Abstract
Purpose
To determine the relationship between family uncertainty and family quality of life (QOL) during the recovery period of patients with cerebrovascular disease in Japan, and the factors that influence family uncertainty.
Methods
Data were collected from copies of patient medical files and interviews with family members of 85 patients admitted to two rehabilitation wards in Japan. Family uncertainty was measured using the Japanese version of the Managing Uncertainty in Illness Scale–Family Member form (MUIS-FM) and family QOL using the World Health Organization Five Well-Being Index (WHO-5). Multiple linear regression analysis was applied to investigate associated factors.
Results
WHO-5 score was significantly negatively associated with MUIS-FM score (β = − 0.236, p = 0.03); other factors associated with MUIS-FM score were the Care Shared Decision-Making Questionnaire for care providers score (β = − 0.384, p < 0.001), Short Intolerance of Uncertainty Scale score (β = 0.296, p = 0.001), and history of surgical treatment (β = 0.199, p = 0.032).
Conclusions
Family QOL could be improved by reducing family uncertainty. It is also suggested that promoting shared decision-making between healthcare providers and patients’ families may help reduce family uncertainty. It is necessary to take into account not only family intolerance of uncertainty but also uncertainty that varies by type of acute care provided.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Illness uncertainty among family caregivers of patients is gaining increasing attention. Uncertainty about illness is defined as “the inability to determine the meaning of illness-related events” [1] and is “a cognitive state created when the person cannot adequately structure or categorize an event because of the lack of sufficient cues” [1]. The family’s educational level, their relationship with the patient, and the patient’s medical condition are known to affect the family’s perceived level of uncertainty [2,3,4], which leads to anxiety, stress, and a care burden [5, 6]. Qualitative studies on the impact on family quality of life (QOL) indicated that various uncertainties that arise during the recovery process caused family distress [7] and lower psychological well-being [8,9,10]. Lowering families’ uncertainty is important in maintaining favorable outcomes for their QOL and life satisfaction.
Stroke is a serious disease that, once it occurs, not only greatly affects the lives of patients and their families by bringing in a variety of uncertainty [6, 7] and psychological stress [11,12,13] but also imposes an economic burden on society. In Japan, it is estimated that more than half of stroke patients will die within 1 month or require long-term care [14, 15]. According to government statistics in 2019, stroke, heart disease, and other cardiovascular diseases accounted for the largest share of healthcare costs (19.2% of the total) and were responsible for increasing healthcare and long-term care costs [16]. The psychological stress experienced by families of stroke patients has been reported to limit family members’ social activities [17] and further reduce their ability to care for the patient [18]. These effects have been reported to last for weeks or even longer periods during the recovery from stroke and following rehabilitation [19, 20]. Because family members play an important role in the patient’s recovery process, including acceptance of disability prognosis and rehabilitation [21, 22], it is important that healthcare providers understand and appropriately address the psychosocial impact of the family as well as the patient [23,24,25].
Uncertainty theory presents a model in which an individual’s perception and evaluation of uncertainty influences co** behavior, which in turn influences outcomes such as the individual’s QOL [1]. This QOL among families as the main caregivers has significant implications for the disease management and outcomes for patients in recovery and beyond [26, 27]. The conceptual model has led to studies on illness uncertainty and also on QOL among patients’ families in Western countries [28, 29]. However, such evidence is scarce in Japan, not to mention data focusing on family members of patients with cerebrovascular disease during the recovery period. Therefore, the purpose of this study was, first, to investigate the relationship between family uncertainty and QOL during the recovery period of patients with cerebrovascular disorders in Japan and, second, to investigate the factors that influence their family members’ uncertainty.
Methods
Study design and participants
This was a cross-sectional study conducted from March to December, 2021. Participants were family members of patients hospitalized at two rehabilitation wards in the northern region, who met the following selection criteria: 1) Patients had cerebrovascular diseases (including cerebral infarction, cerebral hemorrhage, subarachnoid hemorrhage, traumatic brain injury, brain tumor, and others) and had been in the rehabilitation wards for less than two weeks; 2) Both patients and their family members were adults aged 20 years or older, and the family members were assessed by the attending physician and the ward supervising nurse to be cognitively competent to participate in the study; 3) Patients’ family members were the primary caregivers of the patient.
Survey items
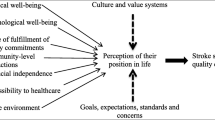
Data were collected by in-person interviews (by the first author) using anonymous questionnaires and transcription of medical records. The survey questionnaire was constructed to follow the conceptual framework shown in Fig. 1 constructed in reference to the uncertainty theory [1].
As the main indicator of interest in the present study, family uncertainty was assessed by the Japanese version of the Managing Uncertainty in Illness Scale–Family Member form (MUIS-FM) [30]. The MUIS-FM measures the extent to which family members caring for a patient perceive uncertainty about the patient’s illness and treatment. The measure consists of 31 questions with 11 reverse items, and answer options are on a five-point scale ranging from “strongly disagree” (1) to “strongly agree” (5). The total score ranges from 31 to 155, with a higher score indicating a greater family uncertainty. Permission to use this scale was obtained from the developer of the Japanese version [30].
To assess the family’s QOL, we used the World Health Organization Five Well-Being Index (WHO-5) [31]. The WHO-5 is widely used to assess subjective psychological well-being and is also used as a screening method for depression. It consists of five questions asking one’s mood state in daily life, and answer options are on a six-point scale ranging from 0 to 5. The total score ranges from 0 to 25, with a higher score indicating a better QOL. A score less than 13 is defined as screen positive for depression [31].
As background factors possibly related to family uncertainty, the following items were investigated: shared decision-making, uncertainty intolerance, and social support. The Japanese version of the Care Shared Decision-Making (SDM) Questionnaire for care providers [32] was used to evaluate shared decision-making cognition with healthcare providers. The measurement consists of nine items, each of which is rated on a six-point scale ranging from “not at all applicable” (0) to “very applicable” (5). The total maximum score is 45 and a higher score indicates a higher level of cognition of shared decision-making. Cronbach’s alpha coefficient was 0.92 in this study. The Short Intolerance of Uncertainty Scale Japanese version [33] (SIUS) was used to evaluate one’s tendency to react to uncertain situations. The SIUS consists of 12 items, each of which is rated on a five-point scale ranging from “not at all applicable” (1) to “very applicable” (5). The total maximum score is 60 and a higher score indicates higher uncertainty intolerance. Cronbach’s alpha coefficient was 0.90 in this study. The Japanese version of the Social Support Scale (SS) [34] was used to evaluate families’ perceived level of social support. The measurement consists of 12 items, each of which is rated on a seven-point scale ranging from “strongly disagree” (1) to “strongly agree” (7). The total maximum score is 84, and a higher score indicates higher social support. The Cronbach alpha coefficient was 0.94 in this study.
Other basic family attributes included age, gender, education, relationship to the patient, whether or not they live with the patient, prior caregiving experience, income, health literacy level, degree of anxiety toward COVID-19, and existence of a future care plan. The patient’s medical information included age, gender, frequency of onset, treatment type (medical or surgical), disease diagnosis, level of consciousness (Japan Coma Scale; JCS), functional independence level (Functional Independence Measure; FIM), and the number of days from the onset of illness to admission to the rehabilitation ward. The family member’s degree of anxiety toward COVID-19 was assessed against four answer options: not at all worried, slightly worried, very worried, and very worried and horrified. The former two and latter two answers were classified as low anxiety and high anxiety, respectively. The family member’s health literacy level was assessed by asking about confidence in completing a medical form with a five-point scale ranging from “not confident at all” (1) to “very confident” (5). A five-point answer was classified as a high health literacy level, and answers of four points or lower were classified as a low health literacy level.
Statistical analysis
Our analysis followed the conceptual framework shown in Fig. 1. First, univariate analyses were performed to assess factors associated with MUIS-FM and WHO-5 scores (Tables 1 and 2). T test or one-way ANOVA was used for categorical variables and Pearson’s correlation coefficient for continuous variables. Second, the association between the MUIS-FM and WHO-5 scores was examined using multiple regression analysis by entering WHO-5 score as a dependent variable, MUIS-FM score as the main independent variable of interest, and items that were associated with both (p value less than 0.1) as covariates (Table 3). Third, multiple regression analysis was performed to investigate factors associated with MUIS-FM score. We entered MUIS-FM score as the dependent variable and items that were associated at the level of a p value less than 0.1 in univariate analyses (Table 4). Our purpose was to explore factors associated with the main outcome, and the significance level in the univariate analysis was, therefore, set at a p value of less than 0.1 rather than the conventionally used 0.01. The statistical software SPSS Statistics 28.0 for Windows (IBM Corp., Armonk, NY, USA) was used.
Ethical considerations
This study was approved by the Ethics Committee of Fukushima Medical University (No. General 2020–277). We also obtained approvals from study sites. After an oral explanation of the study, receiving answers on survey sheets was considered as obtaining consent from family members. As for collecting medical information from patients, written consent was obtained. In case a patient was unable to give written consent due to health problems, proxy consent was obtained from a family member.
Results
Basic characteristics of family and patients (Table 1 and Table 2)
A total of 85 participants were included in the analysis, excluding three who declined to participate in the survey and one who was not eligible. The most common age group of family members was 50–69 years (n = 50, 58.8%), and 48 (56.5%) were women. In terms of relationships, 48 (56.5%) were a child of the patient. The mean SIUS score was 34.8 (SD 8.5), the mean SS score 65.2 (SD 12.9), and the mean SDM score 33.5 (SD 7.6). As for patients, 36 (42.4%) were aged 70–79 years, and 43 (50.6%) were women. Seventy-one (83.5%) were first-onset, cerebral infarction was the most common disease diagnosis in 52 patients (61.2%), and 67 (78.8%) did not undergo surgery. Sixty-nine patients (81.2%) had impaired consciousness, the mean FIM total score was 56.7 (SD 23.9), and the mean number of days from onset of illness to admission to recovery rehabilitation was 27.9 (SD 21.0).
The MUIS-FM, assessing family uncertainty and with Cronbach’s alpha coefficient of 0.89 among the study participants, had a mean score of 87.5 (SD 15.1). Univariate analysis showed that it was associated (at the level of p value less than 0.1) with income (p = 0.08), existence of a future care plan (p = 0.01), SIUS score (Pearson Correlation Coefficient r = 0.29, p = 0.01), SDM score (r = − 0.43, p = 0.001), and history of surgical treatment (p = 0.02). The WHO-5 score, assessing family QOL and with Cronbach’s alpha coefficient of 0.86 among the study participants, had a mean score of 11.3 (SD 4.9); 51 (60%) had a score less than 13, which is screen positive for depression. Univariate analysis showed that it was associated (at the level of p value less than 0.1) with the family member’s relationship to the patient (p = 0.03), SIUS score (r = − 0.21, p = 0.05), SS score (r = 0.23, p = 0.04), and MUIS-FM score (r = − 0.28, p = 0.01). Sub-analyses limiting subjects to those with first-ever stroke and cerebral infarction (supplementary tables) showed similar results.
Association of family uncertainty with QOL (Table 3)
The variable associated with both MUIS-FM and WHO-5 scores was SIUS score in the above univariate analyses. We thus considered the item as a potential confounder, which was adjusted for in the multivariable analysis, and found that MUIS-FM score was significantly associated with WHO-5 score (β = − 0.236, p = 0.03).
Factors associated with family uncertainty (Table 4 )
Multivariable regression analysis to assess factors associated with the MUIS-FM score showed that a lower SDM score (β = − 0.384, p < 0.001), a higher SIUS score (β = 0.296, p = 0.001), and not undergoing surgical treatment (β = 0.199, p = 0.032) were factors associated with the MUIS-FM score, and the SDM score had the highest absolute value of β.
Discussion
Our results obtained among family members of patients with cerebrovascular disease in the recovery period showed that family uncertainty was negatively correlated with family QOL, and that the factor most strongly associated with family uncertainty was the degree of shared decision-making with healthcare providers. Other associated factors were families’ intolerance to uncertainty and patients’ surgical treatment.
The mean MUIS-FM score for family uncertainty in this subject was 87.5 (SD 15.1). This was higher than the mean scores of 77.2 (15.3) and 78.9 (11.5) reported by an Australian study targeting families of patients admitted to intensive care units treating a variety of illnesses [3]. It was also slightly higher than the mean scores of 83.7 (23.4) and 85.8 (17.6) reported for families of patients with acute brain diseases in Japan and the United States, respectively [4, 30]. Furthermore, a similar study [4] measured the level of uncertainty in families of stroke patients at two time points and reported that they experienced high levels of uncertainty approximately 2 weeks after the onset, which remained after 4 weeks. Similarly in our study, patients were admitted to a rehabilitation ward approximately 1 month (mean 28 days) after the disease onset, and their families showed a high level of uncertainty.
The WHO-5 score, indicating family QOL, had a mean of 11.3 (SD 4.9), which was lower than a previously reported score of 15.3–17.9 (6.9–5.6) for men and 15.9–17.4 (6.1–5.7) for women with varying numbers among different age groups in community-dwelling older people in Japan [35]. In addition, 60% of the participants had a score of 13 or less, which indicates low mental health status. The results suggest that healthcare providers need to pay attention to the QOL and mental health of families when caring for patients with cerebrovascular diseases in recovery.
We then examined whether family uncertainty is associated with family QOL, and confirmed that the higher the uncertainty, the lower the QOL. In other words, it might be possible that family QOL could be improved by decreasing the uncertainty experienced by family members during the recovery period. This result is consistent with a previous study of families of heart failure patients reporting that the level of family uncertainty is important in the favorable outcomes of family QOL and life satisfaction [36].
When exploring factors underpinning family uncertainty, we found that the degree of their perceived shared decision-making with healthcare providers was a primary associated factor. Charles and colleagues listed four key characteristics of the shared decision-making process: namely, both physician and patient being involved, sharing information, building a consensus on the preferred treatment, and reaching an agreement on the treatment to implement [37]. Providing quality information on choices and facilitating the making of a decision can promote individual initiative [38]. Healthcare providers are seen as reliable sources of information, and trusted providers can give meaning to illness-related events and reduce uncertainty as individuals advance their interpretation of events [1]. We suggest that both patients and families should be involved in this process of shared decision-making.
In Japan, the Basic Plan for the Promotion of Measures against Cardiovascular Diseases was developed based on the Basic Act on Measures against Stroke, Heart Disease, and Other Cardiovascular Diseases (2019) to extend healthy life expectancy [39]. To improve medical service quality and efficiency [40, 41], the rehabilitation flow in stroke care is divided into acute, recovery, and maintenance phases [41]. Most patients transition from acute care facilities to rehabilitation wards and then to their homes or facilities [42]. The recovery period is, therefore, a critical stage in which the importance of communication with the multidisciplinary team must be emphasized for providing information and discussing care plans [42]. Patients and families are briefed about their future life with emphasis on rehabilitation after treatment in the acute phase. Therefore, it is essential to consider patients’ and families’ wishes and values through shared decision-making [43]. Of note in our study, uncertainty intolerance was identified as one of the factors related to family uncertainty. Individuals who exhibit high uncertainty intolerance accordingly rate uncertainty as more threatening [44], which possibly in turn causes higher uncertainty. Close communication with family members is, therefore, necessary to ensure careful management that responds to their individual characteristics and tolerance levels toward uncertainty.
Despite the obvious importance, a review on the shared decision-making indicated that the level of patient and family involvement is insufficient [45]. More efforts are needed to build a trust relationship, provide information, and allow individuals to express their views [38]. In relation, it was reported that patients and their families in the stroke rehabilitation phase lacked knowledge and had to seek out accurate information from healthcare providers [46]. The need for information and communication is especially high when transitioning from the acute to the recovery phase; the patient’s condition and physical and mental health change markedly and the need for family involvement increases [47]. In the present study, 81% of the patients presented with impaired consciousness, and it was inferred that family members had limited information available from the patients themselves. Direct information sharing and interactive communication with healthcare providers during the recovery period would play an important role in reducing family uncertainty.
Another clinical factor that influenced family uncertainty was the treatment type. Families of patients with no surgical treatment had significantly higher levels of perceived uncertainty. This was similar to a previous study, conducted among parents of hospitalized children, which reported significantly different total uncertainty scores when comparing parents in the medical and surgical treatment groups [48]. Parents in the medical group were less able to picture children’s symptoms and treatment, felt obtained information was insufficient, and experienced a greater sense of unpredictability than parents in the surgical group. This might also be the case among our study participants. Therefore, uncertainty management among families requires different approaches depending on the content of treatment in the acute phase.
This study had several methodological limitations. First, our sample size was small and participants were recruited from two medical facilities in one region of Japan. Further studies with an increased sample size from different regions are needed to confirm the generalizability of the obtained results. We should note, however, that the internal validity of the results on factors associated with family uncertainty could be considered high because researchers carefully collected information through in-person interviews. Second, the cross-sectional nature of the study made it difficult to determine causal relationships among associations between variables. Confirmation through longitudinal studies or family intervention studies is needed. Third, the survey was conducted during the COVID-19 pandemic. Although we confirmed that the level of anxiety toward COVID-19 was not associated with family uncertainty or QOL, the way in which medical services were provided differed from the normal setting, and this might have influenced our results. Fourth, the survey covered a broad range of cerebrovascular diseases of varying severity. Further studies with larger samples are needed to clarify whether there are significant differences by disease and severity. Fifth, the number of survey items was limited for practical reasons, and, therefore, some attributes were assessed using unvalidated measures. In particular, more robust, validated instruments should be used to look in detail at health literacy level and degree of anxiety toward COVID-19.
Conclusion
Our study among families of patients with cerebrovascular disease in Japan showed that they had a high level of uncertainty, which was associated with their low QOL. Background factors associated with family uncertainty were threefold: namely, family members’ personality traits (intolerance to uncertainty), communication with healthcare providers (shared decision-making), and patients’ treatment types (medical or surgical). Sharing information and interactive communication with patients’ families is important in reducing their uncertainty, and special attention is needed when the patient is treated medically without surgery or when the family member seems intolerant to uncertainty.
References
Mishel MH (1988) Uncertainty in illness. Image J Nurs Sch 20:225–232
Liu J, Liu Q, Huang Y et al (2020) Effects of personal characteristics, disease uncertainty and knowledge on family caregivers’ preparedness of stroke survivors: a cross-sectional study. Nurs Health Sci 22:892–902
Mitchell ML, Courtney M (2004) Reducing family members’ anxiety and uncertainty in illness around transfer from intensive care: an intervention study. Intensive Crit Care Nurs 20:223–231
Byun E, Riegel B, Sommers M et al (2016) Caregiving immediately after stroke: a study of uncertainty in caregivers of older adults. J Neurosci Nurs 48:343–351
Harkness K, Arthur H, McKelvie R (2013) The measurement of uncertainty in caregivers of patients with heart failure. J Nurs Meas 21:23–42
Byun E, Riegel B, Sommers M et al (2017) Effects of uncertainty on perceived and physiological stress in caregivers of stroke survivors: a 6-week longitudinal study. J Gerontol Nurs 43:30–40
McCurley JL, Funes CJ, Zale EL et al (2019) Preventing chronic emotional distress in stroke survivors and their informal caregivers. Neurocrit Care 30:581–589
Greenwood N, Mackenzie A, Wilson N et al (2009) Managing uncertainty in life after stroke: a qualitative study of the experiences of established and new informal carers in the first 3 months after discharge. Int J Nurs Stud 46:1122–1133
White CL, Barrientos R, Dunn K (2014) Dimensions of uncertainty after stroke: perspectives of the stroke survivor and family caregiver. J Neurosci Nurs 46:233–240
Katbamna S, Manning L, Mistri A et al (2017) Balancing satisfaction and stress: carer burden among white and british asian indian carers of stroke survivors. Ethn Health 22:425–441
Shaffer KM, Riklin E, Jacobs JM et al (2016) Mindfulness and co** are inversely related to psychiatric symptoms in patients and informal caregivers in the neuroscience ICU: implications for clinical care. Crit Care Med 44:2028–2036
Loh AZ, Tan JS, Zhang MW et al (2017) The global prevalence of anxiety and depressive symptoms among caregivers of stroke survivors. J Am Med Dir Assoc 18:111–116
Byun E, Evans L, Sommers M et al (2019) Depressive symptoms in caregivers immediately after stroke. Top Stroke Rehabil 26:187–194
Ministry of Health, Labour and Welfare: Comprehensive Survey of Living Conditions. https://www.mhlw.go.jp/toukei/list/20-21.html (accessed January 29, 2022)
Takashima N, Arima H, Kita Y et al (2017) Incidence, management and short-term outcome of stroke in a general population of 1.4 Million Japanese-Shiga Stroke Registry-. Circ J 81:1636–1646
Ministry of Health, Labour and Welfare: Estimates of National Medical Care Expenditure. https://www.mhlw.go.jp/toukei/list/37-21.html (accessed January 29, 2022)
Jellema S, Wijnen MAM, Steultjens EMJ et al (2019) Valued activities and informal caregiving in stroke: a sco** review. Disabil Rehabil 41:2223–2234
Bakas T, Burgener SC (2002) Predictors of emotional distress, general health, and caregiving outcomes in family caregivers of stroke survivors. Top Stroke Rehabil 9:34–45
Greenwood N, Mackenzie A (2010) An exploratory study of anxiety in carers of stroke survivors. J Clin Nurs 19:2032–2038
Watanabe Y, Araki S, Kurihara M (2003) Preliminary results of providing information to stroke family carers how their psychological distress may change during the first 3 months following stroke. Jpn J Rehabil Med 40:848–857
O’Connell B, Baker L (2004) Managing as carers of stroke survivors: strategies from the field. Int J Nurs Pract 10:121–126
Lou S, Carstensen K, Jørgensen CR et al (2017) Stroke patients’ and informal carers’ experiences with life after stroke: an overview of qualitative systematic reviews. Disabil Rehabil 39:301–313
McCullagh E, Brigstocke G, Donaldson N et al (2005) Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke 36:2181–2186
Grant JS, Clay OJ, Keltner NL et al (2013) Does caregiver well-being predict stroke survivor depressive symptoms? a mediation analysis. Top Stroke Rehabil 20:44–51
King RB, Hartke RJ, Houle TT (2010) Patterns of relationships between background characteristics, co**, and stroke caregiver outcomes. Top Stroke Rehabil 17:308–317
Zhao J, Zeng Z, Yu J et al (2021) Effect of main family caregiver’s anxiety and depression on mortality of patients with moderate-severe stroke. Sci Rep. https://doi.org/10.1038/s41598-021-81596-8
Em S, Bozkurt M, Caglayan M et al (2017) Psychological health of caregivers and association with functional status of stroke patients. Top Stroke Rehabil 24:323–329
Sammarco A (2001) Perceived social support, uncertainty, and quality of life of younger breast cancer survivors. Cancer Nurs 24:212–219
Fortier MA, Batista ML, Wahi A et al (2013) Illness uncertainty and quality of life in children with cancer. J Pediatr Hematol Oncol 35:366–370
Iizuka M, Mizuno M (2014) Investigation of the reliability and validity of the Japanese Version of the Managing Uncertainty in Illness Scale-Family Member Form. J Jpn Acad Nurs Sci 34:245–254
Awata S, Bech P, Koizumi Y et al (2007) Validity and utility of the Japanese version of the WHO-Five Well-Being Index in the context of detecting suicidal ideation in elderly community residents. Int Psychogeriatr 19:77–88
Goto Y, Yamaguchi Y, Onishi J et al (2021) Adapting the patient and physician versions of the 9-item shared decision making questionnaire for other healthcare providers in Japan. BMC Med Inform Decis Mak 21:314
Takebayashi Y, Sasagawa S, Sugiura Y (2012) Development and validation of the Japanese Version of the Short Intolerance of Uncertainty Scale. Jpn J T 5:179–187
Iwasa H, Gondo Y, Masui Y et al (2007) Nihongoban“sosharu’sapotoshakudo”noshinraiseinarabinidatosei-chukonenshawotaishotoshitakento. [Reliability and validity of the Japanese Version of the “Social Support Scale” -A Study for Middle-aged and Elderly People]. J Health Welf Statist 54:26–33
Iwasa H, Gondo Y, Masui Y et al (2007) Nihongoban“WHO-5seishintekikenkojotaihyo”noshinraiseinarabinidatosei-chiikikoreishawotaishotoshitakento. [Reliability and validity of the Japanese Version of “WHO-5 Mental Health Status Table” -A Study for the Elderly in the Community]. J Health Welfare Statist 54:48–55
Nauser JA, Bakas T, Welch JL (2011) A new instrument to measure quality of life of heart failure family caregivers. J Cardiovasc Nurs 26:53–64
Charles C, Gafni A, Whelan T (1997) Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med 44:681–692
Elwyn G, Frosch D, Thomson R et al (2012) Shared decision making: a model for clinical practice. J Gen Intern Med 27:1361–1367
Ministry of Health, Labour and Welfare: Japanese National Plan for Promotion of Measures Against Cerebrovascular and Cardiovascular Disease. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/kenkou/jyunkanki/index.html?msclkid=095d1984cf7411ec906a257ae2d9f20d (accessed February 24, 2022)
Ministry of Health, Labour and Welfare: The Comprehensive Reform of Social Security and Tax. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hokabunya/shakaihoshou/kaikaku.html (accessed January 29, 2022)
Ministry of Health, Labour and Welfare: Community-based Integrated Care System. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hukushi_kaigo/kaigo_koureisha/chiiki-houkatsu/ (accessed January 29, 2022)
Kaifukuki Rehabilitation Ward Association. Publications. http://www.rehabili.jp/publications/download.html (accessed January 29, 2022)
Shay LA, Lafata JE (2015) Where is the evidence? a systematic review of shared decision making and patient outcomes. Med Decis Making 35:114–131
Ladouceur R, Talbot F, Dugas MJ (1997) Behavioral expressions of intolerance of uncertainty in worry expressions findings. Behav Modif 21:355–371
Couët N, Desroches S, Robitaille H et al (2015) Assessments of the extent to which health-care providers involve patients in decision making: a systematic review of studies using the OPTION instrument. Health Expect 18:542–561
Stein J, Shafqat S, Doherty D et al (2003) Family member knowledge and expectations for functional recovery after stroke. Am J Phys Med Rehabil 82:169–174
Bulsara C, Saunders R, Emery L et al (2021) Reflecting on experiences of care: an exploratory qualitative descriptive study of the perspectives of stroke survivors, families and staff. BMJ Open 11:e047559-047559
Mishel MH (1983) Parents’ perception of uncertainty concerning their hospitalized child. Nurs Res 32:324–330
Acknowledgements
The authors thank subjects who responded to the survey and all of the medical professionals who assisted us in this study or their contribution towards implementing the project. We also thank Oliver Stanyon for editing a draft of this manuscript.
Funding
This work was supported by JSPS KAKENHI grant number JP20H04354.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
This study was approved by the Ethics Committee of Fukushima Medical University (No. General 2020–277), and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki. We also obtained approvals from study sites.
Informed consent
After an oral explanation of the study, receiving answers on survey sheets was considered as obtaining consent from family members. As for collecting medical information from patients, written consent was obtained. In case a patient was unable to give written consent due to health problems, proxy consent was obtained from a family member.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Honda, K., Murakami, M., Takebayashi, Y. et al. Uncertainty among families of patients with cerebrovascular diseases in Japan: association with quality of life and background characteristics. Aging Clin Exp Res 34, 3097–3105 (2022). https://doi.org/10.1007/s40520-022-02254-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02254-1