Abstract
Introduction
Achondroplasia is a rare autosomal dominant condition characterized by stenosis in spinal canal. Multilevel Ossification of the ligamentum flavum in the spine is a rare occurrence which too can contribute to stenosed canal.
Case presentation
We report a case of an Indian achondroplasic dwarf with multilevel ossification of ligamentum flavum (OLF) at thoracic and lumbar segment. She presented in the outpatient department with bilateral weakness in legs with complete foot drop on the left side and was non-ambulatory. She was managed surgically by instrumentation with multiple interbody fusions with wide decompression and excision of OLF. The patient responded well to the surgery and became a walker after 2-year follow-up.
Discussion
Achondroplasic patients may present rarely with multiregional and multilevel OLF. It is important to identify them preoperatively so as to have good surgical outcome. Wide laminectomy, removal of the ossified ligament, and fusion with instrumentation resulted in the improvement of the patient’s neurological symptoms and functions.
Similar content being viewed by others
Introduction
Achondroplasia has an autosomal dominant inheritance characterized by a defect in endochondral ossification due to mutation in FGFR3 gene. It can lead to disproportionate growth with short limbs and long trunk with craniofacial and vertebral anomalies [1]. The spinal canal of an achondroplasia individual gets narrowed both anteroposteriorly and transversely due to thick laminae, short pedicles, and cranio-caudally decreasing interpedicular distance and vertebral body height leading to congenital stenosis.
Mostly the stenosis is described in lumbar region and lower thoracic region. The common presentation of these patients is claudication pain if only lumbar region is involved, or deterioration in walking pattern along with claudication pain if both thoracic and lumbar region are involved. The degenerative changes such as disc herniation or facetal arthropathy can worsen the condition in an already stenosed canal [2]. Also, the kyphotic nature of thoracolumbar spine seen in such patients may compromise the spinal cord and lead to neurological symptoms.
There has been description of ossification of ligamentum flavum (OLF) mainly in thoracic area in achondroplasia patients which is another cause of neurological symptoms. However, multilevel ossification in both lumbar and thoracic area leading to neurological symptoms has been rarely reported in the literature. We present our experience with a case of tandem stenosis due to OLF at thoracic and luðbar levels, which was surgically managed with an optimal outcome.
Case presentation
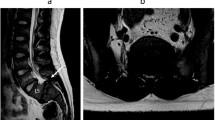
A 34-year-old Indian achondroplasia female dwarf came to us with left side foot drop for 3 years, with progressive weakness in both lower limbs (L»R). The patient was unable to stand and walk without support from last 3 months and was completely unable to walk since last 2 weeks at the time of presentation (Nurick grade 5) [3]. There was a history of spinal surgical intervention 2 years back but no records were available with the patient. General physical examination revealed a short stature of 132 cm with short limbs and long trunk, frontal bossing and depression of the nasal bridge. There was a midline surgical scar at the lower thoracic spine. On specific examination, it is found that she had bilateral plantars extensor with knee and ankle reflex absent and motor deficit in all myotomes of lower limbs, i.e., ASIA impairment scale C (motor power of 3/5 in L2 myotome over right side and 2/5 over left side, 4/5 power in L3, L4 myotome over right side and 2/5 in left L3 with 0/5 in left L4 myotome, 3/5 power in right L5 and 0/5 in left L5 with bilateral S1 was 3/5). On sensory examination, she had reduced touch, vibration, proprioception in bilateral lower limbs below L1 dermatome. She had normal perianal sensation and voluntary anal contraction. Considering the mixed UMN and LMN features, the patient was evaluated with radiological investigations. X-rays show previous laminectomy shadows, decrease interpedicular distance in the lumbar spine and short pedicles indicating canal stenosis. CT shows trefoil canal due to short pedicles with OLF at posterior part of spinal canal at the level of T9-10, T11-12, L1-2, L3-4 & L4-5 (Fig. 1). MRI shows multiregional stenosis with thickened ligamentum flavum (Fig. 2). Both CT and MRI show postoperative soft tissue and bony changes in lower thoracic spine. Dynamic films show no spinal instability (Fig. 3). All laboratory investigations were normal.
In view of progressive weakness and evidence of tandem stenosis, the patient was advised surgical decompression with instrumentation. After proper surgical preparation and well-informed consent, which includes the patient and family education regarding a higher than usual chance of perioperative complications, the patient was taken to the operation theatre. Neuromonitoring was also used. Exposure was done with standard posterior midline approach from T9 to L5. Pedicle screws were inserted from T10-L4. Laminectomy was done at T11-12, T12-L1 and L1-2 levels by using high-speed burr. As expected, ossified ligamentum flavum was noticed which was thinned out using high-speed burr (Fig. 4). Then it was removed in piecemeal by taking care of adhesions with the dura. At thoracic level, dura was also calcified and few flakes of ossified ligamentum flavum were left free floating due to risk of dural injury. L2-3, L3-4 transforaminal lumbar interbody fusion was done using PEEK cage and bone grafting. Stabilization with rods in the pedicle screw was done. The postoperative period was uneventful. Postoperative radiographs showed good positioning of the implants (Fig. 5). The patient was made to sit and stand with support by the day 10. At 6 months postoperatively, the patient’s motor power gradually improved to Grades 3–4 at L2–L3 bilaterally and Grades 2–3 at L4–S1 [AIS D]. The patient also has improvement in sensory symptoms. At 2-year follow-up, the patient is able to walk independently without support (Fig. 5). Her left side foot drop is partially improved for which ankle-foot orthosis was given. Her Nurick’s grading [3] is improved to 2 at the last follow-up.
Discussion
Achondroplasia, an autosomal dominant condition, first originally described by Parrot [4]. It is characterized by disproportionate stature with rhizomelic short limbs, trident hands, macrocephaly with frontal and parietal bossing and saddle nose deformity. Achondroplastic patients have many abnormalities in the spine as well. It includes spinal stenosis, disc degeneration, hypertrophy of ligamentum flavum, thickened lamina and facet joints which further add to the stenosis of spinal canal [5,6,7]. Another spinal manifestation seen in almost 90% of achondroplasia patient is thoracolumbar kyphosis [8] and it is also important from surgical point of view. Many authors have described only decompression [9,10,11] in symptomatic patients but aggravation or development of thoracolumbar kyphosis is seen after this and results were poor. Hence instrumentation is always preferred along with decompression [12, 13].
The symptoms in achondroplasic patients are mostly due to spinal stenosis and kyphotic deformity may add to the stenosis. Since the most common site of stenosis is lumbar spine, hence patient presents with claudication pain [14,15,16]. In later stages, the patient may develop neurological deficit. However, there are very few cases reported with concurrent stenosis of lower thoracic and lumbar spine. In such cases, the clinical picture is a combination of both upper motor neuron and lower motor neuron. Such patients with tandem stenosis present with claudication pain and myelopathy symptoms [9, 17]. Our patient apprised weakness in both lower limbs and inability to walk. She had bilateral plantars extensor with absent deep tendon reflexes of lower limbs which is consistent with tandem stenosis.
Imaging findings in achondroplasia shows shortened vertebral bodies and pedicles along with reduced interpedicular distance and increase in pedicle diameter [18]. All these will ultimately lead to spinal canal stenosis. There might be associated OLF adding to the severity of stenosis. However, OLF is very rare finding in achondroplasia [9]. If present, OLF is more common in thoracic spine. By going through the literature, ten case reports show OLF in achondroplasia [Table 1]. Within the thoracic spine, OLF is more common in lower thoracic spine as seen in nine out of ten case reports mentioned in Table 1. However, to the best of our knowledge, there are only two case reports that discuss about multilevel OLF involving both lower thoracic and lumbar spine [9, 17]. In our patient, all image findings are consistent with above studies and ossified ligamentum flavum can be noticed at T9-10, T11-12, L1-2, L3-4 & L4-5. On CT scan, laminectomy can be seen which was done in previous surgery elsewhere and OLF was not addressed at that time, which may be one of the reasons for no improvement in neurological status of the patient. Another possibility could be that there are no changes in CT or MRI at lumbar level which indirectly points out that lumbar level was not addressed at that time.
Though, in literature the indications of surgery and timing of surgery are not well defined [19] but progressive neurological deficit is undoubtedly an indication for surgery. We did posterior instrumentation from T10-L4 with decompression for the involved levels. In achondroplasia, length of instrumentation and lowest instrumented level after decompression needs separate attention [20]. Post-laminectomy kyphosis is a common complication [12, 13] in such patients and thus requires a long and stable construct to counter-act.
Dural ossification is also a common finding in OLF (40%) [21] and could lead to iatrogenic tears of the dura during decompression in achondroplastic patients with spinal stenosis. Sun et al. reported the incidence of dural tears and cerebrospinal fluid leakage in OLF patients was 32% [22]. Therefore, a CT evaluation to identify an OLF and dural ossification is recommended. In the surgical technique, it is recommended to use a high-speed drill to thin the lamina gradually before using the Kerrison rongeur to remove the bone. Ossified part of ligamentum flavum should be removed with great caution taking care of adhesion and should be done in piecemeal. Out of two case reports, Kachonkittisak et al. [23] mentioned incidental durotomy as an intraoperative complication, which was primarily repaired. However, none of the two articles [23, 24] mentioned deterioration of neurological deficit immediately after surgery. In our case too, neurology rather improved immediate postoperatively with left side ankle showing flickering movements and left hip flexors also showing increase in power
Early surgical decompression is advocated to have better neurological recovery. If there is multilevel ossification causing symptoms, both levels have to be addressed to have optimal recovery. Several posterior decompressive methods (open-door laminectomy, en-bloc laminectomy, fenestration, hemilaminectomy, and key-hole foraminotomy) for the ossified lesions are advocated [25]. But the key to the success is adequate removal of ossified part of the ligamentum flavum. In our case, it was not removed in previous surgery and only a narrow central laminectomy was done, which did not allow the cord to get enough space and hence there was no improvement in neurological status of the patient.
Conclusion
Multilevel OLF especially in both lumbar and thoracic region is a rare finding in achondroplasia causing neurological symptoms. These patients require surgical intervention with posterior instrumentation, laminectomy and proper removal of OLF. Failure to remove OLF may give poor outcomes and hence their preoperative identification is of paramount importance. However, there is dearth of literature for multilevel OLF and more cases are needed to be reported to formulate better guidelines of management.
References
Shiang R, Thompson LM, Zhu YZ, Church DM, Fielder TJ, Bocian M, et al. Mutations in the transmembrane domain of FGFR3 cause the most common genetic form of dwarfism, achondroplasia. Cell 1994;78:335–42.
Srikumaran U, Woodard EJ, Leet AI, Rigamonti D, Sponseller PD, Ain MC. Pedicle and spinal canal parameters of the lower thoracic and lumbar vertebrae in the achondroplast population. Spine. 2007;32:2423–31.
Nurick S. The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain. 1972;95:87–100.
Parrot MJ. Sur la malformation achondroplastique et le Dieu Phtah. Bull Soc Anthropol. 1878;1:296.
Hamamci N, Hawran S, Biering-Sorensen F. Achondroplasia and spinal cord lesion. Three case reports. Paraplegia. 1993;31:375–9.
Thomeer RT, van Dijk JM. Surgical treatment of lumbar stenosis in achondroplasia. J Neurosurg. 2002;96:S292–7.
Ain MC, Elmaci I, Hurko O, Clatterbuck RE, Lee RR, Rigamonti D. Reoperation for spinal restenosis in achondroplasia. J Spinal Disord. 2000;13:168–73.
Srikumaran U, Woodard EJ, Leet AI, Rigamonti D, Sponseller PD, Ain MC. Pedicle and spinal canal parameters of the lower thoracic and lumbar vertebrae in the achondroplastic population. Spine. 2007;32:2423–31.
Suzuki K, Kanamori M, Nobukiyo M. Ossification of the thoracic ligamentum flavum in an achondroplastic patient: a case report. J Orthop Surg. 2008;16:392–5.
Saito K, Miyakoshi N, Hongo M, Kasukawa Y, Ishikawa Y, Shimada Y, et al. Congenital lumbar spinal stenosis with ossification of the ligamentum flavum in achondroplasia: a case report. J Med Case Rep. 2014;8:88.
Chakraborty T, Sharma D, Goyal A, Madan VS. A rare case of ossification of ligamentum flavum presenting as dorsal myelopathy in achondroplasia. J Neurol Stroke. 2017;7:00254. https://doi.org/10.15406/jnsk.2017.07.00254
Ain MC, Shirley ED, Pirouzmanesh A, Hariri A, Carson BS. Post laminectomy kyphosis in the skeletally immature achondroplast. Spine 2006;31:197–201.
Agabegi SS, Antekeier DP, Crawford AH, Crone KR. Post laminectomy kyphosis in an achondroplastic adolescent treated for spinal stenosis. Orthopaedics. 2008;31:168.
Kataoka O. A case of achondroplasia occurred palaplasis after trauma. Spinal Surg 1990;1:346–50.
Nakahashi K, Baba H, Takahasi K, Kawahara N, Kikuchi Y, Tomita K, et al. Achondroplasia with ossification of yellow ligament of the thoracic spine: report of a case. Orthop Surg Traumatol. 1991;34:397–400.
Baba H, Imura S, Tomita K. Achondroplasia with spinal cord or cauda equina symptoms: report of three cases. Orthop Surg. 1992;43:47–52.
Imamura T, Oga M, Tamaru T, Arima J, Ikuta K, Esaki Y, et al. A case of achondroplasia with ossification of the yellow ligament. Orthop Traumatol. 1997;46:1227–32.
Lutte LD, Longstein JE, Winter RB, Langer LO. Anatomy of the achondroplastic lumbar canal. Clin Orthop Relat Res. 1997;126:139–42.
Liao JC, Chen WJ, Lai PL, Chen LH. Surgical treatment of achondroplasia with thoracolumbar kyphosis and spinal stenosis—a case report. Acta Orthop 2006;77:541–4.
MacGibbon B, Farfan HF. A radiologic survey of various configurations of the lumbar spine. Spine. 1979;4:258–66.
Muthukumar N. Dural ossification in ossification of the ligamentum flavum: a preliminary report. Spine. 2009;34:2654–61.
Sun J, Zhang C, Ning G, Li Y, Li Y, Wang P, et al. Surgical strategies for ossified ligamentum flavum associated with dural ossification in thoracic spinal stenosis. J Clin Neurosci. 2014;21:2102–6.
Kachonkittisak K, Kunakornsawat S, Pluemvitayaporn T, Piyaskulkaew C, Pruttikul P, Kittithamvongs P. Congenital spinal canal stenosis with ossification of the ligamentum flavum in an achondroplastic patient: a case report and literature review. Asian J Neurosurg. 2019;14:1231–5.
Gokcen HB, Ozturk C. Ossification of the ligamentum flavum at the thoracic and lumbar region in an achondroplastic patient. World Neurosurg. 2019;126:461–65. https://doi.org/10.1016/j.wneu.2019.03.028.
Vleggeert-Lankamp C, Peul W. Surgical decompression of thoracic spinal stenosis in achondroplasia: indication and outcome. J Neurosurg Spine. 2012;17:164–172. https://doi.org/10.3171/2012.4. 2012SPINE1220.
Takano T, Takano H, Kato Y, Yamashita S, Tsuji H. Four cases of achondroplastic spinal stenosis: long term results. Cent Jpn J Orthop Surg Traumatol. 1987;32:1416–8. 1987
Author information
Authors and Affiliations
Contributions
AN was responsible for proofreading the manuscript. KB was responsible for writing case presentation in the manuscript. AG was responsible for writing the Introduction, Discussion, and conclusion part of the manuscript and also submitting and responding to the reviewer’s comments. KV was responsible for proof reading the manuscript. JM was responsible for literature search in the field of Achondroplasia and related spinal abnormalities. HSC was responsible for proofreading.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nanda, A., Bansal, K., Gupta, A. et al. Multilevel thoracic and lumbar ligamentum flavum ossification in an achondroplasic—a rare presentation. Spinal Cord Ser Cases 7, 69 (2021). https://doi.org/10.1038/s41394-021-00427-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00427-0
- Springer Nature Limited