrl. p = 0.0116; 3 µg N1-MPP + ODN1018 vs 1 µg Neg. Ctrl. p = 0.0031; 1 µg N1-MPP vs 1 µg Neg. Ctrl. p = 0.0143; 1 µg N1-MPP + ODN1018 vs 1 µg Neg. Ctrl. p = 0.0027; 0.1 µg N1-MPP vs 0.1 µg Neg. Ctrl. p = 0.0495; 0.1 µg N1-MPP + ODN1018 vs 0.1 µg Neg. Ctrl. p = 0.0143; the differences between the remaining curves were not statistically significant (p > 0.05). I NI using H7N1Mich15 virus and J ELISA against rec. Mich15 N1-VASP protein with serum from mice vaccinated for the dose de-escalation experiment. Statistical analysis in I and J was performed using an one-way ANOVA corrected for multiple comparisons, shown is mean plus standard deviation.
N2-MPP and B-NA-MPP form stable tetramers and exhibit full enzymatic activity
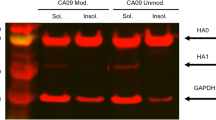
Current circulating influenza viruses in humans include H1N1, H3N2 and influenza B viruses. Therefore, we generated N2-MPP and B-NA-MPP constructs in addition to the N1-MPP construct. We cloned the sequences encoding for N2 of A/Kansas/14/17 (H3N2) and influenza B-NA of B/Colorado/6/17 into a pFastBac Dual vector containing a measles virus phosphoprotein tetramerization domain10. The constructs were expressed in insect cells and purified via an N-terminal hexahistidine tag. Structural integrity of the proteins was verified by visualizing them on a sodium dodecyl-sulfate polyacrylamide gel electrophoresis (SDS-PAGE). Under reducing conditions, N1, N2, and B-NA-MPP were visible as monomers at an expected size of ~60 kDa (Fig. 6A). By adding BS3 crosslinker, which cross-links primary amines, it was possible to confirm successful tetramerization of the N2-MPP and the B-NA-MPP protein. The tetramers were detectable at a size of ~240 kDa (Fig. 6B), which is comparable to the already established N1-MPP construct which was included as a control. Bovine serum albumin (BSA) served as monomeric control. To confirm that the NA-MPP proteins present the correct antigenic epitopes, an ELISA was performed using a broad panel of N2 (Fig. 6C)15 and B-NA (Fig. 6D)16 specific human monoclonal antibodies (mAbs). An irrelevant anti-Lassa antibody KL-AV-1A12 was included as negative control. All mAbs showed strong binding to N2-MPP and B-NA-MPP suggesting that the probed epitopes are presented in a native-like conformation. Next, we wanted to determine if the proteins are enzymatically active. For this, a standard NA-Star assay was performed. N1-MPP was included as a positive control. It was observed that N2-MPP and B-NA-MPP had high enzymatic activity comparable to the already established N1-MPP construct (Fig. 6E). However, the NA activity significantly varied between N1, N2, and B-NA-MPP which is not surprising since the different NA subtypes are known to have varying enzymatic activity based on the strain of origin17.
A SDS-PAGE under denaturating conditions, all proteins show monomeric structures at an expected size of ~60 kDa. BSA was included as a monomer control. B SDS-PAGE using a BS3 crosslinker. N1-MPP, N2-MPP and B-NA-MPP show tetrameric structures at around 240 kDa. BSA was included as a monomer control. C ELISA against rec. N2-MPP using a broad panel of human anti-N2 mAbs to verify correct presentation of epitopes. D ELISA against rec. B-NA-MPP using a broad panel of human anti-B-NA mAbs to verify correct presentation of epitopes. E Enzymatic activity of N1-MPP, N2-MPP, B-NA-MPP was determined via NA-Star assay. Assays in C to E were run once in duplicates and the duplicates were used to calculate one area under the curve (AUC) value.
Vaccination with recombinant N2-MPP and B-NA-MPP provides full protection against lethal influenza virus challenge in the mouse model
To test if the recombinant N2-MPP and B-NA-MPP could induce a protective immune response, we vaccinated mice IM with 3 μg of the respective antigen (n = 5 per group) in a prime-boost regimen. The protein was either given non-adjuvanted or supplemented with CpG 1018. Irrelevant protein was administered as negative control. Vaccination with N1-MPP was included as a positive control. Following vaccination, mice were challenged either with 25xmLD50 of A/Singapore/GP1908/15 (H1N1), A/Switzerland/9715293/13 (H3N2, mouse adapted) or B/New York/PV01181/18. Mice vaccinated with N1-MPP alone experienced a weight loss of around 10%, whereas the N1-MPP + CpG 1018 group did not show any morbidity or mortality (Fig. 7A, B). In case of N2-MPP vaccination, both the non-adjuvanted and adjuvanted group showed ~10% weight loss (Fig. 7D). However, the N2-MPP + CpG 1018 group did not experience any mortality, whereas in the N2-MPP group one mouse succumbed to infection on day 8 post challenge (Fig. 7E). For the B-NA-MPP vaccination, the unadjuvanted group experienced 10% weight loss, with two mice succumbing to infection on day 3 and 5 post challenge (Fig. 7G, H). However, the B-NA-MPP + CpG 1018 group did not show any morbidity or mortality. The antibody response against the individual NA-MPP antigens was tested via ELISA. In general, non-adjuvanted groups induced a lower immune response compared to the groups receiving NA protein with CpG 1018 (Fig. 7C, F, I).
Female 6–8 week old BALB/c (A–C, G–I) or DBA.2 (D–F) mice (n = 5 per group) were vaccinated in a prime/boost regimen with the respective recombinant protein. Blood was obtained 42 days after the prime and used for serological analysis. A Weight loss curve and B survival curve after challenge with 25xmLD50 of A/Singapore/GP1908/15 H1N1 (IVR-180). Differences in survival were analyzed using a Mantel–Cox log-rank test. N1-MPP vs Neg. Contr. p = 0.0035; N1-MPP + ODN1018 vs Neg. Contr. p = 0.0035; other differences were not statistically significant (p > 0.05). C ELISA against rec. Mich15 N1-VASP protein. D Weight loss curve and E survival curve after challenge with 25xmLD50 of A/Switzerland/9715293/13 (H3N2, mouse adapted). Differences in survival were analyzed using a Mantel–Cox log-rank test. N2-MPP vs Neg. Contr. p = 0.0143; N2-MPP + ODN1018 vs Neg. Contr. p = 0.0027; other differences were not statistically significant (p > 0.05). F ELISA against recombinant N2-VASP protein. G Weight loss and H survival after challenge with 25xmLD50 of B/New York/PV01181/18. Differences in survival were analyzed using a Mantel–Cox log-rank test. B-MPP + ODN1018 vs Neg. Contr. p = 0.0035; other differences were not statistically significant (p > 0.05). I ELISA was performed using serum samples against the rec. B-NA-VASP protein. A, C, D, F, G and I: shown is mean plus standard deviation.
A trivalent NA-MPP vaccine formulation does not induce antigenic competition between the individual NAs and is capable of inducing a strong immune response
Since H1N1, H3N2 and influenza B viruses are all circulating in humans, a trivalent vaccine formulation containing all three NAs would be necessary for protection against all three types of viruses. For this reason, mice (n = 5 per group) were vaccinated either with N1-MPP, N1-MPP + CpG 1018, N1 + N2 + B-NA-MPP, N1 + N2 + B-NA-MPP + CpG 1018 or influenza B virus HA protein (negativ control) in a prime-boost regimen. After vaccination, mice were challenged with 25xmLD50 of A/Singapore/GP1908/15 (H1N1). The group which received N1-MPP alone experienced ~10% weight loss with one mouse which succumb to infection on day 6 (Fig. 8A, B). The other groups did not show any morbidity or mortality. To test if vaccination would also protect against challenge with a heterologous N1 virus, another subset of mice was challenged with 5xmLD50 of A/Vietnam/1203/04 (H5N1, 6:2 A/Puerto Rico/8/34 reassortant, HA polybasic cleavage site removed). While all groups experienced weight loss of ~20%, partial protection was observed in all vaccinated groups with the trivalent, adjuvanted formulation performing best (Fig. 8C, D). In terms of serology, mice which had been vaccinated with N1 + N2 + B-NA-MPP + CpG 1018 had the strongest antibody response in ELISA against recombinant Mich15-VASP protein (Fig. 8E). In an NI assay using H7N1Mich15 the inhibition potential of groups N1-MPP + CpG 1018 and N1 + N2 + B-NA-MPP + CpG 1018 was the highest (Fig. 8F).
Female, 6–8 week old BALB/c mice (n = 5 per group) were vaccinated in a prime/boost regimen with the respective antigens. Blood was obtained 42 days after the prime and used for serological analysis. A Weight loss and B survival curve after challenge with 25xmLD50 of A/Singapore/GP1908/15 H1N1 (IVR-180). Differences in survival were analyzed using a Mantel–Cox log-rank test. N1-MPP vs Neg. Ctrl. p = 0.0143; all other vaccinated groups vs Neg. Ctrl. p = 0.0027; other differences were not statistically significant (p > 0.05). C Weight loss and D survival curve after challenge with 5xmLD50 of A/Vietnam/1203/04 H5N1 (6:2 A/Puerto Rico/8/34 reassortant, polybasic cleavage site removed). Differences in survival were analyzed using a Mantel–Cox log-rank test. N1 + N2 + B-NA-MPP + ODN1018 vs. Neg. Ctrl. (p = 0.0116) was statistically significant, the differences between remaining curves were not statistically significant (p > 0.05). D, E ELISA against rec. Mich15 N1-VASP protein. F NI using the reassortant virus H7N1Mich15. A, C, E, and F are shown as mean plus standard deviation.
Discussion
Influenza virus vaccines provide significant protection against influenza virus infections but the current vaccines are impacted by antigenic drift18,19,20,21,Lung titers Plaque assays for virus titration have been conducted as described previously5. Briefly, confluent MDCK monolayers were infected with different sample dilutions (1:10–1:1.000.000) of homogenized lung tissues diluted in 1× minimum essential medium (MEM) ((1% penicillin/streptomycin antibiotics mix, 1% HEPES, 1% L-glutamine and 1% sodium-bicarbonate (Gibco)) for 1 h at 37 °C. Afterwards, the virus dilution was removed and an overlay consisting out of 2% Oxoid agar (ThermoFisher), H2O, 2× MEM, diethylaminoethyl (0.1% (wt/vol) DEAE) dextran and N-p-Tosyl-L-phenylalanine chloromethyl ketone-treated trypsin (1 µg/ml) was added to the cells. Plates were incubated for 2 days at 37 °C and then fixed using 10% paraformaldehyde overnight at 4 °C. Afterwards, the agar overlay was carefully removed, and the plaques visualized by immunostaining. Plates were blocked for 1 h at RT with 3% milk/PBS. The blocking solution was discarded, and the plates incubated with primary antibody (anti-N1 mAb 4A5) diluted 1:3000 in 1% milk/PBS for 1 h at RT. The plates were washed three times with PBS and the secondary antibody (anti-mouse IgG H&L peroxidase-conjugated (Rockland)) was added for 1 h at RT. The plates were washed three times with PBS and then developed by adding KPL TrueBlue Peroxidase Substrate (SeraCare). The number of plaques was counted (n = 3 per group) and the virus titers presented as the log10 plaque forming units (PFU)/ml. The limit of detection for the assay was at 125 PFU/ml. The graphs were generated using GraphPad Prism 8. Titers were compared using a one-way analysis of variance corrected for multiple comparisons. Survival was compared using a Mantel–Cox log-rank test. All statistical analysis was performed in GraphPad Prism 9.0.1. Further information on research design is available in the Nature Research Reporting Summary linked to this article.Statistical analysis
Reporting summary
Data availability
Underlying data are available from the corresponding author upon reasonable request.
References
Memoli, M. J. et al. Evaluation of antihemagglutinin and antineuraminidase antibodies as correlates of protection in an influenza A/H1N1 virus healthy human challenge model. MBio 7, e00417–00416 (2016).
Couch, R. B. et al. Antibody correlates and predictors of immunity to naturally occurring influenza in humans and the importance of antibody to the neuraminidase. J. Infect. Dis. 207, 974–981 (2013).
Monto, A. S. et al. Antibody to influenza virus neuraminidase: an independent correlate of protection. J. Infect. Dis. 212, 1191–1199 (2015).
Maier, H. E. et al. Pre-existing anti-neuraminidase antibodies are associated with shortened duration of influenza A (H1N1)pdm virus shedding and illness in naturally infected adults. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciz639 (2019).
McMahon, M. et al. Mucosal immunity against neuraminidase prevents influenza b virus transmission in guinea pigs. MBio 10, https://doi.org/10.1128/mBio.00560-19 (2019).
Wohlbold, T. J. et al. Vaccination with adjuvanted recombinant neuraminidase induces broad heterologous, but not heterosubtypic, cross-protection against influenza virus infection in mice. MBio 6, https://doi.org/10.1128/mBio.02556-14 (2015).
Johansson, B. E., Moran, T. M. & Kilbourne, E. D. Antigen-presenting B cells and helper T cells cooperatively mediate intravirionic antigenic competition between influenza A virus surface glycoproteins. Proc. Natl Acad. Sci. USA 84, 6869–6873 (1987).
Krammer, F. et al. NAction! how can neuraminidase-based immunity contribute to better influenza virus vaccines? MBio 9, https://doi.org/10.1128/mBio.02332-17 (2018).
Liu, W. C., Lin, C. Y., Tsou, Y. T., Jan, J. T. & Wu, S. C. Cross-reactive neuraminidase-inhibiting antibodies elicited by immunization with recombinant neuraminidase proteins of H5N1 and pandemic H1N1 influenza A viruses. J. Virol. 89, 7224–7234 (2015).
Strohmeier, S. et al. A novel recombinant influenza virus neuraminidase vaccine candidate stabilized by a measles virus phosphoprotein tetramerization domain provides robust protection from virus challenge in the mouse model. mBio 12, e0224121 (2021).
McMahon, M. et al. Correctly folded - but not necessarily functional - influenza virus neuraminidase is required to induce protective antibody responses in mice. Vaccine 38, 7129–7137 (2020).
Strohmeier, S., Carreño, J. M., Brito, R. N. & Krammer, F. Introduction of cysteines in the stalk domain of recombinant influenza virus n1 neuraminidase enhances protein stability and immunogenicity in mice. Vaccines (Basel) 9, https://doi.org/10.3390/vaccines9040404 (2021).
Campbell, J. D. Development of the CpG adjuvant 1018: a case study. Methods Mol. Biol. 1494, 15–27 (2017).
Jackson, S. et al. Immunogenicity of a two-dose investigational hepatitis B vaccine, HBsAg-1018, using a toll-like receptor 9 agonist adjuvant compared with a licensed hepatitis B vaccine in adults. Vaccine 36, 668–674 (2018).
Chen, Y. Q. et al. Influenza infection in humans induces broadly cross-reactive and protective neuraminidase-reactive antibodies. Cell 173, 417–429.e410 (2018).
Madsen, A. et al. Human antibodies targeting influenza B virus neuraminidase active site are broadly protective. Immunity 53, 852–863.e857 (2020).
Lai, J. C. C., Karunarathna, H. M. T. K., Wong, H. H., Peiris, J. S. M. & Nicholls, J. M. Neuraminidase activity and specificity of influenza A virus are influenced by haemagglutinin-receptor binding. Emerg. Microbes Infect. 8, 327–338 (2019).
Chambers, B. S., Parkhouse, K., Ross, T. M., Alby, K. & Hensley, S. E. Identification of hemagglutinin residues responsible for H3N2 antigenic drift during the 2014-2015 influenza season. Cell Rep. 12, 1–6 (2015).
de Jong, J. C., Beyer, W. E., Palache, A. M., Rimmelzwaan, G. F. & Osterhaus, A. D. Mismatch between the 1997/1998 influenza vaccine and the major epidemic A(H3N2) virus strain as the cause of an inadequate vaccine-induced antibody response to this strain in the elderly. J. Med Virol. 61, 94–99 (2000).
Heikkinen, T., Ikonen, N. & Ziegler, T. Impact of influenza B lineage-level mismatch between trivalent seasonal influenza vaccines and circulating viruses, 1999-2012. Clin. Infect. Dis. 59, 1519–1524 (2014).
Skowronski, D. M. et al. Paradoxical clade- and age-specific vaccine effectiveness during the 2018/19 influenza A(H3N2) epidemic in Canada: potential imprint-regulated effect of vaccine (I-REV). Euro Surveill 24, 1900585 (2019).
**e, H. et al. H3N2 mismatch of 2014-15 northern hemisphere influenza vaccines and head-to-head comparison between human and ferret antisera derived antigenic maps. Sci. Rep. 5, 15279 (2015).
Easterbrook, J. D. et al. Protection against a lethal H5N1 influenza challenge by intranasal immunization with virus-like particles containing 2009 pandemic H1N1 neuraminidase in mice. Virology 432, 39–44 (2012).
Deroo, T., Jou, W. M. & Fiers, W. Recombinant neuraminidase vaccine protects against lethal influenza. Vaccine 14, 561–569 (1996).
Kilbourne, E. D. et al. Protection of mice with recombinant influenza virus neuraminidase. J. Infect. Dis. 189, 459–461 (2004).
Marcelin, G. et al. A contributing role for anti-neuraminidase antibodies on immunity to pandemic H1N1 2009 influenza A virus. PLoS ONE 6, e26335 (2011).
Sandbulte, M. R. et al. Cross-reactive neuraminidase antibodies afford partial protection against H5N1 in mice and are present in unexposed humans. PLoS Med. 4, e59 (2007).
Sylte, M. J., Hubby, B. & Suarez, D. L. Influenza neuraminidase antibodies provide partial protection for chickens against high pathogenic avian influenza infection. Vaccine 25, 3763–3772 (2007).
Acknowledgements
This work was supported in part by the National Institute of Allergy and Infectious Disease (NIAID) Collaborative Influenza Vaccine Innovation Centers (CIVIC) contract 75N93019C00051 and by Dynavax.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
F.K. is listed as an inventor on patent applications regarding NA-based influenza virus vaccines filed by the Icahn School of Medicine at Mount Sinai. J.D.C., P.T., and R.L.C. are present or former employees of Dynavax Technologies and may hold stock or stock options.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Strohmeier, S., Amanat, F., Campbell, J.D. et al. A CpG 1018 adjuvanted neuraminidase vaccine provides robust protection from influenza virus challenge in mice. npj Vaccines 7, 81 (2022). https://doi.org/10.1038/s41541-022-00486-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41541-022-00486-w
- Springer Nature Limited