Abstract
Purpose
Medulloblastoma is a rare tumor in adults. The objective of this nationwide, multicenter study was to evaluate the toxicity and efficacy of the Dutch treatment protocol for adult medulloblastoma patients.
Methods
Adult medulloblastoma patients diagnosed between 2010 and 2018 were identified in the Dutch rare tumors registry or nationwide pathology database. Patients with intention to treat according to the national treatment protocol were included. Risk stratification was performed based on residual disease, histological subtype and extent of disease. All patients received postoperative radiotherapy [craniospinal axis 36 Gy/fossa posterior boost 19.8 Gy (14.4 Gy in case of metastases)]. High-risk patients received additional neoadjuvant (carboplatin-etoposide), concomitant (vincristine) and adjuvant chemotherapy (carboplatin-vincristine-cyclophosphamide) as far as feasible by toxicity. Methylation profiling, and additional next-generation sequencing in case of SHH-activated medulloblastomas, were performed.
Results
Forty-seven medulloblastoma patients were identified, of whom 32 were treated according to the protocol. Clinical information and tumor material was available for 28 and 20 patients, respectively. The histological variants were mainly classic (43%) and desmoplastic medulloblastoma (36%). Sixteen patients (57%) were considered standard-risk and 60% were SHH-activated medulloblastomas. Considerable treatment reductions and delays in treatment occurred due to especially hematological and neurotoxicity. Only one high-risk patient could complete all chemotherapy courses. 5-years progression-free survival (PFS) and overall survival (OS) for standard-risk patients appeared worse than for high-risk patients (PFS 69% vs. 90%, OS 81% vs. 90% respectively), although this wasn’t statistically significant.
Conclusion
Combined chemo-radiotherapy is a toxic regimen for adult medulloblastoma patients that may result in improved survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medulloblastoma is a Central Nervous System (CNS) WHO grade 4 primary brain tumor located in the cerebellum. The incidence of medulloblastoma in adults is approximately 0.6 per 1,000,000 per year, compared to 4.1 per 1,000,000 in children [1, 2]. The 2007 WHO classification of CNS tumors divided medulloblastomas into five histological variants: desmoplastic, classic, anaplastic, large cell and medulloblastoma with extensive nodularity [3]. More recently, various molecular subgroups have been recognized with distinct clinical behavior and outcomes [4, 5]. Methylation-based classification changed the diagnostic approach and made it possible to diagnose brain tumors more precisely [6]. In the 2021 WHO classification of CNS tumors, the medulloblastoma types are designated as WNT-activated, SHH-activated/TP53-wildtype, SHH-activated/TP53-mutant and non-WNT/non-SHH (Group 3/4) [7].
Most treatment protocols for adult medulloblastoma patients are based on studies in children, due to limited availability of (prospective) studies in adults. However, adults tolerate chemotherapy less well than children [8, 9]. In 2010, in order to standardize treatment, the Dutch Society for Neuro-Oncology (LWNO) developed a treatment protocol for adult medulloblastoma patients based on the available literature at a time when only one prospective study on treatment of adult medulloblastoma had been published [10]. Since 2010, the large majority of adult medulloblastoma patients in the Netherlands have been treated according to this national treatment protocol. In this nation-wide study, we report the toxicity and efficacy of the treatment regime described in this protocol using an intention-to-treat analysis and correlate the clinical features and outcome to molecular characteristics.
Materials and methods
Patient and tumor material
Adult patients (18 years or older) diagnosed with a medulloblastoma between January 1st 2010 and October 15th 2018 were included if the treatment was intended to follow the national treatment protocol (see below). To collect all data, treated patients were identified from the prospective Dutch rare tumors registry and from the PALGA-database, a Dutch nationwide network and pathology registry. Pathology laboratories send all excerpts (summary of original pathology report including coding lines and pathologist’s conclusion) to this database, which is then encoded by a Trusted Third Party (ZorgTTP) [11]. All patients provided written informed consent and the study was approved by the Medical Ethics Review Committees of the Erasmus Medical Centre (EMC) and other participating institutions (after co-assessment).
Molecular analysis
FFPE tissue sections, mounted on glass slides were scored by a neuropathologist (MK) to identify areas with high tumor content. Selected areas were macrodissected from adjacent unstained slides (IdH) and DNA was extracted using the QIAamp DNA FFPE Tissue Kit: Cat. No./ID: 56404 and run on Illumina Infinium Human Methylation EPIC arrays to obtain genome-wide DNA methylation profiles. Data were uploaded to the DKFZ/Heidelberg Brain tumor classifier (version 11b4; www.molecularneuropathology.org [12]) to provide methylation (sub)class and copy number variation profiles. Data of non-WNT/non-SHH tumors was additionally uploaded to the Medulloblastoma classifier group 3/4 (version 1.0) to determine the subtype. We included all tumors with a calibrated Classifier score of ≥ 0.84 [13]. For tumors below the cut-off value, we only included samples if there was a plausible explanation for the lower value, such as a rare histological subtype. In SHH-activated medulloblastomas, next-generation sequencing (NGS) was performed to determine the TP53-status and other mutations. By using a NGS panel frequently mutated genes could be assessed [14].
Treatment protocol
The national treatment protocol is listed in Fig. 1A. In brief, primary treatment, i.e. surgical resection, was followed by a postoperative MRI within 72 h. In case of residual disease of > 1.5 cm2, a second look operation within 2 weeks was advised, if judged feasible. We divided patients into risk categories, depending on the presence of residual disease of > 1.5 cm2, histological subtype (high-risk in case of large cell/anaplastic phenotype) and extent of disease (presence/absence of metastatic dissemination) [15].
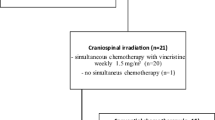
National treatment protocol (A) [17] and overview of patient selection process (B)
Standard-risk patients received postoperative craniospinal irradiation (CSI), whereas high-risk patients received additional neoadjuvant, concomitant and adjuvant chemotherapy. The radiotherapy protocol consisted of CSI (36 Gy; 20 × 1.8 Gy) and a boost on the posterior fossa (19.8 Gy; 11 × 1.8 Gy), or if present posterior fossa and metastases (14.4 Gy; 8 × 1.8 Gy), with a total dose of 50.4–55.8 Gy. The radiotherapy dosage was equal for standard and high-risk patients. All patients received photon radiotherapy; proton radiotherapy was not available before 2018. Standard-risk patients started radiotherapy as soon as they had recovered from surgery. This should commence within 4 weeks of surgery, but preferably within 21 days. High-risk patients received two courses of neoadjuvant chemotherapy (every 3 weeks) prior to radiotherapy. Chemotherapy consisted of carboplatin IV AUC 6 mg/ml/min on day 1 and etoposide IV 150 mg/m2 on days 1–2, preferably starting within 21 days of surgery. Radiotherapy combined with concomitant vincristine (IV 1.5 mg/m2 (max. 2 mg) every 2 weeks) was aimed to start within 3 weeks of the second neoadjuvant course. Patients started with adjuvant chemotherapy after recovering from radiotherapy, preferably within 4–6 weeks after the last fraction. Post-radiation chemotherapy consisted of four 42-day courses of chemotherapy, with carboplatin IV AUC 6 mg/ml/min on day 1, vincristine IV 1.5 mg/m2 (max. 2 mg) on days 1, 8 and 15, and cyclophosphamide 750 mg/m2 on days 22 and 23 (Fig. 1A). Toxicity was evaluated using the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0 [16]. Dose delays and reductions were collected. Toxicity and dose-intensity analysis was limited to patients who received the first course or fraction of the advised therapy.
Statistical analysis
Patient demographics, tumor and treatment characteristics were summarized using descriptive statistics for quantitative data (median with range, count and percentage). All statistical analyses were performed using SPSS (Version 22). We performed survival analyses for standard/high-risk groups and risk groups per methylation subgroup using Kaplan–Meier analysis. Progression-free (PFS) and overall survival (OS) were defined as the time from date of surgery until date of first event (progression/relapse) or death due to all causes, respectively. A log-rank test was used to test the significant difference. An independent samples t-test was used to test the significant difference between age groups. A p-value of < 0.05 was considered significant.
Results
Patient characteristics
Twenty-nine adult medulloblastoma patients were registered in the Dutch rare tumors registry between January 1, 2010 and October 15, 2018. Eighteen patients were additionally identified in the PALGA-database. Six patients had to be excluded because they were treated in a hospital that followed another treatment protocol. Another 13 cases were excluded for multiple reasons (see Fig. 1B). Thirty-two patients were treated following the treatment protocol. We received the clinical information and tumor material of 28 and 20 patients, respectively, from 10 neuro-oncology centers. The selection process is shown in Fig. 1B.
Baseline and treatment characteristics are shown in Table 1. Eighteen patients were male (64%). Median age was 29.5 years (range 18–46). At time of diagnosis, twenty-three patients (82%) had a good performance status (Karnofsky performance score 70–100). The histological variants were mainly classic (43%) and desmoplastic (36%). Twelve patients (43%) were classified as high-risk. One patient was 17 weeks pregnant at time of diagnosis.
Methylation profiling
Upon methylation profiling the calibrated score for three tumors was below 0.84: one patient had a rare histological subtype, medullomyoblastoma, and was included in our cohort despite the lower Classifier score (0.72). The molecular results of the other two patients were not included. The CNV plot was noisy in one of them suggesting low-quality/technical issues. The most frequent molecular subtype was SHH-activated (60%), followed by non-WNT/non-SHH (25%) and WNT-activated (5%). All desmoplastic medulloblastomas belonged to the SHH-activated subtype. The single WNT-activated tumor had a classic phenotype. The correlation between molecular and histological subtype is shown in Fig. 2. Patients with SHH-activated medulloblastomas were generally older (median 30 years; range 18–44) compared to those with non-SHH-activated tumors (median 23 years, range 18–28), although this difference was not statistically significant (p = 0.07).
Two SHH-activated medulloblastomas (17%) had subclonal loss of chromosome 10q and chromosome 17p loss. One of them had additional chromosome 3p loss (8%). No non-WNT/non-SHH tumors had chromosome 8p or 8q losses (Fig. 2). Additional NGS was performed of 10 SHH-activated medulloblastomas. The NGS result of one tumor was unreliable. A TP53 mutation was found in one of the SHH-activated medulloblastomas. Of additional mutations in SHH-activated tumors, TERT promoter mutation was most frequently observed (90%), followed by PTCH1 (40%), DDX3X (30%) and SMO mutation (20%; Fig. 2).
Treatment and toxicities
Treatment
Four of the 28 patients underwent a second operation due to residual tumor. Twenty-six of the 28 patients received the advised radiotherapy dose. Two patients received a lower radiation dose than advised in the treatment protocol without reported reason. In one high-risk patient treatment order was changed due to pregnancy (carboplatin/etoposide courses followed by one course carboplatin/vincristine/cyclophosphamide and, after childbirth, radiotherapy), while one high-risk patient refused all chemotherapy. Neoadjuvant chemotherapy was given to 10 of the 12 high-risk patients. One patient with postoperative meningitis was not given neoadjuvant chemotherapy due to long treatment delay. Eight high-risk patients received vincristine during the radiation phase (67%). Besides the already mentioned pregnancy or chemotherapy refusal, in two other patients no reason for omitting vincristine was given. Adjuvant chemotherapy was started according to treatment protocol in 10 (83%) high-risk patients. We excluded the pregnant and chemotherapy refusing patients for postoperative time to treatment and dose delays/reductions evaluation. Table 1 shows the median treatment intervals. In one of four patients with a second operation, this could be performed within the per-protocol specified treatment window. Half of them had a high-risk subtype. Neoadjuvant chemotherapy started within 21 days of surgery in 30% of the patients (median 27, range 17–52). Radiotherapy started within the per-protocol specified treatment window in only 25% of the standard-risk and 30% of the high-risk patients. Median time between surgery and radiotherapy was 40 days (range 20–161) for standard-risk and 71 days (range 38–94) for high-risk patients, with delay mostly brief (median delay for standard-risk 12 days vs. high-risk 8 days). Postoperative infections were the cause of longer delays. In 70% of the patients who received adjuvant chemotherapy, this was started within the per-protocol specified treatment window [median 75 days after start radiotherapy (range 67–98)].
Dose delays/reductions
The neoadjuvant chemotherapy dose was reduced in one (11%) and 1-week delayed in two (22%) patients. The dose of the second course was not reported in one patient. Seven of the eight patients receiving vincristine during the chemo-radiation phase received the advised three administrations. Radiotherapy was 1-week delayed in one patient (4%). Only one of 10 patients received the total dose of adjuvant chemotherapy as prescribed in the treatment protocol. The dose was reduced or a part of the chemotherapy was discontinued during the adjuvant chemotherapy due to adverse events in nine patients (90%): treatment reductions were made for two patients in the first course (20%), for five patients in the second course (50%) and for eight patients in the third and fourth courses (80%). Adjuvant chemotherapy was completely discontinued after course three in one patient due to toxicity (10%). Especially vincristine was reduced or stopped early due to neuropathy during adjuvant courses. The delays in adjuvant chemotherapy varied between 0 and 5 weeks (median 1 week).
Toxicity
Toxicity could be evaluated in 27 of the 28 patients (Table 2). In one high-risk patient, the radiotherapy phase was not reported. The pregnant patient was only included for the neoadjuvant phase, as the treatment changed afterwards. Hematological toxicity, especially leukopenia (33%) and thrombocytopenia (26%), were most frequently reported CTCAE (v4.0) grade 3–4 toxicity in the whole cohort, thereafter gastro-intestinal toxicity (22%) and infections (15%) were reported. In the high-risk group, hematological toxicity was the only high-grade toxicity reported during the neoadjuvant chemotherapy (leukopenia in 20% and thrombocytopenia in 10%).
Especially high-grade gastro-intestinal toxicity, due to radiotherapy, was reported in the standard-risk group (gastrointestinal toxicity 27%, leukopenia 7% and infection 7%). Whereas in the high-risk group treated with chemoradiation, more high-grade (hematological) toxicity occurred (leukopenia 10%, thrombocytopenia 30%, gastrointestinal toxicity 20% and fatigue 10%). Most adverse events were reported during the adjuvant chemotherapy; in 100% of the patients at least one adverse event was reported at that stage. Grade 3–4 thrombocytopenia and leukopenia were reported in 50% and 80% of the patients, respectively. Eighty percent of the patients had at least one high-grade adverse event during treatment. No fatal adverse events occurred.
Survival
The median follow-up time was 67 months (range 8–111). 5-years PFS was 69% for the standard-risk and 90% for the high-risk group (p = 0.248). 5-years OS was 81% for the standard-risk and 90% for the high-risk group (p = 0.358). Survival for standard-risk patients seemed worse than for high-risk patients, although this difference was not statistically significant. Also, no significant differences were found for the risk group per methylation subgroup (Fig. 3). All patients with either a WNT-activated or high-risk SHH-activated tumor were still alive and without progression at the end of the study period. Three of the five patients with non-WNT/non-SHH tumors had no progression after 5 years (Fig. 3B). Disease progression was seen in one of four patients with a PTCH1 mutation (25%) and in one of three patients with a SMO mutation (33%) after 25 and 32 weeks, respectively. The only patient with a SHH-activated/TP53-mutant medulloblastoma showed progression after 4 years.
Discussion
In this study, we evaluated the toxicity and efficacy of the Dutch national treatment protocol for patients diagnosed with medulloblastoma in adulthood. As in other series [18], the median age of patients was in the late 20 s, the majority of patients had a SHH-activated medulloblastoma and were considered standard-risk. All of our patients received photon-CSI, whereas recent literature showed that proton-CSI leads to less treatment-related morbidity [19]. The chemotherapy treatment schedule was based on previously published regimens for adults but was not tolerated well as only one patient completed all chemotherapy courses. All other patients received adjusted schedules because of toxicity. Especially hematological and gastro-intestinal toxicity were reported frequently. Vincristine was strongly associated with neurotoxicity; early discontinuation during the adjuvant chemotherapy occurred in 50% of the patients. Chemotherapy toxicity also resulted in considerable delays in further treatment. Our data are similar to previous studies showing that adults tolerate chemotherapy poorly compared with children: in the Packer protocol, all adults needed dose reductions due to hematological toxicity, whereas only 14% of the children needed treatment adjustments [8]. More severe (hematological) adverse events were also found in older patients treated in the NOA-07 trial [20], in which all patients were treated with chemotherapy and photon-CSI.
Despite the observed delays in especially radiotherapy in our cohort, survival rates were comparable to published rates. The difference in PFS favoring high-risk patients, a known poor prognostic factor, is intriguing and may be explained by the effects of chemotherapy [18, 21]. The poor tolerance of chemotherapy suggests that our treatment protocol requires adjustments to make it feasible for more patients; the chemotherapy administration may be of greater importance than meeting our per-protocol specified deadlines. Moreover, the difference in survival between the standard-risk and high-risk patients was not significant and PFS and OS were similar to those found by Brandes et al., on which our treatment schedule was based [10]. Studies with (intention to) chemo-radiotherapy for all patients observed 57–68% PFS and 70–89% OS during a follow-up period of 3–5 years [20, 22, 23], also comparable with our findings.
We compared survival between methylation subclasses and found no significant differences. Although this may have been the result of the small number of patients, other series also have failed to identify differences in survival between these categories in adults, as opposed to children[24, 25]. The majority of patients in our cohort had a SHH-subtype (60%). Further molecular stratification of these tumors revealed a high prevalence of TERT promoter, DDX3X, PTCH1 and SMO mutations and low prevalence of TP53 mutations, which is in line with previous literature [25, 26]. Previous studies showed that TP53 mutations are associated with unfavorable outcome [25,26,27], though the only patient in our cohort showed progression only after 4 years. TERT promoter mutations are reported to be associated with a favorable outcome in patients of SHH-activated tumors but a poor outcome in patients with Group 4 tumors [28]. Conflicting data exist regarding prognostic value of PTCH1 and SMO mutations [22, 25]. The majority of patients with PTCH1 or SMO mutations in our cohort survived without progression.
Beside mutations, previous studies in adult patients with SHH-activated tumors have shown that chromosome 3p, 10q or 17p losses were correlated with decreased survival. In contrast, patients with chromosome 8 loss in Group 4 tumors had improved outcomes [22, 25]. In our cohort, the patients with subclonal chromosome 10q loss, chromosome 3p and/or 17p losses survived during the follow-up period. There was no chromosome 8 loss in Group 4 medulloblastomas in our series. Of note, the treatment regimen of our study wasn’t based on molecular stratification.
The strength of our study is the nationwide multicenter consecutive series of patients treated in a uniform manner. Limitations are the relatively low patient numbers and lack of a uniform and standardized registration of adverse events. No significant results were found regarding prognostication of medulloblastoma subgroups. WNT-activated and non-WNT/non-SHH-activated medulloblastomas are underrepresented in adults; this makes prognostication research in these subgroups challenging. However, we showed that toxicity of neoadjuvant chemotherapy led to delay in radiotherapy initiation in more than 2/3 of patients but that nevertheless survival was comparable to that in other series. Moreover, the similar survival shows that chemotherapy is an important modality to consider in medulloblastoma patients [9, 21]. Moots et al. found disease progression in two adult medulloblastoma patients during neo-adjuvant chemotherapy [29]. The Dutch treatment protocol was amended recently for standard-risk patients to radiotherapy combined with concomitant and adjuvant chemotherapy [30]. Also, proton-CSI is now used, which leads to less bone marrow depression and therefore allows for more dose-intense adjuvant chemotherapy administration [19]. Some of the frequent mutations, such as those activating the SHH pathway, hold promise for more tailored treatment. SMO inhibitors, as selective antagonist of this pathway, will be investigated in a prospective trial [31]. Further molecular characterization and discovering new targetable mutations can be appealing steps towards more personalized treatment. For the development of robust risk stratification, international collaboration is required because of the rarity of the medulloblastoma in adults.
Data availability
Raw data that supports the finding of this study are available from the corresponding author, upon reasonable request.
References
Smoll NR, Drummond KJ (2012) The incidence of medulloblastomas and primitive neurectodermal tumours in adults and children. J Clin Neurosci 11:1541–1544. https://doi.org/10.1016/j.jocn.2012.04.009
Ostrom QT, Gittleman H, Liao P et al (2014) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro-Oncol 16:iv1-63. https://doi.org/10.1093/neuonc/nou223
Louis DN, Ohgaki H, Wiestler OD et al (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109. https://doi.org/10.1007/s00401-007-0243-4
Schwalbe EC, Lindsey JC, Nakjang S et al (2017) Novel molecular subgroups for clinical classification and outcome prediction in childhood medulloblastoma: a cohort study. Lancet Oncol 18(7):958–971. https://doi.org/10.1016/S1470-2045(17)30243-7
Cavalli FMG, Remke M, Rampasek L et al (2017) Intertumoral heterogeneity within medulloblastoma subgroups. Cancer Cell 31(6):737-754.e6. https://doi.org/10.1016/j.ccell.2017.05.005
Priesterbach-Ackley LP, Boldt HB, Petersen JK et al (2020) Brain tumour diagnostics using a DNA methylation-based classifier as a diagnostic support tool. Neuropathol Appl Neurobiol 46(5):478–492. https://doi.org/10.1111/nan.12610
Louis DN, Perry A, Wesseling P et al (2021) The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol 23(8):1231–1251. https://doi.org/10.1093/neuonc/noab106
Greenberg HS, Chamberlain MC, Glantz MJ, Wang S (2001) Adult medulloblastoma: multiagent chemotherapy. Neuro Oncol 3(1):29–34. https://doi.org/10.1093/neuonc/3.1.29
Franceschi E, Hofer S, Brandes AA et al (2019) EANO-EURACAN clinical practice guideline for diagnosis, treatment, and follow-up of post-pubertal and adult patients with medulloblastoma. Lancet Oncol 20(12):e715–e728. https://doi.org/10.1016/S1470-2045(19)30669-2
Brandes AA, Franceschi E, Tosoni A, Blatt V, Ermani M (2007) Long-term results of a prospective study on the treatment of medulloblastoma in adults. Cancer 110(9):2035–2041. https://doi.org/10.1002/cncr.23003
Casparie M, Tiebosch ATMG, Burger G et al (2007) Pathology databanking and biobanking in the Netherlands, a central role for PALGA, the Nationwide histopathology and cytopathology data network and archive. Cell Oncol 29(1):19–24. https://doi.org/10.1155/2007/971816
Capper D, Jones DTW, Sill M et al (2018) DNA methylation-based classification of central nervous system tumours. Nature 555(7697):469–474. https://doi.org/10.1038/nature26000
Capper D, Stichel D, Sahm F et al (2018) Practical implementation of DNA methylation and copy-number-based CNS tumor diagnostics: the Heidelberg experience. Acta Neuropathol 136:181–210. https://doi.org/10.1007/s00401-018-1879-y
Synhaeve NE, van den Bent MJ, French PJ et al (2018) Clinical evaluation of a dedicated next generation sequencing panel for routine glioma diagnostics. Acta Neuropathol Commun 6(1):126. https://doi.org/10.1186/s40478-018-0633-y
Dutch neuro-oncology society (2017) Medulloblastoma in adults: treatment protocol. LWNO. https://lwno.nl/media/1014/treatment_protocol_medulloblastoma_23-01-2017_final.pdf. Accessed 30 Jan 2023
U.S. Department of Health and Human Services (2010) Common terminology criteria for adverse events (CTCAE) version 4.03. Accessed 29 Aug 2022
Bromberg JEC, Gijtenbeek JMM, Westerman AM et al (2011) Medulloblastoma in adults: treatment protocol Dutch Society for Neuro-Oncology. Tijdschrift voor Neurologie en Neurochirurgie 112(6):273–278
Kann BH, Lester-Coll NH, Park HS et al (2017) Adjuvant chemotherapy and overall survival in adult medulloblastoma. Neuro Oncol 19(2):259–269. https://doi.org/10.1093/neuonc/now150
Brown AP, Barney CL, Grosshans DR et al (2013) Proton beam craniospinal irradiation reduces acute toxicity for adults with medulloblastoma. Int J Radiat Oncol Biol Phys 86(2):277–284. https://doi.org/10.1016/j.ijrobp.2013.01.014
Beier D, Proescholdt M, Reinert C et al (2018) Multicenter pilot study of radiochemotherapy as first-line treatment for adults with medulloblastoma (NOA-07). Neuro Oncol 20(3):400–410. https://doi.org/10.1093/neuonc/nox155
Kocakaya S, Beier CP, Beier D (2016) Chemotherapy increases long-term survival in patients with adult medulloblastoma–a literature-based meta-analysis. Neuro Oncol 18(3):408–416. https://doi.org/10.1093/neuonc/nov185
Korshunov A, Okonechnikov K, Stichel D et al (2021) Integrated molecular analysis of adult sonic hedgehog (SHH)-activated medulloblastomas reveals two clinically relevant tumor subsets with VEGFA as potent prognostic indicator. Neuro Oncol 23(9):1576–1585. https://doi.org/10.1093/neuonc/noab031
Friedrich C, von Bueren AO, von Hoff K et al (2013) Treatment of adult nonmetastatic medulloblastoma patients according to the paediatric HIT 2000 protocol: a prospective observational multicentre study. Eur J Cancer 49(4):893–903. https://doi.org/10.1016/j.ejca.2012.10.006
Ramaswamy V, Remke M, Bouffet E et al (2016) Risk stratification of childhood medulloblastoma in the molecular era: the current consensus. Acta Neuropathol 131(6):821–831. https://doi.org/10.1007/s00401-016-1569-6
Coltin H, Sundaresan L, Smith KS et al (2021) Subgroup and subtype-specific outcomes in adult medulloblastoma. Acta Neuropathol 142(5):859–871. https://doi.org/10.1007/s00401-021-02358-4
Kool M, Jones DT, Jäger N et al (2014) Genome sequencing of SHH medulloblastoma predicts genotype-related response to smoothened inhibition. Cancer Cell 25(3):393–405. https://doi.org/10.1016/j.ccr.2014.02.004
Zhukova N, Ramaswamy V, Remke M et al (2013) Subgroup-specific prognostic implications of TP53 mutation in medulloblastoma. J Clin Oncol 31(23):2927–2935. https://doi.org/10.1200/JCO.2012.48.5052
Remke M, Ramaswamy V, Peacock J et al (2013) TERT promoter mutations are highly recurrent in SHH subgroup medulloblastoma. Acta Neuropathol 126(6):917–929. https://doi.org/10.1007/s00401-013-1198-2
Moots PL, O’Neill A, Londer H et al (2018) Preradiation chemotherapy for adult high-risk medulloblastoma: a trial of the ECOG-ACRIN Cancer Research Group (E4397). Am J Clin Oncol 41(6):588–594. https://doi.org/10.1097/COC.0000000000000326
Dutch neuro-oncology society (2019) Medulloblastoma in adults: treatment protocol. LWNO. https://lwno.nl/media/1061/treatment-protocol-medulloblastoma-_-20190507.pdf. Accessed 16 Feb 2023
Li Y, Song Q, Day BW (2019) Phase I and phase II sonidegib and vismodegib clinical trials for the treatment of paediatric and adult MB patients: a systemic review and meta-analysis. Acta Neuropathol Commun 7(1):123. https://doi.org/10.1186/s40478-019-0773-8
Funding
Funding was received from: Remmert Adriaan Laan Fonds, Amsterdam, the Netherlands.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by LB, IH, JMK and PJF. The first draft of the manuscript was written by LB. IH, PJF, MCMK, PW and JECB commented on previous versions of the manuscript. The others authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
C.C.D. van der Rijt received grants from the Netherlands Organization for Health Research and Development and KWF personal fees from Lilly (via her institution) both outside the work described in the manuscript. Other authors have no conflicts of interest.
Consent to participate
Informed consent was obtained from all individual participants included in the study. In case of deceased patients, they were included with assuming approval according to the rules and regulations in the Netherlands.
Consent for publication
This is not applicable.
Ethical approval
Approved by the institutional ethical review board of the Erasmus Medical Centre and additional approval by the local institutional ethical review boards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bleeker, L., Kouwenhoven, M.C.M., de Heer, I. et al. Medulloblastoma in adults: evaluation of the Dutch society for neuro-oncology treatment protocol. J Neurooncol 162, 225–235 (2023). https://doi.org/10.1007/s11060-023-04285-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04285-8