Abstract
Introduction
Extremely low birth weight (ELBW) survivors have microvascular structural differences already described in kidney and retina, suggesting changes in endothelial integrity. A biomarker of endothelial integrity is perfused boundary region (PBR), which measures glycocalycal thickness. The endothelial glycocalyx is a complex, highly versatile structure with essential roles in vascular integrity and function. We explored PBR patterns together with other microvascular markers in healthy controls and former ELBW children.
Methods
In the PREMATCH cohort (87 healthy controls, 93 ELBW survivors), we assessed endothelial integrity by calculating PBR (sidestream dark-field imaging), several microvascular markers (blood pressure, estimated glomerular filtration rate (eGFRcysC)), and retinal imaging in early adolescence. We explored differences between both groups, and searched for perinatal determinants of PBR and correlations between different microvascular markers.
Results
We provided reference values for PBR (average 1.90 µm, SD 0.30) in children. PBR was not different from ELBW survivors during early adolescence, despite their higher blood pressure, lower eGFRcysC, and different retinal vessel width and tortuosity.
Conclusions
We generated reference values for PBR in early adolescence. Despite some correlations between microvascular parameters, there seem to be numerous confounders to propose PBR as a marker for endothelial integrity in ELBW survivors.
Impact
-
The endothelial glycocalyx is a complex and versatile structure. Changes in blood pressure and retinal and renal vascularization suggest a disturbance of its integrity in extremely low birth weight (ELBW) survivors. Its thickness can be measured by calculating perfused boundary region (PBR) using sidestream dark-field imaging, with a higher PBR indicating a thinner glycocalyx.
-
We generated reference values for PBR in healthy adolescents. These values were not different in former ELBW children.
-
Despite some correlations of PBR with other microvascular biomarkers, these are not strong enough to describe endothelial integrity and its covariates in former ELBW children.
Similar content being viewed by others
Introduction
As the survival rate after extreme prematurity has substantially increased, complications in former preterms during adulthood became even more relevant. Former extremely low birth weight children (ELBW, birth weight <1000 g), either born preterm (appropriate for gestational age, AGA) or small for gestational age (SGA), have an overall increased mortality rate as an increased risk of cardiovascular disease.1,2 Recent research has shown that ELBW survivors have higher blood pressure during childhood and an increased risk to develop arterial hypertension and lipid disorders in later life, as well as an increased incidence of stroke, ischemic heart disease, and heart failure.3,4,5,6,7,8,9,10 This multi-organ involvement is supported by evidence of reduced kidney function in former extremely low-weight neonates, as well as changes in retinal microcirculation.11,12
These findings align with the Developmental Origins of Adult Health and disease (DOHaD) paradigm, which suggests that the entire developmental period contributes to the occurrence of adult-onset diseases.13 Different potential mechanisms for the association between prematurity and vascular disease have been studied.14 One of the causative pathways being explored is the effect of prematurity on microcirculation. Different studies have shown that former preterm children have reduced flow-mediated vasodilation and increased carotid intima-media thickness.15,16 Moreover, an association of prematurity with increased circulating endothelial progenitor cells and circulating endothelial microparticles was found, supporting altered endothelial integrity as the possible mechanism underlying this risk.17,18
The endothelial glycocalyx is a complex, highly versatile structure that has essential roles in vascular integrity and function.19 In severe illnesses such as sepsis, altered endothelial integrity is reported, possibly following vascular inflammation.20 Besides biochemical biomarkers, glycocalycal thickness can be estimated by calculating the perfused boundary region (PBR, µm). PBR is inversely correlated with the thickness of the endothelial glycocalyx, as loss of integrity allows for deeper penetration of red blood cells into this gel-like layer covering the endothelial lining.17,18,21 An increased PBR signifies a disruption in the endothelial glycocalyx and is associated with changes in microcirculation and a higher prevalence of ischemic heart disease in adults.22,23
In children, there are not yet any reference values for PBR. In the PREMATCH cohort, consisting of 93 former ELBW children and 87 healthy controls, a broad range of tests was conducted during early adolescence, with the purpose of describing their vascular phenotype.24
The objective of the current analysis was to explore PBR patterns in healthy controls and former ELBW children, to provide reference values for PBR in children, and to determine whether PBR is associated with other microvascular markers, particularly in kidney and retina, and could serve as a biomarker for endothelial integrity after prematurity. In the ELBW cases, we searched for perinatal determinants of PBR, both separately and combined into a model.
Methods
Ethics
This study has been conducted in accordance with the Helsinki Declaration for Investigation in Human Subjects. The Ethics Committee of the University Hospitals Leuven (Belgium) approved the study protocol.24 Based on good clinical practice guidance and national law, parents or custodians provided written informed consent, while the children gave informed assent. The study was registered at ClinicalTrials.gov (NCT02147457).
Subjects
All ELBW survivors who were admitted to the Neonatal Intensive Care Unit of UZ Leuven, Belgium between 2000 and 2005 with a well-documented file regarding perinatal characteristics, comorbidities, and care, were invited to participate in the study at the mean age of 11 years.25 Of 140 invited children, 93 agreed to participate (66.4%). In total, the PREMATCH cohort consisted of 93 ELBW survivors and 87 sex- and age-matched, healthy, term-born controls, either friends of the cases (n = 41) or recruited at an elementary school near the research center in Eksel, Belgium (n = 46) (Fig. 1).26 Both cases and controls underwent an extensive series of examinations to describe the vascular profile of the children during early adolescence (median age 11 years). Perinatal data were retrospectively extracted from maternal and neonatal chart reviews.25
Measurements
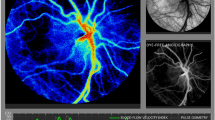
The capillary glycocalyx was visualized in two areas lateral to the frenulum and 3–4 cm anterior to the tongue base using sidestream dark-field imaging with a Handheld Video Capillary Microscope (KK Research Technology, Honiton, United Kingdom). Afterward, the GlycoCheck® (GlycoCheck, Maastricht, The Netherlands) software calculated the PBR (µm). This software also provides total and perfused capillary density (segments per square millimeter). A detailed description of all techniques used for data collection is available in the study protocol and the paper by Gu et al.24,27
Blood pressure was measured using the auscultatory Korotkoff approach (UM-101A, A&D Medical San Jose, CA), in a sitting position after resting for 5 min, using the appropriate cuff size and according to standard guidelines.28 Out of three measurements, mean systolic blood pressure (mmHg), mean diastolic blood pressure (mmHg), and mean arterial pressure (MAP, mmHg) were calculated.
Blood samples were collected after the application of a Rapydan® patch (70 mg lidocaine/70 mg tetracaine, Eurocept, Ankeveen, The Netherlands). Reasons for the unavailability of blood samples were refusal of the child (n = 10), too low sample volume (n = 12), or inability to collect blood after one or two attempts, as a predefined threshold to stop (n = 28). Laboratory testing included serum Cystatin C values (particle-enhanced turbidimetric immunoassay, Integra 400 system, Roche Diagnostics, Basel, Switzerland), from this the Cystatin C-based estimated glomerular filtration rate (eGFRcysC) was calculated.11
Retinal imaging was performed using a Canon Cr-DGi (Canon Co., Kyoto, Japan) non-mydriatic retinal visualization system by two observers. Before obtaining measurements, investigators were trained by interpreting repeated measurements in 30 children, and inter- and intra-observer variability was assessed using intraclass correlation coefficients. The observers took one photo per eye in a dim-lit room.29 The SIVA software (Singapore Eye Research Institute, Singapore), combined the individual measurements into summary indices: central retinal arteriolar equivalent (CRAE), central retinal venular equivalent (CRVE), and arteriole-to-venule ratio (AVR).30 For the intra-observer repeatability, the correlation coefficients were 0.98 for CRAE, 0.99 for CRVE, and 0.98 for AVR, and for inter-observer reproducibility, they were 0.94, 0.93, and 0.87, respectively.12 The software also calculated retinal vessel tortuosity, calculated as the difference between the actual path length of the vessel segment measured by tracking and the straight-line length of the segment divided by the straight-line length.
Data analysis and statistics
For database management and statistical analysis, we used the IBM SPSS system (version 28). To assess correlation, we used Pearson correlation for nominal data, Kendall’s tau test for ordinal data. Continuous variables were tested for normal distribution using a Shapiro–Wilk test, normally distributed variables were expressed as mean and standard deviation (SD), not normally distributed variables as median and interquartile range (IQR). Group means were assessed using appropriate (non)parametric tests (Mann–Whitney U test or independent t-test). Categorical variables were expressed as proportions, and differences in frequency distributions were assessed using one-way ANOVA. Multiple regression analyses were performed to check for a linear association of the number of perinatal determinants with PBR.
Missing data points were not included in further analysis. Outliers (third quartile + 1.5 times the IQR or first quartile – 1.5*IQR) were treated as missing values: a total of 26 outliers were removed from over 3000 measurements. The frequency of outliers was comparable between case and control groups. A two-tailed P level < 0.05 was considered significant.
Results
Perinatal characteristics
Of the 87 controls and the 93 ELBW cases in the PREMATCH cohort, 77 controls and 66 cases completed imaging of the sublingual endothelial glycocalyx. Controls had a median GA of 39 (IQR 2) weeks, and birth weight of 3355 g (IQR 598 g), cases had a median GA of 27 weeks (IQR 2 weeks), and birth weight of 815 g (IQR 165 g). A total of 42 (48.3%) of the controls and 47 (50.5%) of the case children were male. A detailed description of perinatal characteristics in cases can be found in Table 1. Characteristics of cases and controls during early adolescence are given in Tables 2 and 3. Compared to the former ELBW children who did not undergo imaging, included cases had a longer duration of oxygen suppletion and antenatal lung maturation was administered more frequently.
Endothelial biomarkers in healthy controls and ELBW cases
In healthy controls, PBR was on average 1.91 µm (SD 0.32) at the mean age of 11 years. In cases, it was on average 1.88 µm (SD 0.28) (Table 4). A scatterplot of PBR values can be found in Fig. 2. PBR observations between the case and control group were not significantly different. Cases did have significantly higher mean blood pressure (MAP 83 vs 78 mmHg, P < 0.001) and lower eGFRcysC (79 vs 89 mL/min/1.73 m2, P = 0.002) compared with controls. In cases, CRAE (156.39 vs 170.91, P < 0.001), CRVE (223.26 vs 231.52, P < 0.001) and AVR (0.70 vs 0.74, P < 0.001) were significantly lower. Cases had significantly higher vascular tortuosity (1.12 vs 1.10, P < 0.001), more pronounced in arterioles (1.14 vs 1.11, P < 0.001) compared to venules (1.10 vs 1.09, P < 0.001).
A Kendall’s tau correlation showed no significant association of PBR with either blood pressure or eGFRcysC. A Pearson correlation showed a significant association of PBR with vessel tortuosity (rp = 0.278, P = 0.007) in cases, this finding could not be reproduced in the control groups. There was no confounding of age, height, or weight at the time of data acquisition, we did find that PBR was significantly higher in girls compared to boys (1.94 vs 1.85 µm, P = 0.039) in cases, these findings could not be reproduced in the control group.
Determinants of perfused boundary region in ELBW survivors
We searched for perinatal determinants of PBR in the case group. PBR was not significantly correlated with either GA or birth weight. Kendall’s tau correlation showed a significant correlation with AGA (rpb = −0.259, P = 0.036), APGAR score below 5 at 1 min (rpb = 0.315, P = 0.011), use of ibuprofen for pharmacological closure of a patent ductus arteriosus (rpb = −0.264, P = 0.033) and parenteral nutrition ≥28 days (rpb = 0.266, P = 0.037). We performed independent samples t-tests to explore the influence of the different perinatal determinants, described in Table 5.
In a secondary analysis combining these characteristics into a model, awarding 1 point to each of the determinants (AGA, APGAR1 <5, NSAIDs and parenteral nutrition ≥28 days), we found an increasing PBR with the number of determinants present during the perinatal period (Fig. 3). A multiple regression was run and the model significantly predicted PBR, F(4,57) = 4.475, P = 0.003, R2 = 0.239.
Discussion
This study explored PBR findings in normal birth weight, former term-born children, and former ELBW cases in early adolescence. Data were collected using the PREMATCH cohort, a group of 87 healthy controls and 93 ELBW children, in whom the glycocalyx was studied as part of an extensive microcirculatory assessment during a study visit at the median age of 11 years. We hereby generated reference values for PBR in early adolescence. We have not observed a significant difference in PBR between those healthy controls and ELBW cases despite their elevated blood pressure, lower eGFRcysC, and altered retinal microvasculature. PBR was significantly correlated with retinal vascular tortuosity, not with blood pressure or eGFRcysC. In subgroups of ELBW cases with certain perinatal determinants (AGA, APGAR1 <5, NSAIDs, parenteral nutrition ≥28 days), PBR was significantly elevated.
There are not yet any reference values for PBR in children, so we have generated the first data in children around the age of 11 (Table 4). Such observations should be further documented in different pediatric subpopulations of different ages or puberty scores, as pubertal maturation is likely relevant in such reference values. As previously reported, the Tanner puberty scores in the PREMATCH study reflect early puberty (breast/genital 2.3, SD 0.87 and pubic 2.2, SD 0.96). A controlled environment is also of importance, as PBR is influenced by ambient temperature, our evaluations took place in an air-conditioned room.
It is to be noted that in the case group, PBR values differed significantly between both sexes, whereas the difference in the control group was not significant. This could be explained by the assumption that our control group is more homogeneous and overall healthy, whereas the ELBW survivors are a more heterogenic group (e.g., preterm or SGA), which could cause subclinical differences to be more pronounced. As this is an exploratory study, it is an interesting finding that warrants further study.
Our study did not find a significant association of ELBW with increased PBR. This is an unexpected finding, since altered endothelial integrity is suggested by the altered retinal microcirculation, as well as described in other studies using different endothelial biomarkers (circulating endothelial progenitor cells, circulating endothelial microparticles).17,18 Furthermore, elevated PBR was associated with impaired microvascular perfusion and cardiovascular events in adults.22,23 A possible explanation could be that other determinants in the neonatal period, such as nutritional strategy, glycemia levels, or intercurrent infections, are needed to influence endothelial integrity in young adolescence, which is supported by the findings in the ELBW group and in line with the DOHaD paradigm.
We attempted to construct a scoring model to further detect former ELBW children at higher risk for loss of endothelial integrity, and found that PBR increased with the number of determinants present during the perinatal period (AGA, APGAR1 <5, NSAIDs and parenteral nutrition ≥28 days). Again, as exploratory in its design, this model should be validated in further studies with different ELBW cohorts, as it could be a tool to define children at risk, enabling targeted secondary prevention strategies. The model suggests a higher PBR in children who had a birth weight appropriate for their GA, in contrast to children born SGA. This relative advantage of SGA preterms could be inherent to our cohort design (ELBW, i.e., birth weight <1000 g), resulting in the inclusion of relatively more mature, but SGA children in a weight-based cohort (38.7%), compared to GA-based prematurity cohorts, as we discussed in previous research.26 As PBR is higher in SGA cases, our analysis suggests that growth status plays a role in the overall risk calculation. Obviously, this is at present also only an exploratory finding, and without difference in eGFR and retinal vasculature between AGA and SGA children.
It is hereby relevant to note that PBR only measures the endoluminal part of the glycocalyx, and that endothelial integrity disruption could be more pronounced in other components of the capillary endothelium. This could potentially explain why other indicators, such as circulating endothelial progenitor cells or circulating microparticles, did find an association of prematurity with altered endothelial integrity.17,18 Lastly, a recent report on PBR in the neonatal period showed a significant increase in PBR at the corrected age of 30 weeks postmenstrual age in preterms, after initially decreased values at birth (mean difference 0.2–0.3 µm).31 These results indicate PBR is a variable parameter, and could possibly recuperate after an adverse event, potentially explaining why we could not reproduce these findings in early adolescence.
Even though PBR did not describe a direct relationship of ELBW with altered endothelial integrity, other findings suggest microvascular abnormalities: cases had higher blood pressure, lower eGFRcysC, and retinal vessel diameter and tortuosity. Furthermore, PBR correlated significantly with retinal vascular tortuosity. We need to further search for an eligible biomarker describing the endothelial and microcirculatory risk profile in ELBW survivors.
This study should be interpreted within the context of its strengths and limitations. Firstly, it was a homogeneous single-center study with extensive phenoty** of a former ELBW cohort, ensuring an optimal and standardized perinatal treatment, with well-documented and earlier reported perinatal data including complications.25 Secondly, our study assessed a pre-clinically increased cardiovascular risk profile in a non-invasive manner, which could help in the primary prevention of complications. This is also a limitation, as PBR serves as a surrogate endpoint or biomarker for cardiovascular disease. Increased PBR indicating thinner glycocalyx describes a certain risk profile, which is associated with higher cardiovascular risk during adulthood. However, it is not a definite endpoint and therefore a degree of uncertainty should be introduced. Finally, there was no a priori power calculation, so all analyses are rather exploratory, and need further studies. For the power calculations of such future studies, it is relevant to mention that some children were unable to tolerate the sublingual measurements and we stopped the examination upon the first indication of intolerance, causing an increase in missing data.
Moreover, this was a cross-sectional study and longitudinal assessment could be of additional benefit. The use of PBR as a marker for glycocalycal thickness has not yet been reported in former ELBW cases, and more research on its accuracy needs to be conducted, in different populations and environmental conditions. Until more reference data in heterogeneous pediatric cohorts become available, we hereby suggest using the PBR threshold (≥2 µm), as applied in adults, as this is associated with microvascular changes and atherosclerosis.23
Conclusion
This study compared a group of healthy controls to former ELBW children during early adolescence to define their microvascular risk profile, using PBR as an indicator of endothelial integrity, calculated by non-invasive visualization of the sublingual capillary endothelium. We provide the first reference values for PBR in early adolescence, which are to be validated in further research. PBR did not significantly differ between healthy controls and ELBW cases but was correlated with retinal tortuosity in former ELBW children. Furthermore, other microvascular markers (blood pressure, eGFRcysC, retinal imaging) suggest alterations in microcirculation. In subgroups of ELBW cases with certain perinatal determinants (AGA, APGAR1 <5, NSAIDs, parenteral nutrition ≥28 days), PBR was significantly elevated. We conclude there are many confounding factors impeding the direct relationship of PBR with endothelial integrity.
Data availability
The corresponding author can be contacted to share the raw data, if based on a reasonable request and study protocol.
References
Risnes, K. et al. Mortality among young adults born preterm and early term in 4 Nordic nations. JAMA Netw. Open 4, e2032779, https://jamanetwork-com.kuleuven.e-bronnen.be/journals/jamanetworkopen/fullarticle/2774718 (2021).
Stock, K. et al. The impact of being born preterm or small for gestational age on early vascular aging in adolescents. J. Pediatr. 201, 49–54.e1, https://pubmed.ncbi.nlm.nih.gov/29960764/ (2018).
de Jong, F., Monuteaux, M. C., van Elburg, R. M., Gillman, M. W. & Belfort, M. B. Systematic review and meta-analysis of preterm birth and later systolic blood pressure. Hypertension 59, 226–234, https://pubmed.ncbi.nlm.nih.gov/22158643/ (2012).
Haikerwal, A. et al. High blood pressure in young adult survivors born extremely preterm or extremely low birthweight in the post surfactant era. Hypertension 75, 211–217, https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.119.13780 (2020).
Juonala, M. Effect of birth weight on life-course blood pressure levels among children born premature: The Cardiovascular Risk in Young Finns Study. J. Hypertension 33, 1542–1548 (2015).
Crump, C., Sundquist, J. & Sundquist K. Association of preterm birth with lipid disorders in early adulthood: a Swedish cohort study. PLoS Med. 16, e1002947. https://pubmed.ncbi.nlm.nih.gov/31626652/ (2019).
Crump, C., Sundquist, J. & Sundquist, K. Risk of hypertension into adulthood in persons born prematurely: a national cohort study. Eur. Heart J. 41, 1542–1550. https://pubmed.ncbi.nlm.nih.gov/31872206/ (2020).
Crump, C., Sundquist, J. & Sundquist, K. Stroke risks in adult survivors of preterm birth: National Cohort and Cosibling Study. Stroke 52, 2609–2617, https://www-ahajournals-org.kuleuven.e-bronnen.be/doi/abs/10.1161/STROKEAHA.120.033797 (2021).
Crump, C. et al. Association of preterm birth with risk of ischemic heart disease in adulthood. JAMA Pediatr. 173, 736–743, https://pubmed.ncbi.nlm.nih.gov/31157896/ (2019).
Carr, H., Cnattingius, S., Granath, F., Ludvigsson, J. F. & Bonamy, A. K. E. Preterm birth and risk of heart failure up to early adulthood. J. Am. Coll. Cardiol. 69, 2634–2642 (2017).
Raaijmakers, A. et al. Does extremely low birth weight predispose to low-renin hypertension? Hypertension 69, 443–449, https://pubmed-ncbi-nlm-nih-gov.kuleuven.ezproxy.kuleuven.be/28115515/ (2017).
Wei, F. F. et al. Association between cognition and the retinal microvasculature in 11-year old children born preterm or at term. Early Hum. Dev. 118, 1–7 (2018).
Suzuki, K. The develo** world of DOHaD. J. Dev. Orig. Health Dis. 9, 266–269. https://doi.org/10.1017/S2040174417000691 (2018).
Bavineni, M. et al. Mechanisms linking preterm birth to onset of cardiovascular disease later in adulthood. Eur. Heart J. 40, 1107–1112, https://pubmed.ncbi.nlm.nih.gov/30753448/ (2019).
Bassareo, P. P. et al. Reduced brachial flow-mediated vasodilation in young adult ex extremely low birth weight preterm: a condition predictive of increased cardiovascular risk? J. Matern. Fetal Neonatal Med. 23, 121–124. https://www.tandfonline.com/action/journalInformation?journalCode=ijmf20 (2010).
Lee, H. N., Dichtl, S., Mormanova, Z., Dalla Pozza, R. & Genzel-Boroviczeny, O. In adolescence, extreme prematurity is associated with significant changes in the microvasculature, elevated blood pressure and increased carotid intima – media thickness. Arch. Dis. Child. Educ. Pract. Ed. 99, 907–911, https://pubmed.ncbi.nlm.nih.gov/24879769/ (2014).
Markopoulou, P. et al. Increased circulating endothelial progenitor cells (EPCs) in prepubertal children born prematurely: a possible link between prematurity and cardiovascular risk. Pediatr. Res. 90, 156–165 https://pubmed.ncbi.nlm.nih.gov/33038874/ (2021).
Markopoulou, P. et al. Elevated circulating endothelial microparticles (EMPs) in prepubertal children born preterm. Pediatr. Res. 91, 1754–1761 https://pubmed.ncbi.nlm.nih.gov/34285352/ (2022).
Ushiyama, A., Kataoka, H. & Iijima T. Glycocalyx and its involvement in clinical pathophysiologies. J. Intensive Care 4, 59. https://pubmed.ncbi.nlm.nih.gov/27617097/ (2016).
Rovas, A. et al. Association of sublingual microcirculation parameters and endothelial glycocalyx dimensions in resuscitated sepsis. Crit. Care 23, 1–11, https://ccforum.biomedcentral.com/articles/10.1186/s13054-019-2542-2 (2019).
Hubble, S. M. A., Kyte, H. L., Gooding, K. & Shore, A. C. Variability in sublingual microvessel density and flow measurements in healthy volunteers. Microcirculation 16, 183–191, https://pubmed.ncbi.nlm.nih.gov/19206003/ (2009).
Lee, D. H. et al. Deeper penetration of erythrocytes into the endothelial glycocalyx is associated with impaired microvascular perfusion. PLoS ONE 9, e96477 https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0096477 (2014).
Gorshkov, A. Y., Klimushina, M., Boytsov, S. A., Kots, A. Y. & Gumanova, N. G. Increase in perfused boundary region of endothelial glycocalyx is associated with higher prevalence of ischemic heart disease and lesions of microcirculation and vascular wall. Microcirculation 25, e12454. https://pubmed-ncbi-nlm-nih-gov.kuleuven.ezproxy.kuleuven.be/29608790/ (2018).
Raaijmakers, A. et al. Design and feasibility of “PREMATurity as predictor of children’s Cardiovascular-renal Health” (PREMATCH): a pilot study. Blood Press 24, 275–283. https://www.tandfonline.com/action/journalInformation?journalCode=iblo20 (2015).
George, I., Mekahli, D., Rayyan, M., Levtchenko, E. & Allegaert, K. Postnatal trends in creatinemia and its covariates in extremely low birth weight (ELBW) neonates. Pediatr. Nephrol. 26, 1843–1849, https://pubmed.ncbi.nlm.nih.gov/21499946/ (2011).
Raaijmakers, A. et al. Catch–up growth in the first two years of life in extremely low birth weight (ELBW) infants is associated with lower body fat in young adolescence. PLoS ONE 12, e0173349. https://dx.plos.org/10.1371/journal.pone.0173349 (2017).
Gu, Y. M. et al. Characteristics and determinants of the sublingual microcirculation in populations of different ethnicity. Hypertension 65, 993–1001, https://www-ahajournals-org.kuleuven.e-bronnen.be/doi/abs/10.1161/HYPERTENSIONAHA.114.05119 (2015).
Muntner, P. et al. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension 73, E35–66, https://www.heart.org/permissions (2019).
Wei, F. F. Retinal microvascular diameter, a hypertension-related trait, in ECG-gated vs. non-gated images analyzed by IVAN and SIVA. Hypertension Res. 39, 12, https://www.nature.com.kuleuven.e-bronnen.be/articles/hr201681 (2016).
Huang, Q. F. et al. Reproducibility of retinal microvascular traits decoded by the Singapore I Vessel Assessment Software across the human age range. Am. J. Hypertension 31, 438–449, https://academic-oup-com.kuleuven.e-bronnen.be/ajh/article/31/4/438/4657093 (2018).
Puchwein-Schwepcke, A., Artmann, S., Rajwich, L., Genzel-Boroviczény, O. & Nussbaum, C. Effect of gestational age and postnatal age on the endothelial glycocalyx in neonates. Sci. Rep. 11, 3133. https://pubmed.ncbi.nlm.nih.gov/33542284/ (2021).
Acknowledgements
We gratefully acknowledge the contribution of the nurses working at the examination center (Linda Custers, Marie-Jeanne Jehoul, Daisy Thijs, and Hanne Truyens) and the clerical staff at the Studies Coordinating Centre at the time of data acquisition (Vera De Leebeeck and Renilde Wolfs).
Funding
The PREMATCH study was supported by the Agency for Innovation by Science and Technology in Flanders (IWT) through the SAFE-PEDRUG project [IWT/SBO 130033]. KU Leuven Internal Funds (STG-18–00379) supported the Research Unit Hypertension and Cardiovascular Epidemiology, Department of Cardiovascular Sciences, Leuven.
Author information
Authors and Affiliations
Contributions
K.A., E.L., J.A.S., and A.R. conceived and designed the PREMATCH study and obtained the funding. The data on perfused boundary region were analyzed by L.v.L, assisted by K.A., J.A.S., and A.R. All authors were involved in the interpretation and drafting of the manuscript, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Parents or custodians and children provided written informed consent and assent respectively.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Van Loo, L., Allegaert, K., Levtchenko, E. et al. Perfused boundary region as biomarker for endothelial integrity in former preterms in adolescence. Pediatr Res 93, 1936–1942 (2023). https://doi.org/10.1038/s41390-022-02321-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02321-3
- Springer Nature America, Inc.