Abstract
Gelatin-based photopolymerizable methacrylate hydrogel (GelMA) is a promising biomaterial for in situ drug delivery, while aqueous extract of Punica granatum (AEPG) peel fruit rich in gallic acid and ellagic acid is used to improve wound healing. The aim of this study was to develop and analyze the healing properties of GelMA containing AEPG, gallic acid, or ellagic acid in a rodent model. GelMA hydrogels containing 5% AEPG (GelMA-PG), 1.6% gallic acid (GelMA-GA), or 2.1% ellagic acid (GelMA-EA) were produced and their mechanical properties, enzymatic degradation, and thermogravimetric profile determined. Wound closure rates, healing histological grading, and immunohistochemical counts of myofibroblasts were assessed over time. The swelling of hydrogels varied between 50 and 90%, and GelMA exhibited a higher swelling than the other groups. The GPG samples showed higher compression and Young’s moduli than GelMA, GGA, and GAE. All samples degraded around 95% in 48 h. GPG and GGA significantly accelerated wound closure, improved collagenization, increased histological grading, and hastened myofibroblast differentiation in comparison to the control, GelMA, and GEA. GelMA containing AEPG (GPG) improved wound healing, and although gallic acid is the major responsible for such biological activity, a potential synergic effect played by other polyphenols present in the extract is evident.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The skin integrity can be compromised by chronic diseases, such as diabetes and vascular diseases, but also by physical injuries (e.g., accidents and falls, high pressure, surgical interventions) and body immobility. All these factors compromise the role of the skin in kee** homeostasis, increasing the risk of infection, and may even result in high morbidity rates [1].
Wound dressings are instrumental in standard wound treatments, since these delivery systems have the capacity to physically protect the wound against mechanical injury, absorb its drainage, and provide the required moisture to foster and optimize re-epithelialization [2]. Several biomaterials with physiological and mechanical properties that resemble epidermal and dermal tissues have been proposed for the design of optimal wound dressings [3,4,5], aiming to accelerate wound healing and reconstitution of injured skin [6]. However, the design of a reliable and cost-effective wound dressing is still a challenging task, provided that it should respond to the wound drainage and its depth [7].
Among potential biomaterials, hydrogels are reported to be useful to create the required moist environment in which dermal cells (e.g., fibroblasts, macrophages, stem cells, adipocytes, mast and Schwann cells) can thrive for further healing, while being comfortable to the patient. Hydrogels may also facilitate tissue regeneration by acting as a scaffold for stem cells and as a supplier of drugs and other biomolecules [8].
Hydrogels based on methacrylated gelatin (GelMA) obtained by ultraviolet (UV) photoreticulation have been reported as an excellent biomaterial for wound dressings because they allow for proper cell adhesion, are highly permeable to nutrients, proteins, and oxygen, and can be easily degraded by enzymes [9, 10]. GelMA is also reported to be an effective biopolymer to load and deliver bioactive compounds and other drugs to improve wound healing [11, 12].
The formulation of bioactive compounds, from isolated molecules to more complex substances (such as plant extracts), into collagen-based biomaterials (including hydrogels) for wound dressing, has been largely used as a strategy to improve the healing properties of hydrogels [13]. These functional hydrogels are designed, not only to protect the wound bed and promote a proper environment for cell adhesion and proliferation but also to deliver substances that play important pathophysiological functions over the time-course of wound healing (e.g., with antimicrobial, anti-inflammatory, and anti-oxidation activities) and contribute to hemostasis [14, 15].
The pomegranate (Punica granatum Linn) fruit is known for its composition rich in phenolics and tannins [16]. The aqueous extracts of pomegranate peel have been described to stimulate collagen synthesis and proliferation of dermal fibroblasts, besides the potential to impair the activity of major collagen-degrading enzymes [17].
Based on documented evidence that Punica granatum extracts improve wound healing, both in vitro and in vivo [18,19,20], we have recently developed gelatin-based membranes containing aqueous extracts of the fruit peel and evaluated their potential to promote major histological changes towards wound healing [21], namely, improved deposition and arrangement of collagen fibers, formation of new granular tissue, and development of cutaneous appendages.
The biological activities of the aqueous extract of Punica granatum are attributed to its rich composition in phenolic compounds, particularly tannins, such as gallic and ellagic acid [22]. Ellagic acid is a well-known phytochemical metabolite that shows anti-inflammatory activity by changing pro-inflammatory mediators (tumor necrosis factor-α, interleukin-1β, interleukin-6) and by reducing the activity of nuclear factor-κB while increasing nuclear factor erythroid 2-related factor 2 expression [23]. Gallic acid is also known for its anti-inflammatory properties and for being able to inhibit keloid-derived fibroblast proliferation and migration, by downregulating matrix metalloproteinase-1 and -3 while upregulates tissue inhibitors of metalloproteinase-1, by suppressing the AKT/ERK signaling pathway [24]. Both polyphenols, ellagic and gallic acids, are potentially capable of modulating the key phases of the wound healing process, such as inflammation, angiogenesis, and collagenization [21].
Although the functionalization of methacrylated gelatin (GelMA) with tannic compounds, such as gallic acid, has been previously reported [25], there are still no studies either addressing the functionalization with ellagic acid and/or evaluating the healing activity of these functionalized photopolymerizable hydrogels in in vivo models. Therefore, the aim of this study was to design, characterize, and evaluate the healing potential of UV-polymerizable hydrogels based on methacrylated gelatin (GelMA) containing Punica granatum Linn peel extract and polyphenolic compounds for use as dressings on open wounds.
Material and methods
Plant extract material
The aqueous extract of pomegranate (Punica granatum Linn) fruit peel containing 32.24 mg/g of gallic acid and 41.67 mg/g of ellagic acid was prepared and characterized, as previously described by do Nascimento et al. [21]. Briefly, the peels of P. granatum were submitted to a drying procedure at 55 °C for 5 days. Then, 5 g of dried and powdered peels (32 mesh) was subjected to extraction by dynamic maceration in water (1:100 w/v) at 100 °C for 2 h, using a magnetic stirrer. The extract was filtered and concentrated in an airflow oven at 55 °C for 3 days.
Production of gelatin methacryloyl prepolymer (GelMA)
For the production of prepolymer, a well-established, previously described protocol was followed [9, 26, 27]. Briefly, gelatin (10% w/v, Np Comercio De Produtos Alimenticios Ltda, São Paulo, Brazil) was dissolved in Dulbecco’s phosphate-buffered saline (DPBS; GIBCO) at 60 °C, pH 7.4, and methacrylic anhydride (1% v/v) was added to the solution (50 °C). After 3 h, the mixture was dialyzed against distilled water for 1 week. The material was subjected to lyophilization (− 55 °C and vacuum pump at 0.03–0.2 mbar) for 5 consecutive days using a Liotop L101 (Liobras, São Carlos, São Paulo, Brazil) to form the GelMA prepolymer. Subsequently, the photoinitiator Irgacure 2959 (2-hydroxyl-1-[4-(2-hydroxyethoxy) phenyl] -2-methyl-1-propanone, 0.5 w/v%, Sigma-Aldrich, St. Louis, MO, USA) was mixed to a GelMA prepolymer solution (10% w/v in DPBS, 80 °C). Photocrosslinking was achieved by exposing the solution to 6.7 mW cm−2 UV light Philips TL40W/12 RS (light intensity of 8.6 × 104/cm2) (Koninklijke Philips N.V., Amsterdam, The Netherlands) for 60 s. The same formulation was prepared by adding AEPG (0.005 g), gallic acid (0.0016 g, > 99%, 3C6H2CO2H. H2O, MW: 188.13 g/mol, Sigma-Aldrich, St. Louis, MO, USA), or ellagic acid (0.0021 g, > 95%, C14H6O8, MW: 302.19 g/mol, Sigma-Aldrich) based on previously performed chemical analysis of the crude aqueous extract of Punica granatum (do Nascimento et al. [21]), to obtain the formulations composed of 5% GelMA-GPG, 1.6% GelMA-GA, and 2.1% GelMA-EA, respectively.
Characterization of the GelMA-based formulations
Assessment of the swelling ratio (%)
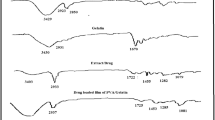
The swelling ratio was assessed as described by ** with enhanced accuracy, being a fast, less expensive, and useful alternative over other analytical techniques. Although destructive, TGA is a high-throughput approach. Samples were heated up to 800 °C (Fig. 2), and, for all developed hydrogels, the highest residual weight was recorded between 200 and 500 °C. Up to 200 °C, the percentage of water loss was lower than 20%, which translates appropriate thermal stability of the developed hydrogels. The first stage of water loss was recorded between 90 and 110 °C attributed to the loss of water adsorbed on the surface of the hydrogels, whereas the most significant was recorded between 110 and 230 °C attributed to the loss of structural water. The presence of the aqueous extract of Punica granatum (GelMA-PG), gallic acid (GelMA-GA), and ellagic acid (GelMA-EA) did not influence the residual weight recorded up to 200 °C, when compared to plain GelMA (control).
Filling the wound area with GelMA containing AEPG (GPG), gallic acid (GGA), and ellagic acid (GEA) improved wound closure on day 3, likely in response to the anti-inflammatory activity of those phenolic compounds, also present in the extract [62]. Hence, the reduction of the area of the wounds filled with GPG, GGA, and GEA in the earlier stages of wound healing would have been a result of the lower severity of inflammation and interstitial edema, rather than a myofibroblast-related wound closure effect. On the 7th and 14th days, GPG and GGA showed significant improvement of wound closure. However, as GelMA and GEA did not show similar results, it is assumed that gallic acid might be the key molecule promoting wound closure acceleration. Supporting our findings, many other studies have previously demonstrated the gallic acid-related improvement of wound closure in wound healing assays [45, 54, 63,64,65]. The healing activity of the hydrogels containing gallic acid reported in the last 3 years (Table 2) has been related to the antioxidant and anti-inflammatory properties of this chemical compound. However, some studies have pointed at a potential modulatory effect of these ellagitannin-containing biomaterials on angiogenesis and collagenization steps of wound healing [44, 46, 50, 51, 54].
To clarify whether the wound closure acceleration was related to the improvement of the pathological features in the scar repairing, a wound healing histological grading system was applied in this study. The main advantages of the system used herein are as follows: (i) it encompasses the basic components of the healing process including angiogenesis, inflammation, fibroplasia, and epithelialization and differentiation and (ii) it is highly specific and standardized, while it is easily reproducible [30]. The very same system has already been successfully used in previous studies of wound healing in rodents [12, 21, 66]. The improvement of the histological grading of wound healing observed in all the groups whose skin wounds were filled with the gelatin-based biomaterials (GelMA, GPG, GGA, and GEA), in comparison to unfilled wounds (CTR), is possibly related to the bioconductive properties of the hydrogel, whose 3D-polymeric structure works as a scaffold for cell adhesion, proliferation, and migration, thus facilitating the earlier formation of granulation tissue and further reconstitution of the dermal lost tissue [9,10,11,12]. However, since GPG and GGA presented significantly better histological gradings over the time-course of the experiment, gallic acid released into the wound bed could likely be triggering additional pathophysiological, biochemical, or molecular scarring mechanisms, in addition to those promoted by GelMA, providing even better healing outcomes. Supporting these findings, gallic acid has previously been demonstrated to increase the viability of cultured cells subjected to oxidative stress through free radical scavenging, to modulate the expression of antioxidant genes in keratinocytes and fibroblasts, and to accelerate cell migration of keratinocytes and fibroblasts in an in vitro healing model [63]. In addition, it has been demonstrated that the healing properties of gallic acid-containing hydrogels could result from increased VEGF and TGF-β expressions, which would promote the improvement of the angiogenesis and myofibroblast differentiation, consequently improving the granulation tissue and collagen scar formation [46, 54].
Since the 2000s, the intensity of deposition, morphology, and architectural arrangement of collagen fibers are considered key events to assess the success of wound healing, particularly in secondary intention healing [67,68,69]. A significant increase in collagen deposition in wounds with great loss of substance can determine the formation of hypertrophic scars at the end of the process [70], whereas the reduced collagenization induces depressed/atrophic scarring [71]. The Sirius red histochemical technique, analyzed under polarized light microscopy, is highly sensitive and specific method for the identification and quantification of collagen fibers by means of birefringence patterns, differences in diameter, and structures of these fibers. Type III collagen forms thin fibers consisting of delicate fibrils, loosely arranged showing a weak greenish and yellow-green birefringence, whereas type I collagen forms fibers of variable thickness, arranged parallel or intertwined, with golden and reddish birefringence [72]. As observed in our study, the scarce deposition of type III collagen fibrils in the earliest stages of wound healing, which are further degraded and replaced by compact bundles (with less interfibrillar spaces) of type I collagen in the later stages, has already been reported in other studies [12, 21, 66]. This is because thin and delicate type III collagen fibrils are initially deposited in order to provide a three-dimensional scaffold that guides endothelial migration during the early stages of granulation tissue development. Subsequently, these fibers are progressively replaced by thicker type I collagen fibers with greater tensile strength as the scar tissue matures [73].
In a previous study, we have demonstrated that AEPG stimulates collagen deposition in rodent model of wound healing [21]. Hence, we investigated whether such a stimulatory effect would be promoted by gallic acid or ellagic acid found in AEPG. The application of GelMA improved type III collagen deposition on day three, regardless of whether or not it contains bioactive compounds, possibly by facilitating the influx of fibroblasts into the wound bed. However, GPG and GGA promoted greater improvement of collagenization on day seven, suggesting a possible role played by gallic acid on collagen synthesis during wound healing. The effects of gallic acid on collagen deposition are still controversial. Dermal fibroblasts treated with gallic acid-coated gold nanoparticles have been shown to prevent UV-induced photoaging by suppressing the expression of MMP-1, the major collagenase capable of destroying type I and III collagen [74]. In addition, gallic acid-induced upregulation of collagen synthesis required for proper wound healing has been reported and attributed to its antioxidant or anti-inflammatory activities [64]. On the other hand, other investigations pointed at a potential inhibitory effect of gallic acid on collagen synthesis in bleomycin-induced pulmonary fibrosis [75] and pressure overload-induced cardiac fibrosis [76]. This apparent paradox might be related to possible differences in the response pattern of dermal fibroblasts and those ones present in other connective tissues to gallic acid.
We have previously demonstrated histological evidence of the association between increased myofibroblast activity and improved wound healing promoted by the use of collagen-based membranes containing an aqueous extract of Punica granatum in rodent model [21]. Similarly, the AEPG delivered in GelMA also enhanced myofibroblast differentiation on day seven in the current study. The proliferative phase of wound healing that occurs from days seven to 14 in a rodent model is typically characterized by abundant myofibroblast differentiation [42], which explains the low myofibroblast number on day three. Moreover, the number of myofibroblasts was also increased in response to the delivery of gallic acid, but not ellagic acid, although the number of myofibroblast was even greater in wounds treated with AEPG than with gallic acid. These data suggest that gallic acid is at least in part responsible for the increased myofibroblast number on day 7, but other chemicals present in the extract might be playing a synergic or additional role on this pathophysiological event. Paradoxically, gallic acid has been demonstrated to induce apoptosis of excessive myofibroblasts via activation of p53 pathway, attenuating lung fibrosis [76]. Furthermore, GA treatments markedly suppressed the mRNA level of α-SMA, a local event needed to generate differentiated myofibroblasts [77]. Hence, although it is unlikely that gallic acid directly stimulated the formation of myofibroblasts, based on our results, a probable indirect effect on this pathophysiological event could still be assumed. In fact, as no significant difference in myofibroblast number was observed between groups on day 14, the greater number of myofibroblasts on day 7 could rather be a result of acceleration than the increase of myofibroblast differentiation. In this way, not only gallic acid but also other phenolic compounds are able to attenuate inflammation and oxidative stress in rodents [77, 78], which could ultimately favor the earlier development of an appropriate microenvironment for fibroblastic proliferation and subsequent myofibroblast differentiation. In addition, since myofibroblasts are specialized cells rich in contractile filaments of actin that facilitate rapid wound closure in healing tissues [79], it is possible to assume that the improvement in wound closure was mediated by earlier myofibroblast activity.
Interestingly, it is well established that ellagic acid is also able to modulate the inflammatory response and free radical formation [80, 81]. These data suggest that, even at lower concentrations, gallic acid was more efficient than ellagic acid to modulate the initial stages of wound healing. On the other hand, the presence of other phenolic compounds in the AEPG, such as ellagic acid [21], even in lower contractions, may have acted synergistically in modulating inflammation and inhibiting oxidative stress, which would have determined better results by using the GelMA containing the extract.
Conclusions
In conclusion, the present study suggests that the photopolymerizable hydrogel based on methacrylated gelatin (GelMA) containing an aqueous extract of Punica granatum (AEPG) is a promising biomaterial to accelerate the healing of wounds with loss of substance. We demonstrated that this biomaterial not only has adequate mechanical properties for use as a moldable filling material for open wounds but also accelerates wound closure, improves the histological gradation of wound healing, and modulates myofibroblast differentiation in rodent model. Furthermore, our data suggest that gallic acid seems to represent the chemical compound present in the extract responsible for promoting the biological effects of this latter.
Data availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Murphree RW. Impairments in skin integrity. Nurs Clin North Am. 2017;52(3):405–17. https://doi.org/10.1016/j.cnur.2017.04.008.
Obagi Z, Damiani G, Grada A, Falanga V. Principles of wound dressings: a review. Surg Technol Int. 2019;35:50–7.
Shahnawaz Khan M, Abdelhamid HN, Wu H-F. Near infrared (NIR) laser mediated surface activation of graphene oxide nanoflakes for efficient antibacterial, antifungal and wound healing treatment. Colloids Surf B. 2015;127:281–91. https://doi.org/10.1016/j.colsurfb.2014.12.049.
Hussein KH, Abdelhamid HN, Zou X, Woo H-M. Ultrasonicated graphene oxide enhances bone and skin wound regeneration. Mater Sci Eng, C. 2019;94:484–92. https://doi.org/10.1016/j.msec.2018.09.051.
Soliman M, Sadek AA, Abdelhamid HN, Hussein K. Graphene oxide-cellulose nanocomposite accelerates skin wound healing. Res Vet Sci. 2021;137:262–73. https://doi.org/10.1016/j.rvsc.2021.05.013.
Dai C, Shih S, Khachemoune A. Skin substitutes for acute and chronic wound healing: an updated review. J Dermatol Treat. 2020;31(6):639–48.
Tang N, Zheng Y, Cui D, Haick H. Multifunctional dressing for wound diagnosis and rehabilitation. Adv Healthcare Mater. 2021;10(22):2101292.
Op’t Veld RC, Walboomers XF, Jansen JA, Wagener FA. Design considerations for hydrogel wound dressings: strategic and molecular advances. Tissue Eng Part B Rev. 2020;26(3):230–48.
Yue K, Trujillo-de Santiago G, Alvarez MM, Tamayol A, Annabi N, Khademhosseini A. Synthesis, properties, and biomedical applications of gelatin methacryloyl (GelMA) hydrogels. Biomaterials. 2015;73:254–71.
Klotz BJ, Gawlitta D, Rosenberg AJ, Malda J, Melchels FP. Gelatin-methacryloyl hydrogels: towards biofabrication-based tissue repair. Trends Biotechnol. 2016;34(5):394–407.
Rehman SRU, Augustine R, Zahid AA, Ahmed R, Tariq M, Hasan A. Reduced graphene oxide incorporated GelMA hydrogel promotes angiogenesis for wound healing applications. Int J Nanomedicine. 2019:9603–17.
de Almeida BM, Dos Santos IDD, de Carvalho F, Correa LC, Cunha JL, Dariva C, et al. Himatanthus bracteatus-composed in situ polymerizable hydrogel for wound healing. Int J Mol Sci. 2022;23(23):15176.
Sharma S, Rai VK, Narang RK, Markandeywar TS. Collagen-based formulations for wound healing: a literature review. Life Sci. 2022;290:120096. https://doi.org/10.1016/j.lfs.2021.120096.
Liang Y, He J, Guo B. Functional hydrogels as wound dressing to enhance wound healing. ACS Nano. 2021;15(8):12687–722.
Cao D, Ding J. Recent advances in regenerative biomaterials. Regener Biomater. 2022;9.
Viuda-Martos M, Fernández-López J, Pérez-Álvarez J. Pomegranate and its many functional components as related to human health: a review. Compr Rev Food Sci Food Saf. 2010;9(6):635–54.
Aslam MN, Lansky EP, Varani J. Pomegranate as a cosmeceutical source: pomegranate fractions promote proliferation and procollagen synthesis and inhibit matrix metalloproteinase-1 production in human skin cells. J Ethnopharmacol. 2006;103(3):311–8.
Zekavat O, Amanat A, Karami M, Paydar S, Gramizadeh B, Zareian-Jahromi M. Wound healing studies using Punica granatum peel: an animal experimental study. Adv Skin Wound Care. 2016;29(5):217–25.
Lukiswanto BS, Miranti A, Sudjarwo SA, Primarizky H, Yuniarti WM. Evaluation of wound healing potential of pomegranate (Punica granatum) whole fruit extract on skin burn wound in rats (Rattus norvegicus). J Adv Vet Anim Res. 2019;6(2):202.
Celiksoy V, Moses RL, Sloan AJ, Moseley R, Heard CM. Evaluation of the in vitro oral wound healing effects of pomegranate (Punica granatum) rind extract and punicalagin, in combination with Zn (II). Biomolecules. 2020;10(9):1234.
do Nascimento MF, Cardoso JC, Santos TS, Tavares LA, Pashirova TN, Severino P, et al. Development and characterization of biointeractive gelatin wound dressing based on extract of Punica granatum Linn. Pharmaceutics. 2020. https://doi.org/10.3390/pharmaceutics12121204.
Vučić V, Grabež M, Trchounian A, Arsić A. Composition and potential health benefits of pomegranate: a review. Curr Pharm Des. 2019;25(16):1817–27.
Ríos J-L, Giner RM, Marín M, Recio MC. A pharmacological update of ellagic acid. Planta Med. 2018;84(15):1068–93.
Wang X, Liu K, Ruan M, Yang J, Gao Z. Gallic acid inhibits fibroblast growth and migration in keloids through the AKT/ERK signaling pathway. Acta Biochim Biophys Sin. 2018;50(11):1114–20.
Jongprasitkul H, Turunen S, Parihar VS, Kellomäki M. Sequential cross-linking of gallic acid-functionalized GelMA-based bioinks with enhanced printability for extrusion-based 3D bioprinting. Biomacromol. 2023;24(1):502–14. https://doi.org/10.1021/acs.biomac.2c01418.
Van Den Bulcke AI, Bogdanov B, De Rooze N, Schacht EH, Cornelissen M, Berghmans H. Structural and rheological properties of methacrylamide modified gelatin hydrogels. Biomacromol. 2000;1(1):31–8. https://doi.org/10.1021/bm990017d.
Hoch E, Schuh C, Hirth T, Tovar GE, Borchers K. Stiff gelatin hydrogels can be photo-chemically synthesized from low viscous gelatin solutions using molecularly functionalized gelatin with a high degree of methacrylation. J Mater Sci - Mater Med. 2012;23(11):2607–17. https://doi.org/10.1007/s10856-012-4731-2.
**ao W, He J, Nichol JW, Wang L, Hutson CB, Wang B, et al. Synthesis and characterization of photocrosslinkable gelatin and silk fibroin interpenetrating polymer network hydrogels. Acta Biomater. 2011;7(6):2384–93. https://doi.org/10.1016/j.actbio.2011.01.016.
Nichol JW, Koshy ST, Bae H, Hwang CM, Yamanlar S, Khademhosseini A. Cell-laden microengineered gelatin methacrylate hydrogels. Biomaterials. 2010;31(21):5536–44.
Gupta A, Kumar P. Assessment of the histological state of the healing wound. Plast Aesthet Res. 2015;2:239–42. https://doi.org/10.4103/2347-9264.158862.
Miot HA, Brianezi G. Análise morfométrica do colágeno dérmico a partir da segmentação por conglomerados (clusters) de cor. An Bras Dermatol. 2010;85.
Hutson CB, Nichol JW, Aubin H, Bae H, Yamanlar S, Al-Haque S, et al. Synthesis and characterization of tunable poly (ethylene glycol): gelatin methacrylate composite hydrogels. Tissue Eng Part A. 2011;17(13–14):1713–23.
Barroso IA, Man K, Robinson TE, Cox SC, Ghag AK. Photocurable gelma adhesives for corneal perforations. Bioengineering. 2022;9(2):53.
Ju Y, Hu Y, Yang P, **e X, Fang B. Extracellular vesicle-loaded hydrogels for tissue repair and regeneration. Mater Today Bio. 2023;18:100522. https://doi.org/10.1016/j.mtbio.2022.100522.
Tabatabaei F, Moharamzadeh K, Tayebi L. Fibroblast encapsulation in gelatin methacryloyl (GelMA) versus collagen hydrogel as substrates for oral mucosa tissue engineering. J Oral Biol Craniofac Res. 2020;10(4):573–7. https://doi.org/10.1016/j.jobcr.2020.08.015.
Goto R, Nishida E, Kobayashi S, Aino M, Ohno T, Iwamura Y, et al. Gelatin methacryloyl-riboflavin (GelMA-RF) hydrogels for bone regeneration. Int J Mol Sci. 2021. https://doi.org/10.3390/ijms22041635.
Monteiro N, Thrivikraman G, Athirasala A, Tahayeri A, França CM, Ferracane JL, et al. Photopolymerization of cell-laden gelatin methacryloyl hydrogels using a dental curing light for regenerative dentistry. Dent Mater. 2018;34(3):389–99. https://doi.org/10.1016/j.dental.2017.11.020.
Fan F, Saha S, Hanjaya-Putra D. Biomimetic hydrogels to promote wound healing. Front Bioeng Biotechnol. 2021;9:718377.
El-Sherbiny IM, Yacoub MH. Hydrogel scaffolds for tissue engineering: progress and challenges. Glob Cardiol Sci Pract. 2013;2013(3):38.
Zhuo RX, Li W. Preparation and characterization of macroporous poly (N-isopropylacrylamide) hydrogels for the controlled release of proteins. J Polym Sci Part A Polym Chem. 2003;41(1):152–9.
Ijaola AO, Akamo DO, Damiri F, Akisin CJ, Bamidele EA, Ajiboye EG, et al. Polymeric biomaterials for wound healing applications: a comprehensive review. J Biomater Sci Polym Ed. 2022;33(15):1998–2050.
Almeida BMD, Nascimento MFD, Pereira-Filho RN, Melo GCD, Santos JCD, Oliveira CRD, et al. Immunohistochemical profile of stromal constituents and lymphoid cells over the course of wound healing in murine model. Acta Cir Bras. 2014;29:596–602.
Velasco-Rodriguez B, Diaz-Vidal T, Rosales-Rivera LC, García-González CA, Alvarez-Lorenzo C, Al-Modlej A, et al. Hybrid methacrylated gelatin and hyaluronic acid hydrogel scaffolds. Preparation and systematic characterization for prospective tissue engineering applications. Int J Mol Sci. 2021;22(13):6758.
Zhang T, Guo L, Li R, Shao J, Lu L, Yang P, et al. Ellagic acid-cyclodextrin inclusion complex-loaded thiol-ene hydrogel with antioxidant, antibacterial, and anti-inflammatory properties for wound healing. ACS Appl Mater Interfaces. 2023;15(4):4959–72. https://doi.org/10.1021/acsami.2c20229.
He W-Y, Wang X-C, Gong W, Huang H-B, Hou Y-Y, Wang R, et al. Construction of an antibacterial hydrogel based on diammonium glycyrrhizinate and gallic acid for bacterial-infected wound healing. Colloids Surf B Biointerfaces. 2023;222:112975.
Hu Q, Nie Y, **ang J, **e J, Si H, Li D, et al. Injectable sodium alginate hydrogel loaded with plant polyphenol-functionalized silver nanoparticles for bacteria-infected wound healing. Int J Biol Macromol. 2023;234:123691. https://doi.org/10.1016/j.ijbiomac.2023.123691.
Gong W, Huang H-B, Wang X-C, He W-Y, Hu J-N. Coassembly of fiber hydrogel with antibacterial activity for wound healing. ACS Biomater Sci Eng. 2023;9(1):375–87. https://doi.org/10.1021/acsbiomaterials.2c00716.
Gong W, Wang R, Huang H, Hou Y, Wang X, He W, et al. Construction of double network hydrogels using agarose and gallic acid with antibacterial and anti-inflammatory properties for wound healing. Int J Biol Macromol. 2023;227:698–710. https://doi.org/10.1016/j.ijbiomac.2022.12.085.
Gong W, Huang H-B, Wang X-C, He W-Y, Hou Y-Y, Hu J-N. Construction of a sustained-release hydrogel using gallic acid and lysozyme with antimicrobial properties for wound treatment. Biomater Sci. 2022;10(23):6836–49. https://doi.org/10.1039/D2BM00658H.
Chen H, Zheng T, Wu C, Wang J, Ye F, Cui M, et al. A shape-adaptive gallic acid driven multifunctional adhesive hydrogel loaded with scolopin2 for wound repair. Pharmaceuticals (Basel, Switzerland). 2022. https://doi.org/10.3390/ph15111422.
Ren Y, Ma S, Zhang D, Guo S, Chang R, He Y, et al. Functionalized injectable hyaluronic acid hydrogel with antioxidative and photothermal antibacterial activity for infected wound healing. Int J Biol Macromol. 2022;210:218–32. https://doi.org/10.1016/j.ijbiomac.2022.05.024.
Huang H, Gong W, Wang X, He W, Hou Y, Hu J. Self-assembly of naturally small molecules into supramolecular fibrillar networks for wound healing. Adv Healthc Mater. 2022;11(12):e2102476. https://doi.org/10.1002/adhm.202102476.
Wang X-C, Huang H-B, Gong W, He W-Y, Li X, Xu Y, et al. Resveratrol triggered the quick self-assembly of gallic acid into therapeutic hydrogels for healing of bacterially infected wounds. Biomacromol. 2022;23(4):1680–92. https://doi.org/10.1021/acs.biomac.1c01616.
Park SG, Li M-X, Cho WK, Joung YK, Huh KM. Thermosensitive gallic acid-conjugated hexanoyl glycol chitosan as a novel wound healing biomaterial. Carbohyd Polym. 2021;260:117808.
Song R, Murphy M, Li C, Ting K, Soo C, Zheng Z. Current development of biodegradable polymeric materials for biomedical applications. Drug Des Devel Ther. 2018:3117–45.
McCarthy RC, Breite AG, Green ML, Dwulet FE. Tissue dissociation enzymes for isolating human islets for transplantation: factors to consider in setting enzyme acceptance criteria. Transplantation. 2011;91(2):137.
Benton JA, DeForest CA, Vivekanandan V, Anseth KS. Photocrosslinking of gelatin macromers to synthesize porous hydrogels that promote valvular interstitial cell function. Tissue Eng Part A. 2009;15(11):3221–30.
Chen D, Liu W, Pi Q, Yang J, Zhang YS. Preparation of injectable GelMA nanoparticles-based 3D printed wound healing filler. J Control Release. 2017;259:e23.
Pillai O, Panchagnula R. Polymers in drug delivery. Curr Opin Chem Biol. 2001;5(4):447–51.
Shi L, Yang N, Zhang H, Chen L, Tao L, Wei Y, et al. A novel poly (γ-glutamic acid)/silk-sericin hydrogel for wound dressing: synthesis, characterization and biological evaluation. Mater Sci Eng C. 2015;48:533–40.
Zielińska A, Karczewski J, Eder P, Kolanowski T, Szalata M, Wielgus K, et al. Scaffolds for drug delivery and tissue engineering: the role of genetics. J Control Release. 2023. https://doi.org/10.1016/j.jconrel.2023.05.042.
BenSaad LA, Kim KH, Quah CC, Kim WR, Shahimi M. Anti-inflammatory potential of ellagic acid, gallic acid and punicalagin A&B isolated from Punica granatum. BMC Complement Altern Med. 2017;17:1–10.
Yang DJ, Moh SH, Son DH, You S, Kinyua AW, Ko CM, et al. Gallic acid promotes wound healing in normal and hyperglucidic conditions. Molecules. 2016;21(7):899.
Singh MP, Gupta A, Sisodia SS. Wound healing activity of Terminalia bellerica Roxb. and gallic acid in experimentally induced diabetic animals. J Complement Integr Med. 2019;17(2):20190133.
Yin M, Wu J, Deng M, Wang P, Ji G, Wang M, et al. Multifunctional magnesium organic framework-based microneedle patch for accelerating diabetic wound healing. ACS Nano. 2021;15(11):17842–53.
Santos TS, Santos IDD, Pereira-Filho RN, Gomes SV, Lima-Verde IB, Marques MN, et al. Histological evidence of wound healing improvement in rats treated with oral administration of hydroalcoholic extract of Vitis labrusca. Curr Issues Mol Biol. 2021;43(1):335–52.
Jørgensen LN. Collagen deposition in the subcutaneous tissue during wound healing in humans: a model evaluation. APMIS Suppl. 2003;115:1–56.
Ajwee DM, Disi AM, Qunaibi EA, Taha MO. Ethosuximide and phenobarbital promote wound healing via enhancing collagenization. Chem Biol Drug Des. 2012;79(1):137–42.
de Souza TR, Rocha VL, Rincon GDCN, de Oliveira Junior ER, Celes MRN, Lima EM, et al. Topical application of melatonin accelerates the maturation of skin wounds and increases collagen deposition in a rat model of diabetes. J Tissue Viability. 2022;31(4):606–13.
Berman B, Maderal A, Raphael B. Keloids and hypertrophic scars: pathophysiology, classification, and treatment. Dermatol Surg. 2017;43:S3–18.
Konda S, Potter K, Ren VZ, Wang AL, Srinivasan A, Chilukuri S. Techniques for optimizing surgical scars, part 1: wound healing and depressed/atrophic scars. Skinmed. 2017;15(4):271–6.
Rittié L. Method for picrosirius red-polarization detection of collagen fibers in tissue sections. Fibrosis: methods and protocols. 2017:395–407.
Alves MC, Nascimento MF, de Almeida BM, Alves MM, Lima-Verde IB, Costa DS, et al. Hydrophilic scaffolds containing extracts of Stryphnodendron adstringens and Abarema cochliacarpa for wound healing: in vivo proofs of concept. Pharmaceutics. 2022;14(10):2150.
Wu Y-Z, Tsai Y-Y, Chang L-S, Chen Y-J. Evaluation of gallic acid-coated gold nanoparticles as an anti-aging ingredient. Pharmaceuticals. 2021;14(11):1071.
Rong Y, Cao B, Liu B, Li W, Chen Y, Chen H, et al. A novel gallic acid derivative attenuates BLM-induced pulmonary fibrosis in mice. Int Immunopharmacol. 2018;64:183–91.
** L, Sun S, Ryu Y, Piao ZH, Liu B, Choi SY, et al. Gallic acid improves cardiac dysfunction and fibrosis in pressure overload-induced heart failure. Sci Rep. 2018;8(1):9302.
Tabolacci C, Forni C, Jadeja RN, Facchiano F. Natural compounds against cancer, inflammation, and oxidative stress. BioMed Res Int. 2019;2019.
Dludla PV, Nkambule BB, Jack B, Mkandla Z, Mutize T, Silvestri S, et al. Inflammation and oxidative stress in an obese state and the protective effects of gallic acid. Nutrients. 2018;11(1):23.
Monika P, Waiker PV, Chandraprabha MN, Rangarajan A, Murthy KNC. Myofibroblast progeny in wound biology and wound healing studies. Wound Repair Regen. 2021;29(4):531–47.
Hosseinzadeh A, Mehrzadi S, Siahpoosh A, Basir Z, Bahrami N, Goudarzi M. The ameliorative effect of ellagic acid on di-(2-ethylhexyl) phthalate-induced testicular structural alterations, oxidative stress, inflammation and sperm damages in adult mice. Reprod Biol Endocrinol. 2021;19(1):146. https://doi.org/10.1186/s12958-021-00830-0.
Shahidi S, Komaki A, Raoufi S, Salehi I, Zarei M, Mahdian M. The anti-nociceptive effect of ellagic acid in streptozotocin-induced hyperglycemic rats by oxidative stress involvement. Basic Clin Neurosci. 2021;12(6):861–72. https://doi.org/10.32598/bcn.2021.2413.1.
Acknowledgements
E. B. Souto acknowledges FCT—Fundação para a Ciência e a Tecnologia, I.P., in the scope of the projects UIDP/04378/2020 and UIDB/04378/2020 of the Research Unit on Applied Molecular Biosciences—UCIBIO and the project LA/P/0140/2020 of the Associate Laboratory Institute for Health and Bioeconomy—i4HB.
Funding
Open access funding provided by FCT|FCCN (b-on). The research was funded by the National Council for Scientific and Technological Development (CNPq, Brazil).
Author information
Authors and Affiliations
Contributions
Marismar F. do Nascimento, Clauberto R. de Oliveira, Juliana C. Cardoso, Natalia C. T. Bordignon, Rogério Gondak, and Ricardo L. C. de Albuquerque Júnior contributed to the conceptualization, methodology, data validation, formal analysis, and investigation and for the writing of the first version of the manuscript. Patrícia Severino, Eliana B. Souto and Ricardo L. C. de Albuquerque Júnior contributed to literature review, software management, writing and reviewing the second version, project administration, resources, supervision, and funding acquisition. All authors have made a substantial contribution to the work. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This work raises ethics issues as part of the experiments run in animals. All the experimental procedures were implemented according to the National Animal Experiment Control Council for experiments in animals (CONCEA-Brazil), previously approved by the Ethical Committee for Animal Experimentation (approval #030915).
Consent to participate
Not applicable.
Consent for publication
All authors agreed with the final version of this manuscript and with the current submission.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
do Nascimento, M.F., de Oliveira, C.R., Cardoso, J.C. et al. UV-polymerizable methacrylated gelatin (GelMA)-based hydrogel containing tannic acids for wound healing. Drug Deliv. and Transl. Res. 13, 3223–3238 (2023). https://doi.org/10.1007/s13346-023-01383-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-023-01383-y