Abstract
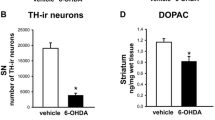
The gut-brain axis plays an important role in Parkinson’s disease (PD) by acting as a route for vagal propagation of aggregated α-synuclein in the gut-first endophenotype and as a mediator of gastrointestinal dyshomeostasis via the nigro-vagal pathway in the brain-first endophenotype of the disease. One important mechanism by which the gut-brain axis may promote PD is by regulating gastrointestinal redox homeostasis as overwhelming evidence suggests that oxidative stress plays a key role in the etiopathogenesis and progression of PD and the gastrointestinal tract maintains redox homeostasis of the organism by acting as a critical barrier to environmental and microbiological electrophilic challenges. The present aim was to utilize the bilateral intrastriatal 6-hydroxydopamine (6-OHDA) brain-first PD model to study the effects of isolated central pathology on redox homeostasis of the gastrointestinal tract. Three-month-old male Wistar rats were either not treated (intact controls; CTR) or treated bilaterally intrastriatally with vehicle (CIS) or 6-OHDA (6-OHDA). Motor deficits were assessed with the rotarod performance test, and the duodenum, ileum, and colon were dissected for biochemical analyses 12 weeks after the treatment. Lipid peroxidation, total antioxidant capacity, low-molecular-weight thiols, and protein sulfhydryls, the activity of total and Mn/Fe superoxide dismutases, and total and azide-insensitive catalase/peroxidase were measured. Both univariate and multivariate models analyzing redox biomarkers indicate that significant disturbances in gastrointestinal redox balance are not present. The findings demonstrate that motor impairment observed in the brain-first 6-OHDA model of PD can occur without concurrent redox imbalances in the gastrointestinal system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is a chronic progressive neurodegenerative condition characterized by the degeneration of dopaminergic neurons in substantia nigra (SN) pars compacta that results in the development of bradykinesia, tremor at rest, rigidity, and postural instability [1]. Although the etiopathogenesis of the disease remains to be elucidated accumulating evidence points to the involvement of the gastrointestinal tract as (i) the prodromal non-motor symptoms affecting the gastrointestinal tract (e.g., dysphagia, delayed gastric emptying, and constipation) are prevalent and precede the motor phase of PD (sometimes by decades) [2,3,4]; (ii) a stereotypical spreading pattern of α-synuclein pathology [5, 6] supports the hypothesis that misfolded α-synuclein may originate from the gut [7]; and (iii) mechanistic animal studies clearly demonstrate that pathophysiological events in the gastrointestinal tract are sufficient to trigger and promote the development of the central nervous system (CNS) pathology resembling PD (e.g., [8,9,10,11]). Based on the aforementioned evidence a body-first hypothesis of PD has been proposed with the gastrointestinal tract considered the most likely site of early molecular pathophysiological events [12].
In contrast, some studies suggest that in a considerable proportion of patients, PD does not propagate in concordance with the Braak staging system [13, 14]. Furthermore, although highly prevalent, gastrointestinal symptoms are not present in all patients diagnosed with PD, and they do not always appear before the onset of motor symptoms [2, 15]. Consequently, it is evident that in some patients a brain-first hypothesis provides a more accurate explanation of the PD progression.
Based on the aforementioned data, a working model has been proposed which recognizes PD as a complex disease composed of at least two clusters of phenotypes (brain-first and gut-first) [12, 16]. The gut-brain axis plays an important role in both subtypes acting as a route for vagal propagation of aggregated α-synuclein in the gut-first phenotype and as a mediator of gastrointestinal dyshomeostasis via the nigro-vagal pathway in the brain-first phenotype (e.g., [17]). Nevertheless, the mechanisms by which the gut-brain axis may contribute to the propagation of the disease and the appearance of gastrointestinal symptoms remain poorly understood and challenging to study due to overlap** brain and gut pathology in animal models.
In this context, the CNS-targeted 6-hydroxydopamine (6-OHDA) rodent models provide a unique way to study the effects of the brain-first predominant subtype of the disease on the pathophysiological alterations in the gut as the toxin cannot cross the blood-brain barrier. The central 6-OHDA administration model was first introduced by Ungerstedt following the idea that high selectivity of the toxin towards the dopamine uptake sites may result in a specific nigrostriatal dopaminergic lesion [18]. Since its introduction, the model was widely used for investigating many aspects of PD as it successfully recapitulates several important features observed in patients suffering from the idiopathic form of the disease: (i) administration of 6-OHDA mimics increased oxidative stress in dopaminergic neurons found in PD [19, 20]; (ii) SN pars compacta that shows the greatest susceptibility to 6-OHDA-induced injury is also the most affected area in PD patients [21]; (iii) 6-OHDA toxicity can be facilitated with iron [22] and iron dyshomeostasis plays an important role in the etiopathogenesis and progression of PD [23,24,25,26,27,28]; (iv) 6-OHDA is produced in physiological conditions upon oxidation of dopamine and it is present in the urine of patients suffering from PD. Consequently, it is possible that endogenous 6-OHDA may be involved in the etiopathogenesis of PD in humans [29, 30].
Some groups already utilized the model to study the mechanisms of gastrointestinal dyshomeostasis in the context of the brain-first PD-like nigrostriatal lesion primarily with a focus on gastrointestinal motility (e.g., [31,32,85,86,87] may have provided a different insight.
Data Availability
Raw data can be obtained from the corresponding author. The manuscript has been preprinted on bioRxiv [88].
References
Poewe W, Seppi K, Tanner CM et al (2017) Parkinson disease. Nat Rev Dis Primers 3:17013. https://doi.org/10.1038/nrdp.2017.13
Fu P, Gao M, Yung KKL (2020) Association of intestinal disorders with Parkinson’s disease and Alzheimer’s disease: a systematic review and meta-analysis. ACS Chem Neurosci 11:395–405. https://doi.org/10.1021/acschemneuro.9b00607
Travagli RA, Browning KN, Camilleri M (2020) Parkinson disease and the gut: new insights into pathogenesis and clinical relevance. Nat Rev Gastroenterol Hepatol 17:673–685. https://doi.org/10.1038/s41575-020-0339-z
Skjærbæk C, Knudsen K, Horsager J, Borghammer P (2021) Gastrointestinal dysfunction in Parkinson’s disease. J Clin Med 10:493. https://doi.org/10.3390/jcm10030493
Braak H, Del Tredici K, Rüb U et al (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211. https://doi.org/10.1016/s0197-4580(02)00065-9
Braak H, Rüb U, Gai WP, Del Tredici K (2003) Idiopathic Parkinson’s disease: possible routes by which vulnerable neuronal types may be subject to neuroinvasion by an unknown pathogen. J Neural Transm (Vienna) 110:517–536. https://doi.org/10.1007/s00702-002-0808-2
Braak H, de Vos RAI, Bohl J, Del Tredici K (2006) Gastric alpha-synuclein immunoreactive inclusions in Meissner’s and Auerbach’s plexuses in cases staged for Parkinson’s disease-related brain pathology. Neurosci Lett 396:67–72. https://doi.org/10.1016/j.neulet.2005.11.012
Kim S, Kwon S-H, Kam T-I et al (2019) Transneuronal propagation of pathologic α-synuclein from the gut to the brain models Parkinson’s disease. Neuron 103:627–641.e7. https://doi.org/10.1016/j.neuron.2019.05.035
Challis C, Hori A, Sampson TR et al (2020) Gut-seeded α-synuclein fibrils promote gut dysfunction and brain pathology specifically in aged mice. Nat Neurosci 23:327–336. https://doi.org/10.1038/s41593-020-0589-7
Espinosa-Oliva AM, Ruiz R, Soto MS et al (2022) Inflammatory bowel disease induces α-synuclein aggregation in gut and brain. bioRxiv preprint 2022.01.26.477259. https://doi.org/10.1101/2022.01.26.477259
Liu W, Lim K-L, Tan E-K (2022) Intestine-derived α-synuclein initiates and aggravates pathogenesis of Parkinson’s disease in Drosophila. Transl Neurodegener 11:44. https://doi.org/10.1186/s40035-022-00318-w
Van Den Berge N, Ulusoy A (2022) Animal models of brain-first and body-first Parkinson’s disease. Neurobiol Dis 163:105599. https://doi.org/10.1016/j.nbd.2021.105599
Parkkinen L, Pirttilä T, Alafuzoff I (2008) Applicability of current staging/categorization of alpha-synuclein pathology and their clinical relevance. Acta Neuropathol 115:399–407. https://doi.org/10.1007/s00401-008-0346-6
Attems J, Jellinger KA (2008) The dorsal motor nucleus of the vagus is not an obligatory trigger site of Parkinson’s disease. Neuropathol Appl Neurobiol 34:466–467. https://doi.org/10.1111/j.1365-2990.2008.00937.x
Cersosimo MG, Raina GB, Pecci C et al (2013) Gastrointestinal manifestations in Parkinson’s disease: prevalence and occurrence before motor symptoms. J Neurol 260:1332–1338. https://doi.org/10.1007/s00415-012-6801-2
Borghammer P, Van Den Berge N (2019) Brain-first versus gut-first Parkinson’s disease: a hypothesis. J Parkinsons Dis 9:S281–S295. https://doi.org/10.3233/JPD-191721
Garrido-Gil P, Rodriguez-Perez AI, Dominguez-Meijide A et al (2018) Bidirectional neural interaction between central dopaminergic and gut lesions in Parkinson’s disease models. Mol Neurobiol 55:7297–7316. https://doi.org/10.1007/s12035-018-0937-8
Ungerstedt U (1968) 6-Hydroxy-dopamine induced degeneration of central monoamine neurons. Eur J Pharmacol 5:107–110. https://doi.org/10.1016/0014-2999(68)90164-7
Trist BG, Hare DJ, Double KL (2019) Oxidative stress in the aging substantia nigra and the etiology of Parkinson’s disease. Aging Cell 18:e13031. https://doi.org/10.1111/acel.13031
Smith MP, Cass WA (2007) Oxidative stress and dopamine depletion in an intrastriatal 6-hydroxydopamine model of Parkinson’s disease. Neuroscience 144:1057–1066. https://doi.org/10.1016/j.neuroscience.2006.10.004
Simola N, Morelli M, Carta AR (2007) The 6-hydroxydopamine model of Parkinson’s disease. Neurotox Res 11:151–167. https://doi.org/10.1007/BF03033565
Youdim MBH, Stephenson G, Ben Shachar D (2004) Ironing iron out in Parkinson’s disease and other neurodegenerative diseases with iron chelators: a lesson from 6-hydroxydopamine and iron chelators, desferal and VK-28. Ann N Y Acad Sci 1012:306–325. https://doi.org/10.1196/annals.1306.025
Riederer P, Monoranu C, Strobel S et al (2021) Iron as the concert master in the pathogenic orchestra playing in sporadic Parkinson’s disease. J Neural Transm (Vienna) 128:1577–1598. https://doi.org/10.1007/s00702-021-02414-z
Sian-Hülsmann J, Mandel S, Youdim MBH, Riederer P (2011) The relevance of iron in the pathogenesis of Parkinson’s disease. J Neurochem 118:939–957. https://doi.org/10.1111/j.1471-4159.2010.07132.x
Youdim MB, Ben-Shachar D, Riederer P (1993) The possible role of iron in the etiopathology of Parkinson’s disease. Mov Disord 8:1–12. https://doi.org/10.1002/mds.870080102
Foley PB, Hare DJ, Double KL (2022) A brief history of brain iron accumulation in Parkinson disease and related disorders. J Neural Transm (Vienna) 129:505–520. https://doi.org/10.1007/s00702-022-02505-5
Ma L, Gholam Azad M, Dharmasivam M et al (2021) Parkinson’s disease: alterations in iron and redox biology as a key to unlock therapeutic strategies. Redox Biol 41:101896. https://doi.org/10.1016/j.redox.2021.101896
Berg D, Gerlach M, Youdim MB et al (2001) Brain iron pathways and their relevance to Parkinson’s disease. J Neurochem 79:225–236. https://doi.org/10.1046/j.1471-4159.2001.00608.x
Linert W, Herlinger E, Jameson RF et al (1996) Dopamine, 6-hydroxydopamine, iron, and dioxygen—their mutual interactions and possible implication in the development of Parkinson’s disease. Biochim Biophys Acta 1316:160–168. https://doi.org/10.1016/0925-4439(96)00020-8
Jellinger K, Linert L, Kienzl E et al (1995) Chemical evidence for 6-hydroxydopamine to be an endogenous toxic factor in the pathogenesis of Parkinson’s disease. J Neural Transm Suppl 46:297–314
Zhu HC, Zhao J, Luo CY, Li QQ (2012) Gastrointestinal dysfunction in a Parkinson’s disease rat model and the changes of dopaminergic, nitric oxidergic, and cholinergic neurotransmitters in myenteric plexus. J Mol Neurosci 47:15–25. https://doi.org/10.1007/s12031-011-9560-0
Colucci M, Cervio M, Faniglione M et al (2012) Intestinal dysmotility and enteric neurochemical changes in a Parkinson’s disease rat model. Auton Neurosci 169:77–86. https://doi.org/10.1016/j.autneu.2012.04.005
**u X-L, Zheng L-F, Liu X-Y et al (2020) Gastric smooth muscle cells manifest an abnormal phenotype in Parkinson’s disease rats with gastric dysmotility. Cell Tissue Res 381:217–227. https://doi.org/10.1007/s00441-020-03214-9
de Moraes Thomasi BB, Valdetaro L, MCG R et al (2022) Enteric glial cell reactivity in colonic layers and mucosal modulation in a mouse model of Parkinson’s disease induced by 6-hydroxydopamine. Brain Res Bull 187:111–121. https://doi.org/10.1016/j.brainresbull.2022.06.013
Yan J-T, Liu X-Y, Liu J-H et al (2021) Reduced acetylcholine and elevated muscarinic receptor 2 in duodenal mucosa contribute to the impairment of mucus secretion in 6-hydroxydopamine-induced Parkinson’s disease rats. Cell Tissue Res 386:249–260. https://doi.org/10.1007/s00441-021-03515-7
Homolak J (2021) Redox homeostasis in Alzheimer’s disease. Redox signaling and biomarkers in ageing https://doi.org/10.1007/978-3-030-84965-8_15
Sharma A, Singh S, Garg G, Singh AK (2022) Impaired redox status and age-related neurodegenerative disorders. In: Çakatay U (ed) Redox signaling and biomarkers in ageing. Springer International Publishing, Cham, pp. 287–302
Cakatay U (2022) Redox signaling and biomarkers in ageing. Springer Nature
Dias V, Junn E, Mouradian MM (2013) The role of oxidative stress in Parkinson’s disease. J Parkinsons Dis 3:461–491. https://doi.org/10.3233/JPD-130230
Blesa J, Trigo-Damas I, Quiroga-Varela A, Jackson-Lewis VR (2015) Oxidative stress and Parkinson’s disease. Front Neuroanat 9:91. https://doi.org/10.3389/fnana.2015.00091
Wei Z, Li X, Li X et al (2018) Oxidative stress in Parkinson’s disease: a systematic review and meta-analysis. Front Mol Neurosci 11:236. https://doi.org/10.3389/fnmol.2018.00236
Dorszewska J, Kowalska M, Prendecki M et al (2021) Oxidative stress factors in Parkinson’s disease. Neural Regen Res 16:1383–1391. https://doi.org/10.4103/1673-5374.300980
Circu ML, Aw TY (2012) Intestinal redox biology and oxidative stress. Semin Cell Dev Biol 23:729–737. https://doi.org/10.1016/j.semcdb.2012.03.014
Bhattacharyya A, Chattopadhyay R, Mitra S, Crowe SE (2014) Oxidative stress: an essential factor in the pathogenesis of gastrointestinal mucosal diseases. Physiol Rev 94:329–354. https://doi.org/10.1152/physrev.00040.2012
Homolak J (2023) Gastrointestinal redox homeostasis in ageing. Biogerontology. https://doi.org/10.1007/s10522-023-10049-8
McCord JM (1987) Radical explanations for old observations. Gastroenterology 92:2026–2028. https://doi.org/10.1016/0016-5085(87)90640-8
Salkovic-Petrisic M, Perhoc AB, Homolak J et al (2021) Experimental approach to Alzheimer’s disease with emphasis on insulin resistance in the brain. In: Kostrzewa RM (ed) Handbook of neurotoxicity. Springer International Publishing, Cham, pp. 1–52
Barilar JO, Knezovic A, Perhoc AB et al (2020) Shared cerebral metabolic pathology in non-transgenic animal models of Alzheimer’s and Parkinson’s disease. J Neural Transm 127:231–250. https://doi.org/10.1007/s00702-020-02152-8
Homolak J, Babic Perhoc A, Knezovic A et al (2021) Failure of the brain glucagon-like peptide-1-mediated control of intestinal redox homeostasis in a rat model of sporadic Alzheimer’s disease. Antioxidants 10:1118. https://doi.org/10.3390/antiox10071118
Homolak J, Babic Perhoc A, Knezovic A et al (2021) Disbalance of the duodenal epithelial cell turnover and apoptosis accompanies insensitivity of intestinal redox homeostasis to inhibition of the brain glucose-dependent insulinotropic polypeptide receptors in a rat model of sporadic Alzheimer’s disease. Neuroendocrinology. https://doi.org/10.1159/000519988
Homolak J, Virag D, Kodvanj I et al (2022) A hacked kitchen scale-based system for quantification of grip strength in rodents. Comput Biol Med 144:105391. https://doi.org/10.1016/j.compbiomed.2022.105391
Knezovic A, Piknjac M, Osmanovic Barilar J et al (2023) Association of cognitive deficit with glutamate and insulin signaling in a rat model of Parkinson’s disease. Biomedicines 11. https://doi.org/10.3390/biomedicines11030683
Monville C, Torres EM, Dunnett SB (2006) Comparison of incremental and accelerating protocols of the rotarod test for the assessment of motor deficits in the 6-OHDA model. J Neurosci Methods 158:219–223. https://doi.org/10.1016/j.jneumeth.2006.06.001
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248–254. https://doi.org/10.1006/abio.1976.9999
Homolak J, Babic Perhoc A, Knezovic A et al (2021) Is galactose a hormetic sugar? An exploratory study of the rat hippocampal redox regulatory network. Mol Nutr Food Res:e2100400. https://doi.org/10.1002/mnfr.202100400
Anderson ME (1985) Determination of glutathione and glutathione disulfide in biological samples. Methods Enzymol 113:548–555. https://doi.org/10.1016/s0076-6879(85)13073-9
Homolak J, Babic Perhoc A, Knezovic A et al (2022) The effect of acute oral galactose administration on the redox system of the rat small intestine. Antioxidants 11:37. https://doi.org/10.3390/antiox11010037
Marklund S, Marklund G (1974) Involvement of the superoxide anion radical in the autoxidation of pyrogallol and a convenient assay for superoxide dismutase. Eur J Biochem 47:469–474. https://doi.org/10.1111/j.1432-1033.1974.tb03714.x
Li X (2012) Improved pyrogallol autoxidation method: a reliable and cheap superoxide-scavenging assay suitable for all antioxidants. J Agric Food Chem 60:6418–6424. https://doi.org/10.1021/jf204970r
Homolak J (2022) In vitro analysis of catalase and superoxide dismutase mimetic properties of blue tattoo ink. Free Radic Res:1–15. https://doi.org/10.1080/10715762.2022.2102976
Hadwan MH (2018) Simple spectrophotometric assay for measuring catalase activity in biological tissues. BMC Biochem 19:7. https://doi.org/10.1186/s12858-018-0097-5
Homolak J (2021) The effect of a color tattoo on the local skin redox regulatory network: an N-of-1 study. Free Radic Res:1–9. https://doi.org/10.1080/10715762.2021.1912340
Ma X, Deng D, Chen W (2017) Inhibitors and activators of SOD, GSH-Px, and CAT. IntechOpen
Homolak J, Kodvanj I, Perhoc AB et al (2021) Nitrocellulose redox permanganometry: a simple method for reductive capacity assessment. MethodsX:101611. https://doi.org/10.1016/j.mex.2021.101611
Percie du Sert N, Ahluwalia A, Alam S et al (2020) Reporting animal research: explanation and elaboration for the ARRIVE guidelines 2.0. PLoS Biol 18:e3000411. https://doi.org/10.1371/journal.pbio.3000411
Therneau T (2023) A package for survival analysis in R. R package version 3.5-7. https://CRAN.R-project.org/package=survival
Kassambara A, Kosinski M, Biecek P, Fabian S (2021) survminer: drawing survival curves using “ggplot2” R package version 0.4.9. https://CRAN.R-project.org/package=survminer
Homolak J, Babic Perhoc A, Knezovic A et al (2023) Exploratory study of gastrointestinal redox biomarkers in the presymptomatic and symptomatic Tg2576 mouse model of familial Alzheimer’s disease: phenotypic correlates and effects of chronic oral d-galactose. ACS Chem Neurosci 14:4013–4025. https://doi.org/10.1021/acschemneuro.3c00495
Pellegrini C, Fornai M, Colucci R et al (2016) Alteration of colonic excitatory tachykininergic motility and enteric inflammation following dopaminergic nigrostriatal neurodegeneration. J Neuroinflammation 13:146. https://doi.org/10.1186/s12974-016-0608-5
Roedter A, Winkler C, Samii M et al (2001) Comparison of unilateral and bilateral intrastriatal 6-hydroxydopamine-induced axon terminal lesions: evidence for interhemispheric functional coupling of the two nigrostriatal pathways. J Comp Neurol 432:217–229. https://doi.org/10.1002/cne.1098
Tieu K (2011) A guide to neurotoxic animal models of Parkinson’s disease. Cold Spring Harb Perspect Med 1:a009316. https://doi.org/10.1101/cshperspect.a009316
Anselmi L, Toti L, Bove C et al (2017) A nigro-vagal pathway controls gastric motility and is affected in a rat model of Parkinsonism. Gastroenterology 153:1581–1593. https://doi.org/10.1053/j.gastro.2017.08.069
Ayala A, Muñoz MF, Argüelles S (2014) Lipid peroxidation: production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxidative Med Cell Longev 2014:360438. https://doi.org/10.1155/2014/360438
Janero DR (1990) Malondialdehyde and thiobarbituric acid-reactivity as diagnostic indices of lipid peroxidation and peroxidative tissue injury. Free Radic Biol Med 9:515–540. https://doi.org/10.1016/0891-5849(90)90131-2
Morales M, Munné-Bosch S (2019) Malondialdehyde: facts and artifacts. Plant Physiol 180:1246–1250. https://doi.org/10.1104/pp.19.00405
Carty E, Nickols C, Feakins RM, Rampton DS (2002) Thromboxane synthase immunohistochemistry in inflammatory bowel disease. J Clin Pathol 55:367–370
Lugrin J, Rosenblatt-Velin N, Parapanov R, Liaudet L (2014) The role of oxidative stress during inflammatory processes. Biol Chem 395:203–230. https://doi.org/10.1515/hsz-2013-0241
Campbell EL, Colgan SP (2019) Control and dysregulation of redox signalling in the gastrointestinal tract. Nat Rev Gastroenterol Hepatol 16:106–120. https://doi.org/10.1038/s41575-018-0079-5
Chang K-H, Chen C-M (2020) The role of oxidative stress in Parkinson’s disease. Antioxidants (Basel) 9:597. https://doi.org/10.3390/antiox9070597
van der Vliet A, Tuinstra TJ, Bast A (1989) Modulation of oxidative stress in the gastrointestinal tract and effect on rat intestinal motility. Biochem Pharmacol 38:2807–2818. https://doi.org/10.1016/0006-2952(89)90435-8
Peluso I, Campolongo P, Valeri P et al (2002) Intestinal motility disorder induced by free radicals: a new model mimicking oxidative stress in gut. Pharmacol Res 46:533–538. https://doi.org/10.1016/s1043661802002372
Vermorken AJM, Andrès E, Cui Y (2016) Bowel movement frequency, oxidative stress and disease prevention. Mol Clin Oncol 5:339–342. https://doi.org/10.3892/mco.2016.987
Barata-Antunes S, Teixeira FG, Mendes-Pinheiro B et al (2020) Impact of aging on the 6-OHDA-induced rat model of Parkinson’s disease. Int J Mol Sci 21:E3459. https://doi.org/10.3390/ijms21103459
Klæstrup IH, Just MK, Holm KL et al (2022) Impact of aging on animal models of Parkinson’s disease. Front Aging Neurosci 14:909273. https://doi.org/10.3389/fnagi.2022.909273
Atayik MC, Çakatay U (2022) Mitochondria-targeted senotherapeutic interventions. Biogerontology 23:401–423. https://doi.org/10.1007/s10522-022-09973-y
Yanar K, Atayik MC, Simsek B, Çakatay U (2020) Novel biomarkers for the evaluation of aging-induced proteinopathies. Biogerontology 21:531–548. https://doi.org/10.1007/s10522-020-09878-8
Anandhan A, Chen W, Nguyen N et al (2022) α-Syn overexpression, NRF2 suppression, and enhanced ferroptosis create a vicious cycle of neuronal loss in Parkinson’s disease. Free Radic Biol Med 192:130–140. https://doi.org/10.1016/j.freeradbiomed.2022.09.015
Homolak J, Joja M, Grabaric G, et al (2022) The absence of gastrointestinal redox dyshomeostasis in the brain-first rat model of Parkinson’s disease induced by bilateral intrastriatal 6-hydroxydopamine. bioRxiv 2022.08.22.504759. https://doi.org/10.1101/2022.08.22.504759
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was funded by the Croatian Science Foundation (IP-2018-01-8938). The research was co-financed by the Scientific Centre of Excellence for Basic, Clinical, and Translational Neuroscience (project “Experimental and clinical research of hypoxic-ischemic damage in perinatal and adult brain”; GA KK01.1.1.01.0007 funded by the European Union through the European Regional Development Fund).
Author information
Authors and Affiliations
Contributions
JH, ABP, AK, and JOB—in vivo part of the experiment, tissue collection. JH, MJ, GG, ES—biochemical measurements. JH—data curation, data analysis, writing the first draft of the manuscript. MJ, GG, ES, DV, ABP, AK, JOB, and MSP—critical revision of the manuscript. MSP—funding, supervision.
Corresponding author
Ethics declarations
Ethics Approval
Only certified researchers worked with the animals, and the experiment was conducted with the highest standard of animal welfare. The animal procedures were conducted in concordance with current institutional (University of Zagreb School of Medicine), national (The Animal Protection Act, NN135/2006; NN 47/2011), and international (Directive 2010/63/EU) guidelines governing the use of experimental animals. The experiments were approved by the Croatian Ministry of Agriculture (EP 186 /2018) and the Ethical Committee of the University of Zagreb School of Medicine (380-59-10106-18-111/173).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 169 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Homolak, J., Joja, M., Grabaric, G. et al. The Absence of Gastrointestinal Redox Dyshomeostasis in the Brain-First Rat Model of Parkinson’s Disease Induced by Bilateral Intrastriatal 6-Hydroxydopamine. Mol Neurobiol (2024). https://doi.org/10.1007/s12035-023-03906-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12035-023-03906-7