Abstract
Purpose
Peripheral T-cell lymphoma (PTCL) is notorious for its heterogeneity as well as poor prognosis. High mortality remains a challenge. Our study aims to assess whether the leukocyte-lymphocyte ratio (LLR) and neutrophil-lymphocyte ratio (NLR) can be applied as prognostic indexes for patients with PTCL and supplement the prognostic system of PTCL.
Methods
We reviewed the data of 108 newly diagnosed PTCL patients in the clinic. The χ2 test was applied to contrast baseline characteristics between patients in different groups divided according to the cut-off value of LLR or NLR. The Kaplan-Meier method was adapted to develop the survival curve. The COX ratio risk regression model was used to identify the indexes related to patient survival.
Results
LLR ≥ 10.30, NLR ≥ 8.25, Eastern Cooperative Oncology Group (ECOG) score ≥ 2, International prognostic index (IPI) score > 2, Prognostic Index for T cell lymphoma (PIT) ≥ 2, B symptom, Ann Arbor stage III-IV and high level of Lactic dehydrogenase (LDH) were poor prognosis factors impacting patients’ overall survival (OS) by the univariate analysis. The multivariate analysis illustrated that only LLR ≥ 10.30 was significantly related to OS (P all < 0.05).
Conclusion
Overall, our analysis revealed that LLR ≥ 10.30 was significantly associated with poorer OS and was a novel prognostic index for PTCL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Peripheral T-cell lymphoma (PTCL) is a group of malignant lymphoma, which is renowned for its poor clinical outcomes. It is highly aggressive and exhibits a poor response to conventional chemotherapy. PTCL accounts for about 25–30% of non-Hodgkin’s lymphomas (NHL) in China [1]. Whereas, the prevalence of PTCL in Western countries is lower than in Asia. It comprises approximately 10% of all NHL in Western countries, with an annual incidence rate of 0.5-2 per 100,000 people [2].
In recent decades, several prognostic tools for PTCL have been proposed, among which the International Prognostic Index (IPI) consisting of age, performance status (PS), lactate dehydrogenase (LDH) level, Ann Arbor stage, and extranodal involvement [3], and the Prognostic Index for T cell lymphoma (PIT) are the most commonly used. PIT, consisting of age, PS, LDH, and bone marrow (BM) involvement, was made particularly for cases with Peripheral T-cell lymphoma, not otherwise specified (PTCL,NOS) [4]. Both IPI and PIT are confirmed to be related to progression-free survival, overall survival (OS), and therapeutic response in cases with PTCL [5]. Even so, high mortality remains an urgent problem to solve, requiring the discovery of additional prognostic indexes to better the outcomes of patients further. It has been demonstrated that cancer-related inflammation and host immune function have a significant impact on accelerating cancer progression and deciding patients’ outcomes [6]. Paydas et al. investigated the prognostic value of the leukocyte-lymphocyte ratio (LLR) by combining it and the prognostic nutritional index (PNI) into the IPS-3 system and develo** new scores systems as prognostic tools in patients with classical Hodgkin lymphoma [7]. Several elements and derivatives of the complete blood count (CBC) when diagnosed have been investigated extensively as prognostic factors in a variety of tumors in recent years, among which the neutrophil-to-lymphocyte ratio (NLR) has been confirmed to indicate prognostic significance in solid tumors and hematologic malignancies [8,9,10,11]. However, for PTCL, these parameters have not been widely explored yet.
Our study aims to evaluate whether LLR and NLR can be applied as prognostic indexes for patients with PTCL and add new information to the prognostic system of PTCL.
2 Materials and methods
2.1 Patient selection
We retrospectively went over 108 newly diagnosed PTCL patients treated at the Harbin Medical University Cancer Hospital from February 2005 to July 2017. The following were the included standards: (1) histopathological diagnosis of PTCL first; (2) entire clinical record availability. Patients with incomplete laboratory test data and those who lost contact and could not be followed up were excluded.
2.2 Data collection
The data we collected from medical records were listed as follows: age, gender, Ann Arbor stage, Eastern Cooperative Oncology Group (ECOG), B symptoms, IPI score, PIT score, pathological types, amount of extranodal involvement sites, BM involvement, LDH, platelet (PLT) and hemoglobin (Hb). The LLR is obtained by dividing leukocyte by lymphocyte. The NLR is calculated by dividing neutrophils by lymphocytes. Leukocyte, lymphocyte, neutrophils, LDH, Hb, and platelet count are all from blood samples collected immediately before the first treatment. Follow-up was carried out through phone calls or the check of medical records. OS was calculated as the period from preliminary diagnosis to the day of the last follow-up or death from whatever the cause is. Patients who survived were checked at their last follow-up date.
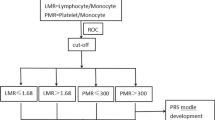
2.3 Statistical analysis
The categorical variables were recorded in the form of quantities and percentages (n, %). The optimum cut-off value of LLR related to the survival state of patients was established by the receiver operating characteristic (ROC) curve. For NLR, the 75th quantile of 8.25 was identified as the most optimum cut-off value for survival by the log-rank test. The χ2 test was applied to contrast baseline characteristics between patients in different groups divided according to the cut-off value of LLR or NLR. The Kaplan-Meier method was adapted to develop the survival curve. The log-rank test was performed to contrast the survival distributions. The Cox proportional model was applied to recognize which indicators were related to OS. Data processing and analysis were conducted using the statistical software package SPSS 26.0. The two-sided P < 0.05 was generally supposed to be statistically significant.
3 Results
3.1 Patient cohorts and characteristics
Our study involved 108 PTCL patients in total, among whom the median age of preliminary diagnosis was 57.5 years (range, 7–82 years) and the male-to-female ratio is about 2.3:1. Based on the WHO classification criteria, the distribution of pathological types in all patients was listed as follows: PTCL, NOS, 13 (12.04%); angioimmunoblastic T cell lymphoma (AITL), 68 (62.96%); anaplastic large cell kinase-negative anaplastic large cell lymphoma (ALK-ALCL), 14 (12.96%) and anaplastic large cell kinase-positive anaplastic large cell lymphoma (ALK + ALCL), 13 (12.04%). Among the enrolled patients, 31 (28.70%) were in stage I-II and 77 (71.30%) were in stage III-IV; 12 (11.11%) were identified with ECOG ≥ 2 and 62 (57.41%) patients showed B symptoms. The distribution of patients in relation to the IPI were: low risk, 31 (28.704%); low-intermediate risk, 42 (38.889%); high-intermediate risk, 26 (24.074%) and high risk, 9 (8.333%). According to PIT, the following groups of patients were established: group 1, 31 (28.70%); group 2, 24 (22.22%); group 3, 35 (32.41%) and group 4, 18 (16.67%). Of the 108 patients, 17 (15.74%) patients had a number of extranodal lesions > 1 site; 10 (9.26%) had bone marrow involved; 52 (48.15%) were with LDH level increased, while 21 (19.44%) with PLT decreased, 30 (27.78%) with hemoglobin decreased. LLR ≥ 10.30 was detected in 30 (27.78%) patients, and NLR ≥ 8.25 was recorded in 27 (25.00%) patients. The follow-up time ranged from 0.3 to 181.1 months, with a median of 16.63 months. There were 83(76.9%) patients receiving chemotherapy with cyclophosphamide, doxorubicin, vincristine and Prednisone (CHOP) or CHOP like regimen, 14 patients receiving chemotherapy regimen other than CHOP, and 5 patients receiving surgical treatment only as first-line treatment. Six people did not receive treatment. 11 of the patients received consolidation radiotherapy. The clinical characteristics of the patients are shown in Table 1.
3.2 Characteristics of patients by different levels of LLR and NLR
Patients were classified into two groups based on the cut-off value of LLR: 78 patients had LLR < 10.30, and 30 patients had LLR ≥ 10.30. There was a significant distinction between the individuals with LLR < 10.30 and those with LLR ≥ 10.30 concerning Age (P = 0.037), Ann Arbor stage (P = 0.029), B symptom (P = 0.012), IPI (P = 0.004), PIT (P = 0.023), LDH (P = 0.017) and NLR (P < 0.001), as listed in Table 2. Patients were classified into two groups based on the cut-off value of NLR: 81 patients had NLR < 8.25, and 27 patients had NLR ≥ 8.25. There was a notable distinction between the patients with NLR < 8.25 and those with NLR ≥ 8.25 concerning Ann Arbor stage (P = 0.020), B symptom (P = 0.043), IPI (P = 0.013), PIT (P = 0.035), histology (P = 0.017), LDH (P = 0.026) and LLR (P < 0.001). The clinical data were recorded in Table 3.
3.3 The Cox proportional hazard regression analysis for OS
Univariate Cox proportional hazards analysis identified LLR ≥ 10.30 (P = 0.002), NLR ≥ 8.25 (P = 0.036), ECOG ≥ 2 (P = 0.003), IPI > 2 (P = 0.005), PIT ≥ 2 (P = 0.006), B symptom (P = 0.025), Ann Arbor stage III-IV (P = 0.021) and Elevated LDH (P = 0.007) as significant prognostic indicators with inferior OS (Table 4). Then we built up a multivariate model with variables significantly related to prognosis. It was worth noting that we analyzed the IPI score and its elements respectively to avoid duplication. In addition, according to the results of univariate analysis, we chose IPI to be the prognostic tool due to its higher correlation with survival than PIT. Multivariate cox proportional hazards analysis revealed that only LLR ≥ 10.30 was significantly related to an inferior OS with a hazard ratio (HR) of 2.500 (95% CI 1.064–5.873; P = 0.036). Combined with univariate and multivariate analysis, LLR was a self-dependent prognostic index of PTCL.
3.4 Survival and LLR
In this investigation, recurrence occurred in 49 patients and 79 patients pass away from diverse causes. The median OS of the population was 20.567 months (95%CI 13.295–27.839 months). The most discriminative cut-off value for the LLR based on the ROC analysis was 10.30 (sensitivity 32.90% and specificity 86.20%) and the area under curve(AUC) was 0.555(95% CI 0.435–0.675) (Fig. 1). Patients who had an LLR < 10.30 presented a considerably longer survival time than those with LLR ≥ 10.30, with the median OS being 26.4 months (95%CI 18.631–34.169) vs. 8 months (95% CI 1.004–14.996), respectively (P = 0.002; Fig. 2).
3.5 Survival and NLR
According to the quartile of NLR, patients were divided into four groups. Figure 3 showed the survival curves of these four groups, which indicated that the highest quartile subgroup had the worst survival compared with the other quartiles. We then divided these patients into two groups (higher vs. lower) based on the 75th quantile with the cut-off point of 8.25. The survival curves of these two groups are shown in Fig. 4. Patients with lower NLR had longer OS than those with higher NLR, with the median survival being 24.833 (95%CI: 18.502–31.164) vs. 12.967 (95%CI: 0.260-25.674) months (P = 0.034).
3.6 Survival by IPI and LLR
The IPI showed substantial prognostic prediction capability in this cohort of PTCL patients as well. Patients were divided into two groups according to IPI score: the group with a score of 0–2 and the group with a score of 3–4. The lower score group had significantly longer OS than the higher group, with the median survival being 25.23 (95% CI 19.23–31.23) vs. 10.80 (95% CI 8.81–12.79) months (P = 0.005; Fig. 5). Furthermore, we categorize patients into four groups by combining these two independent prognostic indicators, IPI and LLR. As a result, patients with IPI score 0–2 and LLR ≥ 10.30 exhibited a close OS to those with IPI 3–4 and LLR < 10.30, showing an intermediate survival between patients with IPI score 0–2 as well as an LLR < 10.30 and patients with IPI score 3–4 and an LLR ≥ 10.30 (Fig. 6).
3.7 Survival and first-line treatment
The patients were divided into four groups according to their first-line treatment. There were significant differences in survival among groups (P = 0.035). The median OS of the CHOP/CHOP-like regimen group was 25.2 months (95% CI 19.370-31.096), the longest of the four groups, followed by the group of patients who used a regimen other than CHOP, which had a median OS of 16.3 months. The median OS was shorter in the surgical treatment only group and the group without treatment (Fig. 7). In addition, we also perform the subgroup analysis stratified by treatment regimens on NLR and LLR. Among who using the CHOP/CHOP like regimen, patients with lower LLR had longer OS than those with higher LLR (p = 0.008, Fig. 8) and patients who had an NLR < 8.25 presented a considerably longer survival time than those with NLR ≥ 8.25 (p = 0.038, Fig. 9). Consequently, although patients adopt the same chemotherapy regimen, these two indicators still have predictive efficacy in predicting prognosis.
4 Discussion
PTCL is a rare but highly invasive NHL and CHOP regimen, CHOPE regimen (cyclophosphamide, doxorubicin, vincristine, prednisone and etoposide) and DA-EPOCH regimen (dose adjusted etoposide, prednisone, vincristine, cyclophosphamide and doxorubicin) are usually used as the first-line treatment of PTCL at present. However, some of patients have a poor response to conventional chemotherapy, which means the requirements for further treatment have not been met. With the finding of various prognostic indicators, remarkable progress has been achieved in the prognosis prediction of patients with PTCL in the past few decades. Even though some prognostic models such as IPI, and PIT have been generally used to guide the treatment of PTCL in the clinic, neither of them takes an index derived from the complete blood count. Recently, many scholars have studied the prognostic significance of lymphocyte monocyte ratio [12], thrombocytopenia [13], and the derived neutrophil-lymphocyte ratio [14] in PTCL. This is a study to investigate the prognostic capability of LLR in a cohort of PTCL patients for the first time. Since the data of leukocytes, lymphocytes, and neutrophils can be easily obtained in clinical treatment as the components of CBC, we confirm that LLR and NLR have the potential to supplement the existing prognostic system. While LLR and NLR are significantly correlated to the inferior OS in the univariate analysis, only LLR is an independent predictor of OS. In our analysis, the group with LLR < 10.30 exhibited a longer OS time than the group with LLR ≥ 10.30. In addition, our study found that when holding the same IPI score, patients with LLR ≥ 10.30 still presented poorer survival than those with LLR < 10.30.
It is reported that cancer-related systemic inflammation, on the one hand, promotes cancer cell survival and hyperplasia, vascular regeneration, tumor invasion, and progression [15], repressed host immunologic function, on the other hand, resulting in an antitumor efficacy [16]. Previous reports had revealed that the close relationship between inflammation and malignancy was established by leukocytes in the tumor microenvironment [17]. Decreased lymphocytes might indicate a weakened specialized antitumor immune function. Lymphopenia was reported to be related to inferior survival in solid tumors and hematologic malignancies such as Hodgkin lymphoma, advanced carcinomas, sarcomas, acute myeloblastic leukemia (AML), acute lymphoblastic leukemia (ALL), and diffuse large B cell lymphoma (DLBCL) [18,19,20,21,22,23,24]. Currently, only Paydas et al. investigated the prognostic significance of LLR in classical Hodgkin lymphoma [7]. Although it has been demonstrated that LLR is prognostic valuable for Hodgkin’s lymphoma, up to now, no one has studied its value in PTCL. By analyzing the clinical data of 108 cases with PTCL, our study confirmed that LLR can predict the prognosis of individuals with PTCL independently, and cases with LLR ≥ 10.30 presented worse OS than those with LLR less than 10.30. Lately, POD24 (progression of disease within 24 months) has been reported to be a powerful prognostic factor within multiple categories of lymphoma, involving extranodal NK/T-cell lymphoma, nasal type [25], follicular lymphoma [26, 27], and marginal zone lymphomas(MZLs) [28]. Suzuki et al. reported their investigation that POD24 was associated with the survival of PTCL patients, and the no POD24 group has a longer OS than the group that reached POD24 [29]. Surprisingly, we found that 80% of patients with LLR ≥ 10.30 reached POD24 in our study. Combined with our finding that patients with LLR ≥ 10.30 have worse OS than those with LLR < 10.30, we consider that LLR can predict the occurrence of POD24 to some extent, so as to prompt the prognosis in the early stage of the disease.
Immunocytes promote tumor advancement by various mechanisms like releasing factors that can benefit survival, stimulating vascularization, accelerating DNA injury, and assisting immune escape [30]. Cancer-related inflammation and host immune function, which are two independent but related procedures, take a remarkable part in cancer progression and deciding patients’ prognosis [6]. NLR might reflect both of them. The prognostic value of NLR has been studied intensively in DLBCL and a variety of solid tumors like Gastroesophageal carcinoma, Hepatocellular carcinoma, breast cancer, and Non-small cell lung cancer [8,9,10, 31]. However, the investigation of NLR is relatively rare in PTCL. As for whether NLR is an independent prognostic index in PTCL, different studies have different conclusions. Some investigations revealed that NLR showed significance in both univariate and multivariate analysis, while some studies only find it in univariate analysis [32,33,34]. Our study only revealed it to be significant in predicting OS within univariable analysis, which contradicts the conclusion of the research in PTCL, NOS [11]. We considered that it is probably due to the distinction in the ratio of pathological subtypes among included cases. Even so, NLR retained its prognostic value in PTCL. We found that in the group of patients who applied the CHOP/CHOP like regimen, patients with NLR ≥ 8.25 had a worse prognosis than those with NLR < 8.25. More analysis of datasets from diverse regions is required to determine if LLR and NLR can be applied to direct the treatment of PTCL.
5 Conclusion
Our study showed that LLR ≥ 10.30 and NLR ≥ 8.25 were significantly associated with inferior OS within univariable analysis, while in multivariable analysis, only LLR showed significance, and NLR lost its predictive value. Consequently, LLR was proved to be an independent prognostic factor of PTCL. Furthermore, our analysis indicated that even when two groups had the same IPI score or adopt the same chemotherapy remigen, patients with LLR ≥ 10.30 exhibited a worse survival than those with LLR < 10.30. The LLR and NLR are cheap indexes and are easily available in clinics. Therefore, we supported their potential to be powerful complements to the existing prognostic tools of PTCL. Prospective studies in larger cohorts are required to verify their prognostic value.
Availability of data and materials
The datasets generated during and analysed during the current study are not publicly available due to privacy but are available from the corresponding author on reasonable request.
Abbreviations
- PTCL:
-
Peripheral T cell lymphoma
- NHL:
-
Non-Hodgkin’s lymphomas
- IPI:
-
International prognostic index
- PS:
-
Performance status
- LDH:
-
Lactic dehydrogenase
- PIT:
-
Prognostic index for T cell lymphoma
- BM:
-
Bone marrow
- PTCL, NOS:
-
Peripheral T cell lymphoma, not-otherwise-specified
- OS:
-
Overall survival
- LLR:
-
Leukocyte-lymphocyte ratio
- PNI:
-
Prognostic nutritional index
- CBC:
-
Complete blood count
- NLR:
-
Neutrophil-lymphocyte ratio
- ECOG:
-
Eastern cooperative oncology group
- PLT:
-
Platelet
- Hb:
-
Hemoglobin
- ROC:
-
Receiver operating characteristic
- AITL:
-
Angioimmunoblastic T cell lymphoma
- ALK(–)ALCL:
-
Anaplastic large cell kinase-negative anaplastic large cell lymphoma
- ALK(+)ALCL:
-
Anaplastic large cell kinase-positive anaplastic large cell lymphoma
- CHOP:
-
Cyclophosphamide,doxorubicin,vincristine and prednisone
- HR:
-
Hazard ratio
- AUC:
-
Area under curve
- CHOPE:
-
Cyclophosphamide,doxorubicin,vincristine,prednisone and etoposide
- DA-EPOCH:
-
Dose adjusted etoposide,prednisone,vincristine,cyclophosphamide and doxorubicin
- AML:
-
Acute myeloblastic leukemia
- ALL:
-
Acute lymphoblastic leukemia
- DLBCL:
-
Diffuse large B cell lymphoma
- POD24:
-
Progression of disease within 24 months
- MZLs:
-
Marginal zone lymphomas
References
Shi Y. Current status and progress of lymphoma management in China. Int J Hematol. 2018;107(4):405–12. https://doi.org/10.1007/s12185-018-2404-8.
A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin’s lymphoma. The non-hodgkin’s lymphoma classification project. Blood. 1997;89(11):3909–18. https://doi.org/10.1182/blood.V89.11.3909.
International Non-Hodgkin’s Lymphoma Prognostic Factors Project. A predictive model for aggressive non-hodgkin’s lymphoma. N Engl J Med. 1993;329(14):987–94. https://doi.org/10.1056/NEJM199309303291402.
Gallamini A, Stelitano C, Calvi R, Bellei M, Mattei D, Vitolo U, Morabito F, Martelli M, Brusamolino E, Iannitto E, et al. Peripheral T-cell lymphoma unspecified (PTCL-U): a new prognostic model from a retrospective multicentric clinical study. Blood. 2004;103(7):2474–9. https://doi.org/10.1182/blood-2003-09-3080.
Gutierrez-Garcia G, Garcia-Herrera A, Cardesa T, Martinez A, Villamor N, Ghita G, Martinez-Trillos A, Colomo L, Setoain X, Rodriguez S, et al. Comparison of four prognostic scores in peripheral T-cell lymphoma. Ann Oncol. 2011;22(2):397–404. https://doi.org/10.1093/annonc/mdq359.
Germano G, Allavena P, Mantovani A. Cytokines as a key component of cancer-related inflammation. Cytokine. 2008;43(3):374–9. https://doi.org/10.1016/j.cyto.2008.07.014.
Paydas S, Lacin S, Dogan M, Barista I, Yildiz B, Seydaoglu G, Karadurmus N, Civriz S, Kaplan MA, Yagci M, et al. Easier and more explanatory indices by integrating leukocyte lymphocyte ratio (LLR) and prognostic nutritional index (PNI) to IPS systems in cases with classical Hodgkin Lymphoma. Leuk Res. 2021;107:106586. https://doi.org/10.1016/j.leukres.2021.106586.
Porrata LFRK, Habermann T, Inwards DJ, Micallef IN, Markovic SN. Predicting survival for diffuse large B-cell lymphoma patients using baseline neutrophil/lymphocyte ratio. Am J Hematol. 2010;85(11):896–9. https://doi.org/10.1002/ajh.21849.
Keam B, Ha H, Kim TM, Jeon YK, Lee SH, Kim DW, Kim CW, Heo DS. Neutrophil to lymphocyte ratio improves prognostic prediction of International Prognostic Index for patients with diffuse large B-cell lymphoma treated with rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone. Leuk Lymphoma. 2015;56(7):2032–8. https://doi.org/10.3109/10428194.2014.982642.
Templeton AJ, McNamara MG, Seruga B, Vera-Badillo FE, Aneja P, Ocana A, Leibowitz-Amit R, Sonpavde G, Knox JJ, Tran B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6): dju124. https://doi.org/10.1093/jnci/dju124.
Beltran BEAC, Quiñones P, Morales D, Chavez JC, Sotomayor EM, Castillo JJ. The neutrophil-to-lymphocyte ratio is an Independent prognostic factor in patients with peripheral T-cell lymphoma, unspecified. Leuk Lymphoma. 2016;57(1):58–62. https://doi.org/10.3109/10428194.2015.1045897.
Zhang YSY, Shen H, Shou L, Fang Q, Zheng X, Zhu M, Huang X, Huang J, Li L, et al. The value of a new prognostic model developed by lymphocyte-monocyte ratio and platelet-monocyte ratio in peripheral T-cell lymphoma. Cancer Cell Int. 2021;21(1):29. https://doi.org/10.1186/s12935-021-02275-2.
Choi M, Lee JO, Jung J, Lee JY, Lee E, Lee H, Bang SM, Eom HS, Lee JS. Prognostic value of platelet count in patients with peripheral T cell lymphoma. Acta Haematol. 2019;141(3):176–86. https://doi.org/10.1159/000495337.
Hong HFX, Huang H, Wang Z, Lin T, Yao H. The derived neutrophil-to-lymphocyte ratio is an independent prognostic factor in patients with angioimmunoblastic T-cell lymphoma. Br J Haematol. 2020;189(5):908–12. https://doi.org/10.1111/bjh.16447.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–7. https://doi.org/10.1038/nature01322.
Porta C, Larghi P, Rimoldi M, Totaro MG, Allavena P, Mantovani A, Sica A. Cellular and molecular pathways linking inflammation and cancer. Immunobiology. 2009;214(9–10):761-10 77. https://doi.org/10.1016/j.imbio.2009.06.014.
Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357(9255):539–45. https://doi.org/10.1016/S0140-6736(00)04046-0.
Ayoub JP, Palmer JL, Huh Y, Cabanillas F, Younes A. Therapeutic and prognostic implications of peripheral blood lymphopenia in patients with Hodgkin’s disease. Leuk Lymphoma. 1999;34(5–6):519–27. https://doi.org/10.3109/10428199909058479.
De Angulo G, Palla YC, Anderson SL, Zweidler-McKay PM. Absolute lymphocyte count is a novel prognostic indicator in ALL and AML: implications for risk stratification and future studies. Cancer. 2008;112(2):407–15. https://doi.org/10.1002/cncr.23168.
Ege HGM, Markovic SN, Lacy MQ, Dispenzieri A, Hayman SR, Kumar SK, Porrata LF. Prediction of survival using absolute lymphocyte count for newly diagnosed patients with multiple myeloma: a retrospective study. Br J Haematol. 2008;141(6):792–8. https://doi.org/10.1111/j.1365-2141.2008.07123.x.
Kim DH, Baek JH, Chae YS, Kim YK, Kim HJ, Park YH, Song HS, Chung JS, Hyun MS, Sohn SK. Absolute lymphocyte counts predicts response to chemotherapy and survival in diffuse large B-cell lymphoma. Leukemia. 2007;21(10):2227–30. https://doi.org/10.1038/sj.leu.2404780.
Oki YYK, Kato H, Kuwatsuka Y, Taji H, Kagami Y, Morishima Y. Low absolute lymphocyte count is a poor prognostic marker in patients with diffuse large B-cell Lymphoma and suggests patients’ survival benefit from rituximab. Eur J Haematol. 2008;81(6):448–53. https://doi.org/10.1111/j.1600-0609.2008.01129.x.
Ray-Coquard I, Van Glabbeke CC, Sebban M, Le Cesne C, Judson A, Tredan I, Verweij O, Biron J, Labidi P. Lymphopenia as a prognostic factor for overall survival in advanced carcinomas, sarcomas, and Lymphomas. Cancer Res. 2009;69(13):5383–91. https://doi.org/10.1158/0008-5472.CAN-08-3845.
Song MK, Chung JS, Seol YM, Kim SG, Shin HJ, Choi YJ, Cho GJ, Shin DH. Influence of low absolute lymphocyte count of patients with nongerminal center type diffuse large B-cell lymphoma with R-CHOP therapy. Ann Oncol. 2010;21(1):140–4. https://doi.org/10.1093/annonc/mdp505.
Yamaguchi M, Suzuki R, Kim SJ, Ko YH, Oguchi M, Asano N, Miyazaki K, Terui Y, Kubota N, Maeda T, et al. Early disease progression in patients with localized natural killer/T-cell lymphoma treated with concurrent chemoradiotherapy. Cancer Sci. 2018;109(6):2056–62. https://doi.org/10.1111/cas.13597.
Yoon SECJ, Kim WS, Kim SJ. Impact of transformation on the survival of patients diagnosed with follicular lymphoma that progressed within 24 months. J Cancer. 2021;12(9):2488–97. https://doi.org/10.7150/jca.54434.
Sortais CLA, Tessoulin B, Gastinne T, Mahé B, Dubruille V, Blin N, Touzeau C, Moreau A, Bossard C, et al. Progression of Disease within 2 years (POD24) is a clinically relevant endpoint to identify high-risk follicular lymphoma patients in real life. Ann Hematol. 2020;99(7):1595–604. https://doi.org/10.1007/s00277-020-04025-2.
Luminari SMM, Rattotti S, Tarantino V, Marcheselli L, Cavallo F, Varettoni M, Bianchi B, Merli F, Tedeschi A, et al. Early progression as a predictor of survival in marginal zone Lymphomas: an analysis from the FIL-NF10 study. Blood. 2019;134(10):798–801. https://doi.org/10.1182/blood.2019001088.
Suzuki Y, Yano T, Suehiro Y, Iwasaki H, Hidaka M, Otsuka M, Sunami K, Ikeda H, Sawamura M, Ito T, et al. Evaluation of prognosis following early disease progression in peripheral T-cell lymphoma. Int J Hematol. 2020;112(6):817–24. https://doi.org/10.1007/s12185-020-02987-7.
de Visser KE, Eichten A, Coussens LM. Paradoxical roles of the immune system during cancer development. Nat Rev Cancer. 2006;6(1):24–37. https://doi.org/10.1038/nrc1782.
Chen T, Song C, Liang GF, Xu XY, Wang C, Zhang ZC, Tang MQ. Neutrophil-to-lymphocyte ratio, Platelet-to-Lymphocyte Ratio, and their variations as a basis for a prediction model in advanced NSCLC patients receiving Anlotinib. Dis Markers. 2022;2022:5879137.https://doi.org/10.1155/2022/5879137.
Marcheselli RBA, Tadmor T, Marcheselli L, Cox MC, Pozzi S, Ferrari A, Baldini L, Gobbi P, Aviv A, et al. Neutrophil-lymphocyte ratio at diagnosis is an Independent prognostic factor in patients with nodular sclerosis Hodgkin lymphoma: results of a large multicenter study involving 990 patients. Hematol Oncol. 2017;35(4):561–6. https://doi.org/10.1002/hon.2359.
Reddy JP, Hernandez M, Gunther JR, Dabaja BS, Martin GV, Jiang W, Akhtari M, Allen PK, Atkinson BJ, Smith GL, et al. Pre-treatment neutrophil/lymphocyte ratio and platelet/lymphocyte ratio are prognostic of progression in early stage classical Hodgkin lymphoma. Br J Haematol. 2018;180(4):545–9. https://doi.org/10.1111/bjh.15054.
Beltran BECD, De La Cruz-Vargas JA, C otrina E, Gallo A, Sotomayor EM, Castillo JJ. The neutrophil-lymphocyte ratio is prognostic in patients with early stage aggressive peripheral T cell lymphoma. Br J Haematol. 2019;184(4):650–3. https://doi.org/10.1111/bjh.15141.
Acknowledgements
We would like to thank Dr. Yu-Peng Liu for his technical support; This work was supported by BEIJING MEDICAL AWARD FOUNDATION (grant number YXJL-2020-0785-1072) and Harbin Medical University Cancer Hospital HAIYAN SCIENTIFIC RESEARCH FUND (grant number JJZD 2022-10).
Funding
This study was funded by BEIJING MEDICAL AWARD FOUNDATION (grant number YXJL-2020-0785-1072) and Harbin Medical University Cancer Hospital HAIYAN SCIENTIFIC RESEARCH FUND, (grant number JJZD 2022-10).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Shi-Qi Gao, Yue Xu, Bo-Ya Lei, Zi-Jian Zhang, Shu Zhao, **ng-Jian Niu, Wen-Hui Zhao and Qing-Yuan Zhang. The first draft of the manuscript was written by Shi-Qi Gao and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Bioethics Committee of the Harbin Medical University Cancer Hospital approved this study.
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gao, SQ., Lei, BY., Xu, Y. et al. Identification of leukocyte-lymphocyte ratio as a novel prognostic factor in Peripheral T-cell lymphoma. Holist Integ Oncol 2, 40 (2023). https://doi.org/10.1007/s44178-023-00062-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44178-023-00062-9