Abstract
Purpose of Review
To provide a summary of current literature and propose potential mechanistic models to help us understand the role of HIV infection/antiretroviral therapy (ART), salt taste sensitivity (STS), and salt sensitivity of blood pressure (SSBP) in hypertension development.
Recent Findings
The epithelial sodium channel (ENaC) is the main protein/sodium channel for recognizing Na + in the tongue and mediates preference to low-medium salt concentrations in animals and humans. Considering the pressor response to oral salt in individuals with SSBP, poor STS may worsen blood pressure. Specific genetic variants in ENaC are linked to salt taste perception and hypertension. HIV infection, some ART, and specific antihypertensive drugs are associated with reduced STS and an increased liking for salty foods.
Summary
Persons with HIV (PWH) on ART may have a decreased STS and are at a higher risk of develo** salt-sensitive hypertension. Inflammation mediated by dietary salt is one of the drivers of poor STS and salt-sensitive hypertension among PWH.



Similar content being viewed by others
Data Availability
All data presented are contained within this manuscript.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Roura E, Foster S, Winklebach A, Navarro M, Thomas W, Campbell K, et al. Taste and hypertension in humans: targeting cardiovascular disease. Curr Pharm Des. 2016;22:2290–305. https://doi.org/10.2174/1381612822666160216151545.
Masenga SK, Hamooya BM, Nzala S, Kwenda G, Heimburger DC, Mutale W, et al. Patho-immune mechanisms of hypertension in HIV: a systematic and thematic review. Curr Hypertens Rep. 2019;21:56. https://doi.org/10.1007/s11906-019-0956-5.
Pangmekeh PJ, Awolu MM, Gustave S, Gladys T, Cumber SN. Association between highly active antiretroviral therapy (HAART) and hypertension in persons living with HIV/AIDS at the Bamenda Regional Hospital, Cameroon. Pan Afr Med J. 2019;33:87. https://doi.org/10.11604/pamj.2019.33.87.15574.
Masenga SK, Elijovich F, Koethe JR, Hamooya BM, Heimburger DC, Munsaka SM, et al. Hypertension and metabolic syndrome in persons with HIV. Curr Hypertens Rep. 2020;22:78. https://doi.org/10.1007/s11906-020-01089-3.
Henn IW, da Silva ROC, Chaiben CL, Fernandes Â, Naval Machado MÂ, de Lima AAS. Perception of taste in HIV-positive individuals in treatment antiretroviral: results of a case-control study. Spec Care Dentist. 2017;37:3–9. https://doi.org/10.1111/scd.12186.
Black HR. The burden of cardiovascular disease: following the link from hypertension to myocardial infarction and heart failure. Am J Hypertens. 2003;16:4S-6S. https://doi.org/10.1016/S0895-7061(03)00969-5.
Fasunla AJ, Daniel A, Nwankwo U, Kuti KM, Nwaorgu OG, Akinyinka OO. Evaluation of olfactory and gustatory function of HIV infected women. AIDS Res Treat. 2016;2016:2045383. https://doi.org/10.1155/2016/2045383.
•• Masenga SK, Kirabo A, Hamooya BM, Nzala S, Kwenda G, Heimburger DC, et al. HIV-positive demonstrate more salt sensitivity and nocturnal non-dip** blood pressure than HIV-negative individuals. Clin Hypertens. 2021;27. https://doi.org/10.1186/s40885-020-00160-0. This clinical trial demonstrates that the pressor response to dietary salt is higher in persons with HIV and hypertension.
Shah ASV, Stelzle D, Lee KK, Beck EJ, Alam S, Clifford S, et al. Global burden of atherosclerotic cardiovascular disease in people living with HIV: systematic review and meta-analysis. Circulation. 2018;138:1100–12. https://doi.org/10.1161/CIRCULATIONAHA.117.033369.
Elvstam O, Marrone G, Engström G, Nilsson PM, Carlander C, Treutiger CJ, et al. Associations between HIV Viremia during antiretroviral therapy and cardiovascular disease. AIDS. 2022;36:1829–34. https://doi.org/10.1097/QAD.0000000000003240.
Karmous I, Plesník J, Khan AS, Šerý O, Abid A, Mankai A, et al. Orosensory detection of bitter in fat-taster healthy and obese participants: genetic polymorphism of CD36 and TAS2R38. Clin Nutr. 2018;37:313–20. https://doi.org/10.1016/j.clnu.2017.06.004.
Piovesana PDM, Sampaio KDL, Gallani MCBJ. Association between taste sensitivity and self-reported and objective measures of salt intake among hypertensive and normotensive individuals. Int Sch Res Notices. 2012;2013:e301213. https://doi.org/10.5402/2013/301213.
Murtaugh MA, Beasley JM, Appel LJ, Guenther PM, McFadden M, Greene T, et al. Relationship of sodium intake and blood pressure varies with energy intake: secondary analysis of the DASH (dietary approaches to stop hypertension)-sodium trial. Hypertension. 2018;71:858–65. https://doi.org/10.1161/HYPERTENSIONAHA.117.10602.
•• Martinelli J, Conde SR, de Araújo AR, Marcadenti A. Association between salt taste sensitivity threshold and blood pressure in healthy individuals: a cross-sectional study. Sao Paulo Med J. 2020;138:4–10. https://doi.org/10.1590/1516-3180.2019.0166.R1.02102019. In this study, they report that salt taste sensitivity is associated with increased salt intake and elevated blood pressure independent of other risk factors for hypertension.
Kirabo A. A new paradigm of sodium regulation in inflammation and hypertension. Am J Physiol Regul Integr Comp Physiol. 2017;313:R706–10. https://doi.org/10.1152/ajpregu.00250.2017.
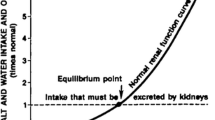
Elijovich F, Weinberger MH, Anderson CAM, Appel LJ, Bursztyn M, Cook NR, et al. Salt sensitivity of blood pressure. Hypertension. 2016;68:e7–46. https://doi.org/10.1161/HYP.0000000000000047.
Lindhorst J, Alexander N, Blignaut J, Rayner B. Differences in hypertension between Blacks and Whites: an overview. Cardiovasc J Afr. 2007;18:241–7.
Morris RC, Sebastian A, Forman A, Tanaka M, Schmidlin O. Normotensive salt sensitivity. Hypertension. 1999;33:18–23. https://doi.org/10.1161/01.HYP.33.1.18.
Mishra S, Ingole S, Jain R. Salt sensitivity and its implication in clinical practice. Indian Heart J. 2018;70:556–64. https://doi.org/10.1016/j.ihj.2017.10.006.
Choi HY, Park HC, Ha SK. Salt sensitivity and hypertension: a paradigm shift from kidney malfunction to vascular endothelial dysfunction. Electrolyte Blood Press. 2015;13:7–16. https://doi.org/10.5049/EBP.2015.13.1.7.
Weinberger MH, Fineberg NS, Fineberg SE, Weinberger M. Salt sensitivity, pulse pressure, and death in normal and hypertensive humans. Hypertension. 2001;37:429–32. https://doi.org/10.1161/01.hyp.37.2.429.
Melis M, Mastinu M, Sollai G, Paduano D, Chicco F, Magrì S, et al. Taste changes in patients with inflammatory bowel disease: associations with PROP phenotypes and polymorphisms in the salivary protein, gustin and CD36 receptor genes. Nutrients. 2020;12:409. https://doi.org/10.3390/nu12020409.
•• Tapanee P, Tidwell DK, Schilling MW, Peterson DG, Tolar-Peterson T. Genetic variation in taste receptor genes (SCNN1B, TRPV1) and its correlation with the perception of saltiness in normotensive and hypertensive adults. Int J Hypertens. 2021;2021:5559831. https://doi.org/10.1155/2021/5559831. This case-control study links genetic variants in the taste receptor genes to salt taste sensitivity and hypertension risk. They further show that people with hypertension have a higher salt taste threshold than those with normotension.
Pilic L, Mavrommatis Y. Genetic predisposition to salt-sensitive normotension and its effects on salt taste perception and intake. Br J Nutr. 2018;120:721–31. https://doi.org/10.1017/S0007114518002027.
Diószegi J, Llanaj E, Ádány R. Genetic background of taste perception, taste preferences, and its nutritional implications: a systematic review. Front Genet. 2019;10:1272. https://doi.org/10.3389/fgene.2019.01272.
Gravina SA, Yep GL, Khan M. Human biology of taste. Ann Saudi Med. 2013;33:217–22. https://doi.org/10.5144/0256-4947.2013.217.
Mattes RD. Fat taste in humans: is it a primary? In Fat Detection: taste, texture, and post ingestive effects; Montmayeur J-P, le Coutre J, editors; Front Neurosci; CRC Press/Taylor & Francis: Boca Raton (FL); 2010. ISBN 978-1-4200-6775-0.
Contreras RJ. Salt taste and disease. Am J Clin Nutr. 1978;31:1088–97. https://doi.org/10.1093/ajcn/31.6.1088.
• Bigiani A. Does ENaC work as sodium taste receptor in humans? Nutrients. 2020;12:1195. https://doi.org/10.3390/nu12041195. This review provides a comprehensive description of current knowledge on ENaC’s salt sensing mechanisms and its role in mediating a liking for salty food.
• Nomura K, Nakanishi M, Ishidate F, Iwata K, Taruno A. All-electrical Ca2+-independent signal transduction mediates attractive sodium taste in taste buds. Neuron. 2020;106:816–829.e6. https://doi.org/10.1016/j.neuron.2020.03.006. This work reveals ENaC-independent salt attraction via signal transduction mechanisms.
Shigemura N, Ohkuri T, Sadamitsu C, Yasumatsu K, Yoshida R, Beauchamp GK, et al. Amiloride-sensitive NaCl taste responses are associated with genetic variation of ENaC α-subunit in mice. Am J Physiol Regul Integr Comp Physiol. 2008;294:R66–75. https://doi.org/10.1152/ajpregu.00420.2007.
Pitzer AL, Van Beusecum JP, Kleyman TR, Kirabo A. ENaC in salt-sensitive hypertension: kidney and beyond. Curr Hypertens Rep. 2020. https://doi.org/10.1007/s11906-020-01067-9.
Canessa CM, Schild L, Buell G, Thorens B, Gautschi I, Horisberger JD, et al. Amiloride-sensitive epithelial Na+ channel is made of three homologous subunits. Nature. 1994;367:463–7. https://doi.org/10.1038/367463a0.
Huque T, Cowart BJ, Dankulich-Nagrudny L, Pribitkin EA, Bayley DL, Spielman AI, et al. Sour ageusia in two individuals implicates ion channels of the ASIC and PKD families in human sour taste perception at the anterior tongue. PLoS ONE. 2009;4:e7347. https://doi.org/10.1371/journal.pone.0007347.
Rossier O, Cao J, Huque T, Spielman AI, Feldman RS, Medrano JF, et al. Analysis of a human fungiform papillae CDNA library and identification of taste-related genes. Chem Senses. 2004;29:13–23. https://doi.org/10.1093/chemse/bjh002.
Stähler F, Riedel K, Demgensky S, Neumann K, Dunkel A, Täubert A, et al. A role of the epithelial sodium channel in human salt taste transduction? Chem Percept. 2008;1:78–90. https://doi.org/10.1007/s12078-008-9006-4.
Bachmanov AA, Bosak NP, Lin C, Matsumoto I, Ohmoto M, Reed DR, et al. Genetics of taste receptors. Curr Pharm Des. 2014;20:2669–83. https://doi.org/10.2174/13816128113199990566.
Vandenbeuch A, Kinnamon SC. Is the Amiloride-sensitive Na+ channel in taste cells really ENaC? Chem Senses. 2020;45:233–4. https://doi.org/10.1093/chemse/bjaa011.
Lyall V, Heck GL, Vinnikova AK, Ghosh S, Phan T-HT, Alam RI, et al. The mammalian amiloride-insensitive non-specific salt taste receptor is a vanilloid receptor-1 variant. J Physiol. 2004;558:147–59. https://doi.org/10.1113/jphysiol.2004.065656.
Dias AG, Rousseau D, Duizer L, Cockburn M, Chiu W, Nielsen D, et al. genetic variation in putative salt taste receptors and salt taste perception in humans. Chem Senses. 2013;38:137–45. https://doi.org/10.1093/chemse/bjs090.
Ruiz C, Gutknecht S, Delay E, Kinnamon S. Detection of NaCl and KCl in TRPV1 knockout mice. Chem Senses. 2006;31:813–20. https://doi.org/10.1093/chemse/bjl024.
Treesukosol Y, Lyall V, Heck GL, DeSimone JA, Spector AC. A psychophysical and electrophysiological analysis of salt taste in Trpv1 null mice. Am J Physiol Regul Integr Comp Physiol. 2007;292:R1799–809. https://doi.org/10.1152/ajpregu.00587.2006.
Ferraris C, Turner A, Kaur K, Piper J, Veysey M, Lucock M, et al. Salt taste genotype, dietary habits and biomarkers of health: no associations in an elderly cohort. Nutrients. 2020;12:1056. https://doi.org/10.3390/nu12041056.
Menon V, Chen Y-CD. Commentary: The role of the anion in salt (NaCl) detection by mouse taste buds. Front Cell Neurosci. 2019;13.
•• Pilic L, Lubasinski NJ, Berk M, Ward D, Graham CA-M, Da Silva Anastacio V, et al. The associations between genetics, salt taste perception and salt intake in young adults. Food Qual Prefer. 2020;84:103954, https://doi.org/10.1016/j.foodqual.2020.103954. This is an important study demonstrating genetic variants in taste receptor genes driving salt perception and salt intake in young adults.
Elijovich F, Weinberger MH, Anderson CAM, Appel LJ, Bursztyn M, Cook NR, et al. Salt sensitivity of blood pressure: a scientific statement from the American Heart Association. Hypertension. 2016;68:e7–46. https://doi.org/10.1161/HYP.0000000000000047.
Kurtz TW, DiCarlo SE, Pravenec M, Morris RC. An appraisal of methods recently recommended for testing salt sensitivity of blood pressure. J Am Heart Assoc. 2017;6:e005653. https://doi.org/10.1161/JAHA.117.005653.
Cavka A, Cosic A, Jukic I, Jelakovic B, Lombard JH, Phillips SA, et al. The role of cyclo-oxygenase-1 in high-salt diet-induced microvascular dysfunction in humans. J Physiol (Lond). 2015;593:5313–24. https://doi.org/10.1113/JP271631.
Jablonski KL, Fedorova OV, Racine ML, Geolfos CJ, Gates PE, Chonchol M, et al. Dietary sodium restriction and association with urinary marinobufagenin, blood pressure, and aortic stiffness. Clin J Am Soc Nephrol. 2013;8:1952–9. https://doi.org/10.2215/CJN.00900113.
Pathak CM, Ix JH, Anderson CAM, Woodell TB, Smits G, Persky MS, et al. Variation in sodium intake and intra-individual change in blood pressure in chronic kidney disease. J Ren Nutr. 2018;28:125–8. https://doi.org/10.1053/j.jrn.2017.07.002.
Lu J, Wang H-W, Ahmad M, Keshtkar-Jahromi M, Blaustein MP, Hamlyn JM, et al. Central and peripheral slow-pressor mechanisms contributing to angiotensin ii-salt hypertension in rats. Cardiovasc Res. 2018;114:233–46. https://doi.org/10.1093/cvr/cvx214.
Van Beusecum J, Barbaro NR, McDowell Z, Aden LA, **ao L, Pandey AK, et al. High salt activates CD11c+ antigen-presenting cells via SGK (serum glucocorticoid kinase) 1 to promote renal inflammation and salt-sensitive hypertension. Hypertension. 2019;74:555–63. https://doi.org/10.1161/HYPERTENSIONAHA.119.12761.
Dickinson KM, Clifton PM, Keogh JB. Endothelial function is impaired after a high-salt meal in healthy subjects1–3. Am J Clin Nutr. 2011;93:500–5. https://doi.org/10.3945/ajcn.110.006155.
•• Masenga SK, Pilic L, Hamooya BM, Nzala S, Heimburger DC, Mutale W, et al. Immediate pressor response to oral salt and its assessment in the clinic: a time series clinical trial. Clinical Hypertension. 2022;28:25. https://doi.org/10.1186/s40885-022-00209-2. This is a recent clinical trial demonstrating the immediate pressor response of oral salt in people of African descent. This study suggests that the amount of dietary salt currently consumed by the Western world and African populations in single meals may increase the 24-h BP load, which is a risk factor for hypertension. It also demonstrates the predictive applicability of systolic blood pressure to identify an immediate pressor response to salt in 30 min.
Lim J, Pearman ME, Park W, Alkatan M, Machin DR, Tanaka H. Impact of blood pressure perturbations on arterial stiffness. Am J Physiol Regul Integr Comp Physiol. 2015;309:R1540-1545. https://doi.org/10.1152/ajpregu.00368.2015.
•• Blobner BM, Kirabo A, Kashlan OB, Sheng S, Arnett DK, Becker LC, et al. Rare variants in genes encoding subunits of the epithelial Na+ channel are associated with blood pressure and kidney function. Hypertension. 2022;79:2573–82. https://doi.org/10.1161/HYPERTENSIONAHA.121.18513. This study demonstrates that variants in extrarenal ENaC subunits, in addition to ENaCs expressed in kidneys, influence blood pressure and kidney function.
Barbaro NR, Foss JD, Kryshtal DO, Tsyba N, Kumaresan S, **ao L, et al. Dendritic cell amiloride-sensitive channels mediate sodium-induced inflammation and hypertension. Cell Rep. 2017;21:1009–20. https://doi.org/10.1016/j.celrep.2017.10.002.
Azinge EC, Sofola OA, Silva BO. Relationship between salt intake, salt-taste threshold and blood pressure in Nigerians. West Afr J Med. 2011;30:373–6.
Suliburska J, Duda G, Pupek-Musialik D. The influence of hypotensive drugs on the taste sensitivity in patients with primary hypertension. Acta Pol Pharm. 2012;69:121–7.
Henkin RI. Drug-induced taste and smell disorders: incidence, mechanisms and management related primarily to treatment of sensory receptor dysfunction. Drug Saf. 1994;11:318–77. https://doi.org/10.2165/00002018-199411050-00004.
Tomita H, Yoshikawa T. Drug-related taste disturbances. Acta Otolaryngol Suppl. 2002. https://doi.org/10.1080/00016480260046490.
Pugazhenthan T, Singh H, Kumar P, Hariharan B. Is Dysguesia going to be a rare or a common side-effect of amlodipine? Ann Med Health Sci Res. 2014;4:S43–4. https://doi.org/10.4103/2141-9248.131714.
Tsuruoka S, Wakaumi M, Nishiki K, Araki N, Harada K, Sugimoto K, et al. subclinical alteration of taste sensitivity induced by candesartan in healthy subjects. Br J Clin Pharmacol. 2004;57:807–12. https://doi.org/10.1111/j.1365-2125.2003.02063.x.
Schlienger RG, Saxer M, Haefeli WE. Reversible ageusia associated with losartan. Lancet. 1996;347:471–2. https://doi.org/10.1016/s0140-6736(96)90047-1.
Heeringa M, van Puijenbroek EP. Reversible dysgeusia attributed to losartan. Ann Intern Med. 1998;129:72. https://doi.org/10.7326/0003-4819-129-1-199807010-00023.
Mizuta E. Impact of taste sensitivity on lifestyle-related diseases. Yakugaku Zasshi. 2015;135:789–92. https://doi.org/10.1248/yakushi.14-00250-5.
Thomas DC, Chablani D, Parekh S, Pichammal RC, Shanmugasundaram K, Pitchumani PK. Dysgeusia. J Am Dent Assoc. 2022;153:251–64. https://doi.org/10.1016/j.adaj.2021.08.009.
Raja JV, Rai P, Khan M, Banu A, Bhuthaiah S. Evaluation of gustatory function in HIV-infected subjects with and without HAART. J Oral Pathol Med. 2013;42:216–21. https://doi.org/10.1111/jop.12006.
Shintani T, Fujii T, Yamasaki N, Kitagawa M, Iwata T, Saito S, et al. Oral environment and taste function of Japanese HIV-infected patients treated with antiretroviral therapy. AIDS Care. 2020;32:829–34. https://doi.org/10.1080/09540121.2019.1656327.
Schiffman SS, Zervakis J, Heffron S, Heald AE. Effect of protease inhibitors on the sense of taste. Nutrition. 1999;15:767–72. https://doi.org/10.1016/s0899-9007(99)00152-5.
Fasunla AJ, Nwankwo U, Adebayo AM, Nwaorgu OG. Association between sex, CD4 cell counts, antiretroviral medications, and olfactory and gustatory functions of HIV-infected adults. Otolaryngol Head Neck Surg. 2018;158:90–9. https://doi.org/10.1177/0194599817733664.
Fahme SA, Bloomfield GS, Peck R. Hypertension in HIV-infected adults: novel pathophysiologic mechanisms. Hypertension. 2018;72:44–55. https://doi.org/10.1161/HYPERTENSIONAHA.118.10893.
Deeks SG. HIV infection, inflammation, immunosenescence, and aging. Annu Rev Med. 2011;62:141–55. https://doi.org/10.1146/annurev-med-042909-093756.
Deeks SG, Tracy R, Douek DC. Systemic effects of inflammation on health during chronic HIV infection. Immunity. 2013;39:633–45. https://doi.org/10.1016/j.immuni.2013.10.001.
Zicari S, Sessa L, Cotugno N, Ruggiero A, Morrocchi E, Concato C, et al. Immune activation, inflammation, and non-AIDS co-morbidities in HIV-infected patients under long-term ART. Viruses. 2019;11:200. https://doi.org/10.3390/v11030200.
Sahinoz M, Elijovich F, Ertuglu LA, Ishimwe J, Pitzer A, Saleem M, et al. Salt-sensitivity of blood pressure in Blacks and women: a role of inflammation, oxidative stress and ENaC. Antioxid Redox Signal. 2021. https://doi.org/10.1089/ars.2021.0212.
Barbaro NR, Van Beusecum J, **ao L, do Carmo L, Pitzer A, Loperena R, et al. Sodium activates human monocytes via the NADPH oxidase and isolevuglandin formation. Cardiovasc Res. 2020. https://doi.org/10.1093/cvr/cvaa207.
• Masenga SK, Elijovich F, Hamooya BM, Nzala S, Kwenda G, Heimburger DC, et al. Elevated eosinophils as a feature of inflammation associated with hypertension in virally suppressed people living with HIV. J Am Heart Assoc. 2020;9:e011450, https://doi.org/10.1161/JAHA.118.011450. This study elaborates the role of HIV-associated inflammation and inflammatory cells in predisposing to hypertension.
Acknowledgements
Graphics were produced using www.Biorender.com.
Funding
This work was supported by the Fogarty International Center of the National Institutes of Health grants R03HL155041, R01HL147818, and R01HL144941 (AK) and 2D43TW009744, D43 TW009744, and D43 TW009337 (SKM). The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
SKM conceptualized the study and wrote the draft manuscript. SKM, LP, and AK wrote and edited different sections of the manuscript. SKM created all the figures. LP and AK edited and reviewed the manuscript. AK conceptualized the framework and finalized the manuscript as well as obtained funding for the manuscript. All authors contributed to article reviews, edited, and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Inflammation and Cardiovascular Diseases
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Masenga, S.K., Pilic, L. & Kirabo, A. Salt Taste and Salt Sensitive Hypertension in HIV. Curr Hypertens Rep 25, 25–33 (2023). https://doi.org/10.1007/s11906-023-01236-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-023-01236-6