Abstract
Background
Despite the demonstrated efficacy and safety of biosimilar filgrastim-aafi (Nivestim™), few studies have compared its use in real-life clinical practice to the originator filgrastim (Neupogen™).
Objectives
This study aimed to compare the effectiveness and safety of filgrastim and filgrastim-aafi for the primary prophylaxis of chemotherapy induced-febrile neutropenia in the real-life setting.
Patients and methods
A retrospective cohort study included all adult cancer patients at the King Hussein Cancer Centre requiring primary prophylaxis for chemotherapy-induced febrile neutropenia between 2014 and 2016. Two cohorts were selected: patients who received filgrastim and those who received filgrastim-aafi. The primary endpoint was the incidence of febrile neutropenia; the secondary endpoints were the incidence of adverse drug reactions (ADRs), hospital admissions due to febrile neutropenia, and the mean length of hospitalization. Chi-squared tests were performed to evaluate differences between groups. Logistic regression was conducted to adjust for confounding factors.
Results
A total of 268 patients were identified, with 88 in the filgrastim cohort and 180 in the filgrastim-aafi cohort; 64%were females. The mean age was 47 (±15) years. The incidence of febrile neutropenia was 21.6% in the filgrastim cohort and 15% in the filgrastim-aafi cohort (P = 0.179). No statistically significant differences were detected in the incidence of hospital admission (P = 0.551) or ADRs (P = 0.623) between the two cohorts. Upon adjusting for the confounding factors, results remained statistically insignificant.
Conclusion
Filgrastim and filgrastim-aafi had comparable effectiveness and safety as primary prophylaxis for chemotherapy-induced febrile neutropenia. More extensive prospective studies with additional insight on the cost implications are required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Real-life data in the study showed that the use of filgrastim-aafi (Nivestim™) as an alternative to filgrastim (Neupogen™) in preventing chemotherapy-induced febrile neutropenia can be a safe and effective alternative. |
Healthcare systems should have clear policies for biosimilar items’ use and interchangeability, in addition to structured documentation of pharmacovigilance reports to allow better clinical and financial decision making and sustain patient safety. |
1 Introduction
Febrile neutropenia (FN) is a serious adverse drug reaction (ADR) to myelosuppressive therapy [1]. It can predispose patients to life-threatening infections, lead to delayed or reduced chemotherapy doses, negatively affect treatment efficacy, and increase the financial impact on healthcare systems [2, 3].Therefore, prevention and timely management of FN are of great importance.
Granulocyte colony stimulating factors (G-CSF) enhance the production of neutrophil progenitors and release neutrophils from the bone marrow into blood [4]. G-CSFs have been found to decrease the risk of FN significantly [5]. The first commercially available G-CSF is filgrastim (Neupogen™), a non-glycosylated recombinant granulocyte-colony-stimulating factor, first licensed in 1991 [6].
The affordability of G-CSF represents a significant challenge for healthcare systems [7]. The emergence of biosimilars can address the affordability challenge due to their reduced cost compared with original reference products [8]. Such a reduction in the budget impact of G-CSF should improve access to using G-CSF primary prophylaxis for chemotherapy-induced FN, thus improving patients’ outcomes [9].
Biosimilars are large complex biological agents, considered relatively similar to originator reference products. They are expected to demonstrate high similarity to the licensed biological product (originator) in structure, function, quality, clinical efficacy, and safety [10].
Biosimilars for filgrastim emerged after its patency expired in 2006. The European Commission granted marketing authorization for filgrastim-aafi (Nivestim™) to Hospira UK Ltd in June 2010 [11]. In July 2018, filgrastim-aafi was approved by the US Food and Drug Administration (FDA) as the second approved biosimilar in the country, under the name filgrastim-aafi, with the same approved indications as filgrastim [12].
The similarity of filgrastim-aafi to filgrastim was demonstrated in pre-clinical and clinical studies. Comparability to filgrastim was shown in two randomized phase 1 trials, while therapeutic equivalence to filgrastim was demonstrated in one randomized phase 3 trial [13,14,15].
Although bioequivalence has been demonstrated, post-marketing evaluation of biosimilars in less controlled real-world settings is essential to provide evidence when biosimilars are considered as alternatives to originator reference products. In addition, real-world evidence complements generated knowledge from randomized control trials (RCTs) and improves their external validity (generalizability) [16].
Real-world evidence on the effectiveness and safety of filgrastim-aafi (Nivestim) biosimilar is limited and may not be diverse. Most published studies assessed other brands in countries of different populations and healthcare systems [17,18,19,20].
Filgrastim-aafi was introduced at the King Hussein Cancer Center (KHCC) in mid-2015 to replace filgrastim and became the only formulary brand for G-CSF at KHCC. The impact of the replacement policy has not been studied. In this study, we aimed to assess the clinical impact of G-CSF replacement at KHCC by comparing the effectiveness and safety of filgrastim-aafi and filgrastim in primary prophylaxis of chemotherapy-induced FN.
2 Material and Methods
We conducted a comparative retrospective cohort observational study at KHCC, a comprehensive cancer center in Jordan. It aimed to test the following null hypothesis:
There is no difference between filgrastim and filgrastim-aafi in a primary prophylaxis for chemotherapy-induced FN in cancer patients.
2.1 Study Setting
The use of filgrastim is based on institutional Pharmacy and Therapeutic Committee guidelines for the therapeutic use of G-CSF at KHCC. Primary prophylaxis with filgrastim is recommended for prevention of FN in high-risk patients based on age, medical history, disease characteristics, and myelotoxicity of the chemotherapy regimen. Patients over the age of 65 years, likely to require prolonged hospitalization, and receiving chemotherapy with an expected incidence of FN ≥ 20% are considered candidates for receiving GCSF as primary prophylaxis after the first cycle of chemotherapy. G-CSF is administered at 5 µg/kg/day 24 h after chemotherapy for 7–10 days or until recovery of the neutrophil count to the normal range. G-CSF is used in both inpatient and outpatient settings.
2.2 Participants and Inclusion and Exclusion Criteria
A list of newly diagnosed patients who received their first chemotherapy regimen at KHCC between 2014 and 2017 was generated. Then, patients who used filgrastim or filgrastim-aafi from 2014 to 2017 were identified using the KHCC claims database. Focusing on newly diagnosed patients facilitated tracking only primary prophylaxis episodes by identifying the first chemotherapy date at KHCC as our index date.
The study included two comparative cohorts: cohort 1—patients who received filgrastim from 2014 up to mid-2015, and cohort 2—patients who received filgrastim-aafi from mid-2015 to 2017.
Pediatric patients (aged less than 18 years), patients receiving filgrastim for secondary prophylaxis, and patients using filgrastim for any indication other than primary prophylaxis for FN were excluded.
2.3 Sample Size
The study aimed to compare the effectiveness and safety between the two cohorts. A sufficient power is needed to detect a non-inferiority of 10% in the incidence of FN between filgrastim and filgrastim-aafi. Therefore, sample size was calculated using 80% power and a two-sided α = 2.5% yielding a sample size of 86 patients filgrastim and 171 patients per filgrastim-aafi.
2.4 Variables: Exposure and Outcomes
The exposure was defined as the use of filgrastim brand, and the primary outcome was the incidence of FN. According to KHCC FN clinical practice guidelines, FN is defined as: “Patients with absolute neutrophil cell count (ANC) ≤ 500 or ANC expected to decrease to < 500 during the next 48 hour (h), AND a single oral temperature measurement ≥ 38.3 °C, in the absence of obvious environmental causes or a sustained oral temperature ≥ 38.0 °C for more than 1 h.” Secondary outcomes included: incidence of both Adverse Drug Reactions (ADRs), and admission due to FN, in addition to mean length of hospital stay.
Patients were scanned to identify chemotherapy that required primary prophylaxis according to G-CSF therapeutic guidelines. Only patients who used G-SCF starting from the first chemotherapy cycle as a primary prophylaxis were included, followed up until the end of their chemotherapy to identify any FN event during the full chemotherapy course.
2.5 Measurement of Outcomes
Detection of FN occurrence was based on finding a documented emergency department visit for this condition in the patient’s electronic medical record. Patients with FN that resulted in hospitalization were identified from hospital admission records or admission notes documented in the patient’s records. Both admission and discharge dates were recorded to calculate FN hospitalization length of stay.
ADRs were identified based on physicians’ notes or ADR notes if present in the patient’s medical record during their chemotherapy course.
2.6 Data Collection Tool
The study investigators designed a data collection form to collect patients’ demographics (age, gender) and disease characteristics (type of cancer, chemotherapy regimen, cancer stage for solid tumors) along with primary and secondary outcome data.
2.7 Statistical Analysis
Descriptive analysis was used to describe patients' characteristics. Chi-squared tests were used to test for statistical differences in incidences of FN, and admission due to FN, length of hospital stay, and ADR incidence between the two cohorts. P values < 0.05 were considered statistically significant. Potential confounders were identified using logistic regression. Adjusted and unadjusted odds ratios were reported. Analysis was conducted using SAS version 9.4 software package.
2.8 Ethics Approval
The study was approved by the Institutional Review Board (IRB) at KHCC with a waiver of consent.
3 Results
3.1 Patients’ Characteristics
Two hundred and sixty-eight patients satisfied the eligibility criteria. Eighty-eight patients were included in the filgrastim cohort and 180 in the filgrastim-aafi cohort. Sixty-four percent of the patient population were females with a mean age of 47 (SD± 15) years. Sixty-nine percent of patients had solid tumors, among whom 40.3% were diagnosed with breast cancer (see Online Supplementary Material (OSM) Table 1). The mean duration of filgrastim use was 6 (SD±1.4) days. The most commonly used chemotherapy in the filgrastim cohort was the ABVD (doxorubicin hydrochloride (adriamycin), bleomycin sulfate, vinblastine sulfate, and dacarbazine) regimen, while docetaxel was the most frequently used chemotherapy in the filgrastim-aafi cohort. OSM Table 2 shows the frequency of the most commonly used chemotherapy regimens that required primary prophylaxis with filgrastim among the two cohorts.
There was a statistically significant difference between the two cohorts in terms of gender, type of cancer (hematological or solid), and cancer stage (Table 1 in the OSM). Those characteristics were considered potential confounders. Therefore, we used logistic regression analysis to assess the impact of those confounders on the primary and secondary outcomes. Both unadjusted and adjusted odds ratios were reported.
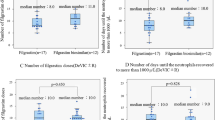
3.2 Febrile Neutropenia
The unadjusted results showed that the incidence of FN was 21.6% (n = 19) in the filgrastim cohort and 15% (n = 27) in the filgrastim-aafi cohort (P = 0.179) (Fig. 1 in the OSM). The proportions hospitalized due to severe FN were 37.2% (n = 16) of those receiving filgrastim and 43.1% of those receiving filgrastim-aafi (P = 0.551). Risk differences and 95% confidence intervals (CIs) are reported in the form of a forest plot in OSM Fig. 1.
There was, however, a statistically significant difference in the mean duration of hospitalization (P = 0.012), with a mean length of stay of 8.1 days (SD±10) for patients who received filgrastim compared to 4.1 days (SD±3.3) for those who received filgrastim-aafi.
3.3 Safety
Bone pain was identified as the most common ADR to filgrastim in both cohorts. The incidence of bone pain was not statistically significant among the two cohorts (P = 0.623). Around 5% (n = 4) of patients receiving filgrastim had bone pain compared with 3.3% (n = 6) in the filgrastim-aafi cohort. Risk differences and 95% CIs are reported in the form of a forest plot in OSM Fig. 1.
3.4 Subgroup Analysis Results
Around 40% (n = 108) of the patients had been diagnosed with breast cancer and the majority of those patients were in the filgrastim-aafi cohort. Therefore, we conducted a subgroup analysis on this sub-group. The results showed a statistically significant difference between the cohorts according to the chemotherapy protocols used. Seventy-nine of the breast cancer patients in the filgrastim-aafi cohort were on the docetaxel regimen compared with 50% in the filgrastim cohort.
3.4.1 Logistic Regression Adjusted Results
The logistic regression results showed that the difference between the two cohorts remained statistically insignificant after adjustment for gender, cancer type, diagnosis, stage, filgrastim duration, and the total number of chemotherapy cycles of the included courses. The adjusted odds ratio of FN incidence was 2.44 (95% CI 0.367–16.296), while the adjusted odds ratio of having severe FN that led to hospitalization was 0.414 (95% CI 0.06–2.905). For the incidence of ADRs, the reported adjusted odds ratio was 2.424 (95% CI 0.379–15.49).
4 Discussion
In our study, filgrastim-aafi showed no statistically significant difference in the incidence of FN, severe FN which led to hospital admissions, or in the incidence of bone pain ADR compared to filgrastim. Those real-world results were consistent with the reported results in other previously published RCTs and observation studies [13,14,15, 21]. In our study, the incidence of FN was higher in the filgrastim cohort (21.6 %) compared to the filgrastim-aafi cohort (15%), but the difference was not statistically significant, and the results fall within the range of the reported incidence (9-40%) in the published RCTs which compared biosimilar and original filgrastim [13,14,15, 22, 23]. The logistic regression showed that the results remained statistically insignificant between the two cohorts after adjusting for potential confounders. However, the reported odds ratio showed that the likelihood of FN (odds ratio 2.446) is higher in the filgrastim cohort compared to filgrastim-aafi. On the other hand, the odds of hospital admission due to FN was higher in the filgrastim-aafi cohort. Previous observational clinical trials in countries such as France, Germany, and the USA addressed the effectiveness and safety of biosimilars for filgrastim other than filgrastim-aafi. Only one non-interventional observational study in breast cancer patients has been conducted with filgrastim-aafi, in which the incidence of FN was 16% after treatment with either filgrastim or filgrastim-aafi [24]. Our subgroup analysis for breast cancer patients showed a statistically significant difference between the cohorts according to the used chemotherapy protocols. However, there was a relatively lower incidence of FN in the filgrastim-aafi cohort (8.8%). In our study, most of the breast cancer patients (94%) who required primary prophylaxis with filgrastim were in the filgrastim-aafi group and most of those patients received docetaxel chemotherapy in the early stages (1–3). This result can be explained in the context of the clinical practice changes at KHCC during 2015, where prophylaxis with filgrastim became required for all early-stage patients on docetaxel.
The incidence of hospitalization for FN was higher in the filgrastim-aafi cohort (43%) than in the filgrastim cohort (37.2%), and the incidence in both cohorts was higher than that reported in the VENICE observational study [25].
Despite having a statistically insignificant difference in terms of hospital admissions due to FN in both cohorts, we found a significant difference in the mean length of stay between them. Patients on filgrastim spent 4 days more in the hospital upon admission due to FN. This result can be explained within the context of the baseline characteristics of both cohorts. More patients with hematological malignancies were included in the filgrastim cohort. The mean length of stay per episode of FN in our study (4.1–8 days) was comparable to previously reported ranges (6–11.5 days) [26,27,28,29,30,31,32,33,34,35].
Hematological malignancies, old age, comorbid conditions, invasive fungal infection, the severity of dehydration, and pneumonia have been reported as predictors of a higher mean length of hospitalization due to FN [29,30,31,32]. Further studies are required to determine whether the filgrastim brand used can be considered a predictor for the mean length of hospitalization.
In terms of safety, as in previous studies, the most common filgrastim ADR is bone pain; however, the incidence of identified bone pain as an ADR in our study was less in both cohorts (3–5%) than what was reported in a previously published meta-analysis where the incidence was 20% [22]. The discrepancy may be due to differences in the study population, chemotherapy regimens used, number of patients, and the under-reporting of ADRs.
4.1 Limitations
First, no subgroup analysis was conducted of patients with diagnoses other than breast cancer. Further studies should be designed to identify differences according to the type of cancer and/or type of chemotherapy regimens. Second, the two groups differed significantly in gender, type of cancer (hematological or solid tumor), and stage. We adjusted the impact of such an imbalance using logistic regression rather than matching the two cohorts as upon conducting the match, the sample size was greatly reduced. However, a propensity score weighting was used to adjust for the imbalances in baseline characteristics. This method includes all the individuals in the study and avoids the impact of matching on sample size [36]. The regression model results after adding the propensity score weights showed that the effect of the G-CSF brand on the incidence of FN, incidence of admission due to FN, and the incidence of G-CSF ADRs were not significant after adjusting for gender, type of cancer, and stage.
Moreover, future studies with a larger number of patients to reach the required sample size after matching are required.
Third, the incidence of hospital admission due to FN was not analyzed according to whether the admission was to an intensive care unit or a general ward; this information would have provided more specific data for each cohort.
4.2 Policy Implications
The introduction of biosimilars to the oncology market is expected to influence the reimbursement policies, especially for those biosimilars that showed comparable results to reference originator products. Our real-world study confirms previous RCT results even within different ethnic groups in different healthcare systems.
Reaching such consistent results regarding the use of filgrastim in preventing chemotherapy-induced FN complements available knowledge and provides a comparable alternative at a lesser cost. Furthermore, both the National Comprehensive Cancer Network (NCCN) and the European Society for Medical Oncology (ESMO) clinical practice guidelines recommend the use of licensed filgrastim biosimilars [37, 38]. On the other hand, a real-world comparison of biosimilar filgrastim with pegfilgrastim biosimilar brands might be needed to identify the most cost-effective option [39, 40].
Having a hospital-based pharmacovigilance system facilitates monitoring the use of biosimilars. Thus, it is recommended to include biosimilar pharmacovigilance processes as part of a specific hospital policy for biosimilars. Moreover, it is recommended to investigate the outcomes of filgrastim-aafi in the pediatric population and indications other than chemotherapy-induced FN.
5 Conclusion
The two medications were found to be comparable; further larger observational studies in other settings are warranted. In addition, studying the cost-effectiveness and financial impact of filgrastim-aafi in primary prophylaxis of chemotherapy-induced febrile neutropenia is recommended.
References
Mitchell S, Li X, Woods M, Garcia J, Hebard-Massey K, Barron R, et al. Comparative effectiveness of granulocyte colony-stimulating factors to prevent febrile neutropenia and related complications in cancer patients in clinical practice: a systematic review. J Oncol Pharm Pract. 2016;22(5):702–16.
Liu Z, Doan QV, Malin J, Leonard R. The economic value of primary prophylaxis using pegfilgrastim compared with filgrastim in patients with breast cancer in the UK. Appl Health Econ Health Policy. 2009;7(3):193–205.
Klastersky J, de Naurois J, Rolston K, Rapoport B, Maschmeyer G, Aapro M, et al. Management of febrile neutropaenia: ESMO Clinical Practice Guidelines. Ann Oncol. 2016;27(Suppl_5):v111–8.
Price TH, Chatta GS, Dale DC. Effect of recombinant granulocyte colony-stimulating factor on neutrophil kinetics in normal young and elderly humans. Blood. 1996;88:335–40.
Morrison VA, Wong M, Hershman D, Campos LT, Ding B, Malin J. Observational study of the prevalence of febrile neutropenia in patients who received filgrastim or pegfilgrastim associated with 3–4 week chemotherapy regimens in community oncology practices. J Manag Care Pharm. 2007;13(4):337–48.
Rapoport BL, Aapro M, Paesmans M, van Eeden R, Smit T, Krendyukov A, et al. Febrile neutropenia (FN) occurrence outside of clinical trials: occurrence and predictive factors in adult patients treated with chemotherapy and an expected moderate FN risk. Rationale and design of a real-world prospective, observational, multinational. BMC Cancer. 2018;18(1):917.
de Mora F. Biosimilars: a value proposition. BioDrugs. 2019;33(4):353–6. https://doi.org/10.1007/s40259-019-00360-7.
Dinan MA, Hirsch BR, Lyman GH. Management of chemotherapy-induced neutropenia: measuring quality, cost, and value. J Natl Compr Canc Netw. 2015;13(1):e1–7.
Cornes P, Krendyukov A. The evolution of value with filgrastim in oncology. Future Oncol. 2019;15(13):1525–33. https://doi.org/10.2217/fon-2018-0762.
Declerck P, Danesi R, Petersel D, Jacobs I. The language of biosimilars: clarification, definitions, and regulatory aspects. Drugs. 2017;77(6):671–7. https://doi.org/10.1007/s40265-017-0717-1.
Hospira. Nivestym (filgrastim) [package insert]. Washington DC: US Food and Drug Administration; 2019. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761080s000lbl.pdf. Accessed 16 Jun 2019.
Hospira. Nivestim (filgrastim) [package insert]. London: European Medicines Agency; 2019. www.ema.europa.eu/en/documents/product-information/nivestim-epar-product-information_en.pdf. Accessed 16 Jun 2019.
Waller CF, Semiglazov VF, Tjulandin S, Bentsion D, Chan S, Challand R. A phase III randomized equivalence study of biosimilar filgrastim versus Amgen filgrastim in patients receiving myelosuppressive chemotherapy for breast cancer. Oncol Res Treat. 2010;33(10):504–11.
Waller CF, Bronchud M, Mair S, Challand R. Pharmacokinetic profiles of a biosimilar filgrastim and Amgen filgrastim: results from a randomized, phase I trial. Ann Hematol. 2010;89(9):927–33.
Waller CF, Bronchud M, Mair S, Challand R. Comparison of the pharmacodynamic profiles of a biosimilar filgrastim and Amgen filgrastim: results from a randomized, phase I trial. Ann Hematol. 2010;89(10):971–8.
Sherman RE, Anderson SA, Dal Pan GJ, Gray GW, Gross T, Hunter NL, LaVange L, Marinac-Dabic D, Marks PW, Robb MA, Shuren J, Temple R, Woodcock J, Yue LQ, Califf RM. Real-world evidence—what is it and what can it tell us? N Engl J Med. 2016;375(23):2293–7. https://doi.org/10.1056/NEJMsb1609216.
Nahon S, Rastkhah M, Ben Abdelghani M, Soumoudronga RF, Gasnereau I, Labourey JL. Zarzio®, biosimilar of filgrastim, in prophylaxis of chemotherapy-induced neutropenia in routine practice: a French prospective multicentric study. Support Care Cancer. 2016;24(5):1991–8.
Douglas AG, Schwab P, Lane D, Kennedy K, Slabaugh SL, Bowe A. A comparison of brand and biosimilar granulocyte-colony stimulating factors for prophylaxis of chemotherapy-induced febrile neutropenia. J Manage Care Spec Pharm. 2017;23(12):1221–6.
Damaj GL, Benbrahim O, Hacini M, Voronina I, Benabed K, Soumoudronga RF, et al. ZOHé: a prospective study of the use of biosimilar filgrastim Zarzio in clinical practice in patients treated with chemotherapy for lymphoid malignancies. Clin Lymphoma Myeloma Leuk. 2017;17(6):362–9.
Schwartzberg LS, Lal LS, Balu S, Campbell K, Brekke L, Elliott C, et al. incidence of febrile neutropenia during chemotherapy among patients with nonmyeloid cancer receiving filgrastim vs a filgrastim biosimilar. Clinicoecon Outcomes Res. 2018;10:493–500.
Yao HM, Ottery FD, Borema T, et al. PF-06881893 (Nivestym™), a Filgrastim Biosimilar, Versus US-Licensed Filgrastim Reference Product (US-Neupogen®): Pharmacokinetics, Pharmacodynamics, Immunogenicity, and Safety of Single or Multiple Subcutaneous Doses in Healthy Volunteers. BioDrugs. 2019;33:207–20. https://doi.org/10.1007/s40259-019-00343-8.
Kuderer NM, Dale DC, Crawford J, Lyman GH. Impact of primary prophylaxis with granulocyte colony-stimulating factor on febrile neutropenia and mortality in adult cancer patients receiving chemotherapy: a systematic review. J Clin Oncol. 2007;25(21):3158–67.
Cooper KL, Madan J, Whyte S, Stevenson MD, Akehurst RL. Granulocyte colony-stimulating factors for febrile neutropenia prophylaxis following chemotherapy: a systematic review and meta-analysis. BMC Cancer. 2011;11:404.
Brito M, Esteves S, André R, Isidoro M, Moreira A. Comparison of effectiveness of biosimilar filgrastim (NivestimTM), reference Amgen filgrastim and pegfilgrastim in febrile neutropenia primary prevention in breast cancer patients treated with neo(adjuvant) TAC: a non-interventional cohort study. Support Care Cancer. 2016;24(2):597–603.
Fruehauf S, Otremba B, Stötzer O, Rudolph C. Compatibility of biosimilar filgrastim with cytotoxic chemotherapy during the treatment of malignant diseases (VENICE): a prospective, multicenter, non-interventional, longitudinal study. Adv Ther. 2016;33(11):1983–2000.
Kamioner D, Fruehauf S, Maloisel F, Cals L, Lepretre S, Berthou C. Study design: two long-term observational studies of the biosimilar filgrastim NivestimTM (Hospira filgrastim) in the treatment and prevention of chemotherapy-induced neutropenia. BMC Cancer. 2013;13(1):547.
Lathia N, Mittmann N, DeAngelis C, Knowles S, Cheung M, Piliotis E, et al. Evaluation of direct medical costs of hospitalization for febrile neutropenia. Cancer. 2010;116(3):742–8.
Dulisse B, Li X, Gayle JA, Barron RL, Ernst FR, Rothman KJ, et al. A retrospective study of the clinical and economic burden during hospitalizations among cancer patients with febrile neutropenia. J Med Econ. 2013;16(6):720–35.
Lal A, Bhurgri Y, Rizvi N, Virwani M, Memon RU, Saeed W, et al. Factors influencing in-hospital length of stay and mortality in cancer patients suffering from febrile neutropenia. Asian Pac J Cancer Prev. 2008;9(2):303–8.
Schelenz S, Giles D, Abdallah S. Epidemiology, management and economic impact of febrile neutropenia in oncology patients receiving routine care at a regional UK cancer centre. Ann Oncol. 2012;23(7):1889–93.
Leese B. The costs of treating febrile neutropenia in six UK hospitals. Eur J Cancer. 1993;29A(Suppl):S15–8.
Kuderer NM, Dale DC, Crawford J, Cosler LE, Lyman GH. Mortality, morbidity, and cost associated with febrile neutropenia in adult cancer patients. Cancer. 2006;106(10):2258–66.
Kawatkar AA, Farias AJ, Chao C, Chen W, Barron R, Vogl FD, et al. Hospitalizations, outcomes, and management costs of febrile neutropenia in patients from a managed care population. Support Care Cancer. 2017;25(9):2787–95.
Weycker D, Barron R, Kartashov A, Legg J, Lyman GH. Incidence, treatment, and consequences of chemotherapy-induced febrile neutropenia in the inpatient and outpatient settings. J Oncol Pharm Pract. 2014;20(3):190–8.
Li S, Liu J, Bowers C, Garawin TAFS, Kim C, Bensink ME, et al. Febrile neutropenia-related care and associated costs in elderly patients with breast cancer, lung cancer, or non-Hodgkin lymphoma. Support Care Cancer. 2019. https://doi.org/10.1007/s00520-019-04795-0.
Olmos A, Govindasamy P (2015) A Practical Guide for Using Propensity Score Weighting in R. PracticalAssessment, Research & Evaluation, 20(13). http://pareonline.net/getvn.asp?v=20&n=13
Klastersky J, de Naurois J, Rolston K, Rapoport B, Maschmeyer G, Aapro M, Herrstedt J, ESMO Guidelines Committee. Management of febrile neutropaenia: ESMO Clinical Practice Guidelines. Ann Oncol. 2016;27(suppl 5):v111–8. https://doi.org/10.1093/annonc/mdw325.
National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncoloy.Hematopoietic Growth Factors Version 4.2021. Fort Washington (PA): National Comprehensive Cancer Network; 2021. https://www.nccn.org/professionals/physician_gls/pdf/growthfactors.pdf.
Cornes P, Gascon P, Vulto AG, Aapro M. Biosimilar pegfilgrastim: improving access and optimising practice to supportive care that enables cure. BioDrugs. 2020;34(3):255–63. https://doi.org/10.1007/s40259-020-00411-4.
Cornes P, Gascon P, Chan S, et al. Systematic review and meta-analysis of short- versus long-acting granulocyte colony-stimulating factors for reduction of chemotherapy-induced febrile neutropenia. Adv Ther. 2018;35(11):1816–29. https://doi.org/10.1007/s12325-018-0798-6.
Acknowledgements
We would like to thank our colleagues Ms. Dalia Al-Rimawi and Ms. Ayat Taqash from the biostatistics unit at OSAR for their immense support in planning and conducting the statistical analysis of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclosure
The authors received no financial support for the research, authorship, or publication of this article.
Conflict of interest
All authors declare no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Ethics approval
The Institutional Review Board has approved the study at King Hussein Cancer Center.
Consent to participate
This is a retrospective study, and participant consent is not required.
Consent for publication (include appropriate statements)
The study was approved by the Institutional Review Board at King Hussein Cancer Center for publication.
Availability of data and material
All raw data are available in a protected database at King Hussein Cancer Center.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Al-Rabayah, A.A., Al Mashni, O., Hanoun, E. et al. Effectiveness and Safety of Filgrastim (Neupogen™) versus Filgrastim-aafi (Nivestim™) in Primary Prophylaxis of Chemotherapy-Induced Febrile Neutropenia: An Observational Cohort Study. Drugs - Real World Outcomes 9, 589–595 (2022). https://doi.org/10.1007/s40801-022-00312-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-022-00312-8