Abstract
Background
Secondary conditions may reduce function and participation in individuals with chronic Spinal Cord Injury (SCI). The knowledge of reasons for readmission to the hospital may be enlightening to prevent them and remodel the health services.
Study design
Multicenter prospective observational study of all consecutive readmissions of persons with SCI after rehabilitation completion.
Objectives
To explore the characteristics of individuals with SCI readmitted to the hospital, the reasons for readmissions and the burden on hospitalization in terms of length of stay (LoS) for different conditions.
Setting
31 Italian specialized SCI centers.
Methods
Data on people with traumatic SCI readmitted to SCI centers were recorded about: age, sex, SCI level and severity group, geographical origin, readmission causes, clinical interventions during hospitalization, LoS and discharge destination. Linear and multiple logistic regression analyses were performed considering LoS (days) as dependent variable for correlations with independent variables. All tests were two-sided.
Results
Among 1039 persons with traumatic SCI enrolled (mean age 46, males 85%, tetraplegia 43%), 59.09% of the readmissions were caused by urological problems, 39.74% by pressure injury and 35.41% by spasticity (68% readmitted for ≥2 causes, associated with longer LoS). The mean LoS was 48 days: pressure injury, rehabilitative needs, sexual, bowel, and pain problems were associated with longer and urological problems with shorter LoS. People from the South of the country were frequently (68%) readmitted to the northern centers.
Conclusions
Urological problems, pressure injury and spasticity were the most frequent causes of re-hospitalization in individuals with traumatic SCI. The migration trend seeking SCI-specific treatments suggests geographic areas to which health care organizations need to pay more attention.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a complex condition and people with SCI often experience serious secondary medical and non-medical problems that impact on their vulnerability enough to be readmitted to the hospital [1]. Furthermore, a wide range of secondary conditions may reduce their function, community participation, quality of life, and may involve high costs [2, 3]. In recent years, the increase in the age of incidence and in life expectancy [4, 5] have increased interest in SCI complications and chronic secondary conditions and their consequences. Several of these can cause readmission to health facilities, with important personal, social, and economic repercussions.
Recent studies have investigated the health care utilization after SCI from different points of view, as well as readmission rates and its burden, especially in the first period at home after discharge from rehabilitation [6, 7]. Reasons for readmissions following SCI have also been reported and have proved to be quite different in several studies [8, 9]. These studies have identified urological, skin, and respiratory problems as the main causes of readmission. From the literature we know that older age and more severe neurological injuries (quadriplegia and complete injuries) are predictors of hospital readmission for secondary conditions [10,11,12]. Also, a part of the SCI population with functional, mobility and social limitations may be less easily reached by follow-up programs and more exposed to risk of readmission shortly after rehabilitation discharge [13]. The only data about the Italian situation regarding readmissions after SCI are described in a survey, carried out 20 years ago in a network of Italian rehabilitation SCI-specialized centers [14]. Readmissions were found for approximately the same absolute number of admissions for acute traumatic and non-traumatic SCI in the study period. The main burden, in terms of total days of stay, was represented by functional gain programs, pressure injuries, and urological complications.
There are typically two types of readmission in Italy: general medicine acute wards that deal primarily with medical complications (i.e., urological with surgical necessities, plastic surgery, serious infections, pneumonia, etc.) or specialized SCI rehabilitation centers that deal primarily with rehabilitation-related problems and clinical consequences (such as spasticity, pain, respiratory, urological or bowel management problems, pressure injury in postoperative phase, etc.).
Age and life expectancy trends certainly influence characteristics and burden of readmissions after SCI in a chronic phase. As a result of the multifaceted characteristics of readmissions and the differences in SCI-related health services across countries, it is difficult to examine this topic.
No studies have been conducted in Italy after 2008. Studies conducted in other countries are not uniform regarding readmission rates and causes, depending on local, demographic, injury-related conditions, as well as study settings and design [8,9,10].
A better understanding of numerous lifelong necessities of persons with SCI who experience a hospital readmission could be beneficial for public health facilities. Consequently, longitudinal planning of SCI health services in Italy could benefit from this knowledge regarding prevention and/or treatment of long-term SCI complications. The current prospective observational cohort study has been designed to detect the characteristics of persons with SCI readmitted to hospital at least 1 year after a period of post-acute rehabilitation program, the reasons for hospitalization and hospital burden, in terms of length of stay (LoS) for different conditions in order to provide an updated overview on this data to the public health services and to better face the lifetime needs of individuals with SCI.
Methods
This prospective observational cohort study was conducted by the Italian Spinal Cord Injury (SCI) study Group, involving 31 specialized SCI centers from 13 Italian regions (Fig. 1) [15]. The study was approved and obtained a grant from the Italian Ministry of Health (CCM number 15756 of 17-07-2012 and “Institutional research”). A regional network for a systematic data collection was created under the supervision of National Agency for Regional Health Services (Age.Na.S.).
All consecutive readmissions of persons with SCI (traumatic or non-traumatic etiology) for any clinical or rehabilitation necessity and their relative LoS, from February 1st 2013 to October 31st 2015 were recorded in an electronic database. The physician of each participating center responsible for the research project prospectively collected the data at admission (T1) and discharge (T2) over the re-hospitalization period. People who were still hospitalized at the end of enrollment (October 31st, 2015) were assessed at discharge regardless of the date. Readmission was defined as re-hospitalization of individuals with SCI who had completed the post-acute rehabilitation program, at least 12 months before readmission.
In this article, only data on readmissions of people with traumatic SCI (TSCI) were considered. Exclusion criteria were readmission LoS < 72 h; age < 16 years; non-traumatic etiology; and other neurological conditions leading to SCI (congenital e.g., spina bifida, new SCI in the context of palliative care, neurodegenerative disorders e.g., Multiple sclerosis, amyotrophic lateral sclerosis and Guillain Barré syndrome).
The patients’ demographic characteristics included in this analysis were: sex, age, and geographical origin of the patient. In light of the fact that in Italy the specialized care facilities for people with SCI are not homogeneously distributed throughout the country, we have also collected information on the geographical origin of the inpatient’s residence, grouped in North, Center, and South as well as the region of the facility where they were readmitted. This data tracked and highlighted the “migration” of individuals with SCI for receiving SCI-specific healthcare services among regions. It was also registered whether they were readmitted from home to the SCI centers or transferred from other facilities. In particular, this data was collected to observe how many readmissions were related to the transfers from acute general medicine wards, since normally, in Italy persons with SCI are readmitted to general medicine acute wards and rarely to SCI specialized units. Following the treatment of their urgent clinical cause of readmission, they can be transferred to the SCI specialized centers for rehabilitation. At T1 the following clinical data were collected: level and severity group of injury defined by International Standards for Neurological Classification of SCI (ISNCSCI) and ASIA Impairment Scale (AIS), respectively. For the statistical analysis, level and severity grade of injury were grouped as: AIS ABC-paraplegia (T1-S5 ABC); AIS ABC-tetraplegia (C1-C4 ABC, C5-C8 ABC); and all D [16]. Causes of readmission were defined as urological, pressure injury(s), respiratory, musculoskeletal, pain, spasticity, bowel, and sexual problems. Complex clinical evaluation (in terms of evaluating complex and personalized assistive devices), rehabilitation training, and social and/or nursing needs impacting home care were also recorded. In many readmission episodes more than one cause of readmission was recorded explaining the number of causes exceeding the number of readmissions. All causes were analyzed separately. For statistical analysis, a dichotomous variable was considered, defined as 1 or 2 or more reasons for readmission. Furthermore, in addition to the cause recorded at readmission, the type of clinical interventions performed during hospitalization was also recorded. This included urologic, pressure injury, pain, spasticity, bowel, and sexual problems. It was also recorded whether any surgical intervention (invasive or minimally invasive; e.g., plastic surgery for pressure injury or botulinum toxin injection by cystoscopy for spasticity) was performed. If mechanical ventilation was initiated for respiratory problems, this was recorded as a noninvasive procedure, except in the case of a tracheostomy. A dichotomous variable was also used for the interventions recorded, defined as 1 intervention versus 2 or more interventions. At T2, in addition to the LoS readmission, the discharge destination was also collected, meant as patient returning home or referral to social and health care facilities (acute general medicine ward, nursing home, rehabilitation center, and specialized SCI center).
The main outcome considered as dependent variable was LoS (days) and it was analyzed for correlation with independent variables.
Statistical analysis
Categorical variables were calculated as frequencies and percentages for the whole sample. Standard descriptive statistics were used to summarize data, with respect to demographic and clinical characteristics.
Linear regression was used to investigate which factors were associated with LoS. Independent variables of interest were readmission from (home, acute general medicine ward, nursing home, rehabilitation center, and specialized SCI center), sex, age, migration, severity group, interventions and causes of readmission. Multiple logistic regression analyses were performed to account for several confounding variables simultaneously and included all variables of interest.
Analysis was performed by using STATA version 12.1 (StataCorp. 2011. Stata Statistical Software: Release 12. College Station, TX:StataCorp LP).
All tests were two-sided, and an alpha level of 0.05 was set for statistical significance.
Results
Out of the 1827 total consecutive readmissions in the 31 SCI-specialized centers during the study period, 1039 met the inclusion criteria. The remaining were excluded for the following reasons: non traumatic etiology of SCI (n = 524), stay for less than 72 h (n = 228), missing data including LoS or cause of admission (n = 36).
The mean age (±SD) at readmission was 46 (±15) years. The characteristics of the people with SCI who underwent to readmission are reported in Table 1: males were involved in 85% of cases (male/female ratio 5,7:1); according to the level of the lesion, 43% presented tetraplegia and 54% paraplegia. At T1 complete lesions resulting in complete motor impairment, AIS A and AIS B were the most prevalent (65% and 14%, respectively). When grou** patients by level and SCI severity grade by AIS classification, 12% were included in C1–C4 ABC group, 27% in C5–C8 ABC, 49% in T1-S5 ABC, and 7% in all D lesions.
As for most of readmissions, 76% of persons accessed from their home at admission, the remainder had a previous admission to an acute general medicine ward (13%), or to a specialized SCI center in a different geographical area or other sources (11%). Expectedly, most part of the participants were discharged to home (95%); the small remainder to acute general medicine (2%), nursing home (1%), and other rehabilitation centers (2%). In 542 of readmissions, people lived in the north of Italy, while 210 were resident in Center, and 277 in South and Italian islands.
Two hundred ninety-six readmissions (28%) involved people with traumatic SCI readmitted in rehabilitation centers located in a different region than people residence/geographical origin at admission. This “health migration” mainly occurred from southern regions to the North and Center or, in part, from Center to North. Indeed, one in three individuals with SCI readmitted to the facilities located in North were resident in another geographical area (Table 2).
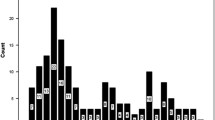
The most frequent clinical complications recorded at T1 were urologic problems (n = 614), pressure injuries (n = 413), and spasticity (n = 368). Invasive interventions were performed to treat the corresponding complication in 160 (26%), 186 (45%), and 63 (17%) of these cases, respectively. In a relevant number of readmissions other three conditions were found: new rehabilitative needs (rehabilitation training in 424 readmissions), long-term complex clinical evaluation (in 375), social and/or nursing needs impacting on home care (in 126). The description of the clinical complications causes of readmission in the centers and the clinical interventions carried out during stay is presented in Fig. 2.
In 311 readmissions (30%), only 1 cause was recorded, in 703 (68%) 2 or more causes were registered (in 25, 2%, missing). In 382 readmissions, patients underwent 0 or 1 clinical intervention, in 573, 2 or more interventions were offered (in 84, 8%, missing).
The LoS median (range IQ) was 29 days (12–64).
When analyzing LoS as a function of the independent variables, univariate analysis (Table 3P value) showed that transfer to a location other than residence (eg, to a general acute care unit or another center SCI) was associated with an increase in LoS of 45 days; residence in a region other than the location of the rehabilitation center (approximately 7 days more), classification in the “C5–C8 and T1-S5” group (approximately 4 days). There was a direct association between some readmission causes and LoS, which were significantly associated with it: social care needs (32 days longer LoS), pressure injuries (29 days), rehabilitation problems (21 days), sexual problems (18 days), bowel problems (14 days), and pain (8 days). Conversely, urological causes of readmission were significantly associated with shorter LoS (−16 days). As for clinical intervention, a significant association was found between longer LoS and having received interventions for pressure injury both invasive (i.e., surgical operation; 40 days LoS after surgery) and non invasive (i.e., accurate injury medications, mobilization, correct positioning, and other usual care during the hospitalization; 21 days); respiratory surgical intervention (tracheostomy; 31 days), bowel non-invasive intervention (14 days) and having more than 1 cause or needing more than 1 intervention during the admission period. In contrast, urological intervention, both invasive and non-invasive, was associated with shorter LoS (−34 and −9 days, respectively).
In the multivariate analysis (Table 3) coming from other places rather than home (i.e., acute general medicine ward or different SCI centers or other); coming from another region with respect to the rehabilitation center’s location, not being classified in the group “all D” and recording >1 cause of readmission were all independently associated with increased LoS.
Discussion
The aim of this SCI centers-based study was to explore the characteristics of people living with SCI who needed readmission, as well as the causes and main interventions implemented in 13 regions of Italy, in order to identify possible points of criticism in a network of SCI centers. This multicenter study, involving 31 Italian centers specialized in the comprehensive treatment of SCI and rehabilitation, included more than one thousand consecutive readmissions after traumatic SCI (representing 44% of all patients treated during this period). It shows that secondary complications in persons with SCI occur long after the acute trauma. In a study conducted in Italy between 1997 and 1999, including both traumatic and non-traumatic SCI, readmissions accounted for 51.0% of the total admissions (n = 2070) registered during the 2-year study [14]. The results highlighted the value of this type of longitudinal data collection and comparative studies on the health status of the chronic SCI population in our country.
The results of this current study revealed that the most frequent clinical complications were urological problems (60%), of these 25% treated through invasive surgery; pressure injury (40%) surgically treated in almost half of the cases; and spasticity reported in one third of readmissions, (17% managed by invasive surgery). These results confirm the data reported by various studies on principal reasons for hospital readmission following a period of rehabilitation [8, 9, 17,18,19,20]. All reports included skin-related problems (e.g., pressure injury) and the genitourinary system (e.g., urinary tract infections [UTIs]) and complications of the upper urinary tract as the most frequent reasons for readmission. Some of the aforementioned clinical complications demonstrated in this study require specific treatment options (e.g., intrathecal baclofen or botulinum toxin) that are available only in specific centers.
Multivariate analysis on LoS showed that being classified in the three most serious neurological classifications (not D group), readmitted from facilities other than home, and readmitted in SCI centers located in regions other than the residency area was independently predictive of longer LoS. The comprehension of the most frequent secondary complications leading to readmission in more severe SCI may help to develop preventive strategies [21].
The long LoS was independently correlated with receiving assistance far from home due to the inability to find skilled health care services nearby the residency, linked also to the low prevalence of SCI among neurological conditions. The last point has already been demonstrated in acute care management [22]. Networks with precise geographical referrals can, however, assist in avoiding delays in taking care of secondary conditions and complications [23].
In the analysis of the geographic areas of readmission with respect to the area of origin for “health migration”, people from the south of Italy tend to move to centers located in the north (68%). Despite improvements in the health service network for people with SCI in Italy over the last few decades, the supply and demand for health services remain unbalanced. Accordingly, the National Health Service must be encouraged to better organize its healthcare network for individuals with SCI to cover the whole territory.
The data analysis allows an update of the general framework on any possible condition contributing to readmission, in order to avoid under-reporting the wide range of needs after SCI as suggested by principally qualitative evaluations [24] thus enlightening the main necessities. In more than 40% of the sample, a rehabilitation request was recorded among causes of readmission. This finding is consistent with the data found by Middleton et al. (11%) [18] and Skelton et al (12%) [7]. It mirrors also the characteristic of the Italian network of specialized SCI centers, which are mainly categorized as rehabilitation centers.
In a proportion of cases (12%), social needs were registered at admission. There was a direct significant correlation between this readmission cause and LoS causing a heavy burden (additional 32 days of stay) on the health care system. This aspect was also pointed out by research incorporating both medical and non-medical variables. Dryden et al. reported that multidisciplinary outreach services have a role to play in providing information and support for many aspects of not only medical but also social care for persons with SCI [25].
Providing adequate facilities and attention to pressure injuries is essential. Literature reports its impact as consequential when considering the LoS associated with this specific complication [8, 14, 18]. The median of LoS, considered as proxy of this burden, was 29 days in line with what was found by Pagliacci et al. (median = 28.5) [14], but not comparable with other studies [8, 18,19,20]. Maybe longer LoS found in this current study was due to the SCI center-based nature of the study that did not include minor and simplest cases. The LoS shows direct correlation with causes of readmission; in fact pressure injury is associated with increase in LoS, when treated by both conservative (21 days) and surgical methods (40 days after surgery). Pressure injury represents still a serious condition, affecting individuals with SCI with alarming consequences on their quality of life [26].
177 cases of readmission were attributed to respiratory complications, with 13,7% of cases requiring invasive surgical operations (such as tracheotomy and subsequent mechanical ventilation). This small but significant rate may be justified by the growing skill of SCI dedicated centers to manage persons with SCI suffering from high tetraplegia and respiratory failure.
According to our results, a large proportion of people with traumatic SCI had tetraplegia (40% with cervical ABC injuries). This may indicate a higher risk of complications and health care and/or rehabilitation needs in this more frail population [27], as identified also by non-neurological factors in comparison to individuals with paraplegia and incomplete D injuries [17, 28].
As a final note, 85% of the patients who were readmitted were male. Data presented here do not reflect general epidemiological rates, but rather the Italian reality. In fact, epidemiological data in Italy show a higher incidence of men with traumatic SCI in the last decades compared to other international countries [15]. However, due to the different objectives of the study, we were unable to determine whether sex can be considered a risk factor.
Some limitation of this study should be considered when interpreting the findings. The study design did not allow to explore the entire burden of readmission of a prevalent population or a cohort of persons with SCI and it was not possible to compare results of this study to others SCI population-based studies. Furthermore, it is to consider that a part of patients can be missed who were admitted to acute general medicine wards for complications and were not transferred to SCI centers. Besides, longitudinal SCI population-based studies of readmissions report that a part of people with long term needs after SCI may not have had access to specialized SCI centers. Indeed, in a sample of Individuals with SCI in Great Britain between 1990 and 1996, 64% required hospital treatment for late medical complications (127 patients, with 481 readmissions), but only 58% were readmitted into specialized SCI centers [8]. Finally, there is a long time between data collection and manuscript submission due to the long period between the completion of data collection, their extraction and analysis, and the numerous group meetings for discussion of the results and consensus on the concept for the manuscript preparation.
In this study, readmissions shorter than 72 h were not considered since, in Italy, they are usually linked to non-complicated issues and did not reflect the study objectives. This implies that a high number of readmissions caused by urological problems (data not included), such as urological minimally invasive surgery, which usually does not require hospitalization, may have been ruled out. All the readmissions considered for this study are referred to people who had completed the rehabilitation of the acute SCI and had been discharged at least 1 year before the readmission. Only SCI readmissions among the network of specialized SCI centers were considered, hence missing cases with exclusively mild rehabilitation and/or minor medical needs.
This remains an important study that sheds light on readmissions and complications among individuals with Traumatic SCI in Italy that will hopefully inform care, policy, and further studies to improve long-term outcomes.
Data availability
The data supporting the findings of this study are available as supplementary data.
References
Johnson RL, Gerhart KA, McCray J, Menconi JC, Whiteneck GG. Secondary conditions following spinal cord injury in a population-based sample. Spinal Cord. 1998;36:45–50.
Ackery A, Tator C, Krassioukov A. A global perspective on spinal cord injury epidemiology. J Neurotrauma. 2004;21:1355–70.
Adriaansen JJ, Ruijs LE, van Koppenhagen CF, van Asbeck FW, Snoek GJ, van Kuppevelt D, et al. Secondary health conditions and quality of life in persons living with spinal cord injury for at least ten years. J Rehabil Med. 2016;48:853–60.
Ferro S, Cecconi L, Bonavita J, Pagliacci MC, Biggeri A, Franceschini M, et al. Incidence of traumatic spinal cord injury in Italy during 2013-2014: a population-based study. Spinal Cord. 2017;55:1103–7.
National Spinal Cord Injury Statistical Center NSCISC, Annual Statistical Report 2020.https://www.nscisc.uab.edu/.
DeJong G, Tian W, Hsieh CH, Junn C, Karam C, Ballard, et al. Rehospitalization in the first year of traumatic spinal cord injury after discharge from medical rehabilitation. Arch Phys Med Rehabil. 2013;94:S87–97.
Skelton F, Hoffman JM, Reyes M, Burns SP. Examining health-care utilization in the first year following spinal cord injury. J Spinal Cord Med. 2015;38:690–5.
Savic G, Short DJ, Weitzenkamp D, Charlifue S, Gardner BP. Hospital readmissions in people with chronic spinal cord injury. Spinal Cord. 2000;38:371–7.
Jaglal SB, Munce SE, Guilcher SJ, Couris CM, Fung K, Craven BC, et al. Health system factors associated with rehospitalizations after traumatic spinal cord injury: a population-based study. Spinal Cord. 2009;47:604–9.
Gabbe BJ, Nunn A. Profile and costs of secondary conditions resulting in emergency department presentations and readmission to hospital following traumatic spinal cord injury. Injury. 2016;47:1847–55.
Jensen MP, Truitt AR, Schomer KG, Yorkston KM, Baylor C, Molton IR, et al. Frequency and age effects of secondary health conditions in individuals with spinal cord injury: a sco** review. Spinal Cord. 2013;51:882–92.
Krause JS, Murday D, Corley EH, DiPiro ND. Concentration of costs among high utilizers of health care services over the first 10 years after spinal cord injury rehabilitation: a population-based study. Arch Phys Med Rehabil. 2019;100:938–44.
Ivie CS 3rd, DeVivo MJ. Predicting unplanned hospitalizations in persons with spinal cord injury. Arch Phys Med Rehabil. 1994;75:1182–8.
Pagliacci MC, Celani MG, Spizzichino L, Zampolini M, Franceschini M. Gruppo Italiano Studio Epidemiologico Mielolesioni (GISEM) group. Hospital care of postacute spinal cord lesion patients in Italy: analysis of readmissions into the GISEM study. Am J Phys Med Rehabil. 2008;87:619–26.
Franceschini M, Bonavita J, Cecconi L, Ferro S, Pagliacci MC, Italian SCI Study Group. Traumatic spinal cord injury in Italy 20 years later: current epidemiological trend and early predictors of rehabilitation outcome. Spinal Cord. 2020;58:768–77. https://doi.org/10.1038/s41393-020-0421-y.
DeVivo MJ, Biering-Sørensen F, New P, Chen Y. International spinal cord injury data set. Standardization of data analysis and reporting of results from the International Spinal Cord Injury Core Data Set. Spinal Cord. 2011;49:596–9.
Cardenas DD, Hoffman JM, Kirshblum S, McKinley W. Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil. 2004;85:1757–63.
Middleton JW, Lim K, Taylor L, Soden R, Rutkowski S. Patterns of morbidity and rehospitalisation following spinal cord injury. Spinal Cord. 2004;42:359–67.
Paker N, Soy D, Kesiktaş N, Nur Bardak A, Erbil M, Ersoy S, et al. Reasons for rehospitalization in patients with spinal cord injury: 5 years’ experience. Int J Rehabil Res. 2006;29:71–6.
Dorsett P, Geraghty T. Health-related outcomes of people with spinal cord injury-a 10 year longitudinal study. Spinal Cord. 2008;46:386–91.
Consortium for Spinal Cord Medicine. Early acute management in adults with spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2008;31:403–79.
Wing PC. Early acute management in adults with spinal cord injury: a clinical practice guideline for health-care providers. Who should read it? J Spinal Cord Med. 2008;31:360.
Ronca E, Brunkert T, Koch HG, Jordan X, Gemperli A. Residential location of people with chronic spinal cord injury: the importance of local health care infrastructure. BMC Health Serv Res. 2018;18:657.
Braaf SC, Lennox A, Nunn A, Gabbe BJ. Experiences of hospital readmission and receiving formal carer services following spinal cord injury: a qualitative study to identify needs. Disabil Rehabil. 2018;40:1893–9.
Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord. 2004;42:513–25.
Mashola MK, Olorunju SAS, Mothabeng J. Factors related to hospital readmissions in people with spinal cord injury in South Africa. S Afr Med J. 2019;109:107–11.
Lee BB, Cripps R, New P, Fitzharris M, Noonan V, Hagen EM, et al. Demographic profile of spinal cord injury. In: Chhabra HS (ed). ISCoS-textbook on comprehensive management of spinal cord injuries. 1st ed. New Delhi, Wolters Kluwe Polska; 2015. pp. 36–52.
Charlifue S, Lammertse DP, Adkins RH. Aging with spinal cord injury: changes in selected health indices and life satisfaction. Arch Phys Med Rehabil. 2004;85:1848–53.
Acknowledgements
This study was financed within the framework of the 2012 CCM Program. CCM is the National Center for Disease Prevention and Control whose task is to liaise with the Ministry of Health and the regional governments as far as surveillance and prevention are concerned and whose aim is to promptly respond to emergencies. http://www.ccm-network.it/progetto.jsp?id=node/1846&idP=740.
Funding
This study was funded by Italian Ministry of Health (CCM, and Ricerca Corrente).
Author information
Authors and Affiliations
Consortia
Contributions
MF, JB, SF, MCP contributed to the conceptualization and the study design, ethical aspects and acquired data. LC contributed to the statistical analysis. All the authors contributed to the ethical aspects and interpreting the results. MF, JB, SF and MCP drafted the manuscript for important intellectual content. MF, SP and MCP revised the manuscript. JB and SP edited it. All the authors red and approved the final version. All the authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The current study was approved and obtained a grant from Italian Ministry of Health (code: CCM number 15756 of 17-07-2012). The study was conducted according to the guidelines of the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Franceschini, M., Cecconi, L., Bonavita, J. et al. Causes and length of stay of readmission among individuals with traumatic spinal cord injury: a prospective observational cohort study. Spinal Cord 61, 383–390 (2023). https://doi.org/10.1038/s41393-023-00874-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00874-6
- Springer Nature Limited