Abstract
Background
Women aged 65 years and over are at increased risk of falling. Falls in this age group increase the risk of morbidity and mortality.
Aims
The aim of the present study was to find the most common factors that increase the risk of falling in older women, by using four different assessment methods.
Methods
682 women, who attended a geriatric outpatient clinic and underwent comprehensive geriatric assessment, were included in the study. History of falling last year, the Timed Up and Go (TUG) test, Performance-Oriented Mobility Assessment (POMA), and 4-m walking speed test were carried out on all patients.
Results
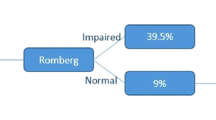
The mean age (SD) of patients were 74.4 (8.5) years. 31.5% of women had a history of falling in the last year. 11%, 36.5%, and 33.3% of patients had a falling risk according to POMA, TUG and 4-m walking speed test, respectively. We identified the following risk factors that increase the risk of falling, according to these four methods: urinary incontinence, dizziness and imbalance, using a walking stick, frailty, dynapenia, higher Charlson Comorbidity Index and Geriatric Depression Scale score, and lower basic and instrumental activities of daily living scores (p < 0.05). We found a significant correlation between all the assessment methods (p < 0.001).
Conclusion
There is a strong relationship between fall risk and dizziness, using a walking stick, dynapenia, high number of comorbidities, low functionality, and some geriatric syndromes such as depression, frailty, and urinary incontinence in older women. Therefore, older women should routinely be screened for these risk factors.
Similar content being viewed by others
References
Lakhan P, Jones M, Wilson A et al (2015) A prospective cohort study of geriatric syndromes among older medical patients admitted to acute care hospitals. J Am Geriatr Soc 59:2001–2008
Tinetti ME, Kumar C (2010) The patient who falls: “it’s always a trade-off”. JAMA 303:258–266
World Health Organization (2007) WHO global report on falls prevention in older age. WHO, Geneva
World Health Organization. 16 Jan 2018. http://www.who.int/news-room/fact-sheets/detail/falls
King B, Pecanac K, Krupp A et al (2018) Impact of fall prevention on nurses and care of fall risk patients. Gerontologist 58:331–340
Mazur K, Wilczyński K, Szewieczek J (2016) Geriatric falls in the context of a hospital fall prevention program: delirium, low body mass index, and other risk factors. Clin Interv Aging 11:1253–1261
Ambrose AF, Paul G, Hausdorff JM (2013) Risk factors for falls among older adults: a review of the literature. Maturitas 75:51–61
Stevens JA, Ballesteros MF, Mack KA et al (2012) Gender differences in seeking care for falls in the aged Medicare population. Am J Prev Med 43:59–62
Duckham RL, Procter-Gray E, Hannan MT et al (2013) Sex differences in circumstances and consequences of outdoor and indoor falls in older adults in the MOBILIZE Boston cohort study. BMC Geriatr 13:133
Stevens JA, Sogolow ED (2005) Gender differences for non-fatal unintentional fall related injuries among older adults. Inj Prev 11:115–119
Unutmaz GD, Soysal P, Tuven B et al (2018) Costs of medication in older patients: before and after comprehensive geriatric assessment. Clin Interv Aging 13:607–613
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, Arlington. https://doi.org/10.1176/appi.books.9780890425596
Aydin AE, Soysal P, Isik AT (2017) Which is preferable for orthostatic hypotension diagnosis in older adults : active standing test or head-up tilt table test? Clin Interv Aging 12:207–212
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Morris JC (1993) The clinical dementia rating (CDR): current version and scoring rules. Neurology 43:2412–2414
Dokuzlar O, Soysal P, Usarel C et al (2018) The evaluation and design of a short depression screening tool in Turkish older adults. Int Psychogeriatr 30:1541–1548
Durmaz B, Soysal P, Ellidokuz H et al (2018) Validity and reliability of geriatric depression scale—15 (short form) in Turkish older adults. North Clin Istanb 5:216–220
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel index. Md State Med J 14:61–65
Guigoz Y (2006) The Mini Nutritional Assessment (MNA) review of the literature—what does it tell us? J Nutr Health Aging 10:466–485
van Kan GA, Rolland YM, Morley JE (2008) Frailty: toward a clinical definition. J Am Med Dir Assoc 9:71–72
Bulut EA, Soysal P, Aydin AE et al (2017) Vitamin B12 deficiency might be related to sarcopenia in older adults. Exp Gerontol 95:136–140
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39:142–148
Shumway-Cook A, Brauer S, Woollacott M (2000) Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther 80:896–903
Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34:119–126
Al-Momani M, Al-Momani F, Alghadir AH et al (2016) Factors related to gait and balance deficits in older adults. Clin Interv Aging 11:1043–1049
BCGuidelines.ca (2017) Frailty in older adults—early identification and management. https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/bcguidelines/frailty-gaitspeed.pdf. Accessed 18 Oct 2018
Gale CR, Cooper C, Aihie Sayer A (2016) Prevalence and risk factors for falls in older men and women: the English longitudinal study of ageing. Age Ageing 45:789–794
Brown J, Kurichi JE, **e D et al (2014) Instrumental activities of daily living staging as a possible clinical tool for falls risk assessment in physical medicine and rehabilitation. PM R 6:316–323
Sekaran NK, Choi H, Hayward RA et al (2013) Fall-associated difficulty with activities of daily living in functionally independent individuals aged 65 to 69 in the United States: a cohort study. J Am Geriatr Soc 61:96–100
Stenhagen M, Ekström H, Nordell E et al (2014) Both deterioration and improvement in activities of daily living are related to falls: a 6-year follow-up of the general elderly population study Good Aging in Skåne. Clin Interv Aging 9:18391846
Kojima R, Ukawa S, Ando M et al (2016) Association between falls and depressive symptoms or visual impairment among Japanese young–old adults. Geriatr Gerontol Int 16:384–391
Stewart Williams J, Kowal P, Hestekin H et al (2015) Prevalence, risk factors and disability associated with fall-related injury in older adults in low- and middle-income countries: results from the WHO Study on global AGEing and adult health (SAGE). BMC Med 13:147
Holtzer R, Verghese J, Xue X et al (2006) Cognitive processes related to gait velocity: results from the Einstein aging study. Neuropsychology 20:215–223
Callisaya ML, Ayers E, Barzilai N et al (2016) Motoric cognitive risk syndrome and falls risk: a multi-center study. J Alzheimers Dis 53:1043–1052
Landi F, Liperoti R, Russo A et al (2012) Sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr 31:652–658
Tanimoto Y, Watanabe M, Sun W et al (2014) Sarcopenia and falls in community-dwelling elderly subjects in Japan: defining sarcopenia according to criteria of the European working group on sarcopenia in older people. Arch Gerontol Geriatr 59:295–299
Benjumea A-M, Curcio C-L, Duque G et al (2018) Dynapenia and sarcopenia as a risk factor for disability in a falls and fractures clinic in older persons. Open Access Maced J Med Sci 6:344–349
Bijlsma AY, Pasma JH, Lambers D et al (2013) Muscle strength rather than muscle mass is associated with standing balance in elderly outpatients. J Am Med Dir Assoc 14:493–498
Soysal P, Ates Bulut E, Yavuz I et al (2018) Decreased basal metabolic rate can be an objective marker for sarcopenia and frailty in older males. J Am Med Dir Assoc S1525–8610:30362-1
Samper-Ternent R, Karmarkar A, Graham J et al (2012) Frailty as a predictor of falls in older Mexican Americans. J Aging Health 24:641–653
Deandrea S, Lucenteforte E, Bravi F et al (2010) Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology 21:658–668
Reed-Jones RJ, Solis GR, Lawson KA et al (2013) Vision and falls: a multidisciplinary review of the contributions of visual impairment to falls among older adults. Maturitas 75:22–28
Jiam NTL, Li C, Agrawal Y (2016) Hearing loss and falls: a systematic review and meta-analysis. Laryngoscope 126:2587–2596
Bloch F, Thibaud M, Tournoux-Facon C et al (2013) Estimation of the risk factors for falls in the elderly: can meta-analysis provide a valid answer? Geriatr Gerontol Int 13:250–263
Siddiqui NY, Levin PJ, Phadtare A et al (2014) Perceptions about female urinary incontinence: a systematic review. Int Urogynecol J 25:863–871
Padmanabhan P, Dmochowsi R (2014) Urinary incontinence in women: a comprehensive review of the pathophysiology, diagnosis and treatment. Minerva Ginecol 66:469–478
Soliman Y, Meyer R, Baum N (2016) Falls in the elderly secondary to urinary symptoms. Rev Urol 18:28–32
Bresee C, Dubina ED, Khan AA et al (2014) Prevalence and correlates of urinary incontinence among older community-dwelling women. Female Pelvic Med Reconstr Surg 20:328–333
Bates DW, Pruess K, Souney P et al (1995) Serious falls in hospitalized patients: correlates and resource utilization. Am J Med 99:137–143
Vu T, Finch CF, Day L (2011) Patterns of comorbidity in community-dwelling older people hospitalised for fall-related injury: a cluster analysis. BMC Geriatr 11:45
Ng CT, Tan MP (2013) Osteoarthritis and falls in the older person. Age Ageing 42:561–566
Khalaj N, Osman NAA, Mokhtar AH et al (2014) Balance and risk of fall in individuals with bilateral mild and moderate knee osteoarthritis. PLoS ONE 9:e92270
Chau RMW, Ng TKW, Kwan RLC et al (2013) Risk of fall for people with diabetes. Disabil Rehabil 35:1975–1980
Kachroo S, Kawabata H, Colilla S et al (2015) Association between hypoglycemia and fall-related events in Type 2 diabetes mellitus: analysis of a U.S. commercial database. J Manag Care Spec Pharm 21:243–253
Zia A, Kamaruzzaman SB, Tan MP (2015) Polypharmacy and falls in older people: balancing evidence-based medicine against falls risk. Postgrad Med 127:330–337
Richardson K, Bennett K, Kenny RA (2015) Polypharmacy including falls risk-increasing medications and subsequent falls in community-dwelling middle-aged and older adults. Age Ageing 44:90–96
Author information
Authors and Affiliations
Contributions
OD performed data collection and manuscript writing; SKO and AEA contributed to data collection; IY conducted data analysis; LS performed manuscript writing; PS designed the study and performed manuscript writing; and ATI designed the study and supported manuscript writing and conceptualism.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
All participants provided informed consent prior to their participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dokuzlar, O., Koc Okudur, S., Smith, L. et al. Assessment of factors that increase risk of falling in older women by four different clinical methods. Aging Clin Exp Res 32, 483–490 (2020). https://doi.org/10.1007/s40520-019-01220-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01220-8