Abstract
The novel coronavirus disease 2019 (COVID-19) pandemic underscores the importance of place of residence as a determinant of health. Prior work has primarily examined the relationship between neighbourhoods’ sociodemographic traits and COVID-19 infection rates. Using data from the City of Toronto, Canada, we assess how the built environments of neighbourhoods, in conjunction with their sociodemographic profiles, shape the pattern of spread of COVID-19 in low-, middle-, and high-income neighbourhoods. Our results show that COVID-19 spread faster in neighbourhoods with a higher share of overcrowded households, large commercial areas, and poor walkability. The extent to which neighbourhood walkability is associated with a slower increase in COVID-19 infections varied by neighbourhood income level, with a stronger negative association in low-income neighbourhoods. Net of the share of overcrowded households, population density is associated with a faster increase in COVID-19 infections in low-income neighbourhoods, but slower increase in high-income neighbourhoods. More green space is associated with a slower increase in COVID-19 infections in low-income, but not higher-income, neighbourhoods. Overall, our findings suggest that post-pandemic urban planning efforts cannot adopt a one-size-fits-all policy when reconstructing neighbourhoods in ways that promote health and reduce their vulnerability to infectious diseases. Instead, they should tailor the rebuilding process in ways that address the diverse needs of residents in low-, middle-, and high-income neighbourhoods.
Parmi les déterminants de la santé, la récente pandémie de coronavirus (COVID-19) a souligné l’importance du lieu de résidence. Les travaux de recherche antérieurs se sont essentiellement attachés à étudier le lien entre les caractéristiques démographiques des quartiers et les taux d’infection à la COVID-19. En nous appuyant sur les données de la ville de Toronto au Canada, nous avons évalué la façon dont l’environnement bâti des quartiers, de pair avec leurs profils sociodémographiques, pouvait façonner les schémas de propagation de la COVID-19 dans les secteurs à faibles revenus, à revenus moyens et à revenus élevés. Nos résultats montrent que la COVID-19 se propage plus rapidement dans les quartiers à forte proportion de logements surpeuplés, où les grandes zones commerciales sont plus nombreuses et où les potentiels piétonniers sont moindres. Le degré de corrélation entre le potentiel piétonnier et la progression plus lente des cas de contamination à la COVID-19 dépend du niveau de revenu d’un quartier, et cette corrélation s’avère plus fortement négative dès lors que les revenus y sont faibles. Déduction faite de la proportion de logements surpeuplés, la densité de population est corrélée à une progression plus forte des cas de contamination à la COVID-19 dans les secteurs à faibles revenus, et à une propagation plus lente au sein des quartiers à revenus élevés. Dans les secteurs à faibles revenus, la présence d’espaces verts en plus grand nombre est corrélée à une progression plus lente des cas de contamination à la COVID-19, ce qui n’est pas le cas dans les quartiers à revenus élevés. Dans l’ensemble, nos résultats montrent que pour reconstruire les quartiers de manière à promouvoir la santé et réduire la vulnérabilité aux maladies infectieuses, les efforts de planification urbaine postpandémie ne pourront adopter une approche uniformisée. Au contraire, les processus de reconstruction devront être adaptés pour répondre aux différents besoins des résidents de tous les quartiers, quels que soient leurs niveaux de revenus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Health inequalities by place are profound and enduring. Morbidity and mortality patterns vary systematically by neighbourhood socioeconomic status (SES) (Alvarado, 2019; Bosma et al., 2001; Oakes et al., 2015; Sampson, 2003). Even after controlling for individual characteristics, living in socioeconomically disadvantaged neighbourhoods is associated with higher rates of age-specific mortality, communicable diseases, cardiovascular disease, obesity, mental health problems, and poorer self-rated health (Boylan & Robert, 2017; Browning & Cagney, 2003; O’Campo et al., 2015; Phelan et al., 2010) .
The novel coronavirus disease 2019 (COVID-19) pandemic further highlights the importance of one’s neighbourhood as a determinant of their health. Low-income neighbourhoods with high shares of racial minority and foreign-born residents have had disproportionately high COVID-19 infection and fatality rates (Choi et al., 2021a, 2021b; Mein, 2020; Patel et al., 2020; Rollston & Galea, 2020). Furthermore, many public health measures designed to curb the spread of the virus depend on the availability and usage of neighbourhoods’ built environments.Footnote 1 Low-income communities may have borne the brunt of the COVID-19 pandemic in part because they lack the physical infrastructure and amenities that promote residents’ health and facilitate residents’ ability to adhere to public health guidelines.
Several studies have applied the place perspective and documented the uneven spatial and demographic distribution of COVID-19 infections and deaths. This research primarily describes the distribution of COVID-19 across relatively large and socially heterogeneous administrative areas such as counties in the USA (Abedi et al., 2020; Finch & Hernández Finch, 2020) or health regions in Canada (Denice et al., 2020). Such analyses belie the substantial spatial variation at more localized scales (e.g., neighbourhoods) in how individuals identify with a sense of place, individuals’ exposure to infectious diseases, and the pace at which diseases like COVID-19 spread (Riley, 2007; Thomas et al., 2020; Wang et al., 2018). The reliance of existing work on census and survey data has also meant a focus on the sociodemographic correlates of infection (Borjas, 2020; Denice et al., 2020). To our knowledge, few studies have so far examined how the built environments of neighbourhoods have contributed to the disparities in COVID-19 infection trajectories by neighbourhood socioeconomic status (for an exception, see Oishi et al., 2021). This gap exists even though the built environment of a neighbourhood can shape its residents’ ability to follow public health guidelines and the amenities on which they can draw to avoid infection or once they or others in their social circles become infected (Frumkin, 2021; Lai et al., 2020; Sarkar & Weber, 2017). Finally, the few studies that address this issue have not examined whether the relationship between built environments and COVID-19 infection trajectories varies according to neighbourhood socioeconomic status. This is an important oversight since residents of lower-income neighbourhoods may depend differently, and perhaps more, on community resources because they have fewer personal resources at their disposal.
In this article, we examine the relationship between neighbourhoods’ social contexts—that is, their built environments and sociodemographic composition—and the spread of COVID-19 across the 140 neighbourhoods in the City of Toronto, Ontario, Canada. Using two-level growth curve models, we first examine how the built environments and sociodemographic traits of neighbourhoods shape the COVID-19 infection trajectories over time. Then, we assess whether the association between neighbourhood social contexts and the COVID-19 infection trajectories varies across low-, middle-, and high-income neighbourhoods.
The City of Toronto is a useful context for our study of the spread of COVID-19 for several reasons. First, City of Toronto is frequently described as the “city of neighbourhoods.” The City of Toronto delineates 140 neighbourhoods with recognizable physical boundaries like rivers, roads, and railroads. They are often used as planning areas for the municipal governments, actual neighbourhoods by its residents, and service areas for businesses (City of Toronto, 2014, 2015). These neighbourhoods are also distinctive in terms of the physical, economic, and social attributes (Hulchanski, 2006). Second, Toronto emerged as one of the epicentres of the pandemic in Canada. Third, the municipal government reported and made publicly available neighbourhood-specific COVID-19 infection rates. Finally, unlike other municipalities and provinces, the municipal government has also released rich administrative data on its 140 neighbourhoods, including their sociodemographic composition and several dimensions of their built environments.
This study makes several contributions to the literature on the neighbourhood context of health. First, our study captures neighbourhoods’ social contexts by examining both their sociodemographic composition and their built environments. This aligns with calls to examine the linkages between the built environment of neighbourhoods and the health outcomes of their residents (Sampson, 2003). Second, our study examines multiple dimensions of the built environments of neighbourhoods. Prior work tends to focus on a single dimension or amenity even though people’s health outcomes, including their vulnerability to COVID-19, is shaped by multiple facets of their neighbourhoods’ built environment (Anderson, 2017; Diez Roux & Mair, 2010; Marwell & Gullickson, 2013). Third, we examine the spread of COVID-19 infections across relatively small and socially meaningful geographic areas (i.e., neighbourhoods). Prior work on neighbourhood effects has been criticized due to its overreliance on large and arbitrary geographic units (Sampson, 2003). Finally, our study considers whether the relationship between neighbourhood social contexts and the spread of COVID-19 varies by neighbourhood income levels. Most prior work has identified the average contextual risk factors for COVID-19 for all geographic areas; however, the degree of reliance on community resources and the quality of those amenities may vary for residents of low-, middle-, and high-income neighbourhoods. This is especially important for our analyses given reports that neighbourhoods in Toronto have become increasingly polarized by and divided along income lines (Hulchanski, 2010). Taken together, these findings provide insights for ongoing discussions about how to transform urban spaces in ways that promote health.
2 Background
2.1 Neighbourhood Social Context as a Key Social Determinant of Health
One’s place of residence has implications for nearly every dimension of their personal and social lives (Massey, 1996; Sampson, 2003; Sharkey & Faber, 2014). Neighbourhoods influence one’s educational opportunities (Owens, 2010), social capital and networks (Leyden, 2003; Lochner et al., 2003), proximity to employment (Hellerstein et al., 2008; Kain, 1992), and exposure to crime (Browning & Jackson, 2013). They also shape our health (Sampson, 2003). Research has consistently shown that individual traits alone cannot fully explain health disparities (Robert, 1999; Sampson, 2003). Rather, neighbourhood social contexts affect individual health and contribute to health inequalities independent of individual traits (e.g., Brazil & Clark, 2017; Haan et al., 1987; Sheehan et al., 2017; Yang & South, 2020) .
Two interrelated explanations are used to explain place-based disparities in health. The compositional hypothesis focuses on the sociodemographic composition of neighbourhoods (see reviews by Diez Roux & Mair, 2010; Pickett & Pearl, 2001; Riva et al., 2007). Independent of personal socioeconomic characteristics, residents of socioeconomically disadvantaged neighbourhoods have poorer health than those of more affluent neighbourhoods due to the socioeconomically disadvantaged position of their neighbors and the resulting scarcity of communal resources and information (Ross & Mirowsky, 2008; Sampson, 2003; Wilson, 1987). Living in socioeconomically disadvantaged neighbourhoods is associated with poorer self-rated health, higher rates of cardiovascular disease, and a higher incidence of depressive symptoms (Boylan & Robert, 2017; Browning & Cagney, 2003; Hale et al., 2013).
The contextual explanation underscores the importance of neighbourhoods’ built environments for residents’ health (Browning & Cagney, 2003; Ellen et al., 2001; Fitzpatrick & LaGory, 2003; Hystad et al., 2014; Sampson, 2003; Spring, 2018). For example, neighbourhood walkability is associated with healthier behaviors, lower prevalence of obesity, and lower prevalence of COVID-19 infections and deaths (Creatore et al., 2016; King et al., 2011; Oishi et al., 2021; Sallis et al., 2009). Proximity to supermarkets with fresh produce is associated with healthier eating habits and lower levels of obesity (de Souza et al., 2018; Perrotta et al., 2012; Renalds et al., 2010; Villeneuve et al., 2012). The presence of green space contributes to reduced levels of perceived stress (Awuor & Melles, 2019; Hordyk et al., 2015). Conversely, living in a poorly maintained neighbourhood is related to higher rates of depression (Galea et al., 2005). Residents of low-income neighbourhoods may be unhealthier than residents of wealthier neighbourhoods because they have greater exposure to health deterrents and limited access to health-promoting facilities (Browning & Cagney, 2003).
These explanations are complementary because socioeconomically advantaged individuals tend to reside in neighbourhoods with better access to infrastructure and services that promote human development, gainful and secure employment, and health (Anderson, 2017; Doubeni et al., 2011; Kawachi & Berkman, 2003; Sampson, 2003; Tunstall, 2005). By contrast, the disadvantaged are segregated into areas with more undesirable and fewer health-promoting amenities (Luo et al., 2010; Massey & Denton, 1993; Wilson, 1987).
Empirical work on the link between neighbourhoods and residents’ health has focused on the neighbourhood composition argument in large part due to its reliance on census and survey data, which generally includes social, demographic, and economic indicators of local populations at the exclusion of the built environments of neighbourhoods (O’Campo et al., 2015; Ross & Mirowsky, 2008; Sampson, 2003). Furthermore, even when prior work examines the relationship between neighbourhoods’ built environments and residents’ health, they tend to either focus on a single dimension or rely on a composite index (Pearce et al., 2010). However, focusing on a single dimension is at odds with how residents’ health is shaped by multiple facets of their neighbourhoods’ built environment (Anderson, 2017; Diez Roux & Mair, 2010; Marwell & Gullickson, 2013). And while composite indices provide a more comprehensive picture of built environments overall, they are ill-suited for identifying the specific risk and protective factors that shape health outcomes. This study addresses calls for research to simultaneously consider the role of neighbourhoods’ sociodemographic profiles and multiple facets of their built environments in generating health outcomes and health inequalities.
2.2 The Role of Neighbourhoods in the COVID-19 Pandemic
COVID-19 infections and deaths are clustered in socioeconomically disadvantaged and predominantly minority communities (Abedi et al., 2020; Borjas, 2020; Cordes & Castro, 2020; Denice et al., 2020). To provide insights into policies aimed at curbing the spread of the virus, an emerging body of work has sought to identify the neighbourhood risk factors of COVID-19. These studies point to a number of environmental factors that could render residents of low-income neighbourhoods more vulnerable to infection and death.
Residents of lower-income neighbourhoods are more likely to work in occupations with greater exposure to the COVID-19 virus (Blundell et al., 2019). Low or poor airflow due to inadequate heating, air-conditioning, or ventilation systems may also mean ineffective indoor air circulation and greater difficulty for household members to adhere to stay-at-home policies.
Access to green spaces may be especially important for residents in densely populated urban areas. Researchers in Oslo, Norway, for example, found a nearly 300% increase in outdoor recreational activity in urban green spaces during the country’s first lockdown (March 12–31, 2020) relative to the same period during the prior three years (Venter et al., 2020). Such findings highlight the importance of access to green open spaces in urban settings for facilitating physical distancing and hel** mitigate the spread of COVID-19.
Researchers have underscored the need to design sustainable urban spaces that include built environments that promote health (e.g., Frumkin, 2021). Yet, researchers seldom examine how the built environments of neighbourhoods shape the spread of COVID-19. The few studies that do focus on a single dimension of the built environment of neighbourhoods (e.g., density or crowding, air pollution, green space), even though people’s risk of contracting a COVID-19 infection is shaped by multiple facets of their neighbourhoods’ built environments (Ali & Islam, 2020; Kamis et al., 2021; Venter et al., 2020).
2.3 Socioeconomic Variation in the Health Impacts of Neighbourhoods’ Built Environments
The extant literature suggests that neighbourhoods’ social contexts likely matter differently for residents of neighbourhoods with varying socioeconomic composition. Even if the same types of amenities are present, residents of low-income neighbourhoods may rely more or differently on these community resources because they have fewer individual resources at their own disposal. For instance, those in lower-income neighbourhoods may rely more heavily on public transportation because they are less likely to own cars. As such, accessibility of public transportation and the walkability of neighbourhoods may be more important for residents of lower-income neighbourhoods. Similarly, the existence of green space may be particularly important for the health of residents of lower-income neighbourhoods as they are more likely to reside in crowded households with limited space and inadequate air supply.
Furthermore, prior work has established that neighbourhood amenities in lower-income neighbourhoods are generally of lower quality than those in higher-income neighbourhoods (Algert et al., 2006; Thornton et al., 2016; Vaughan et al., 2013). Sidewalks in low-income neighbourhoods, for example, have poorer aesthetics due to graffiti and litter (Howell, 2019). As a result, residents of lower-income neighbourhoods gain fewer physical or mental health benefits from walking these poorly maintained sidewalks (Howell, 2019; Thornton et al., 2016).
To our knowledge, prior work has not examined whether the relationship between the built environments of neighbourhoods and the spread of COVID-19 varies by neighbourhood socioeconomic status. Such insights are crucial when reimagining urban spaces in ways that reduce the vulnerability of marginalized populations to infectious diseases. Considering health differentials by neighbourhood income levels will be particularly important in Toronto in view of the income polarization over the past few decades (Hulchanski, 2006).
2.4 Context: the City of Toronto During the COVID-19 Pandemic
Canada ranks near the middle among countries in terms of COVID-19 infection and death rates: it is 112th in terms of infection rates and 93rd in terms of death rates (CNN Health Dashboard, 2022). As in other high-income countries, urban centers in Canada were hit especially hard by the pandemic. The City of Toronto has emerged as an epicenter, trailing only the infection and death rates of Montreal in Canada. With a population of nearly 3 million, Toronto has traditionally served as a gateway for immigrants and has an ethnically and socioeconomically diverse population. In fact, researchers argue that there are three cities within the City of Toronto, defined by changes in neighbourhood income levels over time (Hulchanski, 2010). By late December 2021, there had been over 222,247 confirmed cases and 3,740 COVID-19-related deaths in the city, which many perceive to be undercounts. Toronto has faced five waves of the pandemic. Our focus in this article is on the initial two waves of the pandemic—from late January to late November 2020. Following this period, the pandemic’s trajectory and correlates shapeshifted as it dragged on, as vaccines became more readily available, and as outbreaks moved into the workplace (Institute for Work & Health, 2021). Our observation window thereby focuses our attention on a period characterized by community transmission (that is, within neighbourhoods) during the earlier stages of the pandemic and policymakers’ response to it.
Data availability is another feature that makes Toronto a useful case for our analysis. The City of Toronto offered daily reports of COVID-19 infection, hospitalization, and fatality counts for each of its 140 neighbourhoods (average population size: 20,000; each comprised of 2–5 census tracts). This is in contrast to most of Canada, which offers aggregate COVID-19 infection and death counts for health regions—large and heterogeneous geographic units responsible for addressing the health care needs of 415,000 people (Denice et al., 2020). Even in the USA, most COVID-19 data are available at a county level (Abedi et al., 2020; Finch & Hernández Finch, 2020; for exceptions, see Thomas et al., 2020; Oishi et al., 2021). When combined with rich data about neighbourhoods’ built environments and sociodemographic compositions, infection data at the neighbourhood level allow us to more directly test how neighbourhood contexts are associated with the spread of COVID-19.
3 Data and Methods
3.1 Data
Data were pooled from two sources: first, the City of Toronto’s Open Data Catalogue reports (a) the daily counts of confirmed COVID-19 cases reported to Toronto Public Health,Footnote 2 (b) the sociodemographic profile of neighbourhoods estimated by the City government using the 2016 Canadian Census, and (c) the built environments of each neighbourhood obtained from the City’s administrative records.Footnote 3 Second, this information is supplemented with data from Walk Score®, capturing neighbourhoods’ walkability and public transport accessibility level (www.walkscore.com).Footnote 4 Walk score rankings measure the ease with which people can reach neighbourhood amenities from a specific longitude/latitude coordinate, and transit score rankings similarly measure the ease with which people can get around via public transit from a particular location.
3.2 Measures
3.2.1 Dependent Variable
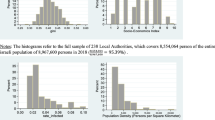
Our dependent variable measures the cumulative COVID-19 infection rate per 100,000 residents for each neighbourhood over time. To compute this rate, we divide the total number of confirmed COVID-19 cases reported for each neighbourhood at five specific time points between January 21 and November 24, 2020, by the number of residents in each neighbourhood, and multiply by 100,000. The five time points we consider correspond to the onset of the pandemic (March 10), the officially designated peak of the first wave (April 15), the partial reopening of the City’s economy (June 24), partial lockdown (October 10), and full reclosure of the City’s economy during second wave of the pandemic (November 24).Footnote 5 We exclude 1,652 (1.6%) COVID-19 cases without neighbourhood identifiers and 3,543 (3.3%) unconfirmed COVID-19 cases. Figure 2 in the Appendix illustrates the number of daily COVID-19 infections in Toronto across this period.
3.2.2 Independent variables
The built environments of neighbourhoods were assessed with six variables: their walkability, ease of access to public transit, population density, percentage of overcrowded private households (i.e., dwellings without enough bedrooms, given the number of household members), the percentage of land covered by open green space, and the percentage of the neighbourhood zoned by the municipal government as a commercial area. Commercial area functions as another measure of population density, to the extent that firms display a preference for locating near population centers, availability of workspaces in high-rise buildings, and access to crowded transit lines (Rosenthal et al., 2021)—all risk factors for the spread of contagious diseases like COVID-19. Walk Score® rankings measure the ease with which people can reach everyday amenities and range from 0 (nothing to walk to) to 100 (most daily errands can be fulfilled by walking). The Transit Score® is computed analogously, capturing an area’s accessibility via public transportation. Because walk and transit score rankings are measured for specific latitude/longitude points, we account for within-neighbourhood variation by computing the mean scores for 10 randomly sampled locations in each neighbourhood. This approach is similar to other studies that have used these measures, including a study that averages city-level walk score rankings to measure walkability at the county-level in the United States (Lima et al., 2021).
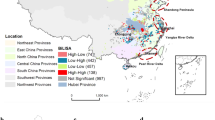
We capture neighbourhoods’ sociodemographic composition using neighbourhood income level (low, middle, and high), the percentage racial minority, the percentage foreign-born, the employment rate of residents between the ages of 25 and 64, the percentage of workers in frontline occupations (e.g., health, sales, manufacturing, and education), and the percentage aged 80 years and older. Neighbourhood income level is our measure of its socioeconomic status. Neighbourhoods are classified into three groups—low-, middle-, and high-income—depending on the share of residents whose after-tax income falls below Statistics Canada’s low-income cut-off (LICO). Low-income neighbourhoods are those in which the share of residents with incomes below the LICO falls in the top tercile (i.e., 19.1% or above). Middle-income neighbourhoods are those whose share of residents with incomes below the LICO falls in the middle tercile (i.e., greater than or equal to 13.8% and less than 19.1%). High-income neighbourhoods are those in which the share of residents with incomes below LICO falls in the bottom tercile (i.e., less than 13.8%). Figure A2 in the Appendix maps Toronto’s neighbourhoods by their income level. To account for differences in distribution of covariates, we standardize all continuous independent variables so that each variable has a mean of 0 and a standard deviation of one.
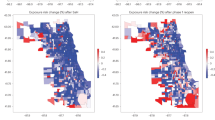
3.3 Spatial Autocorrelation
When spatial data are examined, researchers must take into account the potential effects of spatial autocorrelation (Anselin, 1988). We calculated a global measure of spatial autocorrelation (Moran’s I) for the cumulative number of COVID-19 infections for each of the five time periods: 0.03 in early March, 0.07 in mid-April, 0.50 in late June, 0.62 in early October, and 0.66 in late November of 2020.Footnote 6 While all but the first two values are statistically significant (p < 0.05), these values suggest initially low and then increasing levels of spatial autocorrelation. The increasing and higher values later in the pandemic (beginning in late June 2020) are not surprising and likely reflect the increasing ubiquity of COVID-19 infections across the city. Indeed, the trends in Fig. 1 highlight how all neighbourhoods saw their infection rates increase as the pandemic neared the one-year mark, despite persistent and growing gaps by socioeconomic status. Additionally, local indicators of spatial association (LISA; see Figure A3 in the Appendix) indicate a particular cluster of neighbourhoods with high numbers of COVID-19 infections in the northwestern part of the city (where there is also a cluster of lower-income neighbourhoods) throughout the pandemic, smaller clusters of neighbourhoods with lower COVID-19 counts in higher-income areas of the city, and fewer clusters elsewhere.
We control for the effects of spatial autocorrelation in our models by including spatially lagged cumulative COVID-19 infection rates. A spatially lagged infection rate represents the average level of infection in adjacent neighbourhoods. We calculate spatial lags for each neighbourhood and for each of our five time points. The inclusion of a spatial lag as a covariate accounts for the level of COVID-19 infections in surrounding neighbourhoods, which in effect captures the spatial interaction of the spread of COVID-19 across neighbourhoods. While the effects of COVID-19 in adjacent neighbourhoods on the level of COVID-19 in each neighbourhood are of substantive interest in and of themselves, the inclusion of spatially lagged infection variables is also statistically useful, as it increases the precision of our variables measuring neighbourhoods’ sociodemographic composition and built environments. Our approach follows prior work that examines, for instance, the growth of crime (Kikuchi & Desmond, 2010; Kubrin & Herting, 2003) as well as the spread of COVID-19 (Guliyev, 2020).
3.4 Models
We estimate two-level growth curve models to examine how neighbourhoods’ sociodemographic composition and built environments contribute to the spread of COVID-19 across the City of Toronto’s 140 neighbourhoods.Footnote 7 Growth curve models serve both conceptual and methodological purposes for our study. Conceptually, this approach allows us to focus on neighbourhood COVID-19 infection trajectories and to examine variation in these trajectories. This is especially useful for the spread of contagious diseases like COVID-19 that have affected areas and communities differently. Methodologically, growth curve models allow us to describe the full temporal sequence of the COVID-19 pandemic during our observation window—including both differences in infection rates at the beginning of the pandemic and the pace of spread across distinct time points during its first year (Curran et al., 2010)—instead of examining a single difference between two points in time or a set of differences between pairs of time points. In these ways, we think that growth-curve models enable a richer understanding of change in the spread of COVID-19 infections across Toronto’s neighbourhoods and help us determine the community characteristics associated with infection levels and changes in infections.
The level-1 equation in our study’s growth curve models describes the within-neighbourhood changes in cumulative infection counts (n) over time (t), and can be represented as follows:
Cumulative COVID-19 rates \({(y}_{nt})\) are characterized by a unique intercept (\({\alpha }_{n})\) and a time-dependent slope (\({\beta }_{nt})\). Time (t) is added as a series of four dichotomous variables for the days on which the cumulative COVID-19 infection rates were measured (April 15, June 24, October 10, and November 24; the referent is the first time point, March 10) to capture potential non-linearities in COVID-19 trajectories. The level-2 equation models the variation in cumulative COVID-19 infections among low-, middle-, and high-income neighbourhoods (i.e., between-neighbourhood effects). Formally, level-2 relationships can be represented as follows:
These equations indicate that the random intercepts (\({\alpha }_{n})\) and slopes \(({\beta }_{n})\) are a function of the covariates \({(x}_{nk})\) and error terms (\({u}_{nt}\), \({v}_{nt})\), respectively. We first estimate a growth curve model for a pooled sample of 140 neighbourhoods to identify overall contextual risk and protective factors for the spread of COVID-19. We then disaggregate by neighbourhood income level, and we estimate separate models for low-, middle-, and high-income neighbourhoods. The latter models allow us to determine whether the relationship between neighbourhood social contexts and the spread of COVID-19 varies by neighbourhood income.
Several other analytical decisions deserve mention. First, we considered other dimensions of neighbourhoods’ built environments and sociodemographic composition, but we could not include all of these due to multicollinearity issues (VIF > 10). We contend that the explanatory variables in our models capture a wide-ranging and robust set of neighbourhood characteristics. We estimated alternate models predicting spread of COVID-19 using other covariates; these results are available upon request.Footnote 8 Second, we chose to focus on the spread of the COVID-19 pandemic between January and November 2020. We chose this period because supplementary analyses revealed that the social determinants of COVID-19 in Toronto have changed over time. Starting in late November, Ontario saw more outbreaks in the workplace (Institute of Work & Health, 2021) and employment and occupational status played a larger role as a determinant of COVID-19.Footnote 9 Third, we are conducting our analyses using the census of neighbourhoods in the City of Toronto. Statistical tests are useful when making inferences about a population from sample data (Cowger, 1984; Treiman, 2009). Because we analyze population data, our interpretations do not rely on statistical significance (though we do report it in our tables). Instead, we interpret our findings based on the direction and size of the coefficients and their substantive importance.
4 Results
4.1 Descriptive Results
4.1.1 Built Environment and Sociodemographic Profiles of Neighbourhoods
Table 1 presents summary statistics of neighbourhoods’ built environments and sociodemographic profiles. Toronto is a generally walkable city with an accessible public transportation system. As is the case for most urban metropolises, it has high population density and relatively little green space. One-in-eight people reside in unsuitable and overcrowded housing. The city also has a diverse population. Just under half of the residents in Toronto are visible minorities and foreign-born. Nearly 50% of workers in Toronto are employed in frontline occupations.
The built environments and sociodemographic profiles vary by neighbourhood income level, which suggests that the ways in which these factors relate to the spread of COVID-19 across neighbourhoods may vary as well. Population density is highest in low-income neighbourhoods and lowest in high-income neighbourhoods. In a similar way, a higher share of housing is overcrowded in low-income neighbourhoods as compared to middle and high-income areas. Relative to other neighbourhoods, a higher share of middle-income neighbourhoods has been zoned as a commercial area: 5% of middle-income versus 2–3% of other neighbourhoods. Lower-income neighbourhoods are also more ethnically diverse than higher-income neighbourhoods. Just under two thirds of the residents in low-income neighbourhoods are visible minorities, compared to 46% of residents in middle-income and 30% of residents in high-income neighbourhoods. A similar pattern obtains for the share of foreign-born residents. Frontline workers are also overrepresented in lower-income neighbourhoods.
4.2 COVID-19 Trajectories Among Neighbourhoods in the City of Toronto
Figure 1 illustrates the cumulative COVID-19 infection trajectories across Toronto’s neighbourhoods by their income level. Across the city, COVID-19 infection rates remained flat between January and March, rose rapidly between March and June, and plateaued in late June 2020. The pace of growth slowed down during the summer and early fall of 2020, only to surge again beginning in October 2020. During the onset of COVID-19 until mid-April, there were virtually no differences in cumulative COVID-19 infection rates across low-, middle-, and high-income neighbourhoods. However, as the pandemic progressed, differences between the COVID-19 trajectories in lower- and higher-income neighbourhoods emerged and grew. By the peak of the first wave in early summer 2020, we can see widening gaps in the cumulative COVID-19 rates between low- and higher-income neighbourhoods. By November 2020, the gap between low- and high-income neighbourhoods increased further and a gap between middle- and high-income neighbourhoods also emerged.
4.3 Results from Growth Curve Models
4.3.1 Contextual Risk Factors
Table 2 presents the results from growth curve models predicting the COVID-19 infection trajectories for the 140 neighbourhoods in Toronto. The main effects (α) capture the differences in cumulative COVID-19 rates at the onset of the pandemic, and the slopes (β) capture the differences in growth rates by neighbourhood income across the time points. At the onset of the pandemic, there were virtually no contextual differences in cumulative COVID-19 rates. After this initial phase, neighbourhoods with a higher share of overcrowded households and larger commercial spaces experienced a much faster spread of COVID-19. For example, net of controls, a one standard deviation increase in the percentage of overcrowded households is associated with an additional 377 COVID-19 cases per 100,000 residents between the onset of the pandemic in March 2020 and reclosure of the economy in November 2020. By contrast, COVID-19 grew at a slower pace in highly walkable neighbourhoods. A one standard deviation increase in walkability score is associated with 154 fewer COVID-19 cases per 100,000 residents between the onset of the pandemic in March 2020 and partial closure of the economy in October 2020.
Low-income neighbourhoods experienced a faster spread of COVID-19 than higher-income neighbourhoods. For example, between March and June 2020, low-income neighbourhoods saw 129 additional COVID-19 infections per 100,000 residents than high-income neighbourhoods. COVID-19 also spread faster in neighbourhoods with a higher share of visible minorities, higher rates of employment, a higher share of front-line workers, and a higher share of residents who are 80 years and older. For example, a one standard deviation increase in the percentage of residents who are visible minorities is associated with an additional 164 COVID-19 cases per 100,000 residents between the March and November 2020. By contrast, COVID-19 spread at a slower pace in neighbourhoods with a higher share of foreign-born residents. A one standard deviation increase in the percentage of foreign-born residents is associated with 114 fewer COVID-19 cases per 100,000 residents between March and June 2020. Generally positive coefficients on the spatial lag variable indicate that the prevalence of COVID-19 infections in surrounding neighbourhoods increases the infection rate in a given neighbourhood, as we would expect.
The availability and quality of neighbourhoods’ physical infrastructure may vary by their socioeconomic composition. In addition, residents of low-income neighbourhoods may rely more or differently on community resources than residents of higher-income neighbourhoods because they have fewer individual resources at their disposal. As such, the relationship between neighbourhoods’ social contexts and the spread of COVID-19 may vary across low-, middle-, and high-income areas. In the section that follows, we present the results of our analyses stratified by neighbourhood income level.
4.4 Socioeconomic Variation in the Relationship Between Neighbourhood Social Context and the Spread of COVID-19
Table 3 presents the results from the growth curve models predicting cumulative COVID-19 rates, separately by neighbourhood income level. COVID-19 grew faster across all neighbourhoods with a poorer walkability, a higher share of overcrowded households, larger commercial areas, and a higher share of frontline workers, irrespective of their income levels. However, the extent to which these dimensions of neighbourhood social contexts are associated with the spread of COVID-19 differs according to their income levels. Neighbourhood walkability is associated with a slower surge in COVID-19 infections across all neighbourhoods, but the negative association is much larger in low-income than in middle- or high-income neighbourhoods during the middle portion of our observation period (March through October). For example, in low-income neighbourhoods, a one standard deviation increase in the walk score rankings is associated with 140 fewer COVID-19 cases per 100,000 residents between March and October 2020. By contrast, in high-income neighbourhoods, the corresponding increase is associated with 75 fewer cases in high-income neighbourhoods during the same period. A higher share of frontline workers is associated with a faster increase in COVID-19 infections in all neighbourhoods, but this positive association is much smaller in high-income than in low- or middle-income neighbourhoods.
Some dimensions of the neighbourhood social contexts shape the spread of COVID-19 differently depending on their income levels. Net of the share of overcrowded households, a higher population density is associated with a slower increase in COVID-19 infections in high-income neighbourhoods, but a faster surge in low- and middle-income neighbourhoods. In high-income neighbourhoods, a one unit increase in population density is associated with 221 fewer COVID-19 cases per 100,000 residents between March and June 2020. In low-income neighbourhoods, the corresponding increase is associated with 36 more COVID-19 cases during the same period. By contrast, a higher share of visible minority residents is associated with a slower surge in COVID-19 infections in low-income neighbourhoods, but a faster surge in high-income neighbourhoods. For example, in low-income neighbourhoods, a one standard deviation increase in the percentage of visible minority residents is associated with 83 fewer COVID-19 cases per 100,000 residents between the onset of the pandemic in March 2020 and partial lockdown in October 2020. In high-income neighbourhoods, the corresponding increase is associated with 325 more COVID-19 cases per 100,000 residents during the same time. The opposite pattern obtains for the share of foreign-born residents: a higher share of non-Canadian born residents is associated with a faster spread of COVID-19 in low-income neighbourhoods but a slower spread in higher-income areas.
5 Conclusion
The COVID-19 pandemic has underscored the importance of neighbourhood contexts for residents’ health. Reliance on census and survey data has meant that much of the extant research has focused primarily on the sociodemographic correlates of COVID-19 infection and death rates but has paid less attention to how neighbourhoods’ built environments influence the spread of COVID-19. We fill this gap in the literature by comparing the COVID-19 trajectories of neighbourhoods of varying socioeconomic statuses and assessing whether and how their sociodemographic composition and built environments contribute to the spread of COVID-19. Our study yields several noteworthy findings, which are summarized in Table 4.
We find that the built environment has shaped the pace of COVID-19’s spread across the City of Toronto’s 140 neighbourhoods. Irrespective of a neighbourhood’s socioeconomic status, COVID-19 increased faster in neighbourhoods with a high share of overcrowded households and larger commercial areas. More household members sharing smaller spaces means that residents encounter multiple sources of exposure and lack the space necessary for self-isolation if they are infected with COVID-19 (Kamis et al., 2021). Commercial zones are generally more crowded and are more likely to include facilities with high predicted transmission rates (e.g., stores, restaurants, and stadiums) than residential areas, increasing residents’ risk of exposure to the COVID-19 virus and COVID-19 infections (Chang et al., 2021). These findings suggest that post-pandemic urban planning efforts could entail increasing the supply of housing with enough space for all household members and reducing urban density.
We also show that COVID-19 infections spread at a slower pace in highly walkable neighbourhoods. Residents’ ability to run errands quickly and easily may mean fewer points of exposure to the COVID-19 virus, which in turn would reduce people’s risk of COVID-19 infections (Wali & Frank, 2021). Our findings, however, suggest that neighbourhood walkability mitigates the spread of COVID-19 more in low-income than in middle- or high-income neighbourhoods, at least through the partial lockdown in October 2020. When stores, restaurants, and other establishments were still allowed to operate largely as before, the ability to run errands on foot with ease reduces urban dwellers’ vulnerability to infectious diseases, but it has a larger impact on residents of low-income neighbourhoods. Living in a walkable neighbourhood and shortening travel times may be particularly important for residents of low-income neighbourhoods with lower propensity to own cars, greater reliance on public transit when running errands, and greater exposure to poorly maintained sidewalks. Post-pandemic urban planning efforts should strive to design more walkable urban neighbourhoods, and to prioritize lower-income neighbourhoods when doing so.
Our results further reveal that other dimensions of the built environments shape the spread of COVID-19 infections differently depending on a neighbourhood’s income level. For example, net of the share of overcrowded households, population density is associated with a smaller surge in COVID-19 infection rates in high-income neighbourhoods, but a larger surge in low-income neighbourhoods. In high-income neighbourhoods, high-density apartment buildings come with amenities, like better ventilation systems and additional staff to properly sanitize common areas. In low-income neighbourhoods, similarly dense buildings may be inadequately maintained and lack such amenities. The former likely offers residents of highly dense, high-income neighbourhoods another layer of protection against the COVID-19 virus. The latter enhances the risk of COVID-19 infection among residents of highly dense, low-income neighbourhoods.
Similarly, the association between the sociodemographic profiles of neighbourhoods and the spread of COVID-19 infections may also vary by neighbourhood income levels. A higher share of frontline workers was associated with a larger increase in COVID-19 infection rates across all neighbourhoods. Although this pattern held across neighbourhood with varying socioeconomic status, it had a generally smaller impact in high-income neighbourhoods. Frontline workers (e.g., those in healthcare) tend to have higher exposure to the COVID-19 virus in their workplace (Blundell et al., 2020). Relative to their socioeconomically disadvantaged peers, advantaged frontline workers are more likely to have greater access adequate personal protective equipment (Nguyen et al., 2020; St-Denis, 2020).
Additionally, a higher percentage of foreign-born residents was associated with a slower pace of spread of COVID-19 in middle- and high-income neighbourhoods and a faster spread in low-income neighborhoods. Due to their sustained close contact with their country of origin, some of these immigrants may have been aware of the public health mandates used in countries that were more successful at containing COVID-19 (Choi et al., 2021a, 2021b). They may have adopted some of those preventive measures at the onset of the pandemic, which helped curb the spread of COVID-19 in their neighbourhoods (e.g., East Asian immigrants wore masks at higher rates earlier in the pandemic). Foreign-born individuals living in high-income neighbourhoods are disproportionately more likely than their peers in lower-income neighbourhoods to be high-skilled, economic immigrants. They are a positively selected group disproportionately represented in industries such as international banking or international trade that almost fully transitioned to telecommuting during the pandemic (Papanikolaou & Schmidt, 2020).
Finally, COVID-19 spread faster in high-income neighbourhoods with higher percentages of racial minorities—contrary to what we observe in low-income neighbourhoods. This difference likely reflects the residential settlement patterns of high-income racial minorities. As in many other global cities, socioeconomically advantaged racial minorities in the City of Toronto generally settle in affluent neighbourhoods with higher percentages of co-ethnics (Clark & Fossett, 2008; Walks & Bourne, 2006). Partially due to residential segregation by race, these neighbourhoods are also located near lower-income neighbourhoods with high percentages of racial minorities who have been disproportionately affected by COVID-19 (see Figure A3).
Our study is not without its limitations. First, while Toronto is a useful case study (given that it is sociodemographically diverse and has been an urban epicenter of the COVID-19 pandemic), future studies should examine the relationship between the built environment and the spread of infectious diseases across different urban settings. Second, we considered but were unable to include several other indicators of a neighbourhood’s social context due to a high degree of collinearity. We chose to focus on features that seem to be central to the literature, and in supplementary analyses that included other bundles of neighbourhood amenities and composition measures (available upon request), our results were robust. Nonetheless, our models may have missed some important dimensions of a neighbourhood’s social context. Third, we would have liked to capture variation in the quality and usage of neighbourhoods’ physical infrastructure. Such information is seldom available, including in the otherwise rich administrative datasets provided by the City of Toronto. Fourth, we rely on cross-sectional sociodemographic and contextual data, and our aim is to describe how these may be related to the spread of infectious diseases such as COVID-19. Future studies could make greater efforts to establish the causal links between neighbourhood social contexts and the spread of COVID-19. Finally, it is likely that there has been systematic underreporting of COVID-19 infections and mortality, which in turn poses a challenge to researchers seeking to understand the extent of the pandemic and its social and epidemiological drivers (see, e.g., Albani et al. 2021; Whittaker et al., 2021). At the same time, we contend that the issue is somewhat mitigated by our focus on a single city with more consistent reporting than, say, a province, country, or several countries in a comparative context. If anything, we likely underestimate differences across neighbourhoods by income level, as errors in reporting are more likely in places where residents have less reliable access to health care.
Notwithstanding these limitations, our study makes important contributions by illustrating the importance of neighbourhoods’ built environments in generating health inequalities. COVID-19 spreads more quickly in low-income neighbourhoods, in part because higher shares of their private households are overcrowded and more of their residents’ work in frontline occupations with a greater risk of exposure to COVID-19. In addition to underscoring the importance for future scholarship on neighbourhood effects to explicitly consider the built environment, our findings suggest that introducing and upgrading built environments (e.g., reducing overcrowding, increasing neighbourhoods’ walkability, and building more open green spaces) could provide a way for policymakers to design health-promoting urban centers. Finally, we show that the same dimensions of a neighbourhood’s social context are differentially associated with the spread of infectious diseases in low-, middle-, and high-income neighbourhoods. This suggests that urban planning efforts should not adopt a one-size-fits-all strategy when reimagining cities for a post-pandemic world and be conscientious about the varying needs of residents in low-, middle-, and high-income neighbourhoods to reduce the vulnerability of marginalized communities to infectious diseases.
Data Availability
We use proprietary data from Walk Score, Inc®. Our contract precludes us from making the data available, but we can make our own codes available upon request.
Notes
We use the term “built environment” to refer to the human-made environment such as homes, buildings, parks, streets, and other features that provide settings in which people live and work on a day-to-day basis. The built environment is alternatively referred to as the physical environment or infrastructure, neighbourhood amenities, and built world in other work. We chose “built environment” because it is the term used in Healthy People 2030, an initiative in the USA that seeks to improve health and well-being, including better understanding how neighbourhoods shape residents’ health (Office of Disease Prevention and Health Promotion, n.d.).
Data was provided by Redfin Real Estate (see: https://www.walkscore.com/CA-ON/Toronto).
The Ontario government adopted a province-wide graduated framework for locking down and reopening the economy (see: https://www.ontario.ca/page/reopening-ontario). Our results are robust to the specific choice of these five time points.
Spatial autocorrelation is examined in the R environment.
Growth curve models are estimated in Stata, version 17, using the xtmixed command.
We applied two criteria in the selection of covariates: the selected combination of variables should (a) align with prior empirical work, and (b) balance the inclusion of essential covariates while avoiding multicollinearity issues. Other dimensions of neighbourhoods’ built environment we considered include the number of bars, transit hubs, inadequate or unaffordable housing, and grocery scores. We also considered additional measures of neighbourhoods’ sociodemographic composition, such as the percentage of immigrants without English/French proficiency, an ethnic diversity index, the percentage of adults 65 years and older, the percentage of Black, East Asian, or Latinx residents, and the share of health workers. Please see Table A1 for the distribution of these covariates. Results from growth curve models incorporating these measures are generally similar to those we present here, and are available upon request.
In earlier versions of the paper, we tried alternate time points during the early stages of the pandemic and obtained substantively similar results.
References
Abedi, V., Olulana, V. A., Chaudhary, D., Khan, A., Shahjouei, S., Li, J., & Zand, R. (2020). Racial, economic, and health inequality and COVID-19 infection in the United States. Journal of Racial and Ethnic Health Disparities. https://doi.org/10.1007/s40615-020-00833-4
Albani, V., Loria, J., Massad, E., & Zubelli, J. (2021). COVID-19 underreporting and its impact on vaccination strategies. BMC Infectious Diseases, 21(1), 1111. https://doi.org/10.1186/s12879-021-06780-7
Algert, S. J., Agrawal, A., & Lewis, D. S. (2006). Disparities in access to fresh produce in low-income neighbourhoods in Los Angeles. American Journal of Preventive Medicine, 30(5), 365–370. https://doi.org/10.1016/j.amepre.2006.01.009
Ali, N., & Islam, F. (2020). The effects of air pollution on COVID-19 infection and mortality—a review on recent evidence. Frontiers in Public Health, 8, 1–7. https://doi.org/10.3389/2Ffpubh.2020.580057
Alvarado, S. E. (2019). The indelible weight of place: Childhood neighbourhood disadvantage, timing of exposure, and obesity across adulthood. Health & Place, 58, 102159. https://doi.org/10.1016/j.healthplace.2019.102159
Anderson, K. F. (2017). Racial residential segregation and the distribution of health-related organizations in urban neighbourhoods. Social Problems, 64(2), 256–276. https://doi.org/10.1093/socpro/spw058
Anselin, Luc. (1988). Spatial econometrics, methods and models. Dordrecht, the Netherlands: Kluwer Academic.
Awuor, L., & Melles, S. (2019). The Influence of environmental and health indicators on premature mortality: An empirical analysis of the City of Toronto’s 140 neighbourhoods. Health & Place, 58, 102–155. https://doi.org/10.1016/j.healthplace.2019.102155
Bejan, Raluca, & Kristina Nikolova. (2020). How Canada compares to other countries on COVID-19 cases and deaths. The Conversation. Retrieved October 26, 2020 (http://theconversation.com/how-canada-compares-to-other-countries-on-covid-19-cases-and-deaths-142632).
Blundell, R., Dias, M. C., Joyce, R., & **aowei, Xu. (2020). COVID-19 and inequalities*. Fiscal Studies, 41(2), 291–319. https://doi.org/10.1111/1475-5890.12232
Borjas, G. 2020. Demographic determinants of testing incidence and COVID-19 infections in New York City neighbourhoods. Working Paper No. 26952. Cambridge, MA: National Bureau of Economic Research.
Bosma, H., Dike van de Mheen, H., Borsboom, G. J. J. M., & Mackenbach, J. P. (2001). Neighbourhood socioeconomic status and all-cause mortality. American Journal of Epidemiology, 153(4), 363–371. https://doi.org/10.1093/aje/153.4.363
Boylan, J. M., & Robert, S. A. (2017). Neighbourhood SES is particularly important to the cardiovascular health of low SES individuals. Social Science & Medicine, 188, 60–68. https://doi.org/10.1016/j.socscimed.2017.07.005
Brandén, M., Aradhya, S., Kolk, M., Härkönen, J., Drefahl, S., Malmberg, Bo., Rostila, M., Cederström, A., Andersson, G., & Mussino, E. (2020). Residential context and COVID-19 mortality among adults aged 70 years and older in Stockholm: A population-based, observational study using individual-level data. The Lancet Healthy Longevity, 1(2), e80-88. https://doi.org/10.1016/S2666-7568(20)30016-7
Brazil, N., & Clark, W. A. V. (2017). Individual mental health, life course events and dynamic neighbourhood change during the transition to adulthood. Health & Place, 45, 99–109. https://doi.org/10.1016/j.healthplace.2017.03.007
Browning, C. R., & Cagney, K. A. (2003). Moving beyond poverty: Neighbourhood structure, social processes, and health. Journal of Health and Social Behavior, 44(4), 552–571. https://doi.org/10.2307/1519799
Browning, C. R., & Jackson, A. L. (2013). The social ecology of public space: Active streets and violent crime in urban neighbourhoods. Criminology, 51(4), 1009–1043. https://doi.org/10.1111/1745-9125.12026
Chang, S., Pierson, E., Koh, P. W., Gerardin, J., Redbird, B., Grusky, D., & Leskovec, J. (2021). Mobility network models of COVID-19 explain inequities and inform reopening. Nature, 589, 82–87. https://doi.org/10.1038/s41586-020-2923-3
Choi, K. H., Denice, P., Haan, M., & Zajacova, A. (2021a). Studying the social determinants of COVID-19 in a data vacuum. Canadian Review of Sociology, 58(2), 146–164.
Choi, K. H., Denice, P., & Ramaj, S. (2021b). Vaccine and COVID-19 trajectories. Socius: Sociological Research for a Dynamic World, 7, 1–11.
City of Toronto. (2014). TSNS 2020 Neighbourhood Equity Index: Methodological Documentation. City of Toronto: Social policy analysis and research.
City of Toronto (2015). Toronto Strong Neighbourhoods Strategy 2020. City of Toronto
Clark, W. A. V., & Fossett, M. (2008). Understanding the social context of the schelling segregation model. Proceedings of the National Academy of Sciences, 105(11), 4109–4114. https://doi.org/10.1073/pnas.0708155105
CNN Health Dashboard. (2022). Tracking Covid-19’s global spread. https://www.cnn.com/interactive/2020/health/coronavirus-maps-and-cases/
Cordes, J., & Castro, M. C. (2020). Spatial analysis of COVID-19 clusters and contextual factors in New York City. Spatial and Spatio-Temporal Epidemiology, 34, 100355. https://doi.org/10.1016/j.sste.2020.100355
Cowger, C. D. (1984). Statistical significance tests: scientific ritualism or scientific method? Social Service Review, 58(3), 358–372. http://www.jstor.org/stable/30011734
Creatore, M. I., Glazier, R. H., Moineddin, R., Fazli, G. S., Johns, A., Gozdyra, P., Matheson, F. I., Kaufman-Shriqui, V., Rosella, L. C., Manuel, D. G., & Booth, G. L. (2016). Association of neighbourhood walkability with change in overweight, obesity, and diabetes. JAMA, 315(20), 2211. https://doi.org/10.1001/jama.2016.5898
Curran, P., Obeidat, K., & Losardo, D. (2010). Twelve frequently asked questions about growth curve modeling. Journal of Cognitive Development, 11(2), 121–136.
de Souza, R. J., Gauvin, L., Williams, N. C., Lear, S. A., Oliveira, A. P., Desai, D., Corsi, D. J., Subramanian, S. V., Rana, A., Arora, R., Booth, G. L., Razak, F., Brook, J. R., Tu, J. V., & Anand, S. S. (2018). Environmental health assessment of communities across Canada: Contextual factors study of the Canadian alliance for healthy hearts and minds. Cities & Health, 2(2), 163–180. https://doi.org/10.1080/23748834.2018.1548071
Deitz, S., & Meehan, K. (2019). Plumbing poverty: map** hot spots of racial and geographic inequality in US household water insecurity. Annals of the American Association of Geographers, 109(4), 1092–1109. https://doi.org/10.1080/24694452.2018.1530587
Denice, P., Choi, K. H., Haan, M., & Zajacova, A. (2020). Visualizing the geographic and demographic distribution of COVID-19. Socius, 6, 2378023120948715. https://doi.org/10.1177/2378023120948715
Diez Roux, A. & Mair, C. (2010). Neighbourhoods and health: Neighbourhoods and health. Annals of the New York Academy of Sciences, 1186(1), 125–145. https://doi.org/10.1111/j.1749-6632.2009.05333.x
Diamant, A. L., Hays, R. D., Morales, L. S., Ford, W., Calmes, D., Asch, S., Duan, N., Fielder, E., Kim, S., Fielding, J., Sumner, G., Shapiro, M. F., Hayes-Bautista, D., & Gelberg, L. (2004). Delays and unmet need for health care among adult primary care patients in a restructured urban public health system. American Journal of Public Health, 94(5), 783–789.
Doubeni, C. A., Schootman, M., Major, J. M., Torres, R. A., Stone, A. O., Laiyemo, Y. P., Lian, M., Messer, L., Graubard, B. I., Sinha, R., Hollenbeck, A. R., & Schatzkin, A. (2011). Health status, neighbourhood socioeconomic context, and premature mortality in the United States: The National Institutes of Health–AARP Diet and Health Study. American Journal of Public Health, 102(4), 680–688. https://doi.org/10.2105/AJPH.2011.300158
Ellen, I. G., Mijanovich, T., & Dillman, K.-N. (2001). Neighbourhood effects on health: Exploring the links and assessing the evidence. Journal of Urban Affairs, 23(3–4), 391–408. https://doi.org/10.1111/0735-2166.00096
Finch, W. H., & Hernández Finch M. E. (2020). Poverty and Covid-19: Rates of incidence and deaths in the United States during the first 10 weeks of the pandemic. Frontiers in Sociology 5. https://doi.org/10.3389/fsoc.2020.00047
Fitzpatrick, K. M., & LaGory, M. (2003). 'Placing’ health in an urban sociology: Cities as mosaics of risk and protection. City & Community, 2(1), 33–46. https://doi.org/10.1111/1540-6040.00037
Frumkin, H. (2021). COVID-19, the built environment, and health. Environmental Health Perspectives, 129(7), 1–14.
Galea, S., Ahern, J., Rudenstine, S., Wallace, Z., & Vlahov, D. (2005). Urban built environment and depression: A multilevel analysis. Journal of Epidemiology & Community Health, 59(10), 822–827. https://doi.org/10.1136/jech.2005.033084
Gordon, C., Purciel-Hill, M., Ghai, N. R., Kaufman, L., Graham, R., & Van Wye, G. (2011). Measuring food deserts in New York City’s low-income neighbourhoods. Health & Place, 17(2), 696–700. https://doi.org/10.1016/j.healthplace.2010.12.012
Gould, Elise,& Heidi Shierholz. (2020). Not everybody can work from home: black and hispanic workers are much less likely to be able to telework. Economic Policy Institute. Retrieved November 9, 2020 (https://www.epi.org/blog/black-and-hispanic-workers-are-much-less-likely-to-be-able-to-work-from-home/).
Grafova, I. B. (2008). Overweight children: Assessing the contribution of the built environment. Preventive Medicine, 47(3), 304–308. https://doi.org/10.1016/j.ypmed.2008.04.012
Guliyev, H. (2020). Determining the spatial effects of COVID-19 using the spatial panel data model. Spatial Statistics, 38, 100443.
Haan, M., Kaplan, G. A., & Camacho, T. (1987). Poverty and health prospective evidence from the Alameda county study. American Journal of Epidemiology, 125(6), 989–998. https://doi.org/10.1093/oxfordjournals.aje.a114637
Hale, L., Hill, T. D., Elliot Friedman, F., Nieto, J., Galvao, L. W., Engelman, C. D., Malecki, K. M. C., & Peppard, P. E. (2013). Perceived neighbourhood quality, sleep quality, and health status: Evidence from the survey of the health of Wisconsin. Social Science & Medicine, 79, 16–22. https://doi.org/10.1016/j.socscimed.2012.07.021
Hellerstein, J. K., Neumark, D., & McInerney, M. (2008). Spatial mismatch or racial mismatch? Journal of Urban Economics, 64(2), 464–479. https://doi.org/10.1016/j.jue.2008.04.003
Hordyk, S. R., Hanley, J., & Richard, É. (2015). ‘Nature Is There; Its Free’: Urban greenspace and the social determinants of health of immigrant families. Health & Place, 34, 74–82. https://doi.org/10.1016/j.healthplace.2015.03.016
Howell, Nicholas A. (2019). Interaction between neighbourhood walkability and traffic-related air pollution on hypertension and diabetes: the CANHEART cohort. Environment International 7.
Hulchanski, D. (2006). What factors shape Canadian housing policy? The intergovernmental role in Canada’s housing system in Canada. In R. Young and C. Leuprecht (Editors). State of the Federation 2004: Municipal - Federal - Provincial Relations (Volume 10, pp. 221–247). Queen’s University Press.
Hulchanski, D. (2010). The three cities within Toronto: income polarization among Toronto’s Neighbourhoods, 1970 — 2000 (Research Bulletin 41). Cities Center. https://homelesshub.ca/sites/default/files/Three-Cities-Within-Toronto_2010_Final.pdf
Institute for Work & Health. (2021). Issue briefing: incidence of COVID-19 transmission in ontario work places. Accessed on December 12, 2021. Accessed from: https://www.iwh.on.ca/sites/iwh/files/iwh/reports/iwh_issue_briefing_covid19_workplace_ontario_2021.pdf.
Kain, J. F. (1992). The spatial mismatch hypothesis: Three decades later. Housing Policy Debate, 3(2), 371–460. https://doi.org/10.1080/10511482.1992.9521100
Kamis, C., Stolte, A., West, J., Fishman, S., Brown, T., & Farmer, H. (2021). Overcrowding and COVID-19 deaths across U.S. counties: are disparities growing over time? SSM Population Health, 15, 100845.
Kawachi, I., & Berkman, L. F. (2003). Neighbourhoods and health. Oxford University Press.
Kikuchi, G., & Desmond, S. A. (2010). A longitudinal analysis of neighborhood crime rates using latent growth curve modeling. Sociological Perspectives, 53(1), 127–149.
King, A. C., Sallis, J. F., Frank, L. D., Saelens, B. E., Cain, K., Conway, T. L., Chapman, J. E., Ahn, D. K., & Kerr, J. (2011). Aging in neighbourhoods differing in walkability and income: Associations with physical activity and obesity in older adults. Social Science & Medicine, 73(10), 1525–1533. https://doi.org/10.1016/j.socscimed.2011.08.032
Kravitz-Wirtz, N. (2016). Cumulative effects of growing up in separate and unequal neighbourhoods on racial disparities in self-rated health in early adulthood. Journal of Health and Social Behavior, 57(4), 453–470. https://doi.org/10.1177/0022146516671568
Kubrin, C. E., & Herting, J. R. (2003). Neighborhood correlates of homicide trends: An analysis using growth-curve modeling. The Sociological Quarterly, 44(3), 329–350.
Lai, K. Y., Webster, C., Kumari, S., & Sarkar, C. (2020). The nature of cities and the Covid-19 pandemic. Current Opinion in Environmental Sustainability., 46, 27–31. https://doi.org/10.1016/j.cosust.2020.08.008
Leyden, K. M. (2003). Social capital and the built environment: The importance of walkable neighbourhoods. American Journal of Public Health, 93(9), 1546–1551. https://doi.org/10.2105/AJPH.93.9.1546
Lima, F. T., Brown, N. C., & Duarte, J. P. (2021). Understanding the impact of walkability, population density, and population size on COVID-19 spread: A pilot study of the early contagion in the United States. Entropy, 23(11), 1512. https://doi.org/10.3390/e23111512
Lochner, K. A., Kawachi, I., Brennan, R. T., & Buka, S. L. (2003). Social capital and neighbourhood mortality rates in Chicago. Social Science & Medicine, 56(8), 1797–1805. https://doi.org/10.1016/S0277-9536(02)00177-6
Luo, Z.-C., Wilkins, R., Heaman, M., Martens, P., Smylie, J., Hart, L., Wassimi, S., Simonet, F., Yuquan, Wu., & Fraser, W. D. (2010). Neighbourhood socioeconomic characteristics, birth outcomes and infant mortalityamong first nations and non-first nations in Manitoba, Canada. The Open Women’ s Health Journal, 4(2), 55–61. https://doi.org/10.2174/1874291201004020055
Marwell, N. P., & Gullickson, A. (2013). Inequality in the spatial allocation of social services: Government contracts to nonprofit organizations in New York City. Social Service Review, 87(2), 319–353. https://doi.org/10.1086/670910
Massey, D. S. (1996). The age of extremes: Concentrated affluence and poverty in the twenty-first century. Demography, 33(4), 395–412. https://doi.org/10.2307/2061773
Massey, D. S., & Denton, N. A. (1993). American apartheid: Segregation and the making of the underclass. Harvard University Press.
Mein, S. A. (2020). COVID-19 and health disparities: The reality of ‘the Great Equalizer’. Journal of General Internal Medicine, 35(8), 2439–2440. https://doi.org/10.1007/s11606-020-05880-5
Nguyen, L. H., Drew, D. A., Graham, M. S., Joshi, A. D., Guo, C.-G., Ma, W., Mehta, R. S., Warner, E. T., Sikavi, D. R., Lo, C.-H., Kwon, S., Song, M., Mucci, L. A., Stampfer, M. J., Willett, W. C., Heather Eliassen, A., Hart, J. E., Chavarro, J. E., Rich-Edwards, J. W., & DaviesZhang, R. F. (2020). Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. The Lancet Public Health, 5(9), e475–e483. https://doi.org/10.1016/S2468-2667(20)30164-X
O’Campo, P., Wheaton, B., Nisenbaum, R., Glazier, R. H., Dunn, J. R., & Chambers, C. (2015). The neighbourhood effects on health and well-being (NEHW) Study. Health & Place, 31, 65–74. https://doi.org/10.1016/j.healthplace.2014.11.001
Oakes, J. M., Andrade, K. E., Biyoow, I. M., & Cowan, L. T. (2015). Twenty years of neighbourhood effect research: An assessment. Current Epidemiology Reports, 2(1), 80–87. https://doi.org/10.1007/s40471-015-0035-7
Office of Disease Prevention and Health Promotion. (n.d.). Neighbourhood and built environment. Healthy People 2030. U.S. Department of Health and Human Services. https://health.gov/healthypeople/objectives-and-data/browse-objectives/neighbourhood-and-built-environment
Oishi, Shigehiro, Youngjae Cha, & Ulrich Schimmack. (2021). The social ecology of COVID-19 cases and deaths in New York City: the role of walkability, wealth, and race. Social Psychological and Personality Science 1–10. https://journals.sagepub.com/doi/full/https://doi.org/10.1177/1948550620979259
Owens, A. (2010). Neighbourhoods and schools as competing and reinforcing contexts for educational attainment. Sociology of Education, 83(4), 287–311. https://doi.org/10.1177/0038040710383519
Papanikolaou, Dimitris, & Lawrence D. W. Schmidt. (2020). Working remotely and the supply-side impact of COVID-19. Working Paper No. 27330. Cambridge, MA: National Bureau of Economic Research.
Patel, J. A., Nielsen, F. B. H., Badiani, A. A., Assi, S., Unadkat, V. A., Patel, B., Ravindrane, R., & Wardle, H. (2020). Poverty, inequality and COVID-19: The forgotten vulnerable. Public Health, 183, 110–111. https://doi.org/10.1016/j.puhe.2020.05.006
Pearce, J. R., Richardson, E. A., Mitchell, R. J., & Shortt, N. K. (2010). Environmental Justice and health: The implications of the socio-spatial distribution of multiple environmental deprivation for health inequalities in the United Kingdom. Transactions of the Institute of British Geographers, 35(4), 522–539. https://doi.org/10.1111/j.1475-5661.2010.00399.x
Perrotta, Kim, Campbell, Monica, Chirrey, Shawn, & Frank, Larry. (2012). The walkable city: neighbourhood design and preferences, travel choices, and health. Toronto Public Health.
Phelan, Jo. C., Link, B. G., & Tehranifar, P. (2010). Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. Journal of Health and Social Behavior, 51(1_suppl), S28-40. https://doi.org/10.1177/0022146510383498
Pickett, K. E., & Pearl, M. (2001). Multilevel analyses of neighbourhood socioeconomic context and health outcomes: A critical review. Journal of Epidemiology & Community Health, 55(2), 111–122. https://doi.org/10.1136/jech.55.2.111
Renalds, A., Smith, T. H., & Hale, P. J. (2010). A systematic review of built environment and health. Family & Community Health, 33(1), 68–78. https://doi.org/10.1097/FCH.0b013e3181c4e2e5
Riley, S. (2007). Large-scale spatial-transmission models of infectious disease. Science, 316(5829), 1298–1301. https://doi.org/10.1126/science.1134695
Riva, M., Gauvin, L., & Barnett, T. A. (2007). Toward the next generation of research into small area effects on health: A synthesis of multilevel investigations published since July 1998. Journal of Epidemiology and Community Health, 61(10), 853–861. https://doi.org/10.1136/jech.2006.050740
Robert, S. A. (1999). Socioeconomic position and health: The independent contribution of community socioeconomic context. Annual Review of Sociology, 25, 489–516.
Rollston, R., & Galea, S. (2020). COVID-19 and the social determinants of health. American Journal of Health Promotion, 34(6), 687–689. https://doi.org/10.1177/0890117120930536b
Rosenthal, S. S., Strange, W. C., & Urrego, J. A. (2021). Are city centers losing their appeal? Commercial real estate, urban spatial structure, and COVID-19. Journal of Urban Economics (in Press). https://doi.org/10.1016/j.jue.2021.103381
Ross, C. E., & Mirowsky, J. (2008). Neighbourhood socioeconomic status and health: Context or composition? City & Community, 7(2), 163–179. https://doi.org/10.1111/j.1540-6040.2008.00251.x
Sallis, J. F., Saelens, B. E., Frank, L. D., Conway, T. L., Slymen, D. J., Cain, K. L., Chapman, J. E., & Kerr, J. (2009). Neighbourhood built environment and income: Examining multiple health outcomes. Social Science & Medicine, 68, 1285–1293.
Sampson, R. J. (2003). The neighbourhood context of well-being. Perspectives in Biology and Medicine, 46(3), 12.
Sarkar, C., & Weber, C. (2017). Urban environments and human health: Current trends and future directions. Current Opinion in Environmental Sustainability, 27, 33–44.
Sharkey, P., & Faber, J. W. (2014). Where, when, why, and for whom do residential contexts matter? Moving away from the dichotomous understanding of neighbourhood effects. Annual Review of Sociology, 40, 559–579.
Sheehan, C. M., Cantu, P. A., Powers, D. A., Margerison-Zilko, C. E., & Cubbin, C. (2017). Long-term neighbourhood poverty trajectories and obesity in a sample of California mothers. Health & Place, 46, 49–57. https://doi.org/10.1016/j.healthplace.2017.04.010
Shrimali, B. P., & Hwang, J. (2020). Overcrowding in the Bay Area: Where the housing crisis meets COVID-19. Federal Reserve Bank of San Francisco.
Smith, K. R., Brown, B. B., Yamada, I., Kowaleski-Jones, L., Zick, C. D., & Fan, J. X. (2008). Walkability and body mass index: Density, design, and new diversity measures. American Journal of Preventive Medicine, 35, 237–244.
Spring, A. (2018). Short- and long-term impacts of neighbourhood built environment on self-rated health of older adults. The Gerontologist, 58(1), 36–46. https://doi.org/10.1093/geront/gnx119
Ssentongo, P., Ssentongo, A. E., Heilbrunn, E. S., Ba, D. M., & Chinchilli, V. M. (2020). Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis. PLoS ONE, 15(8), e0238215. https://doi.org/10.1371/journal.pone.0238215
St-Denis, X. (2020). Sociodemographic determinants of occupational risks of exposure to COVID-19 in Canada. Canadian Review of Sociology/revue Canadienne De Sociologie, 57(3), 399–452. https://doi.org/10.1111/cars.12288
Thomas, L. J., Huang, P., Yin, F., Luo, X. I., Almquist, Z. W., Hipp, J. R., & Butts, C. T. (2020). Spatial heterogeneity can lead to substantial local variations in COVID-19 timing and severity. Proceedings of the National Academy of Sciences, 117(39), 24180–24187. https://doi.org/10.1073/pnas.2011656117
Thornton, C. M., Conway, T. L., Cain, K. L., Gavand, K. A., Saelens, B. E., Frank, L. D., Geremia, C. M., Glanz, K., King, A. C., & Sallis, J. F. (2016). Disparities in pedestrian streetscape environments by income and race/ethnicity. SSM - Population Health, 2, 206–216. https://doi.org/10.1016/j.ssmph.2016.03.004
Treiman, D. (2009). Quantitative data analysis: Doing social research to test ideas. Jossey-Bass.
Tunstall, Helena. (2005). Neighbourhoods and health. Kawachi I and Berkman LF (Eds). New York: Oxford University Press Inc
Vaughan, K. B., Kaczynski, A. T., Wilhelm, S. A., Stanis, G. M., Besenyi, R. B., & Heinrich, K. M. (2013). Exploring the distribution of park availability, features, and quality across Kansas City, Missouri by income and race/ethnicity: An environmental justice investigation. Annals of Behavioral Medicine, 45(1), 28–38. https://doi.org/10.1007/s12160-012-9425-y
Venter, Z. S., Barton, D. N., Gundersen, V., Figari, H., & Nowell, M. (2020). Urban nature in a time of crisis: Recreational use of green space increases during the COVID-19 outbreak in Oslo. Norway. Environmental Research Letters, 15, 104075. https://doi.org/10.1088/1748-9326/abb396
Verhagen, Mark D., David M. Brazel, Jennifer Beam Dowd, Ilya Kashnitsky, & Melinda Mills. (2020). Forecasting spatial, socioeconomic and demographic variation in COVID-19 health care demand in England and Wales. OSF Preprints.
Villeneuve, P. J., Jerrett, M., Su, J. G., Burnett, R. T., Chen, H., Wheeler, A. J., & Goldberg, M. S. (2012). A cohort study relating urban green space with mortality in Ontario, Canada. Environmental Research, 115, 51–58. https://doi.org/10.1016/j.envres.2012.03.003
Wali, B., & Frank, L. D. (2021). Neighbourhood-level COVID-19 hospitalizations and mortality relationships with built environment, active and sedentary travel. Health & Place, 71, 102659.
Walks, R. A., & Bourne, L. S. (2006). Ghettos in Canada’s cities? Racial segregation, ethnic enclaves and poverty concentration in Canadian urban areas. The Canadian Geographer / Le Géographe Canadien, 50(3), 273–297. https://doi.org/10.1111/j.1541-0064.2006.00142.x
Wang, Qi., Phillips, N. E., Small, M. L., & Sampson, R. J. (2018). Urban mobility and neighbourhood isolation in America’s 50 largest cities. Proceedings of the National Academy of Sciences, 115(30), 7735. https://doi.org/10.1073/pnas.1802537115
Whittaker, C., Walker, P. G. T., Alhaffar, M., Hamlet, A., Djaafara, B. A., Ghani, A., Ferguson, N., Dahab, M., Checchi, F., & Watson, O. J. (2021). Under-reporting of deaths limits our understanding of true burden of COVID-19. BMJ, 375, 2239. https://doi.org/10.1136/bmj.n2239
Wiemers, E. E., Abrahams, S., Marwa AlFakhri, V., Hotz, J., Schoeni, R. F., & Seltzer, J. A. (2020). Disparities in vulnerability to complications from COVID-19 arising from disparities in preexisting conditions in the United States. Research in Social Stratification and Mobility, 69, 100553. https://doi.org/10.1016/j.rssm.2020.100553
Wilson, W. J. (1987). The truly disadvantaged: The inner city, the underclass, and public policy. University of Chicago Press.
Yang, T.-C., & South, S. J. (2020). Neighbourhood poverty and physical health at midlife: the role of life-course exposure. Journal of Urban Health, 97(4), 486–501. https://doi.org/10.1007/s11524-020-00444-8
Acknowledgements
An earlier version of this paper was presented in the 2021 annual meeting of the Population Association of America.
Funding
This work was supported by the Social Sciences and Humanities Research Council (SSHRC) (grants 430–2017-00920, 435–2021-0701) and the SSHRC Explore Grant.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to the conceptualization and design of the study, the data analysis, and the write-up of the paper.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Table 5
Table 6
Table 7
Rights and permissions
About this article
Cite this article
Choi, K.H., Denice, P. Socioeconomic Variation in the Relationship Between Neighbourhoods’ Built Environments and the Spread of COVID-19 in Toronto, Canada. Can. Stud. Popul. 49, 149–181 (2022). https://doi.org/10.1007/s42650-022-00070-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42650-022-00070-6