Abstract
Obesity is an important risk factor for cardiovascular diseases (CVDs). It is crucial to understand the impact of its duration due to the more extended exposure period and the higher frequency of overweight/obesity at younger ages. In the last decade, various studies have discovered that the duration of obesity, in addition to its severity, might have an impact. Therefore, this study aimed to summarize the current literature to investigate the effect of body mass index (BMI) trajectories and overweight/obesity duration on cardiovascular outcomes. To retrieve related articles, we searched PubMed, EMBASE, Google Scholar, Web of Science, Scopus, and Cochrane electronic databases. The duration of overweight/obesity is significantly associated with CVDs, especially heart failure and atrial fibrillation. However, there are contradictory results regarding the association between coronary heart disease and stroke with the duration of obesity. Additionally, no association with peripheral vascular disease has yet to be reported. The absence of this association may be brought on by covariates or various follow-up times. Nevertheless, it seems that both stable overweight and remarkably stable obesity increase the risk of CVDs, as does both stable overweight and notably stable obesity. Metrics showing both the severity and the duration of overweight/obesity are more effective than each alone, and it is recommended to be used for assessing the risk of various CVDs. There are few studies in these areas, and studies with more extended follow-up periods, with a wide age range, while adjusting for some specific covariates, are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cardiovascular diseases, heart failure, and atrial fibrillation are significantly associated with the duration of overweight/obesity. |
There are contradictory results regarding the association between coronary heart disease and stroke with the duration of overweight/obesity. |
There is no association between peripheral vascular disease and the duration of overweight/obesity. |
Stable overweight and stable obesity trajectories increase the risk of cardiovascular diseases. |
Metrics showing both the severity and the duration of overweight/obesity are more effective than each alone, and it is recommended to be used for assessing the risk of various cardiovascular diseases. |
Introduction
Obesity is excessive fat accumulation usually defined by a body mass index (BMI) above 30 [1]. BMI is a simple calculation using a person's height and weight [2]. Although other methods such as waist circumference and central or peripheral adiposity are alternatives, BMI is the standard method for defining obesity [3]. BMI classifies into six categories, including underweight (< 18.5 kg/m2), normal range (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), obesity class I (30–34.9 kg/m2), obesity class II (35–39.9 kg/m2), and obesity class III (≥ 40 kg/m2) [4, 5]. Between 1975 and 2014, the global mean BMI increased from 21.7 to 24.2 kg/m2 in men and from 22.1 to 24.4 kg/m2 in women [6]. 3.28 billion adults will likely suffer from being overweight or obese by 2030 [7]. As obesity prevalence increases, obesity-related complications also start to grow, where one of these complications is cardiovascular outcome [8, 9]. Figure 1 shows pathophysiologic mechanisms linking obesity duration to cardiovascular diseases (CVDs). Obesity can accelerate the early raising of atherosclerotic lesions in the coronary arteries due to two main mechanisms: inflammation and insulin resistance [10]. The systemic and vascular inflammation caused by obesity increases the chance of low-density lipoprotein oxidation, and insulin resistance can lead to dyslipidemia. These mechanisms promote atherogenesis independent of other risk factors such as hypertension, dyslipidemia, or hyperglycemia [11]. In line with this issue, several studies have investigated the effect of obesity in increasing the risk of CVDs [4, 11,12,13]. A meta-analysis of 302,296 participants indicated that the adjusted relative risk for obesity compared with the normal range was 1.49 (95% CI, 1.32–1.67), and obesity accounts for an increased risk of CVDs [13]. However, considering the prevalence of obesity at younger ages and the longer exposure time, the duration of obesity or trajectories of BMI over time can play a critical role in the progression of CVDs [14]. The results of these studies were contradictory in that some did not statistically correlate the duration of obesity and cardiovascular events; in contrast, other studies found this significantly correlated [15, 16]. However, after adjusting with a series of covariates, the correlation in some studies became statistically insignificant [14]. In this review, we summarized the current literature to examine the effect of BMI trajectories or duration of overweight or obesity on cardiovascular events.
Methods
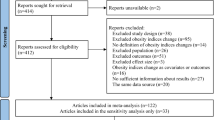
Two authors (R. A. and B. D.) searched PubMed, EMBASE, Google Scholar, Web of Science, Scopus, and Cochrane electronic databases for retrieving English articles published up to December 2022 using the combination of the following search terms (“length of obesity exposure” OR “trajectories of BMI” OR “long-term obesity” OR “overweight duration” OR “Cumulative obesity exposure” OR “BMI years” OR “Excess body mass index years” OR “excess weight duration” OR “obesity duration” OR “long-term obesity” OR “duration of obesity” OR “obese years” OR “trajectories of body mass index” OR “body mass index trajectories” OR “body mass index changes” OR “body mass index trends”) AND (“atrial fibrillation” OR “heart failure” OR “myocardial infarction” OR “acute coronary syndrome” OR “coronary heart disease death” OR “stroke” OR “transient ischemic attack” OR “peripheral arterial disease” Or “myocardial damage” OR “coronary heart disease” OR “cerebrovascular accident” OR “sudden cardiac death” OR “cardiovascular outcome”). We also screened the bibliographic references of relevant articles and existing reviews by hand-searching. Articles investigating the effect of BMI trajectories or duration of overweight or obesity on CVDs were selected (Table 1). We excluded non-human studies, conference papers and abstracts, erratums, commentaries, editorials, and studies that did not provide accurate and clear data or methods. Studies not reporting the weight change in BMI categories, articles regarding childhood obesity, and trajectories of BMI during childhood were also excluded. Resolution of disagreement was resolved by consensus and the third author's final decision (M. S.). The final selection of papers was made based on their relevance and confirmed by all authors. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Cardiovascular Disease
CVDs account for 31% of all global deaths, with an estimated 17.9 million deaths [17]. There is a well-established correlation between obesity and increased risk of CVD [18]; however, most findings are based on a single obesity measurement in the study follow-up time, like at the baseline [16]. This issue may not bring accurate results for various reasons. For instance, BMI and other measures of body composition are inconsistent risk factors for short-term (less than 10 years) cardiovascular outcomes in overweight and obese patients with CVD symptoms [19,20,21]. Regarding this epidemiological reverse, there is a term known as “the obesity paradox” that has been recently documented in various studies [19,20,21]. The obesity paradox's causative factors are unclear. The paradox may relate to possible lead time bias, which happens when overweight or obese patients develop CVDs earlier or are tested and diagnosed with CVDs earlier than normal-weight patients. As a result, these patients receive treatments earlier than normal-weight patients, which can lead to different outcomes [19]. Furthermore, independent of BMI, variations in cardiovascular fitness may account for better CVD outcomes [19]. Lastly, some claim there may be a “lean paradox” in which low body fat percentage, low BMI, and reduced capacity to prevent cardiac cachexia may be more significant indicators of poor CVD outcomes [19, 20]. According to that, recent studies have evaluated the potential cumulative effect of obesity on CVDs rather than a simple BMI at a point in time to measure the relation of obesity duration more accurately, and BMI changes as an independent factor in CVD [16].
In this regard, Abdullah et al. created a new metric called obese-years to determine CVD risk more effectively [16]. Obese-years was a combination of the level of obesity and the duration of obesity. In appearance, this metric is similar to another metric called excess BMI years [14]. However, the main difference between these two metrics is the baseline BMI, so that in obese-years, the reference BMI is reduced from 29, and in excess BMI years, from 25. Finally, in both metrics, these numbers have been multiplied by the number of years having excess BMI. This prospective cohort study was conducted in 2014 from the Framingham Heart Study on 5036 participants (24% obese) to study the association between obese-years metric and 10 obese-years with the risk of CVD [16]. The follow-up examinations were done each 2 years for 50 years. This study used three models, and model 3 included all previous models with additional adjustments. In this study, the risk of CVD significantly increases with an increase in the obese-years metric. Also, with every 10 obese-years, the adjusted hazard ratio (AHR) increases by 1.04 (95% CI 1.03–1.05). This study also estimated a more powerful effect of obese-years in males.
Furthermore, in 2015, Reis et al. conducted a longitudinal cohort from the CARDIA study on 4061 participants to study the effect of excess BMI-years on the incidence of CVD [14]. The follow-up examinations were done 2, 5, 7, 10, 15, 20, and 25 years after baseline. As the same as the analysis by Abdullah et al., this study analyzed excess BMI-years in two forms, as a continuous variable (per 50 excess BMI-years) and as a categorical variable, including five groups of BMI-years (i.e., 0, 1–49, 50–99, 100–149, and ≥ 150). The first model AHR for each additional 50 excess BMI-years and CVD was 1.20 (95% CI 1.08–1.34). This model adjusted for demographic and lifestyle variables. However, the second model, which adjusted for laboratory data, past medical history, and blood pressure variables, showed an AHR of 0.98 (95% CI 0.84–1.14), suggesting these factors as possible covariates.
Another way to evaluate the effect of time on the risk of CVD is by using BMI trajectories. In BMI trajectories, the course of BMI changes over time is examined. In 2021, Iyen et al. used this method [22]. In this population-based cohort study from the UK Clinical Practice Research Datalink (CPRD), 264,230 participants with BMI > 25 were followed for 2, 5, 8, and 10 years and overall CVD was measured. In this study, four trajectories were introduced, including the overweight-stable (overweight-S) group, obese class 1-stable (obese 1-S) group, obese class 2-stable (obese 2-S) group, and obese class 3-stable (obese 3-S) group. Finally, with increasing BMI and getting closer to the obese 3-S group, the unadjusted HR and the AHRs (adjusted model for age, sex, and comorbidities) increased. This increase was such that in the obese 3-S group, the risk increase reached 40% compared to the overweight-S group showing that individuals with stable severe obesity experience the most CVD outcomes.
With the same method, in 2020, Liu et al. suggested another BMI trajectory classification [23]. They introduced five trajectory groups, including stable normal (as the reference), maximum overweight, obese to non-obese, non-obese to obese, and stable obese. These groups were categorized by calculating BMI once in adults aged 40–79 years and then retrospectively BMI at the age of 25 or 10 years before baseline. The difference in BMI between these two groups led to the formation of these five groups. This study reported a significant association between maximum overweight and stable obese with the risk of CVD, which is increased by 1.4-fold and 2.32-fold, respectively. Although this study introduced helpful trajectory groups, since the exact duration of obese and non-obese years is unknown, we cannot rely so much on the AHR of obese to non-obese and non-obese to obese groups.
In addition to these studies, Dhana et al. evaluated the effects of BMI changes over time on the 10-year predicted risk of CVD [24]. This study examined three trajectories: stable weight, progressive weight gain, and progressive weight loss. Finally, after examinations every 4 years for 22 years on 6126 participants, the 10-year predicted risk of CVD increased in all three trajectories. However, the mean 10-year predicted risk of CVD was significantly higher in the group with progressive weight gain than in the group with stable weight.
As a result, according to the mentioned studies, increasing the duration of obesity along with higher BMI and gaining weight over time significantly correlate with an increased CVD risk. In the following, we will discuss each disease in the CVD subgroup, including coronary heart disease (CHD), heart failure (HF), stroke, peripheral vascular disease (PVD), and atrial fibrillation (AF) which was illustrated in Table 1.
Coronary Heart Disease
Obesity is an independent risk factor for CHD through multiple mechanisms, such as increased epicardial fat volume [4, 25]. However, whether weight histories and duration of obesity are also associated with increased risk of CHD is investigated by fewer studies. The results of included studies on the history of obesity and the risk of CHD are pretty controversial; included studies have demonstrated different results in various methodologies [15, 16, 22, 23, 26, 27]. The majority of included studies agreed with the association, although these were not homogeneous, and some results changed in favor of no association after adjusting for specific covariates [14, 28].
In this regard, in 2013, Reis et al. included 3275 Black and White men and women recruited from the CARDIA study from 1985 to 1986, with an average age of 25 [28]. The object of this study was to examine the association between both the presence and 10-year progression of coronary artery calcification (CAC) with the duration of overall obesity. CAC was investigated as a subclinical predictor of CHD. In the course of increasing years with obesity, both the AHRs and adjusted odds ratios (AORs), after adjusting for some factors, had a significant p value for trend, and the risk of presence and 10-year progression for CAC was 2% and 4% per year, respectively. Nevertheless, the association was no longer significant after adjusting for other time-varying variables.
Again in 2015, Reis et al. recruited participants from the CARDIA study to examine the excess BMI-years and per 50 excess BMI-years on the incidence of CHD [14]. As in the previous study, this association was initially significant, and the risk of CHD increased by 25% per 50 excess BMI-years. However, similarly, after adjusting for time-varying covariates, this association was no longer statistically significant. Following time-dependent variables, including antihypertensive and lipid-lowering medication, insulin, diabetes, and specific lab data such as total cholesterol, HDL-cholesterol, and triglycerides, were common covariates in Reis et al. studies. These findings suggest that there is no independent association between the duration of obesity and the risk of CHD, and it is due to the mentioned covariates.
Further, in 2018, Kabootari et al. conducted a study on 4398 participants over 40 years old [15]. This study investigated two factors, including cumulative excess weight (CEW) and general adiposity duration, to study the obesity duration effect. CEW was calculated as a time-weighted average of excess BMI > 25, and general adiposity duration shows the number of years with BMI > 25. Finally, the study did not report any significant association in all models of either sex.
Contrary to the mentioned studies, some studies have spoken in favor of the obesity duration and CHD risk association. Accordingly, in 2021, Calling et al. examined the risk of CHD in different BMI trajectories and 38-year continuous BMI using repeated follow-ups every 8 years [27]; 38-year continuous BMI showed an increase of 6% risk for CHD when BMI increased with almost perfect linearity between these two factors. Also, Abdullah et al. estimated a significant association between the risk of CHD and each additional 10 obese-years in all models and both sexes [16]. Finally, it was stated that per additional 10 obese-years, the risk of CHD increases by 3%.
BMI trajectories are another way of estimating the effect of BMI changes over time. Some individuals experience stable BMIs over time, including stable normal, stable overweight, and stable obese. On this matter, Calling et al. used the stable normal group as the reference [27]. This study stated that a stable overweight and stable obesity were associated with the risk of CHD with an AHR of 1.43 (95% CI 1.03–1.98) and 1.53 (95% CI 0.92–2.55), respectively. After merging stable overweight and stable obesity into one trajectory group, the AHR became 1.45 (95% CI 1.07–1.97). Additionally, Liu et al. showed a significant association between the stable obese group and the risk of CHD, heart attack, and angina pectoris [23]. In comparison with the stable normal group, this study estimated an AHRs of 2.96 (95% CI 1.80–4.89), 3.06 (95% CI 1.97–4.75), and 3.22 (95% CI 1.74–5.98) for the stable obese group, respectively. However, Iyen et al. considered the stable overweight group as the reference and estimated the AHR of 1.14 (95% CI 1.10–1.18), 1.13 (95% CI 1.09–1.18), and 1.06 (95% CI 0.99–1.16) for the risk of CHD in obese 1-S, obese 2-S, and obese 3-S groups, respectively [22]. Unlike the first two mentioned studies, Iyen et al. showed less severe results and even the loss of association in the obese 3-S group. This controversy could be due to the smaller number of participants and the more extended follow-up period of the first two studies or adjustments taken on comorbidities by the third study.
Regarding the same topic, Liu et al. also studied three conditions: CHD, heart attack, and angina pectoris [23]. The “obese to non-obese” group was not significantly associated with all three conditions. However, the “non-obese to obese” group was significantly associated with AHR of 2.42 (95% CI 1.74–3.37), 2.07 (95% CI 1.56–2.75), and 1.70 (95% CI 1.14–2.54), respectively. Also, the “maximum overweight” group was associated with all three conditions, with an AHRs of 1.71 (95% CI 1.29–2.26), 1.59 (95% CI 1.19–2.11), and 1.51 (95% CI 1.08–2.13), respectively. Finally, comparing “obese to non-obese” and “non-obese to obese” groups, and also the “stable overweight” and “stable obese” groups, it can be stated that in addition to obesity duration, obesity severity is an essential and dangerous factor.
Additionally, Choi et al. conducted a significant study on this topic [26]. In this study, 2,611,450 participants with a mean age of 34.5 years were followed for 10 years to study the association between BMI changes with acute myocardial infarction (AMI) and CHD among young adults. Similar to the previous studies, this study used the classic grou**s for BMI classification. However, the range of BMI for each group was different, so in this study, BMI < 23 was the normal weight group, 25 > BMI > 23 was the overweight group, and BMI > 25 was the obese group. Considering stable obesity as the reference group, if the BMI group decreases from the obese group to the overweight or normal group, the risk of AMI and CHD events significantly decreases in men. The greater the weight loss, the greater the risk decreases. However, this association did not differ statistically in women. Compared with stable overweight, shifting the BMI group from overweight to obese increases the risk of CHD in both men and women. Nevertheless, if the group changes from overweight to normal, there is no statistically significant change in CHD and AMI risk. On the other hand, in both sexes, compared with the stable normal group, becoming overweight or obese increases the risk of CHD and AMI statistically.
Finally, there are different opinions regarding the association between the duration of overweight/obesity and the risk of CHD. Studies have focused more on the simultaneous role of severity and duration of overweight/obesity, and a significant association has also been observed with these metrics. Also, it seems that stable obesity is the highest-risk condition for the incidence of CHD. In addition, a history of overweight/obesity or becoming overweight/obese over time has a significant risk of CHD. Nevertheless, some studies have stated no association. These differences could be due to the lack of long-term follow-up or the mentioned covariates, especially diabetes, antihypertensive and lipid-lowering medication, and laboratory factors such as total cholesterol, HDL cholesterol, and triglycerides. Considering these controversial results, studies with more extended follow-up periods while considering covariates should be done.
Heart Failure
HF epidemic features are changing, and the incidence is stabilized or even reduced in some populations; however, it is still a serious clinical problem due to its high prevalence and chronicity [29]. Risk factors play an important role in the incidence of HF [30]. One of these risk factors is obesity, which is rising in societies and can account for the increasing incidence of HF in younger people alarming an opposite trend [29]. Obesity can produce hemodynamic changes, cardiac morphology changes, and ventricular impairment particularly, LV diastolic function resulting in HF [31]. Recent research suggests that a higher BMI is more closely linked to the risk of HF with preserved ejection fraction (HFpEF) than HF with reduced EF (HFrEF) [32]. In fact, Pandey et al. found a stronger correlation between higher BMI and risk of HFpEF in a pooled analysis using data from three large longitudinal studies [33]. Participants with overweight and class I obesity had independent risks of HFpEF that were 38% and 56% higher than those without either condition [33]. This issue raises concerns about whether prolonged exposure to obesity can also increase the risk of incident HF. Various studies have been conducted, most of which agreed on the relation between long-term obesity and increased risk of HF.
In 2014, Reis et al. investigated the association between the duration of obesity and its effect on cardiac structure and function to highlight the burden of prolonged obesity on cardiac function using EF [34]. EF is a clinically useful marker for identifying underlying mechanisms and responses to treatment in HF patients [35]. The study was conducted on 2547 participants from CARDIA longitudinal cohort with various follow-ups and echocardiography at year 25 after baseline. The duration of obesity was calculated at every follow-up examination using a scoring methodology, and then the cumulative duration of overall obesity was calculated. The duration of overall obesity showed a significant relation with lower EF with a p-trend of 0.05. However, after additional adjustments for antihypertensive drugs, pulse rate, diabetes, and blood pressure, the p-trend changed to 0.07, indicating a minimal effect on this association. Each 5 years of overall obesity was associated with a 0.3% lower EF.
In another study by Reis et al. in 2015, the rate of HF per 1000 person-years was higher in participants with more exposure to excess BMI-years, and for each additional 50 excess BMI-years, the risk of HF increased by 32% [14]. Likewise, Abdullah et al. evaluated the influence of obese-years and estimated a 4% increase in the risk of HF with each 10-unit increase in obese-years in the total population [16]. This association was also significant in the males and females group. Similarly, the incident rates were higher in patients exposed to more obese-years.
On the contrary, the TLGS study from Iran did not find an association between CEW or general adiposity duration with the risk of HFrEF [15]. However, it is worth mentioning that this study had a shorter follow-up period compared to previous studies, while HF requires a longer follow-up time for diagnosis due to its chronic nature. Also, this study was conducted only on a sample of people in one city in Iran (Tehran), and anthropometric measurements were not complete for all the participants.
Iyen et al. conducted a study on the severity of long-term obesity and compared three trajectory groups (obese 1-S, obese 2-S, and obese 3-S) with overweight-S [22]. All three groups had a significantly higher risk of incident HF than the overweight-S group, with the highest incident rate in the obese 3-S group. Also, the risk of HF was 3.3-fold higher in this group. Furthermore, Lui et al. investigated weight change patterns and compared 4 BMI trajectory groups with the “stable normal” group [23]. In line with other studies, the incident rate was higher in the “stable obese” group, and this group had the most risk of incident CHF with an AHR of 4.22 (95% CI 2.63, 6.79). Also, the “non-obese to obese” group and the “maximum overweight” group significantly increased this risk, unlike the “obese to non-obese” group.
Finally, from the above studies, it can be concluded that long-term obesity can be associated with the risk of HF. More prolonged exposure to obesity increases the risk of incident HF. In addition to the duration of obesity, its severity also increases this risk, but more studies are needed to distinguish this association separately in HFpEF and HFrEF patients. It is also noteworthy that across all BMI categories, low fitness has been attributed to a noticeably greater risk of HF and may account for close to 50% of the HF risk linked to BMI [36]. Greater physical exercise and fitness levels significantly reduce the risk of develo** HF, and high fitness is a prognosis factor in patients with diagnosed HF [33, 36, 37]. Several studies indicate a favorable prognosis for HF patients with adequate fitness levels, regardless of BMI [19, 37, 38].
Stroke
Obesity is a well-established risk factor for stroke [39]; however, the patterns of weight changes and the cumulative effect of excess body weight are less studied with more controversial results. Accordingly, the CARDIA study reported 32 incident strokes in 4601 young adults and did not find an association between excess BMI-years with incident stroke [14]. In this study, the model 1 AHR for each additional 50 excess BMI-years was 0.90 (95% CI 0.70–1.17), reporting no association, and additional results regarding model 2 AHR were not reported. Similarly, in 2018, the TLGS study investigated the effect of CEW and the duration of general obesity and their association with stroke [15]. The study did not observe a significant association in all three confounder-adjusted models for these exposures in either sex.
Despite these two cohorts that find a null relation between the duration of obesity and stroke, Abdullah et al. estimated that HR increases for cerebrovascular accident (CVA) when the number of obese-years increases every 10 units [16]. Also, this relation was significant in both males and females in all adjusted models. Finally, this study estimated a 3% increase in the risk of stroke per 10-unit increase in obese-years. The discrepancy between the results of these three studies can be due to their different follow-up periods. Abdullah et al. had the most prolonged follow-up period (50 years), which can account for reporting more CVAs. However, based on these conflicting results, more studies with long follow-ups on the duration of obesity and stroke risk are necessary to define the association between the two betters.
Additionally, two studies investigated the effect of changes in obesity over time and how this can associate with incident stroke. In this regard, Iyen et al. compared three BMI trajectories (obese 1-S, obese 2-S, and obese 3-S) with overweight-S [22]. They found a statistically significant association between obese 1-S and obese 2-S with overweight-S in terms of increased risk of stroke/TIA by 9 and 13%, respectively. Interestingly, after adding comorbidities to the adjustment model, obese 3-S did not differ significantly from overweight-S.
In Iyen et al.’s study, the participants of each group had almost the same BMI over time. However, in Lui et al.’s study, the grou**s were in a way that represented changes in BMI during follow-up [23]. They reported HRs of incident stroke with weight change patterns across adulthood. Compared with the “stable normal” group, the “obese to non-obese” group and the “non-obese to obese” group had an increased risk of incident stroke with an AHR of 2.71 (95% CI 1.09–6.72) and 1.60 (95% CI 1.19–2.15) respectively. However, the “maximum overweight” and the “stable obese” groups were not significantly associated with the stroke incident in the adjusted model.
In both mentioned studies, the association between the stable obese group and the risk of stroke became insignificant after adjusting the covariates. Two common covariates exist between these two studies, including smoking and alcohol consumption. It can be implied that these are the cause of the association, and there is no independent association, especially in very severe obese patients. Furthermore, despite the different BMI trajectory groups, according to these two studies, it can be inferred that obesity can increase the risk of stroke over time. This relation remains even after changing from obesity to average weight. However, more studies are needed in this field to achieve more reliable results.
Peripheral Vascular Disease
PVD can be an influential predictor of CVD independent of associated symptoms and is also a sign of systemic atherosclerosis [40]. The effect of obesity has been less investigated in PVD than in other CVDs. Still, a direct relation between overweight and intermittent claudication, which characterizes PVD, has not been observed [12]. However, obesity increases the risk of other diseases, such as elevated blood pressure and diabetes, which along with systemic inflammation, can result in PVD [41]. Likewise, the relation between the duration of obesity or weight changes with PVD is less examined. Among mentioned studies, Iyen et al. evaluated the association between BMI group trajectories and the risk of PVD [22]. Compared to the overweight-S group, the obese 1-S and the obese 2-S groups did not differ significantly; however, the obese 3-S group showed a significantly reduced risk of PVD. This reduced risk and the lack of association can be due to under-diagnosis of this disease or different underlying mechanisms than other CVDs that necessitate further study in this field.
Atrial Fibrillation
AF, which affected an estimated 33.5 million people worldwide in 2010 and is predicted to increase by 5 million cases annually, has also increased significantly over the past few decades [42]. AF lowers the quality of life and raises mortality and morbidity [43]. A fuller comprehension of AF risk factors is crucial since preventing and treating AF involve significant medical and social challenges.
Obesity and the risk of AF have well-known correlations [44]. Nevertheless, studies that take parameters of one’s BMI at one time do not reflect the cumulative impact of obesity throughout a person’s life on the development of AF. In this regard, Tedrow et al. investigated the relation between a BMI change over the 60 months in 32,309 women with the risk of AF [45]. As a result, the women who remained obese tended toward a higher risk of incident AF by year 5. In comparison, the women with new obesity had a significantly higher risk of AF during this time with an AHR of 1.41 (95% CI 1.05–1.90) compared with those who maintained a BMI < 30 kg/m2 over the same period. Contrastingly, women who were obese at baseline but then reached a BMI < 30 kg/m2 by year 5 no longer had a significantly elevated risk of incident AF compared with women who maintained a BMI < 30 kg/m2 at the same time. Later, in 2019 the HUNT study examined the relation between AF and BMI trajectories through three trajectories, including obese, overweight, and normal weight trajectory groups. The obese trajectory group had the highest risk of incident AF, with an increased risk of 90%, followed by the overweight trajectory group, with an increased risk of 20% compared with the normal weight trajectory [43]. These two studies lead to the conclusion that stable obesity and overweight during a period and AF and also new obesity during time are associated with high risks of incident AF.
Conclusions
Being overweight/obese is a risk factor for CVDs as heterogeneous diseases. Due to the increased incidence of overweight/obesity at younger ages and the longer exposure time, it is essential to know the effect of its duration. CVD, HF, and AF seem to be associated with the duration of overweight/obesity, but this does not apply to all CVD subgroups. However, there are contradictory results regarding CHD and stroke with the duration of obesity. Also, no association with PVD has yet to be reported. This lack of association can be due to covariates or different follow-up periods.
Nevertheless, it seems that both stable overweight and remarkably stable obesity increase the risk of CVDs and a history of overweight or obesity in the past is also effective in increasing the risk. On the other side, metrics showing both the severity and the duration of overweight/obesity are more effective than each alone, and it is recommended to be used for assessing the risk of various CVDs. There are few studies in these areas, and studies with more extended follow-up periods, and a wide age range, while adjusting for some specific covariates, are needed.
References
Hassanin A, Hassanein M, Lanier GM, Sadaka M, Rifaat M, Sanhoury M. Prevalence of obesity and its association with cardiometabolic risk factors, heart failure phenotype and mortality among patients hospitalized for heart failure in Egypt. Egyptian Heart J. 2022;74(1):1. https://doi.org/10.1186/s43044-021-00232-y.
Ashwell M, Mayhew L, Richardson J, Rickayzen B. Waist-to-height ratio is more predictive of years of life lost than body mass index. PLoS ONE. 2014;9(9): e103483.
Dixon JB, Zimmet P, Alberti KG, Rubino F, Epidemiology IDFTo, Prevention. Bariatric surgery: an IDF statement for obese type 2 diabetes. Surg Obes Related Dis. 2011;7(4):433–47.
Katta N, Loethen T, Lavie CJ, Alpert MA. Obesity and coronary heart disease: epidemiology, pathology, and coronary artery imaging. Curr Probl Cardiol. 2021;46(3): 100655.
Pang J, Nguyen V, Rhodes D, Sullivan M, Braunschweig C, Fantuzzi G. Relationship of galectin-3 with obesity, IL-6, and CRP in women. J Endocrinol Invest. 2016;39(12):1435–43.
Collaboration NRF. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19· 2 million participants. Lancet. 2016;387(10026):1377–96.
Karimbeiki R, Namkhah Z, Alipoor E, Yaseri M, Hosseinzadeh-Attar MJ. The relationship between low-carbohydrate diet score, dietary insulin index and load with obesity in healthy adults. Eating Weight Disorders-Studies Anorexia Bulimia Obes. 2022;27(8):3341–50. https://doi.org/10.1007/s40519-022-01464-w
Grundy SM. Obesity, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab. 2004;89(6):2595–600.
Pérez-Galarza J, Baldeón L, Franco O, Muka T, Drexhage H, Voortman T, et al. Prevalence of overweight and metabolic syndrome, and associated sociodemographic factors among adult Ecuadorian populations: the ENSANUT-ECU study. J Endocrinol Invest. 2021;44(1):63–74.
Barazzoni R, Gortan Cappellari G, Ragni M, Nisoli E. Insulin resistance in obesity: an overview of fundamental alterations. Eating Weight Disorders-Stud Anorexia Bulimia Obes. 2018;23(2):149–57.
Ortega FB, Lavie CJ, Blair SN. Obesity and cardiovascular disease. Circ Res. 2016;118(11):1752–70.
Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67(5):968–77.
Bogers RP, Bemelmans WJ, Hoogenveen RT, Boshuizen HC, Woodward M, Knekt P, et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: a meta-analysis of 21 cohort studies including more than 300 000 persons. Arch Intern Med. 2007;167(16):1720–8.
Reis JP, Allen N, Gunderson EP, Lee JM, Lewis CE, Loria CM, et al. Excess body mass index-and waist circumference-years and incident cardiovascular disease: the CARDIA study. Obesity. 2015;23(4):879–85.
Kabootari M, Asgari S, Mansournia MA, Khalili D, Valizadeh M, Azizi F, et al. Different weight histories and risk of incident coronary heart disease and stroke: Tehran Lipid and Glucose Study. J Am Heart Assoc. 2018;7(4): e006924.
Abdullah A, Amin FA, Stoelwinder J, Tanamas SK, Wolfe R, Barendregt J, et al. Estimating the risk of cardiovascular disease using an obese-years metric. BMJ Open. 2014;4(9): e005629.
Farah R, Groot W, Pavlova M. Knowledge, attitudes and practices survey of cardiac rehabilitation among cardiologists and cardiac surgeons in Lebanon. Egyptian Heart J. 2021;73(1):87. https://doi.org/10.1186/s43044-021-00212-2.
El Missiri A, Abdel Halim WA, Almaweri AS, Mohamed TR. Effect of a phase 2 cardiac rehabilitation program on obese and non-obese patients with stable coronary artery disease. Egyptian Heart J. 2021;73(1):4. https://doi.org/10.1186/s43044-020-00119-4.
Elagizi A, Kachur S, Lavie CJ, Carbone S, Pandey A, Ortega FB, et al. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. 2018;61(2):142–50.
Horwich TB, Fonarow GC, Clark AL. Obesity and the obesity paradox in heart failure. Prog Cardiovasc Dis. 2018;61(2):151–6.
Lavie CJ, Sharma A, Alpert MA, De Schutter A, Lopez-Jimenez F, Milani RV, et al. Update on obesity and obesity paradox in heart failure. Prog Cardiovasc Dis. 2016;58(4):393–400.
Iyen B, Weng S, Vinogradova Y, Akyea RK, Qureshi N, Kai J. Long-term body mass index changes in overweight and obese adults and the risk of heart failure, cardiovascular disease and mortality: a cohort study of over 260,000 adults in the UK. BMC Public Health. 2021;21(1):1–13.
Liu M, Zhang Z, Zhou C, He P, Zhang Y, Li H, et al. Relationship of weight change patterns from young to middle adulthood with incident cardiovascular diseases. J Clin Endocrinol Metab. 2021;106(2):e812–23.
Dhana K, van Rosmalen J, Vistisen D, Ikram MA, Hofman A, Franco OH, et al. Trajectories of body mass index before the diagnosis of cardiovascular disease: a latent class trajectory analysis. Eur J Epidemiol. 2016;31(6):583–92.
El Shahawy M, Tucker S, Izadi L, Sabatini A, Mohan S. Excess epicardial fat volume in women is a novel risk marker for microvascular dysfunction, which may be a contributing factor in the atypical chest pain syndrome. Egyptian Heart J. 2021;73(1):37. https://doi.org/10.1186/s43044-021-00159-4.
Choi S, Kim K, Kim SM, Lee G, Jeong S-M, Park SY, et al. Association of obesity or weight change with coronary heart disease among young adults in South Korea. JAMA Intern Med. 2018;178(8):1060–8.
Calling S, Johansson S-E, Nymberg VM, Sundquist J, Sundquist K. Trajectories of body mass index and risk for coronary heart disease: a 38-year follow-up study. PLoS ONE. 2021;16(10): e0258395.
Reis JP, Loria CM, Lewis CE, Powell-Wiley TM, Wei GS, Carr JJ, et al. Association between duration of overall and abdominal obesity beginning in young adulthood and coronary artery calcification in middle age. JAMA. 2013;310(3):280–8.
Groenewegen A, Rutten FH, Mosterd A, Hoes AW. Epidemiology of heart failure. Eur J Heart Fail. 2020;22(8):1342–56.
Koutroumpakis E, Kaur R, Taegtmeyer H, Deswal A. Obesity and heart failure with preserved ejection fraction. Heart Fail Clin. 2021;17(3):345–56. https://doi.org/10.1016/j.hfc.2021.02.003.
Ammar W, Basset HA, Al Faramawy A, Hegazy T, Sharaf Y. Bariatric surgery and cardiovascular outcome. Egyptian Heart J. 2020;72(1):67. https://doi.org/10.1186/s43044-020-00096-8.
Pandey A, Patel KV, Vaduganathan M, Sarma S, Haykowsky MJ, Berry JD, et al. Physical activity, fitness, and obesity in heart failure with preserved ejection fraction. JACC. 2018;6(12):975–82.
Pandey A, LaMonte M, Klein L, Ayers C, Psaty BM, Eaton CB, et al. Relationship between physical activity, body mass index, and risk of heart failure. J Am Coll Cardiol. 2017;69(9):1129–42.
Reis JP, Allen N, Gibbs BB, Gidding SS, Lee JM, Lewis CE, et al. Association of the degree of adiposity and duration of obesity with measures of cardiac structure and function: the CARDIA study. Obesity. 2014;22(11):2434–40.
Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. 2013;62(4):263–71.
Pandey A, Cornwell WK, Willis B, Neeland IJ, Gao A, Leonard D, et al. Body mass index and cardiorespiratory fitness in mid-life and risk of heart failure hospitalization in older age: findings from the Cooper Center Longitudinal Study. JACC. 2017;5(5):367–74.
Lavie CJ, Laddu D, Arena R, Ortega FB, Alpert MA, Kushner RF. Healthy weight and obesity prevention: JACC health promotion series. J Am Coll Cardiol. 2018;72(13):1506–31.
Pandey A, Patel KV, Lavie CJ. Obesity, central adiposity, and fitness: understanding the obesity paradox in the context of other cardiometabolic parameters. Mayo Clinic Proceedings: Elsevier; 2018. p. 676–8.
Forlivesi S, Cappellari M, Bonetti B. Obesity paradox and stroke: a narrative review. Eating Weight Disorders-Stud Anorexia, Bulimia Obes. 2021;26(2):417–23.
Ciardullo S, Bianconi E, Cannistraci R, Parmeggiani P, Marone E, Perseghin G. Peripheral artery disease and all-cause and cardiovascular mortality in patients with NAFLD. J Endocrinol Invest. 2022;45(8):1547–53 .
Moussa O, Ardissino M, Muttoni S, Faraj A, Tang A, Khan O, et al. Long-term incidence and outcomes of obesity-related peripheral vascular disease after bariatric surgery. Langenbecks Arch Surg. 2021;406(4):1029–36.
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129(8):837–47.
Feng T, Vegard M, Strand LB, Laugsand LE, Mørkedal B, Aune D, et al. Weight and weight change and risk of atrial fibrillation: the HUNT study. Eur Heart J. 2019;40(34):2859–66.
Aune D, Sen A, Schlesinger S, Norat T, Janszky I, Romundstad P, et al. Body mass index, abdominal fatness, fat mass and the risk of atrial fibrillation: a systematic review and dose–response meta-analysis of prospective studies. Eur J Epidemiol. 2017;32:181–92.
Tedrow UB, Conen D, Ridker PM, Cook NR, Koplan BA, Manson JE, et al. The long-and short-term impact of elevated body mass index on the risk of new atrial fibrillation: the WHS (Women’s Health Study). J Am Coll Cardiol. 2010;55(21):2319–27.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Author Contributions
Conceptualization: Masoumeh Sadeghi, Hamidreza Zefreh; Methodology: Reza Amani-Beni, Bahar Darouei, Erfan Sheikhbahaei, Hamidreza Zefreh; Investigation and Literature Search: Reza Amani-Beni, Bahar Darouei; Data Curation: Reza Amani-Beni, Bahar Darouei; Writing—Original Draft: Reza Amani-Beni, Bahar Darouei, Hamidreza Zefreh; Writing—Review & Editing: Masoumeh Sadeghi, Erfan Sheikhbahaei; Visualization: Reza Amani-Beni, Bahar Darouei, Hamidreza Zefreh; Supervision and Project administration: Reza Amani-Beni, Erfan Sheikhbahaei, Masoumeh Sadeghi.
Disclosures
Reza Amani-Beni, Bahar darouei, Hamidreza Zefreh, Erfan Sheikhbahaei, and Masoumeh Sadeghi have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Amani-Beni, R., Darouei, B., Zefreh, H. et al. Effect of Obesity Duration and BMI Trajectories on Cardiovascular Disease: A Narrative Review. Cardiol Ther 12, 307–326 (2023). https://doi.org/10.1007/s40119-023-00317-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-023-00317-6