Abstract
Background
Uncorrected refractive error (URE) is a readily treatable cause of visual impairment (VI). This study provides updated estimates of global and regional vision loss due to URE, presenting temporal change for VISION 2020
Methods
Data from population-based eye disease surveys from 1980–2018 were collected. Hierarchical models estimated prevalence (95% uncertainty intervals [UI]) of blindness (presenting visual acuity (VA) < 3/60) and moderate-to-severe vision impairment (MSVI; 3/60 ≤ presenting VA < 6/18) caused by URE, stratified by age, sex, region, and year. Near VI prevalence from uncorrected presbyopia was defined as presenting near VA < N6/N8 at 40 cm when best-corrected distance (VA ≥ 6/12).
Results
In 2020, 3.7 million people (95%UI 3.10–4.29) were blind and 157 million (140–176) had MSVI due to URE, a 21.8% increase in blindness and 72.0% increase in MSVI since 2000. Age-standardised prevalence of URE blindness and MSVI decreased by 30.5% (30.7–30.3) and 2.4% (2.6–2.2) respectively during this time. In 2020, South Asia GBD super-region had the highest 50+ years age-standardised URE blindness (0.33% (0.26–0.40%)) and MSVI (10.3% (8.82–12.10%)) rates. The age-standardized ratio of women to men for URE blindness was 1.05:1.00 in 2020 and 1.03:1.00 in 2000. An estimated 419 million (295–562) people 50+ had near VI from uncorrected presbyopia, a +75.3% (74.6–76.0) increase from 2000
Conclusions
The number of cases of VI from URE substantively grew, even as age-standardised prevalence fell, since 2000, with a continued disproportionate burden by region and sex. Global population ageing will increase this burden, highlighting urgent need for novel approaches to refractive service delivery.
Similar content being viewed by others
Introduction
Uncorrected refractive error (URE) is the leading cause of vision impairment globally among both adults and children, and contributes to reduced educational and economic opportunities [1,2,3,4,5,6], decreased quality of life [7] and an increased burden of mortality [8,9,10]. Visual impairment is a significant global health concern and the financial burden with global productivity losses is estimated to be 411 billion US dollars annually [11]. URE is readily treated with spectacles, making it one of the most cost-effective healthcare interventions, alongside cataract surgery [12,13,14,15]. Thus, it is a global priority to improve access to refraction services [11], as set out in ‘Towards universal eye health: Global Action Plan 2014–2019 of the World Health Assembly (WHA) in 2013 [16]. and more recently in the ‘World Report on Vision’ by the World Health Organisation (WHO) in 2019 [17], which called for the routine measurement of refractive error services coverage as a means to address the United Nations (UN) Sustainable Development Goals [18] target 3.8 to “achieve universal health coverage, including financial risk protection, access to quality essential healthcare services and access to safe, effective, quality and affordable essential medicines and vaccines for all”. Furthermore, these recommendations have been adopted in a resolution by the 73rd WHA member states in 2021, which set global targets for a 40% increase in effective refractive error coverage (eREC) by 2030. As we transition from the efforts of VISION 2020: the Right to Sight initiative to tackle avoidable blindness, these focused targets are fundamental to eliminate avoidable vision loss in future.
Refractive error is a common ocular condition which occurs throughout the lifespan [19], and chiefly falls into the following categories: myopia (affecting mostly distance vision), hyperopia (potentially causing impaired vision at distance and near), which may both be accompanied by an astigmatic component, and presbyopia (characterised by poor near vision). The last 20 years have seen rapid increases in the prevalence of myopia across the world, particularly in East Asia [20,21,22,23].
Nearly all individuals, even those without significant refractive error in childhood and earlier adult years will acquire presbyopia by the 5th decade of life, necessitating refractive correction for near work. Presbyopia occurs due to reduced flexibility of the human crystalline lens to accommodate (focus) on near targets, resulting in blurred near vision. It is an essentially universal phenomenon, with age of onset determined by factors such as the presence of latent hyperopia. Without refractive correction, vision deteriorates for near activities, resulting in near visual impairment. Where uncorrected hyperopia is common, due to lack of access to both education (which induces myopia [24]) and refractive services, the onset of presbyopia may even occur in the 30 s, which is a critical working age for those in industries such as garments and textiles [25, 26]. With an ageing global population, the burden of presbyopia and near visual impairment will increase. Coupled with the impact of the increased prevalence of myopia, the burden of URE is likely to grow in the future.
The Vision Loss Expert Group (VLEG) curate a comprehensive, continuously updated, online database of ophthalmic epidemiological data and have made important contributions to knowledge about the burden and causes of vision impairment and blindness globally [27,28,29]. These estimates have been used in the WHO Report on Vision in 2019 [17] and the recent Lancet Global Health commission on Global Eye Health Report [15]. Updated analyses are required to reflect rapidly increasing sources of new population data, and to monitor progress in reduction of avoidable sight loss. The need for new population data on vision impairment has been emphasised in a recent paper highlighting the grand challenge priorities for global eye health [30], and will be vital to monitor and measure success against the WHA global target of a 40% increase in eREC.
Thus, the aim of the current study is to provide updated estimates of the global burden of vision loss due to URE, disaggregated by sex, age, year and region, for the period from 2000 to 2020 covered by VISION 2020: The Right to Sight initiative. For the first time, temporal trends will be calculated to present the burden of visual impairment resulting from uncorrected presbyopia in those 50+ years.
Methods
A systematic review of population-based studies of vision impairment and blindness published between Jan 1, 1980, and Oct 1, 2018, was carried out, which included grey literature sources. Eligible studies from this review were then combined with data from Rapid Assessment of Avoidable Blindness (RAAB) studies and finally, data from the US National Health and Nutrition Examination Survey and the WHO Study on Global Ageing and Adult Health were added. More detailed methods are published elsewhere [30, 31], and outlined below.
In total, the VLEG review identified 243 studies (73% were rapid studies) across 73 countries from which data relating to the contribution of URE to vision loss could be extracted: with 70 studies from the 2010 review [28], and a further 173 studies in an extension of the literature review to 2018 [29]. Studies were primarily national and subnational cross-sectional surveys. By the seven World Global Burden of Disease (GBD) super regions, 43 studies were from Sub-Saharan Africa, 100 from Southeast Asia, East Asia, and Oceania, 44 from South Asia, 16 from North Africa and the Middle East, 25 from Latin America and the Caribbean, 9 from High income, and 6 from Central Europe, Eastern Europe, and Central Asia. Additionally, the VLEG commissioned the preparation of 5-year age-disaggregated RAAB data from the RAAB repository. Studies were included if they met the following criteria: visual acuity data had to be measured using a test chart that could be mapped to the Snellen scale, and the sample had to be representative of the population. Studies based on self-report of vision loss were excluded. The International Classification of Diseases 11th edition [32] criteria for vision loss, as suggested by WHO, was employed, categorizing individuals according to vision in their better eye on presentation. This classification defines moderate vision loss as visual acuity of 6/60 or better but less than 6/18, severe vision loss as a visual acuity of 3/60 or better but less than 6/60, and blindness as visual acuity of less than 3/60 or less than 10° visual field around central fixation (although the visual field definition is rarely used in population-based eye surveys). Moderate and severe visual impairment (MSVI) was combined to present prevalence data. Vision impairment from uncorrected presbyopia was defined as presenting near vision of worse than <N6 or <N8 at 40 cm where best-corrected distance visual acuity was 6/12 or better. Prevalence of near VI from uncorrected presbyopia was based on 25 studies.
The global and regional prevalence and burden of blindness and MSVI due to URE were gathered from the all-cause meta-analysis and modelling. First, we separated raw data into datasets including so-called vision loss envelopes (see Flaxman et al. [28]. for explanation) for all-cause mild, moderate, and severe vision loss, and blindness. Data were input into a mixed-effects meta-regression tool developed by the Institute for Health Metrics and Evaluation and called MR-BRT (meta-regression; Bayesian; regularised; trimmed) [33]. Presenting vision impairment was the reference definition for each level of severity. Prevalence data for URE were extracted directly where available and otherwise calculated by subtracting best-corrected vision impairment from presenting vision impairment prevalence for each level of severity in studies that reported both measures for a given location, sex, age group, and year. All other causes were quantified as part of the best-corrected estimates of vision impairment at each level of severity.
We modelled distance vision impairment and blindness attributable to the following causes: cataract, URE, age-related macular degeneration, myopic macular degeneration, glaucoma, diabetic retinopathy, and other causes of vision impairment (in aggregate).
We produced location-, year-, age-, and sex-specific estimates of MSVI and blindness using Disease Modelling Meta-Regression (Dismod-MR) 2.1 [34]. The details of the data processing steps are described elsewhere [29]. Briefly, Dismod-MR 2.1 models were run for all vision impairment stratified by severity (moderate, severe, blindness) regardless of cause and, separately, for MSVI and blindness due to each modelled cause of vision impairment. Then, models of MSVI due to specific causes were split into moderate and severe vision loss estimates using the ratio of overall prevalence in the all-cause moderate presenting vision impairment and severe presenting vision impairment models. Next, prevalence estimates for all causes stratified by severity were scaled to the models of all-cause prevalence by severity. This produced final estimates by age, sex, year, and location for each individual cause of vision impairment stratified by severity, including refractive error. Model projection was to the year 2020, coincident with the end of VISION 2020: the Right to Sight initiative, and estimates were age-standardised using the GBD standard population [35]. All generated estimates for visual impairment due to URE are accompanied by 95% uncertainty intervals (UI), which represent the 25th and 975th ordered estimates of 1000 draw estimates of the posterior distribution. We considered estimates to be significantly different if the 95% UIs did not overlap. Data are presented for the total population and also for individuals aged 50+ years, as data sources such as RAAB surveys are major sources of data for low-income and low- or middle-income countries (LICs and LMICs) and these surveys are conducted on individuals aged 50 years and older. The data estimates reported in this study were produced in compliance with the Guidelines for Accurate and Transparent Health Estimates Reporting [36].
Data are presented for the seven World super-regions based on the GBD regional classification system [37], and sub-divided into the 21 GBD world regions. These seven super regions are drawn together based on two criteria: epidemiological similarity and geographic proximity.
Results
We used 243 data sources from 73 countries to calculate the global and regional prevalence and burden of blindness and MSVI due to URE. Table 1 presents the number of people, men and women, with blindness (<3/60) or MSVI (<6/18 to >/=3/60) due to URE in 2020 in the seven super-regions based on the GBD classification system. Appendix 1 contains supplementary tables for all 21 GBD world regions in 2020. These estimates reveal that in 2020, 3.70 million people (95% UI 3.10–4.29 million) in the world were blind and 157 million (95% UI 140–175 million) had MSVI due to URE. Focusing on those 50+ years of age, 2.29 million people (95% UI 1.79–2.80 million) were blind due to URE globally and 86.1 million (95% UI 74.2–101 million) had MSVI.
As a percentage of all types of blindness, the burden of blindness due to URE globally is 8.60% (95% UI 7.22–9.99%) and is greatest for the super regions of South Asia (12.71%, 95% UI 10.58–14.82%) and Southeast Asia, East Asia and Oceania (9.34%, 95% UI 7.67–10.94%). These updated data estimate that URE is the leading cause of MSVI globally, accounting for 53.39% (95% UI 47.56–59.51%) of all cases. Focusing on blindness due to URE in those aged 50+ years, South Asia accounts for the largest age-standardised prevalence (0.33% (95% UI 0.26–0.40%)), followed by the super-regions of Southeast Asia, East Asia and Oceania (0.15% (95% UI 0.12–0.18%)) and Sub-Saharan Africa (0.11% (95% UI 0.09–0.14%)).
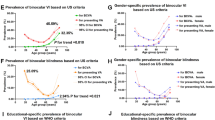
The overall age-standardised prevalence of blindness due to URE in those aged 50+ years was 0.12% (95% UI 0.10–0.15%), and 4.58% for MSVI (95% UI 3.96–5.37%). Figure 1 shows the number of men and women aged 50+ years with blindness and MSVI due to URE in 2020 in the seven World GBD super regions, and includes the global total for overall comparison. Figure 2 presents the crude prevalence of blindness and MSVI due to URE in 2020 across super regions.
a Crude prevalence of blindness due to URE in 2020 by seven World GBD super regions by age. b Crude prevalence of MSVI due to URE in 2020 by seven World GBD super regions by age. c Crude prevalence of Blindness (red) and MSVI (cyan) due to URE in 2020 globally by age, with 95% UI indicated as shading.
Table 2 presents the percentage change in crude prevalence of MSVI and blindness due to URE in men and women aged 50 years and older between 2000 and 2020 for the seven World GBD super regions (see Appendix 1 for all 21 GBD World regions). Over this time period the number of cases of blindness and MSVI increased by +21.8% and +72.0%% respectively, with the greatest increase in the Latin America and Caribbean super-region for both blindness and MSVI. However, the age-standardised prevalence of URE blindness in those 50+ years decreased significantly, by −30.5% (95% UI −30.7 to −30.3) during this time period. The global age-standardised prevalence of MSVI due to URE in those aged 50+ years modestly decreased by −2.4% (95% UI −2.6 to −2.2%) between 2000 and 2020, but with some regional variations. The Latin America and Caribbean super-region demonstrated a slight increase in age-standardised prevalence of MSVI due to URE of +0.8% (95% UI + 0.7 to +1.0%), and the High-Income super-region had no change (+0.1%, 95% UI −0.1 to +0.3).
By a clear margin, South Asia had the highest regional 50+ years age-standardised URE blindness and MSVI prevalence in 2020 (blind: 0.3%, 95% UI 0.3–0.4; MSVI: 10.3%; 95% UI 8.8–12.1%) (Table 1), but also demonstrated the greatest reductions in age-standardised URE blindness between 2000 and 2020 (−46.3% (95% UI −46.5 to −46.2%)) (Table 2).
Globally, the age-standardized ratio of women to men for URE blindness was 1.05:1.00 in 2020 and 1.03:1.00 in 2000. For MSVI, this ratio was 1.08:1.00 in 2020 and 1.06:1.00 in 2000. Thus, in 2020, women continue to suffer an excess burden, with the age-standardized prevalence of women exceeding that of men by 4.76% for URE blindness and 7.40% for URE MSVI. Men exhibited a greater 20-year reduction in age-standardised prevalence compared to women for both blindness and MSVI: MSVI −3.0% (95% UI −3.1 to −2.8) in men, −2.0% (95% UI −2.2 to −1.8) in women; blindness −31.6% (95% UI −31.8 to −31.4) in men, −29.9% (95% UI −30.0 to −29.7) in women. Regionally, women have made smaller gains than men in the reduction of age−standardised prevalence of MSVI due to URE, particularly in the super regions of Central Europe, Eastern Europe and Central Asia, North Africa and Middle East, and Latin America and Caribbean. In the High-Income super-region, age-standardised prevalence of blindness has actually increased modestly for woman at +1.0% (95% UI 0.8 to 1.2%) compared to men −0.1% (95% UI −0.3 to 0.0). However, it is notable that in South Asia, there has been a greater reduction in age-standardised prevalence of both blindness and MSVI for women compared to men (percentage reduction blindness; women −50.0% (95% UI −50.2 to −49.9), men −42.1% (95% UI −42.2 to −41.9): percentage reduction MSVI; women −8.9% (95% UI −9.1 to −8.8), men −4.3% (95% UI −4.5 to −4.1)), although the burden remains substantial.
Table 3 presents the number of people, men and women with near VI from uncorrected presbyopia in the seven super regions. In 2020, an estimated 419 million (95% UI 295–562 million) people aged 50+ had near VI from uncorrected presbyopia globally, with an age-standardised prevalence of 22.3% (95% UI 15.8–29.9%). Approximately 70% of global near VI from presbyopia occurred in two super regions: South Asia and Southeast Asia, East Asia and Oceania (293 million).
Table 4 presents the percentage change in crude prevalence of near VI due to uncorrected presbyopia in men and women aged 50 years and older between 2000 and 2020. Over this time period, the number of cases of near VI due to presbyopia increased substantially (+75.3% (95% UI + 74.6 to +76.0)), while the crude prevalence demonstrated a modest reduction for men (−1.8% (95% UI −2.2 to −1.4%)), but an increase of +0.8% (95% UI 0.4–1.2%) for women. Figure 3 further illustrates these sex differences across super regions, demonstrating significant increases in the number of cases in the 20-year period, with a disproportionate increase for women. The number of cases of near VI due to presbyopia increased in all super regions, ranging from 25.5% (95% UI + 25.0 to +25.9%) in Central Europe, Eastern Europe, and Central Asia to 101% (95% UI + 100.2 to +101.7%) in Latin America and Caribbean super-region. However, the percentage change in crude prevalence decreased in all super regions over the 20-year period except for the High-Income super-region which had a +4.3% (95% UI + 3.9 to +4.7) increase.
Discussion
This study provides up-to-date global and regional, sex-specific and age-specific estimates and temporal trends for vision impairment due to URE, both for distance and near vision impairment. Our study reveals that URE remains a leading cause of MSVI, affecting 157 million individuals worldwide in 2020, and MSVI due to URE accounts for 57% of all MSVI globally. Notably, although there is some variation across the super regions, the percentage of MSVI due to URE remains above 47% in all areas, underscoring the persistent and substantial global burden of avoidable vision loss caused by URE.
In the 20-year period up to 2020, VISION 2020: the Right to Sight initiative sought to prevent avoidable sight loss, and the subsequent Global Action Plan adopted by the WHA in 2013 set a target for a 25% reduction in the prevalence of avoidable vision impairment by 2019 from the baseline of 2010. While progress in reducing the global burden has been made, this target was not achieved [29], highlighting the need for continued focus and effort to eliminate avoidable sight loss.
Encouragingly, the age-standardised prevalence of blindness due to URE in those aged 50+ years has decreased substantially from 2000 to 2020, potentially reflecting the targeted efforts countries have adopted to tackle severe sight loss. This may in part be explained by the increased use of intra-ocular lenses in cataract surgery over the last 20–30 years, leading to a reduction in blindness due to aphakia [38]. In contrast, the age-standardised prevalence of MSVI due to URE in those aged 50+ years only decreased modestly between 2000 and 2020.
The reductions we observed in age-standardised prevalence are counterbalanced by a striking increase in the unadjusted burden of blindness and MSVI due to URE, meaning that the total number of affected persons in the world has risen. This is driven by two key factors: continued global population growth, which is estimated to reach 10.4 billion in 2100, and an ageing population [39]. In common with the majority of vision-impairing ocular diseases, the likelihood of MSVI and blindness due to URE rapidly increases with age, as shown in Fig. 2. UN projections report that between 2020 and 2050 the global population of those aged 65+ years is expected to double from 703 million to 1.5 billion, and that by 2050, one in six people in the world will be aged ≥ 65 years [40].
The super-region of South Asia, comprising countries including India and Pakistan, had the greatest burdens of blindness and MSVI, with a disproportionately high prevalence of older age groups. While globally there was a reduction in age-standardised prevalence of MSVI due to URE, the super-region of Latin America and Caribbean actually demonstrated an increase of +0.8% (95% UI 0.4–1.3). These regional differences in the prevalence of vision loss are likely due to variations in availability of affordable refractive services, particularly in rural locations, and in social conditions. This is evidenced by a recent study investigating the eREC across regions, which demonstrated substantial differences in eREC between super regions in 2021, with 79.1% coverage in the High-Income super-region (95% CI 72·4–85·0), compared to 6.7% in Sub-Saharan Africa (95% CI 3·1–9·0) and 9.0% in South Asia (95% CI 6·5–12·0%) [41].
New eyecare service development has not kept pace with the increasing population demands in any region of the world, and continued population ageing will further increase existing burdens. Alleviating this shortfall will require a combination of capacity-building of trained eyecare personnel, expansion of community-based screening services for diagnosis of refractive errors, development of infrastructure for spectacle provision, outreach efforts to drive demand, and novel technical approaches to allow more services to be delivered by available, less fully-trained cadres. The WHO World Report on Vision, 2019 [17] sets out four key areas to increase access to eyecare services: (i) Increase of the availability of services through training and improved infrastructure; (ii) Increase the accessibility of services to those who need them; (iii) Increase the affordability of services, and (iv) Increase of the acceptability of refractive services, through awareness raising.
While the burden of vision impairment increases with age, focusing only on the population aged 50 years and above provides an incomplete view of vision impairment due to URE, which also frequently affects younger persons. While we report that those aged 50+ years with MSVI total 86 million in 2020, this only accounts for 55% of all MSVI (167 million). For younger people, the burden of URE is likely driven by the concerning global increase in myopia [42], with recent evidence showing these trends are not only confined to Asian populations [43]. However, there remains a paucity of data on vision impairment due to URE in children and younger adults, which needs to be redressed.
A disproportionate number of women continue to be affected by vision impairment due to URE. This is observed globally and across the majority of super regions. Interestingly for presbyopia, while the global crude prevalence decreased for men by −1.8% (−2.2 to −1.4%) from 2000 to 2020, there was an increase for women of +0.8% (+0.4 to +1.2%). It is important to emphasise that these differences persist after age adjustment, and are not simply an artefact of women living longer. This unfair burden among women is likely driven by cultural and social inequities, with less financial autonomy, male prioritisation, and child- and home-care responsibilities [44]. This persistent gap must be addressed through targeted strategies to increase their access to refractive care.
The burden of near visual impairment due to uncorrected presbyopia is another critical area of concern highlighted by our study, with nearly 420 million people aged 50+ years affected by uncorrected presbyopia. There are huge disparities in the age-standardised prevalence of uncorrected presbyopia across super regions, with for example, only a 2.4% prevalence in the High-Income super-region compared with 38.9% in South Asia. This finding is supported by a systematic review reporting the greatest burden of presbyopia in rural areas in low-resource countries [45]. Looking at temporal data, some super regions demonstrated a reduction in crude prevalence but in all areas the number of cases increased significantly, likely due to the ageing population globally and also improvements in data availability in the last 20 years. It was not possible to generate age-standardised estimates due to sparsity of data. The combination of high, rapidly rising burden and the paucity of data underscores the need for more attention to presbyopia among both researchers and health service planners.
The large burden of uncorrected presbyopia may in part reflect a view that correction for near VI is somehow less important than for distance VI, but studies have shown that vision impairment from URE affects the quality of life to a similar degree whether at distance or near VI [14]. Furthermore, a recent study [46] reported on the considerable productivity loss from un- and under-corrected presbyopia in LICs and LMICs. Using GBD data, the authors estimated 238 million people of working age (15–65 years) in LMICs had uncorrected presbyopia, and estimated the resulting direct productivity loss at $54 billion dollars, using productivity-adjusted-life-years. The potential for presbyopic correction to improve real-world work productivity is underscored by recent trials [2].
The strengths of this updated review and data analysis up to 2020 include the addition of new data sources, particularly more RAAB surveys, which enable improvements in disaggregation by cause and a wider coverage of geographical regions in our analysis. This is also the first time we combine reports on the impact of distance and near visual impairment due to URE and presbyopia. However, there remain several LICs and LMICs in regions such as central sub-Saharan Africa, Central Asia, and central and eastern Europe, with scant population-based data where estimates rely on extrapolation from other regions. While our modelling has controlled for a range of confounding factors, it is possible that blindness and MSVI due to URE are underreported. Furthermore, due to data sparsity, we did not include mild visual impairment in this dataset but used a definition of <6/18 for MSVI, so again these data underreport the potential burden of distance vision impairment compared to other studies. Finally, it is possible that the trajectory of the prevalence of vision impairment due to URE might be altered owing to the COVID-19 global pandemic, with reports emerging of an increase in the prevalence of myopia attributed to changes in lifestyle during the pandemic [47]. Future directions for research and policy should be develop population screening services, accurate reporting mechanisms and registries to effectively measure the burden of avoidable vision impairment due to URE, to strengthen data from younger populations, and focus efforts on develo** refractive services in LICs and LMICs to fill the data gaps to achieve greater geographical coverage.
Conclusions
Data from the last 20 years show that the absolute number of people with URE is rising due to population growth and ageing. URE remains a leading global cause of MSVI among persons aged 50+ years, affecting 86 million individuals and accounting for 53.4% of the total figure. This, coupled with the huge burden of near vision impairment due to uncorrected presbyopia, highlights the urgent need for novel and fresh approaches to refractive service delivery. While progress has been made in the last two decades, a reduction in the burden of vision impairment from URE can be realised by adding refractive services to universal health coverage and otherwise improving availability of, and access to, spectacle provision. Though the need is greater in some global regions, URE has not been fully addressed anywhere, and the resulting productivity losses and reduction in quality of life should not be overlooked for any country. Over this decade, the target set by the 73rd WHA member states in 2021, a 40% increase in eREC by 2030, will provide critical leverage to accelerate our efforts to tackle avoidable blindness due to URE.
URE remains the leading cause of MSVI, though spectacle provision is the simplest and least invasive treatment available for any ocular condition. This is a source of frustration after decades of work on VISION 2020, but it underscores the opportunity to accelerate progress towards what is arguably the most attainable goal in vision care, that of eliminating URE.
Summary
What was known before
-
Uncorrected refractive error (URE) is the leading cause of vision impairment globally among both adults and children, and contributes to reduced educational and economic opportunities, decreased quality of life and an increased burden of mortality
-
Visual impairment is a significant global health concern, and the ‘World Report on Vision’ by the World Health Organisation in 2019 called for the routine measurement of refractive error services coverage as a means to address the UN Sustainable Development Goal 3.8 of universal health coverage
-
Uncorrected refractive error (URE) is readily treated with spectacles, making it one of the most cost-effective healthcare interventions, both for distance visual impairment and near visual impairment due to presbyopia
-
The need for new population data on vision impairment is vital to monitor and measure success against global targets to increase the coverage of refractive error services by 40% by 2030
What this study adds
-
This study provides up-to-date global and regional, sex-specific and age-specific estimates and temporal trends for vision impairment due to uncorrected refractive error, both for distance and near vision impairment.
-
We examined age-adjusted and sex-adjusted differences in the contribution of uncorrected refractive error to vision impairment, with a focus on older age groups
-
We incorporated studies from an updated systematic review for a total of 243 sources from 73 countries
-
Our study reveals that over the last 20 years, the absolute number of people with URE has risen due to population growth and ageing, with a continued disproportionate burden by region and sex
-
Uncorrected refractive error (URE) remains a leading cause of MSVI, affecting 157 million individuals worldwide in 2020, and MSVI due to URE accounts for 57% of all MSVI globally
-
Furthermore, an estimated 419 million people aged 50+ had near VI from uncorrected presbyopia globally in 2020
-
These data underscore the persistent and substantial global burden of avoidable vision loss caused by uncorrected refractive error, highlighting the urgent need for novel and fresh approaches to refractive service delivery.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the coordinator of the Vision Loss Expert Group (Professor Rupert Bourne; rb@rupertbourne.co.uk) upon reasonable request. Data are located in controlled access data storage at Anglia Ruskin University.
References
Ma X, Zhou Z, Yi H, Pang X, Shi Y, Chen Q, et al. Effect of providing free glasses on children’s educational outcomes in China: cluster randomized controlled trial. BMJ. 2014;349:23.
Reddy PA, Congdon N, MacKenzie G, Gogate P, Wen Q, Jan C, et al. Effect of providing near glasses on productivity among rural Indian tea workers with presbyopia (PROSPER): a randomised trial. Lancet Glob Health. 2018;6:e1019–e1027.
Slavin RE, Collins ME, Repka MX, Friedman DS, Mudie LI, Owoeye JO, et al. In plain sight: reading outcomes of providing eyeglasses to disadvantaged children. J Educ Stud Placed Risk. 2018;23:250–8.
Naidoo KS, Fricke TR, Frick KD, Jong M, Naduvilath TJ, Resnikoff S, et al. Potential lost productivity resulting from the global burden of myopia: systematic review, meta-analysis, and modelling. Ophthalmology. 2019;126:338–46.
Nie JC, Pang XP, Wang L, Rozelle S, Sylvia S. Seeing is believing: experimental evidence on the impact of eyeglasses on academic performance, aspirations, and dropout among junior high school students in rural China. Econ Dev Cult Change. 2020;68:335–55.
Marques AP, Ramke J, Cairns J, Butt T, Zhang JH, Muirhead D, et al. Global economic productivity losses from vision impairment and blindness. E Clin. Med. 2021;35:26.
Ramrattan RS, Wolfs RC, Panda-Jonas S, Jonas JB, Bakker D, Pols HA, et al. Prevalence and causes of visual field loss in the elderly and associations with impairment in daily functioning: the Rotterdam Study. Arch Ophthalmol. 2001;119:1788–94.
McCarty CA, Nanjan MB, Taylor HR. Vision impairment predicts 5 year mortality. Br J Ophthalmol. 2001;85:322–6.
Lee DJ, Gómez-Marín O, Lam BL, Zheng DD. Visual acuity impairment and mortality in US adults. Arch Ophthalmol. 2002;120:1544–50.
Ehrlich JR, Ramke J, Macleod D, Burn H, Lee CN, Zhang JH, et al. Association between vision impairment and mortality: a systematic review and meta-analysis. Lancet Glob Health. 2021;9:e418–e430.
Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health: Vision Beyond 2020. Lancet Glob Health. 2021;9:e489–e551.
Baltussen R, Naus J, Limburg H. Cost-effectiveness of screening and correcting refractive errors in school children in Africa, Asia, America and Europe. Health Policy. 2009;89:201–15.
Frick KD, Riva-Clement L, Shankar MB. Screening for refractive error and fitting with spectacles in rural and urban India: cost-effectiveness. Ophthalmic Epidemiol. 2009;16:378–87.
Fricke TR, Holden BA, Wilson DA, Schlenther G, Naidoo KS, Resnikoff S, et al. Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ. 2012;90:728–38.
Tahhan N, Papas E, Fricke TR, Frick KD, Holden BA. Utility and uncorrected refractive error. Ophthalmology. 2013;120:1736–44.
WHO. World Health Organization; Geneva: 2013. Universal eye health: a global action plan 2014–2019. https://www.who.int/publications/i/item/universal-eye-health-a-global-action-plan-2014-2019 Accessed 13 Feb 2023.
World Health Organisation. World report on vision. Geneva; 2019. https://www.who.int/publications/i/item/9789241516570 Accessed 13 Feb 2023.
United Nations. Sustainable Development Goals. 2015. https://sdgs.un.org/goals Accessed 14 May 2023.
Hashemi H, Fotouhi A, Yekta A, Pakzad R, Ostadimoghaddam H, Khabazkhoob M. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. J Curr Ophthalmol. 2017;30:3–22.
Sun HP, Li A, Xu Y, Pan CW. Secular trends of reduced visual acuity from 1985 to 2010 and disease burden projection for 2020 and 2030 among primary and secondary school students in China. JAMA Ophthalmol. 2015;133:262–8.
Lee JH, Jee D, Kwon JW, Lee WK. Prevalence and risk factors for myopia in a rural Korean population. Invest Ophthalmol Vis Sci. 2013;54:5466–71.
He MG, Zeng JW, Liu YZ, Xu JJ, Pokharel GP, Ellwein LB. Refractive error and visual impairment in urban children in southern China. Invest Ophth Vis Sci. 2004;45:793–9.
Walline JJ, Lindsley KB, Vedula SS, Cotter SA, Mutti DO, Ng SM, et al. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev. 2020;1:13.
Mountjoy E, Davies NM, Plotnikov D, Smith GD, Rodriguez S, Williams CE, et al. Education and myopia: assessing the direction of causality by Mendelian randomisation. BMJ. 2018;361:6.
Marmamula S, Narsaiah S, Shekhar K, Khanna RC, Rao GN. Visual Impairment in the South Indian State of Andhra Pradesh: Andhra Pradesh - Rapid Assessment of Visual Impairment (AP-RAVI) Project. PLoS ONE. 2013;8:e70120.
Ahmed M, Shefali MK, Husain L, Khondaker M, Alauddin M, Hossain MA, et al. Vision impairment and productivity among female garment workers in Bangladesh: a cohort study. Asia Pac J Ophthalmol. 2022;11:79–84.
Bourne RRA, Flaxman SR, Braithwaite T. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e888–e897.
Flaxman SR, Bourne RRA, Resnikoff S. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221–e1234.
GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e144–e160.
Ramke J, Evans JR, Habtamu E, Mwangi N, Silva JC, Swenor BK, et al. Grand Challenges in Global Eye Health study group. Grand Challenges in global eye health: a global prioritisation process using Delphi method. Lancet Healthy Longev. 2022;3:e31–e41.
Bourne RRA, Steinmetz, Flaxman J, Briant SR, Taylor HRB PS, Resnikoff S, et al. GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Global Health. 2021;9:e130–e143.
International Classification of Diseases 11th edition https://icd.who.int/browse11/l-m/en#/http%253a%252f%252fid.who.int%252ficd%252fentity%252f1103667651 Accessed 14 May 2023.
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. GBD 2019 Diseases, Injuries, and Impairments Collaborators. Global burden of 359 diseases, injuries, and impairments, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
James SL, Abate D, Hassan AK, Abay SM, Abbafati C, et al. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858.
Vollset SE, Goren E, Yuan C-W, Cao J, Smith A, Hsiao T, et al. Fertility, mortality, migration, and population scenarios for 195 countries and territories from 2017 to 2100: a forecasting analysis for the Global Burden of Disease Study. Lancet. 2020;396:1285–306.
Stevens GA, Alkema L, Black RE, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388:e19–23.
IAPB Vision Atlas, List of Seven Super Regions https://www.iapb.org/learn/vision-atlas/about/definitions-and-regions/ Accessed 13 June 2022.
Han X, Zhang J, Liu Z, Tan X, ** G, He M, et al. Real-world visual outcomes of cataract surgery based on population-based studies: a systematic review. Br J Ophthalmol. (2022). https://doi.org/10.1136/bjophthalmol-2021-320997.
United Nations (UN) Department of Economic and Social Affairs World Population Prospects 2022. www.un.org.development.desa.pd/files/wpp2022_summary_of_results.pdf Accessed 13 Feb 2023.
UN World Population Ageing Report 2019 https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf Accessed 13 Feb 2023.
Bourne RRA, Cicinelli MV, Sedighi T, Tapply IH, McCormick I, Jonas JB, et al. Effective refractive error coverage in adults aged 50 years and older: estimates from population-based surveys in 61 countries. Lancet Glob Health. 2022;10:e1754–e1763.
Morgan IG, French AN, Ashby RS, Guo X, Ding X, He M, et al. The epidemics of myopia: aetiology and prevention. Prog Retin Eye Res. 2018;62:134–49.
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42.
Courtright P, Lewallen S. Why are we addressing gender issues in vision loss? Community Eye Health. 2009;22:17–9.
Fricke TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Ho SM, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: systematic review, meta-analysis, and modelling. Ophthalmology. 2018;125:1492–9.
Ma Q, Chen M, Li D, Zhou R, Du Y, Yin S, et al. Potential productivity loss from uncorrected and under-corrected presbyopia in low- and middle-income countries: a life table modelling study. Front Public Health. 2022;10:983423.
Li M, Xu L, Tan CS, Lanca C, Foo LL, Sabanayagam C, et al. Systematic review and meta-analysis on the impact of COVID-19 pandemic-related lifestyle on myopia. Asia Pac J Ophthalmol. 2022;11:470–80.
Funding
This study was funded by Brien Holden Vision Institute, Foundation Thea, Fred Hollows Foundation, Bill & Melinda Gates Foundation, Lions Clubs International Foundation (LCIF), Sightsavers International, and University of Heidelberg.
Author information
Authors and Affiliations
Ethics declarations
Competing interests
GBD 2019 Blindness and Vision Impairment Collaborators: N J Adderley reports grants or contracts paid to their institution from the National Institute for Health and Care Research, UKRI Medical Research Council, Clinical Research Network West Midlands, and Action Against AMD. S Afzal reports support for the present manuscript from King Edward Medical University, Department of Community Medicine which provided study materials, research article, supporting staff and office for working on the manuscript; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from King Edward Medical University; participation on a Data Safety Monitoring Board or Advisory Board with the National Bioethics Committee Pakistan, King Edward Medical University Institutional Ethical Review Board and Ethical Review Committee in Board of Faculty, and Ethical Review Board Fatima **nah Medical University and Sir Ganga Ram Hospital; leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid, Pakistan Association of Medical Editors, Fellow of Faculty of Public Health Royal Colleges UK (FFPH), Society of Prevention, Advocacy And Research, King Edward Medical University. (SPARK), Member Pakistan Society of Infectious Diseases, Member Pakistan Society of Internal Medicine, Member Pakistan Society of Community Medicine and Public Health; other financial or non-financial interests in the Higher Education Commission of Pakistan as a member Research and Publications Committee, and Pakistan Medical and Dental Council as a member Journal Research Evaluation Committee; all outside the submitted work. O C Baltatu reports support for the present manuscript from National Council for Scientific and Technological Development (CNPq, 304224/2022-7), and Anima Institute - AI research professor fellowship; leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid, with the Health and Biotechnology Board at São José dos Campos Technology Park, and Afya – UNINOVAFAPI as Academic Ambassador; all outside the submitted work. T W Bärnighausen reports grants from the European Union (Horizon 2020 and EIT Health), German Research Foundation (DFG), US National Institutes of Health, German Ministry of Education and Research, Alexander von Humboldt Foundation, Else-Kröner-Fresenius - Foundation, Wellcome Trust, Bill & Melinda Gates Foundation, KfW, UNAIDS, and WHO; consulting fees from KfW on the OSCAR initiative in Vietnam; participation on a Data Safety Monitoring Board or Advisory Board with the NIH-funded study “Healthy Options”, Chair, Data Safety and Monitoring Board (DSMB), German National Committee on the “Future of Public Health Research and Education”, Chair of the scientific advisory board to the EDCTP Evaluation, Member of the UNAIDS Evaluation Expert Advisory Committee, National Institutes of Health Study Section Member on Population and Public Health Approaches to HIV/AIDS, US National Academies of Sciences, Engineering, and Medicine’s Committee for the “Evaluation of Human Resources for Health in the Republic of Rwanda under the President’s Emergency Plan for AIDS Relief”, and University of Pennsylvania Population Aging Research Center External Advisory Board Member; leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid, with the Global Health Hub Germany; all outside the submitted work. S Bhaskar reports grants or contracts from the Japan Society for the Promotion of Science (JSPS), JSPS International Fellowship, Japanese Ministry of Education, Culture, Sports, Science and Technology (MEXT), the Australian Academy of Science, Grant-in-Aid for Scientific Research (KAKENHI); leadership or fiduciary roles in board, society, committee or advocacy groups, paid or unpaid with Rotary District 9675 as the District Chair of Diversity, Equity, and Inclusion; the Global Health & Migration Hub Community and the Global Health Hub Germany (Berlin, Germany) as the Chair and Manager; PLOS One, BMC Neurology, Frontiers In Neurology, Frontiers in Stroke, Frontiers in Public Health and BMC Medical Research Methodology as an Editorial Board Member, outside the submitted work. R Bourne reports support for the present manuscript to their institution from the World Health Organization (WHO), Brien Holden Vision Institute, Foundation Thea, Fred Hollows Foundation, Lions Clubs International Foundation; and grants or contracts to their institution from Sightsavers International and the University of Heidelberg. M Cenderadewi reports grants or contracts from James Cook University (International Research Training Program Scholarship for doctoral study), and support for attending meetings and travel from James Cook University; all outside the submitted work. N Congwon reports grants or contracts paid to their institute from the Wellcome Trust Investigator Award. X Dai and J D Steinmetz report support for the present manuscript from the Bill and Melinda Gates Foundation as payments to IHME for the GBD Study. A Dastridiou reports support for attending meetings and/or travel from THEA and ABBVIE; outside the submitted work. T Fricke reports a grant from the International Myopia Institute, and contracts from the Brien Holden Vision Institute and the Victorian Lions Foundation, all paid to the Australian College of Optometry; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from the University of Melbourne and UNSW Sydney; support from attending meetings and travel from the International Myopia Conference as a presenter, and UNSW Sydney as a PhD Candidate; all outside the submitted work. J M Furtado reports consulting fees from SightFirst and Pan American Health Organization; outside the submitted work. I M Ilic reports support for the present manuscript from Ministry of Education, Science and Technological development, Republic of Serbia (project No 175042, 2011-2023). S M S Islam reports grants from NHMRC and the Heart Foundation, outside the submitted work. F Ghassemi reports support for the present manuscript from medical writing. V K Gupta report grants or contracts from National Health and Medical Research Council (NHMRC), Australia, as payments to their institutions; all outside the submitted work. J H Kempen reports support for the present manuscript from Sight for Souls and Mass Eye and Ear Global Surgery Program. K Krishan reports non-financial support from UGC Centre of Advanced Study, CAS II, Department of Anthropology, Panjab University, Chandigarh, India, outside the submitted work. V C Lansingh reports consulting fees from HelpMeSee; and support for attending meetings and travel from HelpMeSee; all outside the submitted work. J L Leasher reports leadership or fiduciary role in other board, society, committee or advocacy group, unpaid as a member of the National Eye Institute National Eye Health Education Program planning committee; outside the submitted work. M Lee reports support for the present manuscript from the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2021R1I1A4A01057428) and Bio-convergence Technology Education Program through the Korea Institute for Advancement Technology (KIAT) funded by the Ministry of Trade, Industry and Energy (No. P0017805). K S Naidoo reports other financial support from OneSight EssilorLuxottica Foundation as an employee; outside the submitted work. M Saylan reports support for attending meetings and/or travel from Janssen Pharmaceuticals; outside the submitted work. J A Singh reports consulting fees from AstraZeneca, Crealta/Horizon, Medisys, Fidia, PK Med, Two labs Inc., Adept Field Solutions, Clinical Care options, Clearview healthcare partners, Putnam associates, Focus forward, Navigant consulting, Spherix, MedIQ, Jupiter Life Science, UBM LLC, Trio Health, Medscape, WebMD, Practice Point communications, and the National Institutes of Health and the American College of Rheumatology; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from the speaker’s bureau of Simply Speaking; support for attending meetings from OMERACT as a member of the steering committee; participation on an Advisory Committee with the FDA Arthritis Advisory Committee; leadership or fiduciary roles in board, society, committee or advocacy groups, paid or unpaid as a past steering committee member of the OMERACT, an international organization that develops measures for clinical trials and receives arms length funding from 12 pharmaceutical companies, Co-Chair of the Veterans Affairs Rheumatology Field Advisory Committee, and the editor and Director of the UAB Cochrane Musculoskeletal Group Satellite Center on Network Meta-analysis; stock or stock options in Atai Life Sciences, Kintara Therapeutics, Intelligent Biosolutions, Acumen Pharmaceutical, TPT Global Tech, Vaxart Pharmaceuticals, Atyu Biopharma, Adaptimmune Therapeutics, GeoVax Labs, Pieris Pharmaceuticals, Enzolytics Inc., Seres Therapeutics, Tonix Pharmaceuticals Holding Corp., and Charlotte’s Web Holdings, Inc, as well as previously owned stock options in Amarin, Viking and Moderna Pharmaceuticals; outside the submitted work. Y S Samodra reports grants or contracts from Taipei Medical University; and other financial or non-financial interests as the co-founder of Benang Merah Research Center, outside the submitted work. N Tahhan reports support for attending meetings and travel from the Brien Holden Foundation to the ISER Conference; outside the submitted work. Y Tan reports support for the present manuscript from the Department of Ophthalmology and the Hospital Central South University and Postdoctoral Station of Clinical Medicine, The Third **angya Hospital of Central South University. J H V Ticoalu reports other financial or non-financial support as a co-founder of Benang Merah Research Center; outside the submitted work.
Vision Loss Expert Group of the Global Burden of Disease Study: A Bron reports payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Théa. N Congdon reports grants or contracts from any entity from Welcome Trust and MRC; consulting fees from Belkin Vision; and support for attending meetings and/or travel from Singapore National Eye Center. M A Del Monte reports support for attending meetings and/or travel from the University of Michigan, and leadership or fiduciary roles in board, society, committee or advocacy groups, paid or unpaid as past president of Costenbader Society. T Fricke reports grants or contracts from any entity from Brien Holden Vision Institute, Victorian Lions Foundation, International Myopia Institute, and Australian government; and support for attending meetings and/or travel from International Myopia Institute. D Friedman reports leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid, from Orbis International as member of board of governors. J M Furtado reports consulting fees from Pan American Health Organization and from Lions Club International Foundation. G Gazzard reports consulting fees from Alcon Laboratories, Inc; Allergan, Inc; BELKIN Vision LTD; Carl Zeiss Meditec; Elios; Genentech/Roche; Reichert; Théa and ViaLase; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Alcon Laboratories, Inc; BELKIN Vision Ltd; Carl Zeiss Meditec; Elios and Ellex; participation on a Data Safety Monitoring Board or Advisory Board with Alcon Laboratories, Inc; Allergan, Inc; BELKIN Vision Ltd; Carl Zeiss Meditec; Elios and Visufarma; and leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid with Glaucoma UK Medical Advisory Board and UK&Eire Glaucoma Society as president. M E Hartnett reports support for the present manuscript (e.g., funding, provision of study materials, medical writing, article processing charges, etc.) from Michael F. Marmor, M.D. Professor of Retinal Science and Disease as endowment to support salary; grants or contracts from any entity (from National Eye Institute R01 EY017011 and National Eye Institute R01 EY015130) as partial salary support; patents planned, issued or pending (WO2015123561A2 and WO2021062169A1); and leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid with Jack McGovern Coats’ Disease Foundation and as director of Women’s Eye Health and Macular Society Grant Review Chair. J H Kempen reports support for the present manuscript (e.g., funding, provision of study materials, medical writing, article processing charges, etc.) from Mass Eye and Ear Global Surgery Program (as support of salary). J E Kim reports consulting fees from Genentech/Roche, DORC, Notal Vision and Outlook Therapeutics (all as payment to J E Kim); participation on a Data Safety Monitoring Board or Advisory Board with Allergan, Amgen, Apellis, Bausch&Lomb, Clearside, Coherus, Novartis and Regeneron (all as participation on advisory board); leadership or fiduciary role in other borad, society, committee or advocacy group, paid or unpaid, with AAO, APRIS, ASRS, Macular Society and NAEVR/AEVR (all unpaid); and receipt of equipment, materials, drugs, medical writing, gifts or other services from Clearside and Genentech/Roche (both for medical writing). V C Lansingh reports consulting fees from HelpMeSee (as an employee); and support for attending meetings and/or travel from HelpMeSee (pay airfare and hotel). J Leasher reports leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid with National Eye Institute (as a member) and National Eye Health Education Program planning committee (unpaid). K S Naidoo reports other financial or non-financial interests from OneSight Essilor Luxottica Foundation as an employee of the non-profit foundation. M Nowak reports participation on a Data Safety Monitoring Board or Advisory Board with Vision Express Co. Poland as the chairman of medical advisory board of Vision Express Co. Poland. P Ramulu reports grants or contracts from National Institute of Health and Perfuse Therapeutics; and consulting fees from Alcon and W. L. Gore. F Topouzis reports grants or contracts from Théa, Omikron, Pfizer, Alcon, Abbvie and Bayer (all paid to Institution); consulting fees from Omikron, Théa and Bausch & Lomb (all paid to Topouzis); payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Omikron (paid to Topouzis), Abbvie and Roche (both paid to Institute); and leadership or fiduciary role in other board, society, committee or advocacy group, paid or unpaid with European Glaucoma Society (as president), Greek Glaucoma Society (as president) and Board of Governors, World Glaucoma Association (all unpaid).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vision Loss Expert Group of the Global Burden of Disease Study., the GBD 2019 Blindness and Vision Impairment Collaborators. Global estimates on the number of people blind or visually impaired by Uncorrected Refractive Error: a meta-analysis from 2000 to 2020. Eye (2024). https://doi.org/10.1038/s41433-024-03106-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41433-024-03106-0
- Springer Nature Limited