Abstract
Introduction
The post-COVID-19 condition (PCC) is characterized by persistent, distressing symptoms following an acute COVID-19 infection. These symptoms encompass various domains, including hedonic tone, which is critical for overall well-being. Furthermore, obesity is both a risk factor for COVID-19 and PCC and associated with impaired hedonic tone. This study aims to investigate whether elevated body mass index (BMI) is associated with hedonic tone in persons with PCC.
Methods
We perform a post hoc analysis of a randomized, double-blind, placebo-controlled clinical trial investigating the impact of vortioxetine on cognitive impairment in persons with PCC. Statistical analysis of baseline data using a generalized linear model was undertaken to determine the relationship of BMI to hedonic tone measured by Snaith-Hamilton Pleasure Scale (SHAPS) scores. The model was adjusted for covariates including age, sex, race, suspected versus confirmed COVID-19 cases, alcohol amount consumed per week, and annual household income.
Results
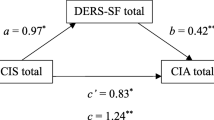
The baseline data of 147 participants were available for analysis. BMI had a statistically significant positive association with baseline SHAPS total scores (β = 0.003, 95% CI [6.251E-5, 0.006], p = 0.045), indicating elevated BMI is associated with deficits in self-reported reward system functioning.
Conclusion
Higher BMI is associated with greater deficits in hedonic tone in persons with PCC, which may impact reward functioning processes such as reward prediction and processing. The mediatory effect of BMI on reward function underscores the need to investigate the neurobiologic interactions to elucidate preventative and therapeutic interventions for persons with PCC. Therapeutic development targeting debilitating features of PCC (e.g., motivation, cognitive dysfunction) could consider stratification on the basis of baseline BMI.
Trial Registration Number
NCT05047952.

Similar content being viewed by others
Data Availability
The data presented in this study are available on request from the corresponding author.
References
World Health Organization. WHO coronavirus (COVID-19) dashboard [Internet]. WHO; 2023.
Vimercati L, de Maria L, Quarato M, et al. Association between long COVID and Overweight/Obesity. J Clin Med. 2021;10(18):4143. https://doi.org/10.3390/jcm10184143.
Quinn KL, Katz GM, Bobos P, et al. Understanding the post COVID-19 condition (long COVID) in adults and the expected burden for Ontario. Ont COVID-19 Sci Advis Table. 2022. https://doi.org/10.47326/ocsat.2022.03.65.1.0.
Soriano JB, Murthy S, Marshall JC, et al. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2022;22(4):e102–7. https://doi.org/10.1016/S1473-3099(21)00703-9.
Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of long COVID. Nat Med. 2021;27(4):626–31. https://doi.org/10.1038/s41591-021-01292-y.
Lechner-Scott J, Levy M, Hawkes C, et al. Long covid or post covid-19 syndrome. Mult Scler Relat Disord. 2021;55: 103268. https://doi.org/10.1016/j.msard.2021.103268.
Visco V, Vitale C, Antonella R, et al. Post-COVID-19 syndrome: involvement and interactions between respiratory, cardiovascular and nervous systems. J Clin Med. 2022;11(3):524. https://doi.org/10.3390/jcm11030524.
Tsampasian V, Elghazaly H, Chattopadhyay R, et al. Risk factors associated with post-COVID-19 condition: a systematic review and meta-analysis. JAMA Intern Med. 2023;183(6):566–80. https://doi.org/10.1001/jamainternmed.2023.0750.
Ryan RM, Huta V, Deci EL. Living well: a self-determination theory perspective on eudaimonia. J Happiness Stud. 2008;9:139–70. https://doi.org/10.1007/s10902-006-9023-4.
Lamontagne SJ, Winters MF, Pizzagalli DA, Olmstead MC. Post-acute sequelae of COVID-19: evidence of mood and cognitive impairment. Brain Behav Immun Health. 2021;17: 100347. https://doi.org/10.1016/j.bbih.2021.100347.
Mazza MG, Palladini M, Poletti S, Benedetti F. Post-COVID-19 depressive symptoms: epidemiology, pathophysiology, and pharmacological treatment. CNS Drugs. 2022;36(7):681–702. https://doi.org/10.1007/s40263-022-00931-3.
Cho J, Goldenson NI, Pester MS, et al. Longitudinal associations between anhedonia and BMI trajectory groups among adolescents. J Adolesc Health. 2018;63(1):81–7. https://doi.org/10.1016/j.jadohealth.2017.12.022.
Reyes S, Rimkus CDM, Lozoff B, et al. Assessing cognitive control and the reward system in overweight young adults using sensitivity to incentives and white matter integrity. PLoS ONE. 2020;15(6):e0233915. https://doi.org/10.1371/journal.pone.0233915.
He R, Zheng R, Zheng J, et al. Causal association between obesity, circulating glutamine levels, and depression: a mendelian randomization study. J Clin Endocrinol Metab. 2023;108(6):1432–41. https://doi.org/10.1210/clinem/dgac707.
Singh R, Rathore SS, Khan H, et al. Association of obesity with COVID-19 severity and mortality: an updated systemic review, meta-aanalysis, and meta-regression. Front Endocrinol. 2022;13: 780872. https://doi.org/10.3389/fendo.2022.780872.
Theoharides TC, Steward JM, Hatziagelaki E, et al. Brain “fog”, inflammation and obesity: key aspects of neuropsychiatric disorders improved by luteolin. Front Neurosci. 2015;9:225. https://doi.org/10.3389/fnins.2015.00225.
Di Nicola M, Pepe M, Montanari S, et al. Vortioxetine improves physical and cognitive symptoms in patients with post-COVID-19 major depressive episodes. Eur Neuropsychopharmacol. 2023;70:21–8. https://doi.org/10.1016/j.euroneuro.2023.02.006.
Brain and Cognition Discovery Foundation. Randomized, Double-Blinded, Placebo-Controlled Clinical Trial Evaluating Vortioxetine for Cognitive Deficits in Persons with Post-COVID-19 Condition. ClinicalTrials.gov identifier: NCT05047952. 2022. https://clinicaltrials.gov/ct2/show/NCT05047952. Accessed 05 April 2023.
McIntyre RS, Phan L, Kwan ATH, et al. Vortioxetine for the treatment of post-COVID-19 condition: a randomized controlled trial. Brain. 2023. https://doi.org/10.1093/brain/awad377.
International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH). Integrated Addendum to ICH E6(R1): Guideline for Good Clinical Practice. 2016. https://database.ich.org/. Accessed 25 Sep 2023.
WMA: The World Medical Association-Declaration of Helsinki. 2008. https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/doh-oct2008/. Accessed 25 Sep 2023.
Snaith RP, Hamilton M, Morley S, et al. A scale for the assessment of hedonic tone the Snaith-Hamilton pleasure scale. Br J Psychiatry. 1995;167(1):99–103. https://doi.org/10.1192/bjp.167.1.99.
Defining Adult Overweight and Obesity [Internet]. Centers for Disease Control and Prevention. 2023. https://www.cdc.gov/obesity/basics/adult-defining.html. Accessed 01 April 2023.
Snaith-Hamilton pleasure scale [Internet]. 2023. https://datashare.nida.nih.gov/instrument/snaith-hamilton-pleasure-scale. Accessed 20 Nov 2023.
Ribeiro G, Camacho M, Santos O, et al. Association between hedonic hunger and body-mass index versus obesity status. Sci Rep. 2018;8:5857. https://doi.org/10.1038/s41598-018-23988-x.
Gill H, Gill B, Lipsitz O, et al. The impact of overweight/obesity on monetary reward processing: a systematic review. J Psychiatr Res. 2021;137:456–64.
Volkow ND, Wang GJ, Baler RD. Reward, dopamine and the control of food intake: implications for obesity. Trends Cogn Sci. 2011;15(1):37–46. https://doi.org/10.1016/j.tics.2010.11.001.
Meemken MT, Kube J, Wickner C, Horstmann A. Kee** track of promised rewards: Obesity predicts enhanced flexibility when learning from observation. Appetite. 2018;131:117–24. https://doi.org/10.1016/j.appet.2018.08.029.
Mansur RB, Subramaniapillai M, Zuckerman H, et al. Effort-based decision-making is affected by overweight/obesity in major depressive disorder. J Affect Disord. 2019;256:221–7. https://doi.org/10.1016/j.jad.2019.06.002.
Rodriguez LR, Rasmussen EB, Kyne-Rucker D, et al. Delay discounting and obesity in food insecure and food secure women. Health Psychol. 2021;40(4):242–51. https://doi.org/10.1037/hea0001042.
Barlow P, Reeves A, McKee M, et al. Unhealthy diets, obesity and time discounting: a systematic literature review and network analysis. Obes Rev. 2016;17(9):810–9. https://doi.org/10.1111/obr.12431.
Tang J, Chrzanowski-Smith OJ, Hutchinson G, et al. Relationship between monetary delay discounting and obesity: a systematic review and meta-regression. Int J Obes. 2019;43(6):1135–46. https://doi.org/10.1038/s41366-018-0265-0.
Ceban F, Ling S, Lui LMW, et al. Fatigue and cognitive impairment in Post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav Immun. 2022;101:93–135. https://doi.org/10.1016/j.bbi.2021.12.020.
Rosenman R, Tennekoon V, Hill LG. Measuring bias in self-reported data. Int J Behav Healthc Res. 2011;2(4):320–32. https://doi.org/10.1504/IJBHR.2011.043414.
Medical Writing and Editorial Assistance
No medical writing or editorial assistance was used for this article.
Funding
The study was sponsored by Brain Cognition Discovery Foundation (BCDF) as part of an unrestricted research grant provided by H. Lundbeck A/S, Copenhagen, Denmark. The BCDF is a not-for-profit research organization. No funding or sponsorship was received for the publication fees.
Author information
Authors and Affiliations
Contributions
Study conception and design of the primary study, a randomized controlled study was performed by Roger S McIntyre. Study conception and design of the current study was performed by Gia Han Le and Roger S McIntyre. Material preparation, data collection and analysis were performed by Gia Han Le and Angela T.H. Kwan. The first draft of the manuscript was written by Gia Han Le and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Roger S. McIntyre has received research grant support from CIHR, GACD, National Natural Science Foundation of China (NSFC), and the Milken Institute; speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, Abbvie, and Atai Life Sciences. Dr. Roger McIntyre is a CEO of Braxia Scientific Corp. Dr. Taeho Greg Rhee was supported in part by the National Institute on Aging (NIA) (#R21AG070666; R21AG078972), National Institute of Mental Health (#R21MH117438), National Institute on Drug Abuse (#R21DA057540) and Institute for Collaboration on Health, Intervention, and Policy (InCHIP) of the University of Connecticut. Dr. Rhee serves as a review committee member for Patient-Centered Outcomes Research Institute (PCORI) and Substance Abuse and Mental Health Services Administration (SAMHSA) and has received honoraria payments from PCORI and SAMHSA. Dr. Rhee has also served as a stakeholder/consultant for PCORI and received consulting fees from PCORI. Dr. Rhee serves as an advisory committee member for International Alliance of Mental Health Research Funders (IAMHRF). Dr. Rhee is currently a co-Editor-in-Chief of Mental Health Science and has received honorarium payments annually from the publisher, John Wiley & Sons, Inc. Dr. Roger Ho has received funding from the National University of Singapore iHeathtech Other Operating Expenses (A-0001415-09-00). Kayla M. Teopiz and Mehala Subramaniapillai have received personal fees from Braxia Scientific Corp. Dr. Joshua D. Rosenblat has received research grant support from the Canadian Institute of Health Research (CIHR), Physician Services Inc (PSI) Foundation, Labatt Brain Health Network, Brain and Cognition discovery Foundation (BCDF), Canadian Cancer Society, Canadian Psychiatric Association, Academic Scholars Award, American Psychiatric Association, American Society of Psychopharmacology, University of Toronto, University Health Network Centre for Mental Health, Joseph M. West Family Memorial Fund and Timeposters Fellowship and industry funding for speaker/consultation/research fees from iGan, Boehringer Ingelheim, Janssen, Allergan, Lundbeck, Sunovion and COMPASS. Gia Han Le, Angela T.H. Kwan, Ziji Guo, Sabrina Wong, Sebastian Badulescu, Shakila Meshkat, Giacomo d’Andrea, Lee Phan, and Rodrigo B. Mansur have nothing to disclose.
Ethical Approval
The study was conducted in adherence to the guidelines of Good Clinical Practice [20] and Declaration of Helsinki [21]. The study protocol was approved by a local research ethics board (REB), specifically Advarra Institutional Review Board (IRB) (IRB#00000971). See Sect. 2.1. “Recruitment and Ethics”.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Le, G.H., Kwan, A.T.H., Wong, S. et al. Impact of Elevated Body Mass Index (BMI) on Hedonic Tone in Persons with Post-COVID-19 Condition: A Secondary Analysis. Adv Ther 41, 686–695 (2024). https://doi.org/10.1007/s12325-023-02760-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02760-2