Abstract
Key points
SADIS with short common limb (< 250 cm) is a malabsorptive operation.
Reoperation is advised in patients requiring admission for severe malnutrition.
Elongation of the common channel is the preferred revisional technique
Introduction: Single-Anastomosis Duodeno-Ileal bypass with Sleeve gastrectomy (SADI-S) is a modification of the duodenal switch. Initial common channel’s length was 200, and after malnutrition was detected in some patients, it was elongated to 250 or 300 cm. The present study analyzes presentation and treatment of malnutrition after SADI-S. Materials: Three hundred and thirty-three consecutive patients undergoing SADI-S between May 2007 and February 2019 were included. The common limb length was 200 cm in 50 cases, 250 cm in 211, 300 in 71 and 350 in 1. Thirty-one patients were admitted for severe hypoalbuminemia and 17 patients were submitted to revisional surgery, and constitute the series of our study. Mean weight before reoperation was 57 kg and mean body mass index (BMI) was 21 kg/m2. Mean number of daily bowel movements was 5,6. Results: Mean time to reoperation was 56 months. The limb was found shorter than expected in 6 cases. Revisional surgery was conversion into a Roux en Y duodenal switch in 3 cases, elongation of the common limb in 11 patients, duodeno-duodenostomy in 1 and duodeno-jejunostomy to the first jejunal loop in 2. Mean weight regain was 14 kg, and mean final BMI 26 kg/m2. Daily bowel movements were reduced to 1,3. Factors related to hypoalbuminemia were hypertension, poor-controlled diabetes, shorter common limb and liver-test alterations. Conclusion: SADI-S is expected to be less malabsorptive than previous biliopancreatic diversions. However, caution must be taken with certain patients to avoid postoperative malnutrition. Adequate follow up with long-term supplementation is required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malnutrition is one of the most feared long-term complications of bariatric surgery. It has been historically related to malabsorptive operations, as jejunoileal bypass (JIB), biliopancreatic diversion (BPD) and duodenal switch (DS), although patients submitted to less aggressive techniques can also present some degrees of malnutrition. Single-Anastomosis Duodeno-Ileal bypass with Sleeve Gastrectomy (SADI-S) was introduced as a simpler alternative to the Duodenal Switch (DS) in which malabsorption was supposed to be milder because of the increase in the length of the common channel [1]. However, a high rate of nutritional problems presented in the first series of patients in which the common limb measured 200 cm. This led us to elongate the absorptive channel (250 to 300 cm) to ameliorate the malabsorptive effect of the operation [2]. The new longer common channel still showed good weight loss results in the long-term, whereas there was a reduction in the nutritional issues [3, 4]. Despite this greater absorption, some patients still present with hypoalbuminemia and other deficiencies [5], perhaps secondarily to a wrong selection, errors in the limb measurement or poor adherence to diet and supplementation. The management of malnourished patients can be difficult, and many times involves the revision of the technique. This seems to be easier in a one-limb operation when compared to Roux en Y configuration, but still the handling of a duodeno-intestinal anastomosis can be a concern for many surgeons.
In the present study, we review our experience on malnutrition after SADI-S and analyze the possible causes for this malnutrition, the markers that permit an early detection of these patients to avoid dreadful consequences, the current surgical solutions to improve their nutritional status and the outcomes after revisional surgery.
Patients and methods
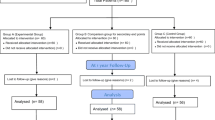
From May 2007 to February 2019, 333 consecutive patients (220 female) were submitted to SADI-S, either as a one-step surgery (273 cases) or as a second surgery after a previous bariatric operation (60 patients). The study was limited to patients operated before 2019 to warrant at least a 5 year follow up. The common limb was 200 cm in 50 cases, 250 cm in 211 cases, 300 cm in 71 and 350 in 1. Indications for SADI-S, surgical technique, supplementation and follow up have been reported previously [5]. The mean age was 47 years (21–71), mean weight 124 kg (61–216), and mean body mass index (BMI) 46.2 kg/m2 (24,7–76). One-hundred and sixty-one patients were diabetics, 58 under insulin treatment. Hypertension was present in 147 cases. Thirty-one patients (9,3%) were admitted for severe malnutrition. This was defined as low albumin levels plus edema, in the absence of an inflammation status, and not amenable for ambulatory management. Seventeen patients were submitted to revisional surgery (5,1%) and constitute the series of our study (Fig. 1, Flow Chart).
Statistics
Data are expressed by mean, range and standard error of the mean in case of normal distribution and median plus inter-quartile rank for non-normal distributions. Comparisons between the study series and the total SADI-S series are done with the t-test or the Kruskal Wallis test for numerical variables, and the chi-square test for categorical ones. Log-rank curves are built for significant continuous variables, and the Youden Index was used to discriminate the cut-off value.
Results
Follow up for the whole series was 85% at 5 years. Seventeen patients (5,1%) were reoperated. They were 6 men and 11 women, with a mean age at the index operation of 50,3 years (35 to 68), a mean initial weight of 118 kg (86 to 180), and a mean initial BMI of 44,1 kg/m2 (38–62). Type 2 diabetes was present in 11 patients, 8 under insulin treatment; 15 patients had hypertension (88%), 11 had dyslipidemia (69%), and 9 had sleep apnea (56%). One patient had been submitted to a previous bariatric operation, a sleeve gastrectomy. SADI-S had been performed with a 2-m common limb in 8 cases (8/50, 16% malnutrition rate for SADI-S 200), and with a 250 cm common limb in the other 9 patients (9/156, 4,3% malnutrition rate for SADI-S 250). No one had undergone SADI-S with a 3-m common limb.
Presentation
The mean time to first admission was 29 months, 3 months being the earliest one and 180 months the latest one. The mean number of hospital admissions before revision was 2 (0–5). Seven patients (41%) had the first episode requiring hospital admission in the first postoperative year, while 4 of them (23,5%) presented with malnutrition more than 5 years from surgery. In all patients with severe malnutrition, triggering causes were investigated — erratic feeding, malabsorption of bile salts (testing with 75Selenium-Homocholic Acid Taurine Scintigraphy—SeHCAT) or Small Intestine Bacterial Overgrowth (SIBO). Most patients responded to dietary education and oral nutritional supplementation, treatment with resin-cholestyramine or antibiotics in cases of suspected SIBO.
The mean time to reoperation was 56 months, from 16 to 186 months; 50% of the patients were reoperated in the first 3 postoperative years, and 37% of them beyond the 5th postoperative year.
Indication for reoperation was individualized, and different parameters influenced this decision, as were age, severity of the episode, psychiatric evaluation, social status, number of episodes, coexisting diseases, etc. The main cause for reoperation was severe malnutrition in most cases (12 patients). The mean (SD) total protein value was 5.3 (0.76) gr/dL, and mean albumin 2.6 (0.6) gr/dL, and all patients presented with edema in lower limbs and moderate to severe deficiencies in fat-soluble vitamins and minerals (zinc, selenium, and copper). Intractable diarrhea was present in some patients (four cases); there was one patient with severe hypocalcemia and 3 had developed liver failure, two secondary to alcohol consumption and one to viral hepatitis and cirrhosis (Table 1).
Mean age at reoperation was 55 years (32v71), mean weight 57 kg (46–74), mean BMI 21 kg/m2 (18,6–27) and mean total weight loss (TWL) 50,2% (32,7–68). All malnourished patients were previously eligible for nutritional support, including total parenteral nutrition in 7 cases, until an adequate nutritional status was achieved before surgery. The mean number of daily bowel movements was 5,6 [2,3,4,5,6,7,8,9,10].
Surgical findings
The common limb was measured in all cases. In patients with an initial SADI-S 200, in 6 cases, the measured length was 2 m; in 1 patient the limb was shorter, 170 cm, and in another one it was longer, 250 cm. In patients submitted to SADI-S 250, we found a correct common limb length in 4 cases, and a shorter one in the other 5 (230, 220, 200, 190 and 150 cm) (Table 1).
Surgical technique
The first three patients had a conversion into a Roux en Y DS through a division of the efferent limb just beyond the anastomosis, and the creation of a new anastomosis between this and the afferent 1 m proximal to the duodeno-ileostomy (Fig. 2). In this way, the three patients had a DS with an antiperistaltic alimentary limb (1 m) and a 2-m common limb. Three patients were submitted to a “total” reversal (1 case, end to end duodeno-duodenostomy) or an “almost-total” reversal, a duodeno-jejunostomy in the first jejunal loop (two cases). The other 11 patients were submitted to an elongation of the common limb through the division of the previous anastomosis and the creation of a new one more proximally, leaving a final common channel of 270 in one case, 300 cm in 3, 320 in 1 and 350 cm in 7 cases. A resizing of the sleeve gastrectomy over a 54 French bougie was performed along with the proximalization of the SADI-S in 3 cases; all three were suffering from severe diarrhea with no or mild hypoalbuminemia and had a very enlarged stomach (Table 1).
Scheme of the conversion of SADI-S to Roux en Y DS with an antiperistaltic alimentary limb. The efferent (common) limb has been divided close to the anastomosis and re-anastomosed to the afferent (biliopancreatic) limb 1 m proximal to the previous duodeno-ileostomy. The final operation has a 100 cm antiperistaltic alimentary limb and a 200 cm common limb
Outcome
After surgery, one patient with an advanced respiratory disease rejected ventilatory support and died. One patient with a Roux-en-Y DS was readmitted with an intestinal obstruction for an internal hernia, and was reoperated; intestinal resection was necessary, and she finally was converted into a Roux-en-Y Gastric Bypass. One patient with a Roux-en-Y DS with an antipersitaltic alimentary limb was reoperated 10 years later for gastro-ileal stasis with postprandial fullness and frequent regurgitation and vomiting. She was converted into a SADI-S with a 300 cm common limb.
Long-term results
In the long term the mean weight was 71 kg (44–89) with a mean weight regain of 14 kg from revisional surgery; the mean BMI was 26 kg/m2 (17–37), and the stool frequency was normalized, with mean number of bowel movements of 1,3 (0,5–4).
Factors related to malnutrition
Clinical and laboratory data of patients needing surgery for malnutrition were crossed with data from the complete series of patients submitted to SADI-S to find out which parameters could be related to the development of malnutrition. Results are presented in Table 2. The presence of hypertension, a low level of preoperative alkaline phosphatase, a higher level of aspartate aminotransferase (AST) and alanine aminotransferase (ALT), a shorter common limb and admission for undernutrition were all significantly related to the need of reoperation. In diabetics, a higher preoperative glycemia, a higher preoperative glycated hemoglobin (HbA1c) and the need of insulin therapy were related to malnutrition. A greater excess weight loss (EWL) in the first 6 and 12 months (EWL > 77% and EWL > 98%, respectively) was also related to severe malnutrition (area under the curve 0,771 and 0,763). No relationship was observed with the presence of steatosis in the pathologic study of the liver.
Discussion
SADI-S is a safe operation for selected patients with adequate follow up and life-long supplementation [4]. However, despite being apparently safer than prior malabsorptive operations as BPD and DS, some patients can experience malnutrition, a life-threatening condition that must be avoided or early detected and treated [5].
The main findings of this review of our experience are that a short common channel (200 cm) is followed by a high rate of severe malnutrition; that errors in the measurement of the small bowel may also lead to malnutrition; and that there are some patients who can be especially vulnerable, as those with hypertension and poor-controlled type-2 diabetes and patients with alterations in the liver tests. Clinicians must be aware when patients lose weight too rapidly, have more severe diarrhea, or their laboratory tests are significantly altered in the first postoperative year, as they are all markers of malnutrition.
The initial operation with a common channel of 2 m was abandoned in 2009 because of the high incidence of malnutrition [2]. The simple increase in 50 cm did not affect the good results on weight loss, and, on the other hand, increased the safety of the operation [5]. To achieve a secure technique, the measurement of the ileum must be accurate enough, either if it is done with marked graspers or if it is performed with a tape of known length [6, 7]. In all the patients included, measurement of the bowel in the first operation had been performed with a grasper marked at 10 cm from the tip. We also recommend measuring the bowel after relaxing the smooth muscle with intravenous Buscopan®, as the stretching of the small bowel has demonstrated to obtain more accurate measurements [8].
Seventy-five percent of the patients had severe protein malnutrition, according to screening questionnaires [Malnutrition Universal Screening Tool (MUST), Nutritional Risk Screening-2002 (NRS-2000) or The Global Leadership Initiative on Malnutrition (GLIM)] [9], and confirmation by low levels of serum proteins and edema, in absence of inflammation (C-reactive protein < 2 mg/dL). Furthermore, patients presented symptoms of muscular weakness suggestive of sarcopenia. Inflammation is a relevant issue for the correct diagnosis of malnutrition as its presence detracts significance to albumin levels [10].
Some bariatric surgery studies have evaluated this clinical condition using the Controlling Nutritional Status (CONUT) score, where malnutrition parameters (serum albumin and cholesterol) are combined with immunologic parameters (total lymphocyte count), to provide additional information on malnutrition related to disease [11].
We did not find a significant association between older age and malnutrition. Cossu et al. [12] reviewed the importance of age on malnutrition in patients submitted to BPD, finding that the group of patients older than 55 years had a 16% rate of malnutrition and an 8% rate of revisional surgery. The authors outlined the difficulty of aged patients in changing alimentary habits after surgery and the clinical importance of some disorders related to aging, as it is loss of appetite, the impaired sense of taste, the lack of teeth and therefore good mastication and sometimes even depression.
We found that hypertension was more prevalent between reoperated patients, as well as higher preoperative values of glycemia and HbA1c. Hypertension and poor control of diabetes, defined by HbA1c above 7% or high glycemia are both related to atherosclerosis, which along with age could be the cause of an impaired intestinal absorption and a decreased adaption capacity of the small bowel. Although there are no studies on microvascularization of the small bowel and nutrition, atherosclerosis has been previously related to malnutrition in patients with peripheral arterial disease [13].
We find no clear explanation to the relationship between a low preoperative alkaline phosphatase (AP) and malnutrition; low AP levels are related to low zinc and magnesium levels, what is seen in malnutrition. Unfortunately, we do not routinely analyze them preoperatively, so we cannot establish a connection between them. Although we didn’t find a correlation between the liver biopsy and malnutrition, alteration of liver tests, AP, AST and ALT, were all related to malnutrition. Liver disease, obesity, weight loss and malnutrition are intimately related. Non-alcoholic fatty liver disease (NAFL) improves after a successful weight loss operation. However, when weight loss happens too fast, the loss of adipose tissue leads to a massive mobilization of free fatty acids that reach the liver and provoke hepatotoxicity. This is compensated by the reduction of liver fat caused by the weight loss [14]. But when other mechanisms are present, as protein malnutrition or deficiency of specific amino acids, or bacterial overgrowth, this toxicity can lead to a liver failure. Bacterial overgrowth is not supposed to happen after SADI-S, because there is not a real blind loop, as it was in old malabsorptive operations. Nevertheless, the mere absence of nutrients in an intestinal loop is enough to induce a substantial change in the jejunal microbiota [15], and this can have dramatic consequences in patients with liver disease. Patients with an underlying liver disease should never be offered this type of surgery because of the risk of hepatic insufficiency [16] that on some occasion has led to the need of liver transplantation [17].
Surgeons and endocrinologists should be specially alerted when weight loss is too fast in the first postoperative year, or when there is a high number of bowel movements. These patients have to be tested for micronutrient or protein insufficiency before clinical manifestations and treated with supplementation of protein and vitamins.
Regarding the revisional technique, we initially introduced the Roux-en-Y configuration with the antiperistaltic alimentary limb to avoid touching the previous duodeno-ileostomy. When we demonstrated the feasibility of dividing the anastomosis and performing a new duodeno-enterostomy without affecting the pylorus function, the initial technique was abandoned. Certainly, its results were not very good. The opening of the mesentery favored an internal hernia in one case, and the antipersitaltic Roux limb jeopardized gastric emptying and originated severe reflux and regurgitation in another one. As a rule we first measure the biliary and the common limb, to know if the cause of malnutrition was an error of the first operation, and to assess how long can the proximalization be done. Then, 100 to 150 cm are usually added to the common limb, placing the new anastomosis at 300 to 350 cm from the ilio-cecal junction. When there is a severe underlying disease, as happened with the psychiatric patient and with those suffering from liver failure, the new anastomosis is placed in the first jejunal loop or even in the duodenum, restoring an almost normal anatomy.
In summary, SADI-S is an effective and safe operation when the selection of patients, the performance of the operation and the supplementation and follow up are correct. Older patients, patients with hypertension, lower BMI, or poor-controlled diabetes, as well as those with severe accompanying conditions or those with problems of adherence to supplementation and follow up should not undergo SADI-S 250. Limitations of this study are the single institution experience, the retrospective nature of the study, the short number of patients and the heterogeneity of the series.
Ethics statement
For this type of study, formal consent is not required. The authors declare that they have no conflicts of interest regarding this manuscript.
Data availability
The data that support the findings of this study are not openly available due to local data protection restrictions but are available from the corresponding author upon reasonable request.
References
Sánchez-Pernaute A, Rubio Herrera MA, Pérez-Aguirre E, García Pérez JC, Cabrerizo L, Díez Valladares L, Fernández C, Talavera P, Torres A (2007) Proximal duodenal-ideal end-to-side bypass with sleeve gastrectomy: proposed technique. Obes Surg 17:1614–1618. https://doi.org/10.1007/s11695-007-9287-8
Sánchez-Pernaute A, Rubio MA, Pérez Aguirre E, Barabash A, Cabrerizo L, Torres A (2013) Single-anastomosis duodenoileal bypass with sleeve gastrectomy: metabolic improvement and weight loss in first 100 patients. Surg Obes Relat Dis 9:731–735. https://doi.org/10.1016/j.soard.2012.07.018
Gagner M (2016) Hypoabsorption not malabsorption, hypoabsorptive surgery and not malabsorptive surgery. Obes Surg 26:2783–2784. https://doi.org/10.1007/s11695-016-2350-6
Vilallonga R, Balibrea JM, Curell A, Gonzalez O, Caubet E, Ciudin A, Ortiz-Zúñiga AM, Fort JM (2017) Technical options for malabsorption issues after single anastomosis duodenoileal bypass with sleeve gastrectomy. Obes Surg 27:3344–3348. https://doi.org/10.1007/s11695-017-2931-z
Sánchez-Pernaute A, Rubio Herrera MA, Pérez Ferré N, Sáez Rodríguez C, Marcuello C, Pañella C, López Antoñanzas L, Torres A, Pérez-Aguirre E (2022) Long-term results of single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). Obes Surg 32:682–689. https://doi.org/10.1007/s11695-021-05879-9
Wagner M, Mayer BFB, Bodenstedt S, Kowalewski K, Nickel F, Speidel S, Fischer L, Kenngott HG, Müller-Stich B (2021) Comparison of conventional methods for bowel length measurement in laparoscopic surgery to a novel computer-assisted 3D measurement system. Obes Surg 31:4692–4700. https://doi.org/10.1007/s11695-021-05620-6
Slagter N, van Wilsum M, de Heide LJM, Jutte EH, Kaiser MA, Damen SL, van Beek AP, Emous M (2022) Laparoscopic small vowel length measurement in bariatric surgery using a hand-over-hand technique with marked graspers: an ex vivo experiment. Obes Surg 32:1201–1208. https://doi.org/10.1007/s11695-022-05918-z
Karagül S, Kayaalp C (2019) Repeated stretched or non-stretched small bowel length measurements in healthy individuals. Turk J Surg 35:1–5. https://doi.org/10.5152/turkjsurg.2018.4087
Cederholm T, Jensen GL, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, Baptista G, Barazzoni R, Blaauw R, Coats AJS, Crivelli AN, Evans DC, Gramlich L, Fuchs-Tarlovsky V, Keller H, Llido L, Malone A, Mogensen KM, Morley JE, Muscaritoli M, Nyulasi I, Pirlich M, Pisprasert V, de van der Schueren MAE, Siltharm S, Singer P, Tappenden K, Velasco N, Waitzberg D, Yamwong P, Yu J, Van Gossum A, Compher C, GLIM Core Leadership Committee, GLIM Working Group (2019) GLIM criteria for the diagnosis of malnutrition - A consensus report from the global clinical nutrition community. J Cachexia Sarcopenia Muscle 10:207–217. https://doi.org/10.1002/jcsm.12383
Cederholm T, Jensen GL, Ballesteros-Pomar MD, Blaauw R, Correia MITD, Cuerda C, Evans DC, Fukushima R, Ochoa Gautier JB, Gonzalez MC, van Gossum A, Gramlich L, Hartono J, Heymsfield SB, Jager-Wittenaar H, Jayatissa R, Keller H, Malone A, Manzanares W, McMahon MM, Mendez Y, Mogensen KM, Mori N, Muscaritoli M, Nogales GC, Nyulasi I, Phillips W, Pirlich M, Pisprasert V, Rothenberg E, de van der Schueren M, Shi HP, Steiber A, Winkler MF, Barazzoni R, Compher C (2023) Guidance for assessment of the inflammation etiologic criterion for the GLIM diagnosis of malnutrition: a modified Delphi approach. Clin Nutr 43:1025–1032. https://doi.org/10.1016/j.clnu.2023.11.026
Gentileschi P, Siragusa L, Alicata F, Campanelli M, Bellantone C, Musca T, Bianciardi E, Arcudi C, Benavoli D, Sensi B (2022) Nutritional Status after Roux-En-Y (Rygb) and One Anastomosis Gastric Bypass (Oagb) at 6-Month Follow-Up: A Comparative Study. Nutrients 14:2823. https://doi.org/10.3390/nu14142823
Cossu ML, Fais E, Meloni GB, Profili S, Masala A, Alagna S, Rovasio PP, Spartà C, Pilo L, Tilocca PL, Noya G (2004) Impact of age on long-term complications after biliopancreatic diversion. Obes Surg 14:1182–1186. https://doi.org/10.1381/0960892042387093
Carvalho J, Correia MA, Kanegusuku H, Longano P, Wolosker N, Ritti-Dias RM, Cucato GG (2022) Association between the risk of malnutrition and functional capacity in patients with peripheral arterial disease: a cross-sectional study. PLoS ONE 17:e0273051. https://doi.org/10.1371/journal.pone.0273051
Vespasiani-Gentilucci U, Vorini F, Carotti S, De Vincentis A, Galati G, Gallo P, Scopinaro N, Picardi A (2017) Hepatic complications of bariatric surgery: the reverse side of the coin. Acta Gastroenterol Belg 80:505–513
Prakash G, Drenick EJ, Wexler H, Delucia L, Finegold SM (2018) Microbial flora in the bypassed jejunum of patients with biliopancreatic bypass for obesity. Am J Clin Nutr 46:273–276
Kirkpatrick V, Moon RC, Teixeira AF, Jawad MA (2018) Cirrhosis following single anastomosis duodeno-ileal switch: a case report. Int J Surg Case Rep 45:130–132. https://doi.org/10.1093/ajcn/46.2.273
Addeo P, Cesaretti M, Anty R, Iannelli A (2019) Liver transplantation for bariatric surgery-related liver failure: a systematic review of a rare condition. Surg Obes Relat Dis 15:1394–1401. https://doi.org/10.1016/j.soard.2019.06.002
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Andrés Sánchez-Pernaute, Bibiana Lasses and Elia Pérez-Aguirre. The first draft of the manuscript was written by Andrés Sánchez-Pernaute, Elia Pérez-Aguirre and Miguel Ángel Rubio, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sánchez-Pernaute, A., Lasses, B., Antoñanzas, L.L. et al. Revisional surgery for malnutrition after SADI-S: prevalence, indications, techniques and outcomes. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01900-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01900-9