Abstract
Objectives
Sleep disorders are a frequent health problem in older patients with diabetes mellitus (DM). There has been no study investigating the factors associated with excessive daytime sleepiness (EDS) in older diabetic patients. We aimed to investigate the prevalence and associated factors of EDS.
Methods
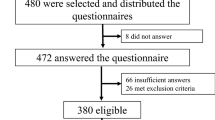
We performed a retrospective cross-sectional study in older diabetic patients. The Epworth Sleepiness Scale score of ≥ 11 points indicated EDS. All patients underwent comprehensive geriatric assessment including demographic characteristics, blood pressures, comorbid diseases, cognitive and nutritional states, basic and instrumental daily living activity indexes, lower urinary tract symptoms, and laboratory values.
Results
Of 227 patients, 73.1% were females, with a mean age of 78.8 ± 6.5. The prevalence of EDS was 19.8%. Patients with EDS were mostly males with dementia and used significantly more medication with more anticholinergic drug burden, falls, urge incontinence, and nocturia (p < 0.05). They had higher SARC-F and lower Barthel index, Lawton-Brodie, Tinetti, MMSE scores, and high-density lipoprotein than the patients without EDS (p < 0.05). After adjusting for age, sex, and dementia, all parameters that were significant in univariate analysis remained associated with EDS, except for falls, and MMSE scores.
Conclusion
The EDS was found in one in five older diabetic patients. There was a significant relationship between EDS and drug use, anticholinergic drug burden, impaired excretory functions, sarcopenia, decreased functional capacity, falls, gait-balance disorder, and cognitive dysfunction. The recognization of EDS and the implementation of interventions may be helpful in the management of geriatric syndromes.
Similar content being viewed by others
Availability of data and materials
Data are available from the authors upon reasonable request.
Code availability
N/A.
References
-https://diabetesatlas.org/. Access date: 16.08.2023.
Gooneratne NS, Weaver TE, Cater JR et al (2003) Functional outcomes of excessive daytime sleepiness in older adults. J Am Geriatr Soc 51:642–649. https://doi.org/10.1034/j.1600-0579.2003.00208.x
Surani S, Brito V, Surani A et al (2015) Effect of diabetes mellitus on sleep quality. World J Diabetes 6:868–873. https://doi.org/10.4239/wjd.v6.i6.868.PMID:26131327;PMCID:PMC4478581
Einhorn D, Stewart DA, Erman MK et al (2007) Prevalence of sleep apnea in a population of adults with type 2 diabetes mellitus. Endocr Pract 13:355–362. https://doi.org/10.4158/EP.13.4.355
Talaz D, Kızılcı S (2015) Tip 2 diyabet riski ve hastalık sürecinde uykunun rolü. Dokuz Eylül Üniv Hemşirelik Fak Elektr Derg 8:203–208
Anothaisintawee T, Reutrakul S, Van Cauter E et al (2016) Sleep disturbances compared to traditional risk factors for diabetes development: systematic review and meta-analysis. Sleep Med Rev 30:11–24. https://doi.org/10.1016/j.smrv.2015.10.002
Shan Z, Ma H, **e M et al (2015) Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care 38:529–537. https://doi.org/10.2337/dc14-2073
Keskin A, Ünalacak M, Bilge U et al (2015) Effects of sleep disorders on hemoglobin A1c levels in type 2 diabetic patients. Chin Med J (Engl) 128:3292–3297. https://doi.org/10.4103/0366-6999.171415.PMID:26668142;PMCID:PMC4797503
Yusuf FLA, Tang TS, Karim ME (2022) The association between diabetes and excessive daytime sleepiness among American adults aged 20–79 years: findings from the 2015–2018 National Health and Nutrition Examination Surveys. Ann Epidemiol 68:54–63. https://doi.org/10.1016/j.annepidem.2022.01.002
Ganidagli S, Ozturk E, Ozturk ZA (2023) Risk factors of poor sleep quality in older adults: an analysis based on comprehensive geriatric assessment. Curr Med Res Opin 39:701–706. https://doi.org/10.1080/03007995.2023.2192124
Koc Okudur S, Soysal P (2021) Excessive daytime sleepiness is associated with malnutrition, dysphagia, and vitamin d deficiency in older adults. J Am Med Dir Assoc 22:2134–2139. https://doi.org/10.1016/j.jamda.2021.05.035
Hayley AC, Williams LJ, Kennedy GA et al (2014) Prevalence of excessive daytime sleepiness in a sample of the Australian adult population. Sleep Med 15:348–354. https://doi.org/10.1016/j.sleep.2013.11.783
Šiarnik P, Klobučníková K, Šurda P et al (2018) Excessive daytime sleepiness in acute ischemic stroke: association with restless legs syndrome, diabetes mellitus, obesity, and sleep-disordered breathing. J Clin Sleep Med 14:95–100. https://doi.org/10.5664/jcsm.6890.PMID:29117882;PMCID:PMC5734901
Ng WL, Shaw JE, Peeters A (2018) The relationship between excessive daytime sleepiness, disability, and mortality, and implications for life expectancy. Sleep Med 43:83–89. https://doi.org/10.1016/j.sleep.2017.11.1132
Ohayon MM, Vecchierini MF (2002) Daytime sleepiness and cognitive impairment in the elderly population. Arch Intern Med 162:201–208. https://doi.org/10.1001/archinte.162.2.201
Brassington GS, King AC, Bliwise DL (2000) Sleep problems as a risk factor for falls in a sample of community-dwelling adults aged 64–99 years. J Am Geriatr Soc 48:1234–1240. https://doi.org/10.1111/j.1532-5415.2000.tb02596.x
Lopes JM, Dantas FG, Medeiros JL (2013) Excessive daytime sleepiness in the elderly: association with cardiovascular risk, obesity and depression. Rev Bras Epidemiol 16:872–879. https://doi.org/10.1590/s1415-790x2013000400007
Soysal P, Smith L, Tan SG et al (2021) Excessive daytime sleepiness is associated with an increased frequency of falls and sarcopenia. Exp Gerontol 150:111364. https://doi.org/10.1016/j.exger.2021.111364
Heybeli C, Soysal P, Oktan MA et al (2022) Associations between nutritional factors and excessive daytime sleepiness in older patients with chronic kidney disease. Aging Clin Exp Res 34:573–581. https://doi.org/10.1007/s40520-021-01966-0
Ali Zohal M, Yazdi Z, Kazemifar AM (2013) Daytime sleepiness and quality of sleep in patients with COPD compared to control group. Glob J Health Sci 5:150–155. https://doi.org/10.5539/gjhs.v5n3p150.PMID:23618484;PMCID:PMC4776817
Plantinga L, Rao MN, Schillinger D (2012) Prevalence of self-reported sleep problems among people with diabetes in the United States, 2005–2008. Prev Chronic Dis. https://doi.org/10.5888/pcd9.110244
Hayashino Y, Yamazaki S, Nakayama T et al (2008) Relations hip between diabetes mellitus and excessive sleepiness during driving. Exp Clin Endocrinol Diabetes 116:1–5. https://doi.org/10.1055/s-2007-984442
Bixler EO, Vgontzas AN, Lin HM et al (2005) Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab 90:4510–4515. https://doi.org/10.1210/jc.2005-0035
Ioja S, Weir ID, Rennert NJ (2012) Relationship between sleep disorders and the risk for develo** type 2 diabetes mellitus. Postgrad Med 124:119–129. https://doi.org/10.3810/pgm.2012.07.2573
Kara B, Kılıç Ö (2015) Predictors of poor sleep quality and excessive daytime sleepiness in Turkish adults with type 2 diabetes. J Clin Nurs 24:1436–1439. https://doi.org/10.1111/jocn.12710
Medeiros C, Bruin V, Férrer D et al (2013) Excessive daytime sleepiness in type 2 diabetes. Arq Bras Endocrinol Metabol 57:425–430. https://doi.org/10.1590/s0004-27302013000600003
Griggs S, Hickman RL, Strohl KP et al (2021) Sleep-wake characteristics, daytime sleepiness, and glycemia in young adults with type 1 diabetes. J Clin Sleep Med 17:1865–1874. https://doi.org/10.5664/jcsm.9402.PMID:33949941;PMCID:PMC8636341
Naharci MI, Katipoglu B, Tasci I (2022) Association of anticholinergic burden with undernutrition in older adults: A cross-sectional study. Nutr Clin Pract 37:1215–1224. https://doi.org/10.1002/ncp.10821
LeRoith D, Biessels GJ, Braithwaite SS et al (2019) Treatment of diabetes in older adults: an endocrine society* clinical practice guideline. J Clin Endocrinol Metab 104:1520–1574. https://doi.org/10.1210/jc.2019-00198.PMID:30903688;PMCID:PMC7271968
Dutoglu E, Soysal P, Smith L et al (2019) Nocturia and its clinical implications in older women. Arch Gerontol Geriatr 85:103917. https://doi.org/10.1016/j.archger.2019.103917
Bastien CH, Vallières A, Morin CM (2001) Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2:297–307. https://doi.org/10.1016/s1389-9457(00)00065-4
Morley JE, Malmstrom TK, Miller DK (2012) A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging 16:601–608. https://doi.org/10.1007/s12603-012-0084-2
Malmstrom TK, Miller DK, Simonsick EM et al (2016) SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle 7:28–36. https://doi.org/10.1002/jcsm.12048
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31. https://doi.org/10.1093/ageing/afy169
Vellas B, Villars H, Abellan G et al (2006) Overview of the MNA–Its history and challenges. J Nutr Health Aging 10:456–463
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index. Md State Med J 14:61–65
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34:119–126. https://doi.org/10.1111/j.1532-5415.1986.tb05480.x
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198. https://doi.org/10.1016/0022-3956(75)90026-6
Durmaz B, Soysal P, Ellidokuz H et al (2018) Validity and reliability of geriatric depression scale-15 (short form) in Turkish older adults. North Clin Istanb 5:216–220. https://doi.org/10.14744/nci.2017.85047.PMID:30688929;PMCID:PMC6323561
Johns MW (1992) Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 15:376–381. https://doi.org/10.1093/sleep/15.4.376
Izci B, Ardic S, Firat H et al (2008) Reliability and validity studies of the Turkish version of the Epworth Sleepiness Scale. Sleep Breath 12:161–168. https://doi.org/10.1007/s11325-007-0145-7
Johns MW (2000) Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the epworth sleepiness scale: failure of the MSLT as a gold standard. J Sleep Res 9:5–11. https://doi.org/10.1046/j.1365-2869.2000.00177.x
Vashum KP, McEvoy MA, Hancock SJ et al (2015) Prevalence of and associations with excessive daytime sleepiness in an Australian older population. Asia Pac J Public Health 27:2275–2284. https://doi.org/10.1177/1010539513497783
Lima CA, Soares WJ, Bilton TL et al (2015) Correlates of excessive daytime sleepiness in community-dwelling older adults: an exploratory study. Rev Bras Epidemiol 18:607–617. https://doi.org/10.1590/1980-5497201500030007
Lee HJ, Oh KS, Kim T et al (2014) Prevalence, risk factors, and impact of excessive daytime sleepiness in an elderly Korean population. Sleep Med Res 5:54–61. https://doi.org/10.17241/smr.2014.5.2.54
Kaneita Y, Ohida T, Uchiyama M et al (2005) Excessive daytime sleepiness among the Japanese general population. J Epidemiol 15:1–8. https://doi.org/10.2188/jea.15.1
Honig E, Green A, Dagan Y (2021) Gender differences in the sleep variables contributing to excessive daytime sleepiness among patients with obstructive sleep apnea. Sleep Breath 25:1837–1842. https://doi.org/10.1007/s11325-020-02276-x
Nugent AM, Gleadhill I, McCrum E et al (2001) Sleep complaints and risk factors for excessive daytime sleepiness in adult males in Northern Ireland. J Sleep Res 10:69–74. https://doi.org/10.1046/j.1365-2869.2001.00226.x
Happe S (2003) Excessive daytime sleepiness and sleep disturbances in patients with neurological diseases: epidemiology and management. Drugs 63:2725–2737. https://doi.org/10.2165/00003495-200363240-00003
Smagula SF, Jia Y, Chang CH et al (2020) Trajectories of daytime sleepiness and their associations with dementia incidence. J Sleep Res 29:e12952. https://doi.org/10.1111/jsr.12952
Soysal P, Tan SG (2021) The prevalence and co-incidence of geriatric syndromes in older patients with early-stage Alzheimer’s disease and dementia with Lewy bodies. Aging Clin Exp Res 33:2599–2603. https://doi.org/10.1007/s40520-020-01774-y
Xu W, Tan CC, Zou JJ et al (2020) Sleep problems and risk of all-cause cognitive decline or dementia: an updated systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 91:236–244. https://doi.org/10.1136/jnnp-2019-321896
Malhotra RK (2022) Neurodegenerative Disorders and Sleep. Sleep Med Clin 17:307–314. https://doi.org/10.1016/j.jsmc.2022.02.009
Cavaillès C, Berr C, Helmer C et al (2022) Complaints of daytime sleepiness, insomnia, hypnotic use, and risk of dementia: a prospective cohort study in the elderly. Alzheimers Res Ther 14:12. https://doi.org/10.1186/s13195-021-00952-y
Tunc M, Soysal P, Pasin O et al (2023) Hypomagnesemia Is associated with excessive daytime sleepiness, but not insomnia, in older adults. Nutrients 15:2467. https://doi.org/10.3390/nu15112467
Maglione JE, Ancoli-Israel S, Peters KW et al (2012) Depressive symptoms and subjective and objective sleep in community-dwelling older women. J Am Geriatr Soc 60:635–643. https://doi.org/10.1111/j.1532-5415.2012.03908.x
Koç Okudur S, Sosyal P, Smıth L et al (2021) Evaluation of the Clinical Effects of Insomnia and Excessive Daytime Sleepiness in Older Adults. Dokuz Eylül Üniv Hemşirelik Fak Elektr Derg 14:433–441. https://doi.org/10.46483/deuhfed.969583
Miner B, Kryger MH (2020) Sleep in the aging population. Sleep Med Clin 15:311–318. https://doi.org/10.1016/j.jsmc.2020.02.016
O’Dwyer M, Maidment ID, Bennett K et al (2016) Association of anticholinergic burden with adverse effects in older people with intellectual disabilities: an observational cross-sectional study. Br J Psychiatry 209:504–510. https://doi.org/10.1192/bjp.bp.115.173971
Cakirca M, Soysal P, Koc Okudur S et al (2022) Anticholinergic burden and increased excessive daytime sleepiness in older women. J Am Med Dir Assoc 23:1092–1093. https://doi.org/10.1016/j.jamda.2022.01.060
Catikkas NM, Erdogan TO, Reginster JY et al (2023) Prevalence and determinants of falls in community-dwelling older adults in Türkiye: a population-based cross-sectional study conducted between 2014 and 2015. Curr Aging Sci 16:133–142. https://doi.org/10.2174/1874609816666230109153424
Dokuzlar O, Koc Okudur S, Soysal P et al (2020) Factors that increase risk of falling in older men according to four different clinical methods. Exp Aging Res 46:83–92. https://doi.org/10.1080/0361073X.2019.1669284
Dokuzlar O, Koc Okudur S, Smith L et al (2020) Assessment of factors that increase risk of falling in older women by four different clinical methods. Aging Clin Exp Res 32:483–490. https://doi.org/10.1007/s40520-019-01220-8
Nakakubo S, Doi T, Shimada H et al (2018) The Association Between Excessive Daytime Sleepiness and gait parameters in community-dwelling older adults: cross-sectional findings from the Obu Study of Health Promotion for the Elderly. J Aging Health 30:213–228. https://doi.org/10.1177/0898264316673253
Huang WC, Lin CY, Togo F et al (2022) Nonlinear associations between sleep patterns and sarcopenia risks in older adults. J Clin Sleep Med 18:731–738. https://doi.org/10.5664/jcsm.9698.PMID:34608860;PMCID:PMC8883095
Tuna F, Üstündağ A, Başak Can H et al (2019) Rapid geriatric assessment, physical activity, and sleep quality in adults aged more than 65 years: A Preliminary Study. J Nutr Health Aging 23:617–622. https://doi.org/10.1007/s12603-019-1212-z
Ida S, Kaneko R, Nagata H et al (2019) Association between sarcopenia and sleep disorder in older patients with diabetes. Geriatr Gerontol Int 19:399–403. https://doi.org/10.1111/ggi.13627
Li X, He J, Sun Q (2023) Sleep duration and sarcopenia: an updated systematic review and meta-analysis. J Am Med Dir Assoc 24:1193-1206.e5. https://doi.org/10.1016/j.jamda.2023.04.032
Sacomori C, Cardoso FL, Louzada FM et al (2014) Excessive daytime sleepiness and nocturia in women. Sleep Med 15:677–680. https://doi.org/10.1016/j.sleep.2014.01.017
Kara O, Elibol T, Koc Okudur S et al (2023) Associations between anemia and insomnia or excessive daytime sleepiness in older adults. Acta Clin Belg 78:223–228. https://doi.org/10.1080/17843286.2022.2116895
Pearlman A, Kreder K (2020) Evaluation and treatment of urinary incontinence in the aging male. Postgrad Med 132:9–17. https://doi.org/10.1080/00325481.2020.1831790
Zhan Y, Chen R, Yu J (2014) Sleep duration and abnormal serum lipids: the China Health and Nutrition Survey. Sleep Med 15:833–839. https://doi.org/10.1016/j.sleep.2014.02.006
Acknowledgements
The authors certify that they comply with the ethical guidelines for authorship and publishing of Aging and Clinical Experimental Research.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
NMC: Methodology, Writing—Original Draft Preparation, Writing—Review & Editing, Formal Analysis. MT: Writing—Review & Editing. PS: Conceptualisation, Methodology, Writing—Review & Editing, Supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. The study was conducted in compliance with the current guidelines of the Helsinki Declaration. The ethics approval was obtained from the local Ethics Committee (Number: E-35700536–108.99–99855 and file number: 2023/99855) and all patients gave their signed consent.
Ethical approval
We obtained ethical approval from the Bezmialem Vakif University Ethical Board.
Statement of human and animal rights
All the procedures performed in this study involving human participants were in accord ance with the ethical standards of the institutional and national research committee.
Consent to participate
We received informed consent from all participants.
Consent for publication
We received informed consent from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Catikkas, N.M., Tunc, M. & Soysal, P. The prevalence of excessive daytime sleepiness and associated factors in older diabetic patients. Aging Clin Exp Res 35, 3205–3214 (2023). https://doi.org/10.1007/s40520-023-02602-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02602-9