Abstract
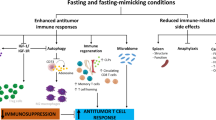
Immune checkpoint inhibitors cause side effects ranging from autoimmune endocrine disorders to severe cardiotoxicity. Periodic Fasting mimicking diet (FMD) cycles are emerging as promising enhancers of a wide range of cancer therapies including immunotherapy. Here, either FMD cycles alone or in combination with anti-OX40/anti-PD-L1 are much more effective than immune checkpoint inhibitors alone in delaying melanoma growth in mice. FMD cycles in combination with anti-OX40/anti-PD-L1 also show a trend for increased effects against a lung cancer model. As importantly, the cardiac fibrosis, necrosis and hypertrophy caused by immune checkpoint inhibitors are prevented/reversed by FMD treatment in both cancer models whereas immune infiltration of CD3+ and CD8+ cells in myocardial tissues and systemic and myocardial markers of oxidative stress and inflammation are reduced. These results indicate that FMD cycles in combination with immunotherapy can delay cancer growth while reducing side effects including cardiotoxicity.
Similar content being viewed by others
Introduction
Immune checkpoint inhibitors (ICIs) boost anti-tumor immune response by mitigating the self-tolerance mechanism of the immune cells, which is hijacked by tumor cells. The clinical application of ICI has profoundly improved prognosis and life expectancy in metastatic cancer patients suffering from melanoma, non-small-cell lung, and kidney cancer, representing a paradigm shift in cancer therapy1,2,3. Immunotherapy is based on the role of cell-surface receptors and ligands accessory to the T-cell receptor in inhibiting cell-mediated immune response. The first monoclonal antibodies targeting this inhibitory axis were developed against the immune checkpoint PD-1 (programmed death-1), its ligand PD-L1 (programmed death ligand-1) and CTLA-4 (cytotoxic T lymphocyte antigen-4). They were first tested in the treatment of melanoma and then applied to the treatment of other cancers characterized by poor prognosis4,5,6,7,8,9,10,11,12. Although ICIs therapy has improved the survival of many cancer patients, the percentage of patients responding remains low. In order to improve efficacy and patient response rates, new therapeutic strategies combining ICIs with adjuvants that augment immune-dependent attack of cancer cells are needed. For example, targeting alternative pathways such as the co-stimulatory molecules OX40, 4-1BB, glucocorticoid-induced TNFR-related protein (GITR) has proven to enhance T-cell mediated immunity in preclinical model13,14,15,16,17, although no clinical studies have confirmed the efficacy of such treatments in humans.
However, ICIs also causes side effects which are uniquely associated with an increase in autoimmunity due to alteration of self-tolerance. A recent study found that 3.5% of patients initiating ICI experience adverse events requiring hospitalization and immunosuppression18,19. Immune-related adverse events (IRAEs) can affect colon, lungs, liver, skin, pituitary, thyroid, and heart20. Although cardiotoxicity accounts for <1% of IRAEs, the onset of such complications, such as myocarditis, arrhythmia, pericarditis and vasculitis results in death in 50% of cases21.
Cardiovascular immune-related adverse events include myocarditis, pericardial disease, vasculitis, Takotsubo syndrome, destabilization of atherosclerotic lesions, venous thromboembolism, and conduction abnormalities22. ICI-associated myocarditis results from inflammation of the conduction system due to infiltration of T cells and macrophages23. Under physiological conditions, the cardiac lymphocyte infiltrate is limited and the macrophages and dendritic cells resident in the heart control the expression of the immune checkpoint proteins in order to maintain homeostasis. Thus, inhibiting the immune checkpoint pathway could lead to adverse outcomes, by promoting the recruitment of lymphocytes and macrophages and triggering an inflammatory response24.
Indeed, in genetically modified mice, deletion of CTLA4 leads to massive lymphoproliferative disease and diffuse lymphocyte infiltration in almost all organs, including the heart. In contrast the deletion of Pdcd1 (encoding PD-1) in Balb/c mice causes cardiomyopathy due to the development of autoantibodies against troponin I25. On the other hand, activation of OX40 with agonistic antibodies stimulates the release of proinflammatory cytokines (IL6, TNFα, IFNγ) by activated T lymphocytes and antigen-presenting cells (APCs)26,27 thus causing a systemic inflammatory response syndrome26,64,65, this condition is associated with systemic inflammation and cytokine storm66 that determines interstitial cardiac infiltration of macrophages or multifocal lymphocytes67. A key factor for the cytokine storm is Interleukin 6 (IL-6) which causes the activation of the T lymphocyte and the release of inflammatory cytokines, generating a positive feedback of immune activation that leads to myocardial damage68.
This study sets the stage for clinical trials aimed at assessing the ability of FMD to increase the efficacy of immunotherapy while reducing its side effects. These results also indicate that the anti-inflammatory and protective effects of FMD cycles in combination with ICI could affect other organs and systems.
Methods
Our studies were carried out in compliance with all relevant ethical regulations. The in vivo experiments on animals were performed according to the protocols approved by the IFOM Institutional Animal Care and Use Committee (IACUC) and the Ministry of Health.
Tumor cell lines
The B16-F10 melanoma tumor cell and LLC1 cell were obtained from ATCC. Cells were grown in DMEM supplemented with 10% fetal bovine serum (FBS), 2 mM l-glutamine, penicillin (100 U ml−1) and streptomycin (100 μg ml−1) at 37 °C with 5% CO2 and maintained at a confluence of 70–80%.
Tumor implantation, Immune checkpoint blockade (ICB) treatment and tumor volume measurement
C57BL/6J female mice, 6–8 weeks old, were purchased from Charles River and housed under pathogen-free conditions at 22 ± 2 °C with 55 ± 10% relative humidity and with 12 h day/light cycles in Cogentech animal facility and with food and water ad libitum. All procedures were carried out in accordance with the guidelines established in the Principles of Laboratory Animal Care (directive 86/609/EEC), were approved by the Italian Ministry of Health, and were performed under the supervision of Institutional Animal Care and Use Committee (OPBA) at IFOM- The AIRC Institute of Molecular Oncology.
In the vivo experiments, tumors were implanted in C57BL/6J mice by injecting subcutaneously (s.c.) 2 × 105 B16-F10 or 5 × 105 LLC1 cells per mouse into the right flank at day 0. Three days after tumor injection, mice from the appropriate groups (at least 5 mice per group) were treated intraperitoneally (i.p.) with anti-PD-L1 (at the dose of 100μg per mouse), anti-OX40 (at dose of 100 μg per mouse), anti-PD1 (at the dose of 100μg per mouse), anti-CTLA4 (at dose of 100 μg per mouse). The ICB therapy was administered every other day for three treatments. The combined anti-OX40/anti-PD-L1 treatment was administered sequentially. The mice were treated with anti-OX40 the first week, while the second week with anti-PD-L1. Anti-PD-1/anti-CTLA4 were administered concurrently on 4, 6 and 8 post-injection day. The mice underwent one or two cycles of FMD (4 days each week) starting the third day after tumor implantation and sacrificed on 21 post-injection day.
One FMD cycle consists of alternating four consecutive days of fasting mimicking diet and three days of refeeding with standard diet. FMD components are described in Brandhorst et al. and Di Biase et al.38,40. Briefly the day 1 diet provides 1.88 kcal/g (50% of normal daily intake) and is made by a mix of various low-calorie broth powders, a vegetable medley powder, extra virgin olive oil, and essential fatty acids mixed with hydrogel; day 2-4 diet contains 0.36 kcal/g (10% of normal day intake) and consist of low-calorie broth powders and glycerol mixed with hydrogel.
Tumors were measured every 3–4 days using a digital caliper; tumor volume was calculated using the formula V = (L × W × H)/2, where V is tumor volume, L is the length of the tumor
(longer diameter), W is the width of the tumor (shorter diameter) and H is the height (diameter of tumor perpendicular to length and width). Mice were monitored for tumor growth and survival. Mice were killed when tumor volume reached 1.5 cm3.
Flow cytometry analysis of tumor-infiltrating lymphocytes and apoptosis
For the flow cytometry analysis of tumor-infiltrating lymphocytes, tumors were minced, B16 were digested for 1 h with Collagenase D (10 mg/ml) and DNAseI (10 mg/ml). Processed tumors were load on Lympholyte gradient and centrifuged at 1500 × g for 30 min. The interphase ring, which contains most live leukocytes cells, was collected and used for FACS staining.
1–2 × 106 cells per sample were stained with the LIVE/DEAD stain (Invitrogen), and then with membrane protein marker (CD45, CD3, CD8, CD4, CD44) followed by fixation with formaldehyde. For intranuclear (Foxp3, Tbet, Klrg1, Eomes, Tcf1/7) and cytoplasmic marker (GzmB) staining, cells were permeabilized and fixed with Foxp3/transcription factor staining kit (Invitrogen eBioscence) or BD cytofix/cyto perm kit (BD bioscences). Data acquisition was performed on Attune NxT Flow Cytometer. Results were analyzed with the FlowJo software. Gating strategies for myeloid and lymphoid cells are illustrated in Supplementary Fig 8.
REAGENT or RESOURCE | SOURCE | IDENTIFIER |
Antibodies FACS | ||
Anti-mouse/human CD44, PB (IM7) | Biolegend | 103020 |
Anti- muse FoxP3, eFluor 506 (FJK-16s) | eBioscience | 69-5773-82 |
Anti-mouse CD274 (PD-L1, B7-H1), Biotin (1-111 A) | eBioscience | 13-9971-81 |
Anti-mouse Eomes, PE (Dan11mag) | eBioscience | 12-4875-82 |
Anti-mouse CD127 (IL-7Rα), PE (A7R34) | Biolegend | 135010 |
Anti-mouse CD8a, PerCP-Vio700 (53-6.7) | Miltenyi Biotec | 130-120-756 |
anti-mouse CD185 (CXCR5), PE/Cy7 (L138D7) | Biolegend | 145516 |
Anti-mouse CD335 (NKp46), PE-eFluor 610 (29A1.4) | eBioscience | 61-3351-82 |
Anti-mouse CD366 (Tim-3), PE/Dazzle 594 (B8.2C12) | Biolegend | 134013 |
Anti-mouse T-bet, AF 647 (4B10) | Biolegend | 644804 |
Anti-mouse/human KLRG1, APC (2F1/KLRG1) | Biolegend | 138412 |
Anti-mouse Ly108, APC (330-AJ) | Biolegend | 134610 |
Anti-mouse CD3, AF 700 (17A2) | eBioscience | 56-0032-82 |
Anti-mouse MRC1, AF 700 (MR6F3) | eBioscience | 56-2061-82 |
Anti-mouse CD25, APC/Cy7 (3C7) | Biolegend | 101918 |
Anti-mouse PD1, Biotin (RMP1-30) | Biolegend | 109106 |
Anti-mouse CD11c, APC-Vio770 (N418) | Miltenyi Biotec | 130-107-461 |
Anti- mouse TCF1/TCF7, AF 488 (C63D9) | Cell Signaling Technology | BK6444S |
Anti-mouse CD11b, VioBlue (REA592) | Miltenyi Biotec | 130-113-810 |
Anti-mouse CD4, VioBright FITC (REA604) | Miltenyi Biotec | 130-118-692 |
Anti-mouse Granzyme B, FITC (REA226) | Miltenyi Biotec | 130-118-341 |
Anti-mouse Ly-6C, FITC (REA796) | Miltenyi Biotec | 130-111-915 |
Anti-mouse MHC Class II, PE (REA813) | Miltenyi Biotec | 130-112-231 |
Anti-mouse CD62L, PE (MEL-14) | Biolegend | 104407 |
Anti-mouse CTLA-4, BV421 (UC10-4B9) | Biolegend | 106311 |
Anti-mouse Ly-6G, PerCP-Vio700 (REA526) | Miltenyi Biotec | 130-117-500 |
Anti-mouse CD45, PE-Vio770 (REA737) | Miltenyi Biotec | 130-110-661 |
Anti-mouse F4/80, APC (REA126) | Miltenyi Biotec | 130-116-525 |
Antibodies in vivo | ||
anti-mouse OX40 (CD134) | BioXcell | BE0031 |
anti-mouse PD-L1 (B7-H1) | BioXcell | BE0101 |
anti-mouse CTLA4 (CD152) | BioXcell | BP0032 |
anti-mouse PD-1 | BioXcell | BE0146 |
Antibodies IHC | ||
Anti-CD3 | Abcam | Ab16669 |
Anti- CD8α | Abcam | Ab217344 |
Anti-Myeloperoxidase | Abcam | Ab208670 |
Anti-B220 | Bd bioscience | 553928 |
Collagen quantification in myocardial tissues
For ex vivo analyses, hearts were excised and fixed in 10% neutral buffered solution. The myocardial tissues were formalin-fixed and paraffin-embedded for morphometry and immunohistochemistry. General morphology was studied using hematoxylin-eosin staining. Sections were stained with hematoxylin/eosin to evaluate the collagen content in tissue. In order to quantify the total collagen content in the heart tissues, measurement of pro-collagen 1α1 (an established biomarker of cardiac fibrosis) was performed using the Mouse Pro-Collagen I alpha 1 CatchPoint SimpleStep ELISA Kit from Abcam (ab229425). Tissues were homogenized, after protein quantification (Bradford assay) 100 µg of proteins were assayed according to manufacturer’s instruction. Fluorescence was measured at 530/590 using a 96-well plate reader Tecan Infinite M200 plate-reader (Tecan Life Sciences Home, Männedorf, Switzerland). Metalloproteases type 9 (MMP-9) were associated with collagen maturation in heart failure, demonstrating the important role of these enzymes in fibrosis through collagen configuration, activation, and deposition. Therefore, we quantified MMP-9 in heart tissues through Mouse MMP9 ELISA Kit (ab253227, Abcam, Milan, Italy) following the manufacturer’s instructions; results are expressed as pg of MMP-9/mg of protein (determined through Bradford assay).
Immunohistochemistry
Mouse tissues were fixed in 10% buffered formalin and paraffin embedded with Diapath automatic processor. To assess histological features Hematoxylin/Eosin (Diapath) staining was performed according to standard protocol and samples were mounted in Eukitt (Bio-Optica).
For immunohistochemical analysis, paraffin was removed with xylene and the sections were rehydrated in graded alcohol. Antigen retrieval was carried out using preheated target retrieval solution (pH 9.0) for 30 minutes. Tissue sections were blocked with FBS serum in PBS for 90 min and incubated overnight with primary antibodies.
For melanoma tumor antibody binding was detected using the conjugated goat anti-rabbit polymer alkaline phosphatase (AP) (Biocare) followed by a Vulcan red chromogen reaction (Peroxidase substrate kit, DAB, SK-4100; Vector Lab).
For lung tumor antibody binding was detected using a polymer detection kit (GAR-HRP, Microtech) followed by a diaminobenzidine chromogen reaction (Peroxidase substrate kit, DAB, SK-4100; Vector Lab). All sections were counterstained with Mayer’s hematoxylin and visualized using a bright-field microscope (LEICA DM750)
For B220 antibody binding was detected using a ABC kit Vectastain (vector, Pk4100) followed by a diaminobenzidine or Magenta chromogen (ENvision flex hrp magenta substrate chromogen system,dako) reaction.
Quantification of CD3+ and CD8+ cells in myocardial tissues
To evaluate for tissue abundance of CD3+ and CD8+ T-cells and diagnosing any myocarditis induced by immunotherapy, formalin-fixed paraffin-embedded (FFPE) sections of heart (4 μm thickness) were stained with rabbit anti mouse CD3 and CD8 antibodies, diluted 1:150 and 1:300 respectively in Dako AR9352 diluent buffer, upon antigen retrieval with 10 mM citrate buffer pH 6 (CD3) or with EDTA antigen retrieval Buffer pH 8 (CD8). Goat anti-rabbit antibodies were used as secondary antibodies for CD3 and CD8.
Visualization of the antibody–antigen reaction was visualized by peroxidase complex kit reagents (SignalStain® DAB Substrate Kit) as the chromogenic substrate. Finally, sections were weakly counterstained with hematoxylin and mounted. Lymphocyte densities (cells/mm2) were quantified by an experienced pathologist (FT).
Quantification of plasma and myocardial cytokines
Cytokines involved in inflammation (IL-1α, IL-1β, IL-2, IL-4, IL-6, IL-10, IL-12, IL17-α, IFN-γ, TNF-α, G-CSF, and GM-CSF) were quantified in heart tissue extracts by using the 12 mouse cytokine Multiplex Assay Kit (Qiagen, Germantown, USA) following the manufacturer’s instructions and summarized in other recent work63. Results were expressed as pg of cytokine/mg of heart tissue.
Quantification of pro-inflammatory biomarkers
After treatments, mice were sacrificed after the proper anesthesia as described before. Hearts were weighed and snap-frozen in dry ice; after, heart tissues were homogenized in a solution 0.1 M PBS (pH 7.4) containing 1% Triton X-100 and protease inhibitor cocktail. Tissues were well homogenized through a step in a high intensity ultrasonic liquid processor. Obtained homogenates were than centrifuged at 4 °C and supernatants were treated for quantification of several inflammation markers. Specifically, leukotriene B4 expression (pg/mL of tissue lysate) was quantified through the LTB4 ELISA Kit (Enzo, Life Technology). Nuclear factor NF-kappa-B p65 subunit (p65-NF-Κb) expression (ng/mL of tissue extract) was quantified through a mouse, rat RelA/NF-kB p65 ELISA Kit (My BioSource, Seattle, WA, USA). NLRP3 inflammasome expression (ng/mL of tissue extract) was quantified by the NLRP3 ELISA Kit (Mouse) (OKEH05486) (Aviva Systems Biology); quantification of systemic and myocardial hydrogen peroxide, a reactive oxygen species (ROS) marker, was performed by using a Fluorimetric Hydrogen Peroxide Assay Kit (Sigma Aldrich, Milan, Italy), in line with other recent work49,69. This kit utilizes a peroxidase substrate that generates a red fluorescent product (λex = 540/λem = 590 nm) after reaction with hydrogen peroxide that was analyzed by a fluorescent microplate reader.
Statistical analysis
GraphPad Prism 9 was used for statistical analysis and graphing. Differences between three or more groups were analyzed using one-way ANOVA followed by post hoc analysis through Tukey’s multiple comparison test. Comparison of CD3 and CD8 immune cell count in heart sections were performed using the Kruskal–Wallis test with post hoc Mann–Whitney U-test. Statistical tests are indicated in the respective sections and figure captions. Differences were considered statistically significant at p value (p) < 0.05. All data are represented as mean ± SEM of three independent experiments.
For in vivo experiments, sample size estimation was performed with G.Power software using a multifactorial variance analysis (ANOVA) repeated measurement, within-between interaction.
A power analysis with significance level α = 0.05, (assuming a large effect size f = 0.4) indicated that n = 8 mice per group are needed to achieve a power (1 – β)=0.9 which is considered adequate to detect difference between means at least of two groups.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data supporting this study, including Supplementary Information and Source Data, are provided with this paper article. All data generated or analysed during this study has been deposited in Figshare, https://doi.org/10.6084/m9.figshare.23283995. Source data are provided with this paper.
References
Admin, U. F. D. KEYTRUDA (pembrolizumab) injection, for intravenous use. (Prescrib. Inf., US Food Drug Admin., Silver Spring, MD., https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/125514s066lbl.pdf, 2020).
Admin, U. F. D. Opdivo (nivolumab). (Drug. Inf., US Food Drug Admin., Silver Spring, MD., https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=125554, 2019).
Admin, U. F. D. Yervoy (ipilimumab). (Drug. Inf.,US Food Drug Admin., Silver Spring, MD, https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=125377, 2019).
Eggermont, A. M. et al. Prolonged survival in stage III melanoma with ipilimumab adjuvant therapy. N. Engl. J. Med. 375, 1845–1855 (2016).
Eggermont, A. M. et al. Adjuvant ipilimumab versus placebo after complete resection of high-risk stage III melanoma (EORTC 18071): a randomised, double-blind, phase 3 trial. Lancet Oncol. 16, 522–530 (2015).
Hodi, F. S. et al. Improved survival with ipilimumab in patients with metastatic melanoma. N. Engl. J. Med. 363, 711–723 (2010).
Larkin, J. et al. Five-year survival with combined Nivolumab and Ipilimumab in advanced melanoma. N. Engl. J. Med. 381, 1535–1546 (2019).
Motzer, R. J. et al. Nivolumab versus Everolimus in advanced renal-cell carcinoma. N. Engl. J. Med. 373, 1803–1813 (2015).
Postow, M. A. et al. Nivolumab and ipilimumab versus ipilimumab in untreated melanoma. N. Engl. J. Med. 372, 2006–2017 (2015).
Reck, M. et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N. Engl. J. Med. 375, 1823–1833 (2016).
Ribas, A. et al. Association of Pembrolizumab with tumor response and survival among patients with advanced melanoma. JAMA 315, 1600–1609 (2016).
Robert, C. et al. Pembrolizumab versus Ipilimumab in advanced melanoma. N. Engl. J. Med. 372, 2521–2532 (2015).
Croft, M. Co-stimulatory members of the TNFR family: keys to effective T-cell immunity? Nat. Rev. Immunol. 3, 609–620 (2003).
Pan, P. Y., Zang, Y., Weber, K., Meseck, M. L. & Chen, S. H. OX40 ligation enhances primary and memory cytotoxic T lymphocyte responses in an immunotherapy for hepatic colon metastases. Mol. Ther. 6, 528–536 (2002).
Piconese, S., Valzasina, B. & Colombo, M. P. OX40 triggering blocks suppression by regulatory T cells and facilitates tumor rejection. J. Exp. Med. 205, 825–839 (2008).
Valzasina, B. et al. Triggering of OX40 (CD134) on CD4(+)CD25+ T cells blocks their inhibitory activity: a novel regulatory role for OX40 and its comparison with GITR. Blood 105, 2845–2851 (2005).
Watts, T. H. TNF/TNFR family members in costimulation of T cell responses. Annu. Rev. Immunol. 23, 23–68 (2005).
Chen, W. et al. Identification of cutaneous immune-related adverse events by International Classification of Diseases codes and medication administration. JAAD Int. 9, 112–115 (2022).
Kalinich, M. et al. Prediction of severe immune-related adverse events requiring hospital admission in patients on immune checkpoint inhibitors: study of a population level insurance claims database from the USA. J. Immunother. Cancer 9, e001935 (2021).
Martins, F. et al. Adverse effects of immune-checkpoint inhibitors: epidemiology, management and surveillance. Nat. Rev. Clin. Oncol. 16, 563–580 (2019).
Mahmood, S. S. et al. Myocarditis in patients treated with immune checkpoint inhibitors. J. Am. Coll. Cardiol. 71, 1755–1764 (2018).
Michel, L., Rassaf, T. & Totzeck, M. Cardiotoxicity from immune checkpoint inhibitors. Int. J. Cardiol. Heart Vasc. 25, 100420 (2019).
Johnson, D. B. et al. Fulminant myocarditis with combination immune checkpoint blockade. N. Engl. J. Med. 375, 1749–1755 (2016).
Grabie, N., Lichtman, A. H. & Padera, R. T cell checkpoint regulators in the heart. Cardiovasc. Res. 115, 869–877 (2019).
Okazaki, T. et al. Autoantibodies against cardiac troponin I are responsible for dilated cardiomyopathy in PD-1-deficient mice. Nat. Med. 9, 1477–1483 (2003).
Barik, S. New treatments for influenza. BMC Med. 10, 104 (2012).
To, K. K. et al. Delayed clearance of viral load and marked cytokine activation in severe cases of pandemic H1N1 2009 influenza virus infection. Clin. Infect. Dis. 50, 850–859 (2010).
Damjanovic, D., Small, C. L., Jeyanathan, M., McCormick, S. & **ng, Z. Immunopathology in influenza virus infection: uncoupling the friend from foe. Clin. Immunol. 144, 57–69 (2012).
Peiris, J. S., Hui, K. P. & Yen, H. L. Host response to influenza virus: protection versus immunopathology. Curr. Opin. Immunol. 22, 475–481 (2010).
Caffa, I. et al. Fasting-mimicking diet and hormone therapy induce breast cancer regression. Nature 583, 620–624 (2020).
Lee, C. et al. Fasting cycles retard growth of tumors and sensitize a range of cancer cell types to chemotherapy. Sci. Transl. Med. 4, 124ra127 (2012).
Nencioni, A., Caffa, I., Cortellino, S. & Longo, V. D. Fasting and cancer: molecular mechanisms and clinical application. Nat. Rev. Cancer 18, 707–719 (2018).
Raffaghello, L. et al. Starvation-dependent differential stress resistance protects normal but not cancer cells against high-dose chemotherapy. Proc. Natl Acad. Sci. USA 105, 8215–8220 (2008).
Vernieri, C. et al. Fasting-mimicking diet is safe and reshapes metabolism and antitumor immunity in patients with cancer. Cancer Discov. 12, 90–107 (2022).
Weng, M. L. et al. Fasting inhibits aerobic glycolysis and proliferation in colorectal cancer via the Fdft1-mediated AKT/mTOR/HIF1alpha pathway suppression. Nat. Commun. 11, 1869 (2020).
Ajona, D. et al. Short-term starvation reduces IGF-1 levels to sensitize lung tumors to PD-1 immune checkpoint blockade. Nat. Cancer 1, 75–85 (2020).
Cortellino, S. et al. Fasting renders immunotherapy effective against low-immunogenic breast cancer while reducing side effects. Cell Rep. 40, 111256 (2022).
Di Biase, S. et al. Fasting-mimicking diet reduces HO-1 to promote T cell-mediated tumor cytotoxicity. Cancer Cell 30, 136–146 (2016).
Pietrocola, F. et al. Caloric restriction mimetics enhance anticancer immunosurveillance. Cancer Cell 30, 147–160 (2016).
Brandhorst, S. et al. A periodic diet that mimics fasting promotes multi-system regeneration, enhanced cognitive performance, and healthspan. Cell Metab. 22, 86–99 (2015).
Cheng, C. W. et al. Prolonged fasting reduces IGF-1/PKA to promote hematopoietic-stem-cell-based regeneration and reverse immunosuppression. Cell Stem Cell 14, 810–823 (2014).
Longo, V. D. & Cortellino, S. Fasting, dietary restriction, and immunosenescence. J. Allergy Clin. Immunol. 146, 1002–1004 (2020).
Wei, M. et al. Fasting-mimicking diet and markers/risk factors for aging, diabetes, cancer, and cardiovascular disease. Sci. Transl. Med. 9, eaai8700 (2017).
Collins, N. et al. The bone marrow protects and optimizes immunological memory during dietary restriction. Cell 178, 1088–1101.e1015 (2019).
Jordan, S. et al. Dietary intake regulates the circulating inflammatory monocyte pool. Cell 178, 1102–1114.e1117 (2019).
Choi, I. Y. et al. A diet mimicking fasting promotes regeneration and reduces autoimmunity and multiple sclerosis symptoms. Cell Rep. 15, 2136–2146 (2016).
Rangan, P. et al. Fasting-mimicking diet modulates microbiota and promotes intestinal regeneration to reduce inflammatory bowel disease pathology. Cell Rep. 26, 2704–2719.e2706 (2019).
Messenheimer, D. J. et al. Timing of PD-1 blockade is critical to effective combination immunotherapy with anti-OX40. Clin. Cancer Res. 23, 6165–6177 (2017).
Quagliariello, V. et al. NLRP3 as putative marker of ipilimumab-induced cardiotoxicity in the presence of hyperglycemia in estrogen-responsive and triple-negative breast cancer cells. Int. J. Mol. Sci. 21, 7802 (2020).
Quagliariello, V. et al. Immune checkpoint inhibitor therapy increases systemic SDF-1, cardiac DAMPs Fibronectin-EDA, S100/Calgranulin, galectine-3, and NLRP3-MyD88-chemokine pathways. Front. Cardiovasc. Med. 9, 930797 (2022).
Colazzo, F., Gelosa, P., Tremoli, E., Sironi, L. & Castiglioni, L. Role of the cysteinyl leukotrienes in the pathogenesis and progression of cardiovascular diseases. Mediators Inflamm. 2017, 2432958 (2017).
Hafstrom, I., Ringertz, B., Gyllenhammar, H., Palmblad, J. & Harms-Ringdahl, M. Effects of fasting on disease activity, neutrophil function, fatty acid composition, and leukotriene biosynthesis in patients with rheumatoid arthritis. Arthritis Rheum. 31, 585–592 (1988).
De Gomez Dumm, I. N., De Alaniz, M. J. & Brenner, R. R. Effect of diet on linoleic acid desaturation and on some enzymes of carbohydrate metabolism. J. Lipid Res. 11, 96–101 (1970).
Liu, S. et al. Cardiovascular toxicity with PD-1/PD-L1 inhibitors in cancer patients: a systematic review and meta-analysis. Front. Immunol. 13, 908173 (2022).
Salem, J. E. et al. Cardiovascular toxicities associated with immune checkpoint inhibitors: an observational, retrospective, pharmacovigilance study. Lancet Oncol. 19, 1579–1589 (2018).
Wang, Y. et al. Adverse event reporting quality in cancer clinical trials evaluating immune checkpoint inhibitor therapy: a systematic review. Front. Immunol. 13, 874829 (2022).
Duhen, R. et al. Neoadjuvant anti-OX40 (MEDI6469) therapy in patients with head and neck squamous cell carcinoma activates and expands antigen-specific tumor-infiltrating T cells. Nat. Commun. 12, 1047 (2021).
Glisson, B. S. et al. Safety and clinical activity of MEDI0562, a humanized OX40 agonist monoclonal antibody, in adult patients with advanced solid tumors. Clin. Cancer Res. 26, 5358–5367 (2020).
Gutierrez, M. et al. OX40 agonist BMS-986178 alone or in combination with Nivolumab and/or Ipilimumab in patients with advanced solid tumors. Clin Cancer Res. 27, 460–472 (2021).
Wang, R. et al. An integrative approach to inform optimal administration of OX40 agonist antibodies in patients with advanced solid tumors. Clin. Cancer Res. 25, 6709–6720 (2019).
Bergendahl, M., Vance, M. L., Iranmanesh, A., Thorner, M. O. & Veldhuis, J. D. Fasting as a metabolic stress paradigm selectively amplifies cortisol secretory burst mass and delays the time of maximal nyctohemeral cortisol concentrations in healthy men. J. Clin. Endocrinol. Metab. 81, 692–699 (1996).
Carbone, A. et al. Takotsubo cardiomyopathy as epiphenomenon of cardiotoxicity in patients with cancer: a meta-summary of case reports. J. Cardiovasc. Pharmacol. 78, e20–e29 (2021).
Quagliariello, V. et al. The SGLT-2 inhibitor empagliflozin improves myocardial strain, reduces cardiac fibrosis and pro-inflammatory cytokines in non-diabetic mice treated with doxorubicin. Cardiovasc. Diabetol. 20, 150 (2021).
Annie, F. H., Alkhaimy, H., Nanjundappa, A. & Elashery, A. Association between myocarditis and mortality in COVID-19 patients in a large registry. Mayo Clin. Proc. Innov. Qual. Outcomes 6, 114–119 (2022).
Witberg, G. et al. Myocarditis after Covid-19 vaccination in a large health care organization. N. Engl. J. Med. 385, 2132–2139 (2021).
Guo, T. et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 5, 811–818 (2020).
Basso, C. et al. Pathological features of COVID-19-associated myocardial injury: a multicentre cardiovascular pathology study. Eur. Heart. J. 41, 3827–3835 (2020).
Siripanthong, B. et al. Recognizing COVID-19-related myocarditis: the possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm 17, 1463–1471 (2020).
Terme, M. et al. IL-18 induces PD-1-dependent immunosuppression in cancer. Cancer Res. 71, 5393–5399 (2011).
Acknowledgements
We are thankful to IFOM and Cogentech facility for technical support. This work was supported by the Associazione Italiana per la Ricerca sul Cancro (AIRC; IG#17605 and IG#21820).
Author information
Authors and Affiliations
Contributions
S.C., V.Q., E.V., O.B., A.S., S.L. and V.S. performed all the in vivo and in vitro experiment. G.D. and C.C. carried out FACS analysis. A.D., F.T. and F.P. performed IHC analysis. G.C., P.D., C.T. and N.M. provides expertise and feedback. All authors discussed the results and contributed to the final manuscript. S.C., V.Q., and V.L. conceived and designed the study and drafted the manuscript.
Corresponding author
Ethics declarations
Competing interests
V.D.L. holds intellectual property rights on clinical uses of FMD and equity interest in L-Nutra, a company that markets medical food. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Michael Greene, Camelia Quek and the other anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cortellino, S., Quagliariello, V., Delfanti, G. et al. Fasting mimicking diet in mice delays cancer growth and reduces immunotherapy-associated cardiovascular and systemic side effects. Nat Commun 14, 5529 (2023). https://doi.org/10.1038/s41467-023-41066-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-023-41066-3
- Springer Nature Limited
This article is cited by
-
Fasting-mimicking diet remodels gut microbiota and suppresses colorectal cancer progression
npj Biofilms and Microbiomes (2024)
-
Fasting and fasting-mimicking conditions in the cancer immunotherapy era
Journal of Physiology and Biochemistry (2024)