Abstract
Background
Unsatisfactory cancer screening results are often associated with poor prognosis. This study synthesized the literatures addressing the impact of patient navigation (PN) interventions on population-based breast cancer screening promotion to identify characteristics of the model for addressing breast cancer disparities.
Methods
We searched Pubmed, Embase, Web of Science, and the Cochrane Central Registry from inception to 31 December 2020 for randomized controlled trials (PROSPERO: CRD42021246890). We double blindly abstracted data and assessed study quality. We assessed screening completion rates and diagnostic resolution using random-effects models between those receiving navigation and controls.
Results
Of 236 abstracts identified, 15 studies met inclusion criteria. Nine of the papers evaluated the impact of PN on breast screening, while the other six were on the resolution of abnormal screening results. Compared to the non-PN group, PN improved screening completion (OR: 2.0, 95% CI: 1.4–2.8]) and shortened the time to diagnosis (WMD: − 9.90 days, 95% CI: − 19.09 to − 0.71).
Conclusions
Patient navigation improves breast cancer screening rates but does not improve resolution of abnormal tests.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Mortality due to breast cancer remains high globally. Two causes include low participation in screening and delays in diagnosis.1 Early detection and treatment reduce breast cancer death.2 However, in some specific populations, socio-economic factors may be an obstacle to participation in population-based breast screening.
Patient navigation (PN) has emerged as one partial solution to reduce disparities in cancer care delivery. Trained navigators can promote cancer screening, follow-up of abnormal tests, and timely treatment.3, 4 However, the literature on navigator effectiveness is mixed5–7 and interpreting these studies is difficult, owing to considerable heterogeneity. Two recent systematic reviews including both RCTs and observational studies concluded that PN improves the screening rate of many tumors, including breast cancer.8, 9 However, these studies did not analyze the impact of PN on the diagnosis rate of abnormal screening findings. Reduction in breast cancer mortality requires that abnormal mammograms be followed by a process that leads to timely definitive diagnosis and treatment.10 Unfortunately, this follow-up process was shown to be incomplete or delayed in some vulnerable populations. Our systematic review aims to assess the impact of patient navigation on screening and resolution of abnormal findings for breast cancer.
PATIENTS AND METHODS
We followed PRISMA guidelines in conducting our review11 and registered our protocol with PROSPERO (CRD42021246890).
Search Strategy and Study Selection
The three authors independently reviewed results from our search of PUBMED, EMBASE, Web of Science, and Cochrane Central Register of Controlled Trials databases from their date of inception to 31 December 2020. The search strategy recommended by a librarian is provided in the Supplementary data. Both unpublished and published studies were eligible for inclusion. After removing the duplicate literature, three authors (Lu T., L. H., and Y. Y.) screened the titles and abstracts of the search results. The final inclusion decision was based on the independent review of the full text by the three authors. Any discrepancies arising from the process should be settled by consensus.
Eligibility Criteria
Our review was limited to randomized trials of PN among female participants over 18 years old and not pregnant. Studies were excluded if any of the following conditions occurred: (1) participant(s) had a history of cancer or were receiving anti-tumor treatment; (2) participant(s) had received PN intervention in the past; (3) participant(s) were/are living in a pension institution; (4) participant(s) had a history of mastectomy; (5) the screening mode was not community-based; (6) interventions did not meet the definition of PN, such as only phone-call or email reminder; (7) data were insufficient to obtain OR and 95% CI for outcome; (8) full texts were unavailable; and (9) the types of literature comprised abstract, letter, review, protocol, conference presentations, editorials, and/or expert opinions. When the same or partially identical cohorts were reported in different published studies, the most comprehensive study was selected.
Data Extraction
For all studies eventually included in the meta-analysis, study characteristics were independently extracted using a standard data extraction form by each of the three authors (Table 1). Again, discrepancies were resolved by consensus. For studies that provided graphs of time to DR by days from initial screening instead of mean and SD, we used the Engauge-Digitizer software (version 11.2) to obtain the approximate number of people diagnosed at a specific time point, so as to reasonably estimate the diagnostic time. For studies that provided data by BI-RADS group or race, we pooled the data to get overall effect measures.
Risk-of-Bias Appraisal
We assessed literature quality using the Cochrane Risk of Bias tool.25 Review Manager (v 5.3.5) was used to generate “risk of bias” graph and summary.
Statistical Analysis
We performed statistical analyses using Stata/SE (College Station, TX, v13.0) and the meta package in R (version 3.4.3). We calculated ORs and their associated 95% CIs to assess outcomes and considered a p value less than 0.05 to be statistically significant. A significant degree of heterogeneity between studies was defined as both the I2 statistic with a cut off of ≥ 50%, and the χ2 test with a p value < 0.10.26 Effect size was calculated using random-effects models.27 We assessed heterogeneity using subgroup analyses (Stata), sensitivity analysis (Stata), and meta regression (R). The criteria of grou** in subgroup analysis was established based on clinical significance and overall data distribution. Publication bias was assessed by Egger’s test with visual inspection of funnel plots (Stata).12 We assessed the potential impact of publication bias using the Trim and Fill approach (Stata).12
RESULTS
Study Characteristics
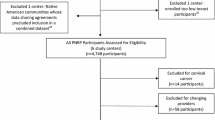
We included 9 papers13–21 on the impact of PN on screening and six papers5, 6, 22–24, 28 on diagnostic resolution (Fig. 1). Study characteristics are presented in Table 1. A considerable number of trials had unclear risk of bias on some measures, suggesting only modest study quality (Fig. 2). Three trials on screening15, 19, 20 were judged to be at high risk of bias. All trials enrolled were partially or fully sponsored by the government.
Effect of PN on Completion of Breast Screening
PN improved the likelihood of completing breast cancer screening (OR: 2.0, 95% CI: 1.4–2.8, I2 = 95.0%, Fig. 3). Sample size (p < 0.01), race (p < 0.01), and education level (p < 0.01) contributed to heterogeneity, explaining 65%, 86%, and 71% respectively.
In our sensitivity analysis, we found that no single study was overly influential. Our results were not significantly changed by excluding trials at high risk of bias (OR: 1.95, 95% CI: 1.3–2.9, I2 = 96.3%).
We found evidence of publication bias (Egger’s test, p = 0.006), though the effect was still significant after adjusting for publication bias (OR 1.7, 95% CI: 1.3–2.2).
Effect of PN on Diagnostic Resolution
Patient navigation did not significantly improve diagnostic resolution (OR: 2.1, 95% CI: 0.99–4.4, I2 = 89.3%, Fig. 4), though it reduced the average time until diagnostic resolution (WMD: − 9.9 days, 95% CI: − 19.1 to − 0.71, I2 = 96.7%, Fig. 5).
For diagnostic resolution, a sample size > 500 and less than 6-month follow-up length explained 94.5% of the heterogeneity. Excluding any single trial did not change our effect estimate. There was no evidence of publication bias (Egger’s test, p = 0.08). For time until diagnostic resolution, sample size and length of follow-up explained 86.1% and 91.5% of the heterogeneity. We found no evidence of publication bias (Egger’s test, p = 0.87).
DISCUSSION
We found that patient navigators doubled the likelihood of screening for breast cancer. The impact of PN on diagnostic resolution was less clear; there was no improvement in resolution, but a reduction in the average time until resolution. This likely reflects the small number of trials; while the odds of diagnostic resolution did not quite meet statistical significance, it was nearly double in the PN group, reflecting inadequate power. The average number of days until resolution improved with PN, by nearly 10 days.
Recent studies have shown that PN improved mammography screening rates in medically underserved settings, and this effect may be especially pronounced for women who have not been previously screened.3, 29 We found that PN is effective in increasing mammography utilization among minority or underserved communities similar to other recent meta-analyses.8, 9 However, there was significant qualitative and quantitative heterogeneity with a great deal of variability in the design and implementation of the programs assessed. Additional studies would help clarify the significance and identify patients most likely to benefit from PN. To facilitate the aforementioned task, exploring the sources of heterogeneity and its significance is important.
Our findings suggest that follow-up time is one of the important sources of heterogeneity, which could be explained by the results of several previously published studies, demonstrating that longer trials demonstrated greater benefits, and shorter trials may underestimate the effectiveness of PN.30, 31 Trialists and policy makers should anticipate this lag when studying and implementing PN, as PN evidently takes time to achieve maximum benefit.6, 30 Other sources of heterogeneity, such as education and race, suggest that PN may be useful in hel** certain patients navigate the health care system.
Reducing mortality rate through breast cancer screening will be incompletely realized if timely diagnostic follow-up for abnormal screening does not occur. We found a trend toward improved diagnostic resolution with a reduction in the number of days between the abnormal mammogram and final disposition. The paucity of trials limited our ability to provide definitive recommendations.
Our study has a number of limitations: first, most of the studies were from the USA; second, we identified evidence of publication bias as it is likely that small studies with negative results could remain unpublished; third, we found that PN doubled diagnostic resolution, an important clinical difference. The lack of statistical significance could be explained by the few included studies; our analysis lacked power. That we reduced the time but not the odds may also reflect differences in parametric and nonparametric tests in demonstrating statistical significance; finally, some studies combined data on the impact of PN on breast, cervical, and rectal screening, making it impossible to extract the data of the breast screening population.
Women needing breast cancer screening are a heterogeneous group, varying by menopausal status, age, education, and race. PN may be particularly useful in assuring screening and follow-up for vulnerable women. PN improves screening rates. Additional studies are required to assess the impact on diagnostic resolution, to determine which subgroups may benefit most and what types of PN interventions are most effective.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Change history
05 January 2023
A Correction to this paper has been published: https://doi.org/10.1007/s11606-022-07944-0
References
DeSantis CE, Bray F, Ferlay J, Lortet-Tieulent J, Anderson BO, Jemal A. International variation in female breast cancer incidence and mortality rates. Cancer Epidemiol Biomark Prev. 2015;24(10):1495-1506.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424.
Wells KJ, Battaglia TA, Dudley DJ, Garcia R, Greene A, Calhoun E, et al. Patient navigation: state of the art or is it science? Cancer. 2008;113(8):1999-2010.
Ramachandran A, Snyder FR, Katz ML, Darnell JS, Dudley DJ, Patierno SR, et al. Barriers to health care contribute to delays in follow-up among women with abnormal cancer screening: data from the Patient Navigation Research Program. Cancer. 2015;121(22):4016-4024.
Bastani R, Mojica CM, Berman BA, Ganz PA. Low-income women with abnormal breast findings: results of a randomized trial to increase rates of diagnostic resolution. Cancer Epidemiol Biomark Prev. 2010;19(8):1927-1936.
Battaglia TA, Bak SM, Heeren T, Chen CA, Kalish R, Tringale S, et al. Boston Patient Navigation Research Program: the impact of navigation on time to diagnostic resolution after abnormal cancer screening. Cancer Epidemiol Biomark Prev. 2012;21(10):1645-1654.
Hoare T, Thomas C, Biggs A, Booth M, Bradley S, Friedman E. Can the uptake of breast screening by Asian women be increased? A randomized controlled trial of a linkworker intervention. J Public Health Med. 1994;16(2):179-185.
Li C, Liu Y, Xue D, Chan CWH. Effects of nurse-led interventions on early detection of cancer: a systematic review and meta-analysis. Int J Nurs Stud. 2020;110:103684.
Nelson HD, Cantor A, Wagner J, Jungbauer R, Fu R, Kondo K, et al. Effectiveness of patient navigation to increase cancer screening in populations adversely affected by health disparities: a meta-analysis. J Gen Intern Med. 2020;35(10):3026-3035.
Lipscomb J, Fleming ST, Trentham-Dietz A, Kimmick G, Wu XC, Morris CR, et al. What predicts an advanced-stage diagnosis of breast cancer? Sorting out the influence of method of detection, access to care, and biologic factors. Cancer Epidemiol Biomark Prev. 2016;25(4):613-623.
Battaglia TA, Roloff K, Posner MA, Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population. A patient navigation intervention. Cancer. 2007;109(2 Suppl):359-367.
Zhou Z, Zhou R, Wei W, Luan R, Li K. Effects of music-based movement therapy on motor function, balance, gait, mental health, and quality of life for patients with Parkinson’s disease: a systematic review and meta-analysis. Clin Rehabil. 2021;35(7):937-951.
Nuño T, Martinez ME, Harris R, García F. A Promotora-administered group education intervention to promote breast and cervical cancer screening in a rural community along the U.S.-Mexico border: a randomized controlled trial. Cancer Causes Control. 2011;22(3):367-374.
Ginsburg OM, Chowdhury M, Wu W, Chowdhury MT, Pal BC, Hasan R, et al. An mHealth model to increase clinic attendance for breast symptoms in rural Bangladesh: can bridging the digital divide help close the cancer divide? Oncologist. 2014;19(2):177-185.
Marshall JK, Mbah OM, Ford JG, Phelan-Emrick D, Ahmed S, Bone L, et al. Effect of patient navigation on breast cancer screening among African American Medicare beneficiaries: a randomized controlled trial. J Gen Intern Med. 2016;31(1):68-76.
Atlas SJ, Zai AH, Ashburner JM, Chang Y, Percac-Lima S, Levy DE, et al. Non-visit-based cancer screening using a novel population management system. J Am Board Fam Med. 2014;27(4):474-485.
Percac-Lima S, Ashburner JM, Zai AH, Chang Y, Oo SA, Guimaraes E, et al. Patient navigation for comprehensive cancer screening in high-risk patients using a population-based health information technology system: a randomized clinical trial. JAMA Intern Med. 2016;176(7):930-937.
Phillips CE, Rothstein JD, Beaver K, Sherman BJ, Freund KM, Battaglia TA. Patient navigation to increase mammography screening among inner city women. J Gen Intern Med. 2011;26(2):123-129.
Maxwell AE, Jo AM, Crespi CM, Sudan M, Bastani R. Peer navigation improves diagnostic follow-up after breast cancer screening among Korean American women: results of a randomized trial. Cancer Causes Control. 2010;21(11):1931-1940.
Braun KL, Thomas WL, Jr., Domingo JL, Allison AL, Ponce A, Haunani Kamakana P, et al. Reducing cancer screening disparities in medicare beneficiaries through cancer patient navigation. J Am Geriatr Soc. 2015;63(2):365-370.
Slater JS, Parks MJ, Nelson CL, Hughes KD. The efficacy of direct mail, patient navigation, and incentives for increasing mammography and colonoscopy in the Medicaid population: a randomized controlled trial. Cancer Epidemiol Biomark Prev. 2018;27(9):1047-1056.
Ferrante JM, Chen PH, Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. J Urban Health. 2008;85(1):114-124.
Dudley DJ, Drake J, Quinlan J, Holden A, Saegert P, Karnad A, et al. Beneficial effects of a combined navigator/promotora approach for Hispanic women diagnosed with breast abnormalities. Cancer Epidemiol Biomark Prev. 2012;21(10):1639-1644.
Raich PC, Whitley EM, Thorland W, Valverde P, Fairclough D. Patient navigation improves cancer diagnostic resolution: an individually randomized clinical trial in an underserved population. Cancer Epidemiol Biomark Prev. 2012;21(10):1629-1638.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:Ed000142.
Siddaway AP, Wood AM, Hedges LV. How to do a systematic review: a best practice guide for conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annu Rev Psychol. 2019;70:747-770.
Delgado-Rodríguez M, Sillero-Arenas M. Systematic review and meta-analysis. Med Int. 2018;42(7):444-453.
Hoffman HJ, LaVerda NL, Young HA, Levine PH, Alexander LM, Brem R, et al. Patient navigation significantly reduces delays in breast cancer diagnosis in the District of Columbia. Cancer Epidemiol Biomark Prev. 2012;21(10):1655-1663.
Paskett ED, Harrop JP, Wells KJ. Patient navigation: an update on the state of the science. CA Cancer J Clin. 2011;61(4):237-249.
Freund KM, Battaglia TA, Calhoun E, Darnell JS, Dudley DJ, Fiscella K, et al. Impact of patient navigation on timely cancer care: the Patient Navigation Research Program. J Natl Cancer Inst. 2014;106(6).
Battaglia TA, Darnell JS, Ko N, Snyder F, Paskett ED, Wells KJ, et al. The impact of patient navigation on the delivery of diagnostic breast cancer care in the National Patient Navigation Research Program: a prospective meta-analysis. Breast Cancer Res Treat 2016;158(3):523-534.
Funding
This research was supported by grants from Tian** Third Central Hospital National Natural Science Foundation Incubation Project of China (Grant No. 2019YNR1), and Tian** Municipal health and Health Committee Science and Technology Talent Cultivation Project of China (Grant No. KJ20008).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lei Huang and Jie Liu should be considered as joint first authors.
Supplementary Information
ESM 1
(DOCX 13 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tian, L., Huang, L., Liu, J. et al. Impact of Patient Navigation on Population-Based Breast Screening: a Systematic Review and Meta-analysis of Randomized Clinical Trials. J GEN INTERN MED 37, 2811–2820 (2022). https://doi.org/10.1007/s11606-022-07641-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-022-07641-y