Abstract
We aimed to determine whether there are signs or symptoms that could help clinicians to distinguish between influenza and other respiratory infections. The clinical data for this matched case–control analysis were derived from a 2-year prospective cohort study of respiratory infections among children aged ≤13 years. At any signs of respiratory infection, the children were examined and nasal swabs were obtained for virologic analyses. Cases were 353 children with laboratory-confirmed influenza and controls were 353 children with respiratory symptoms who tested negative for influenza. Cases and controls were matched for gender, age, and timing of the visit. In the multivariate conditional logistic regression analyses, fever was the only sign that independently predicted influenza virus infection, with odds ratios ranging from 13.55 (95% confidence interval [CI], 6.90–26.63) to 50.10 (95% CI, 16.25–154.45), depending on the degree of fever. In all analyses, the predictive capability of fever increased with incremental elevations in the child’s temperature. The likelihood ratio of fever ≥40.0°C in predicting influenza was 6.00 (95% CI, 2.80–12.96). Among unselected children seen as outpatients during influenza outbreaks, fever is the only reliable predictor of influenza virus infection. The optimal use of influenza-specific antiviral drugs in children may require virologic confirmation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Influenza is an important cause of worldwide morbidity in children, and children have been recognized as a high-risk group for influenza both during seasonal outbreaks and the recent 2009 H1N1 pandemic [1–3]. Although most children with influenza are seen as outpatients, children are also frequently hospitalized with influenza-associated conditions [3–8]. In contrast with other viral respiratory infections, specific antivirals oseltamivir and zanamivir are available for the treatment of influenza. When started early during the course of the illness, antiviral therapy has the potential to substantially shorten the duration of illness and to decrease the occurrence of bacterial complications of influenza [9–11].
The optimal use of influenza-specific antivirals in children is seriously hampered by the difficulty in distinguishing influenza from other respiratory viral infections on clinical grounds alone. Previous studies have demonstrated that the accuracy of a clinical diagnosis of influenza is particularly low in the youngest children [12], among whom only a minor proportion of influenza-like illnesses are actually caused by influenza viruses [8, 10, 13, 14].
Enhanced clinical recognition of influenza would be of great importance especially in settings in which laboratory diagnostics are not readily available or when the number of patients exceeds the capacity for viral testing. Besides optimizing the use of antiviral drugs, increased accuracy of identifying influenza virus infections would help avoid the unnecessary use of antibiotics and laboratory tests in children [15] and also improve the proper cohorting of patients on wards. Although some previous studies have assessed the predictive value of signs and symptoms for influenza in selected groups of children [16–18], few data are available on unselected outpatient children who form the majority of pediatric patients seeking medical care during any influenza outbreak [8, 19]. Further, age is an important confounding factor because the clinical features of influenza in children vary with age [20]. We, therefore, sought to determine the predictive capability of various signs and symptoms for influenza in a carefully matched case–control study in which the clinical data were derived from a large prospectively followed up cohort of unselected children [7].
Materials and methods
Participants
This case–control analysis was based on clinical data derived from a prospective cohort study of respiratory infections performed in Turku, Finland, during two consecutive respiratory seasons of 2000–2002 [7]. Before the start of each respiratory season, children ≤13 years of age were recruited into the study cohort without the use of any exclusion criteria. The parents were asked to bring their child to the study clinic whenever the child was febrile or had signs or symptoms of respiratory infection. The study clinic was open every day, and all visits were free of charge to the families. During each visit, a study physician performed a thorough clinical examination of the child and filled out a standardized case record form that contained detailed questions about the signs and symptoms of the child, detailed findings during the clinical examination, results of any laboratory tests or radiographs obtained, and the diagnosis and treatment.
Overall, the 2-year study comprised 2,231 child-seasons of follow-up. The clinical presentation of influenza in different age groups of children has been reported previously [20]. The study protocol was approved by the Ethics Committee of Turku University Hospital, and written informed consent was obtained from the parents of all participating children.
Viral specimens
During each episode of fever or respiratory infection, a nasal swab was obtained for the determination of the viral etiology of the illness. The specimens were obtained from a depth of 2–3 cm in the nostril using a sterile cotton swab that was then inserted into a vial containing viral transport medium [21]. Influenza viruses in the specimens were detected by viral culture in Madin–Darby canine kidney cell line and subsequent immunoperoxidase staining with monoclonal antibodies [22].
Cases and controls
Of a total of 372 children who were diagnosed with culture-confirmed influenza, 17 children were excluded from this analysis because of incomplete data on fever, and two children because of confirmed simultaneous infection with another virus. All of the remaining 353 children with culture-confirmed influenza were included as cases in this study. The controls were children from the same cohort of outpatient children who visited the study clinic because of signs and symptoms of respiratory infection but who tested negative for influenza. For each case, we selected one control child who provided the closest match to the case with respect to gender, age, and the timing of the visit. The controls were selected with the use of a computerized database that did not provide any information about the signs and symptoms of any children. The outcome of the matching procedure was excellent: all case–control pairs were of the same sex; the age difference was ≤4 weeks in 96.0% of the pairs (median difference, 6 days); and the visit to the study clinic occurred within 1 month in 91.2% of the pairs (median difference, 14 days).
Definitions
Gastrointestinal symptoms included diarrhea, vomiting, and abdominal pain. The diagnosis of conjunctivitis required either distinct redness of the conjunctivae or purulent discharge from an eye. Wheezing was defined as expiratory wheezing on auscultation or acute exacerbation of asthma. Laryngitis included distinct hoarseness, barking cough, and inspiratory stridor. Pharyngitis consisted of distinct redness of the throat or the presence of tonsillar exudates. Impaired general condition was defined subjectively by each attending physician.
Data analysis and statistical methods
For each episode of respiratory infection in the children, only signs and symptoms that were recorded at the first visit to the study clinic were included in the analyses. Subjective symptoms (headache, sore throat, and myalgia) were analyzed only in children ≥3 years of age.
Univariate conditional logistic regression was initially used to examine which signs and symptoms were potential predictors of influenza. In order to identify signs or symptoms that were independent predictors of influenza, all variables with a p-value < 0.1 in the univariate analysis were included in the multivariate conditional logistic regression analyses. The results are expressed using odds ratios with 95% confidence intervals (CIs). The likelihood ratio of a positive test was calculated as sensitivity/(1 − specificity), and the likelihood ratio of a negative test was calculated as (1 − sensitivity)/specificity. Statistical analyses were performed with SAS, version 9.2 (SAS Institute Inc., Cary, NC). p-values < 0.05 were considered to be statistically significant.
Results
Patients
A total of 706 children were included in the analyses (353 influenza-positive cases and 353 matched influenza-negative controls). The median age of the children was 4.4 years (mean age, 5.2 years) in both groups. One hundred (28.3%) children in each group were <3 years of age, 160 (45.3%) were 3–6 years of age, and 93 (26.3%) were ≥7 years of age. One hundred and fifty-five (43.9%) children in each group were girls.
Univariate analyses
The frequencies and results of the univariate conditional logistic regression analyses for different signs and symptoms are presented in Table 1. Among all variables, fever was clearly the sign that was the most strongly associated with influenza virus infection, with the highest odds ratio (58.46, 95% CI, 19.36–176.53) being observed for fever ≥40.0°C. Other signs or symptoms significantly associated with influenza included impaired general condition, gastrointestinal symptoms, pharyngitis, headache, and myalgia.
Multivariate analyses
When all variables with a p-value < 0.1 in the univariate analysis were included in the multivariate logistic regression analyses, fever remained the sole independent predictor of influenza (Table 2). None of the other variables reached statistical significance whether analyzed among all children (excluding subjective symptoms), among children ≥3 years of age (including also subjective symptoms), or separately among children <3 years of age.
Likelihood ratios for various signs and symptoms
Table 3 presents the sensitivities, specificities, and likelihood ratios of the presence or absence of various signs and symptoms in predicting influenza in children. Any degree of fever ≥38.0°C was significantly associated with influenza, and the highest likelihood ratio (6.00, 95% CI, 2.80–12.96) was observed for the presence of fever ≥40.0°C. Other variables with statistically significant likelihood ratios included impaired general condition, headache, gastrointestinal symptoms, and pharyngitis.
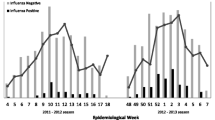
Figure 1 demonstrates a practical application of using likelihood ratios for different levels of fever in children. For example, if 20% of unselected children with medically attended respiratory infections have true influenza (pre-test probability), the presence of fever ≥38.0°C in an individual child increases the probability of influenza to 40%, and the presence of fever ≥40.0°C increases the probability of influenza to 60% (post-test probability). In the same situation, the probability of influenza in a child with a temperature <38.0°C is decreased to 4%.
Discussion
Our carefully matched case–control study among unselected outpatient children demonstrated that, among various signs and symptoms conventionally associated with influenza, fever outdid all others and was the sole sign that could independently predict influenza in children. Moreover, in all analyses, the predictive capability of fever increased with incremental elevations in the child’s temperature. Our findings are well generalizable to clinical practice because the clinical data were collected prospectively from outpatient children who were enrolled in the follow-up cohort without any exclusion criteria. All children were sampled for the determination of the viral etiology of the illness during each episode, regardless of the severity of symptoms or the presence or absence of fever, and no rapid viral tests were used that could have caused selection bias in the analyses. An additional strength of our study was that our cases and controls were very well matched, particularly for age, which is an important confounder for assessing the clinical presentation of influenza in children [20].
To our knowledge, this is the first study to determine the clinical predictors of influenza in children who were not preselected for the presence of influenza by any clinical criteria or laboratory tests. Previously, Friedman and Attia studied children who were selected from emergency department patients at a tertiary care center according to predetermined criteria suggestive of influenza [16]. They found that the symptom triad of cough, headache, and pharyngitis had a sensitivity of 80% and a specificity of 78% in diagnosing influenza in children with a mean age of 6 years. In another study, Ohmit and Monto evaluated the signs and symptoms in children who participated in the clinical trials of the antiviral drugs oseltamivir and zanamivir [17]. Fever ≥37.8°C was used as an inclusion criterion in both trials, and children in the oseltamivir trial also had to test negative for respiratory syncytial virus by the rapid antigen test, which led to high baseline prevalences (66–74%) of influenza among the participants of those trials. In children 5–12 years of age, fever ≥38.2°C, cough, and headache were found to be predictive of influenza, whereas in children 1–4 years of age, the only symptom that increased the likelihood of influenza was myalgia. Recently, Sočan et al. reported on the clinical predictors of influenza in primary care and tertiary hospital clinic patients who were selected for influenza testing by several predetermined clinical criteria [18]. Fever ≥38°C, headache, cough, and lack of abnormal breathing sounds were found to be predictive of influenza in children less than 15 years of age.
Largely in accordance with previous studies, headache, pharyngitis, myalgia, impaired general condition, and gastrointestinal symptoms were associated with influenza in our univariate analysis, but all of these signs and symptoms turned out not to be independent predictors of influenza in the multivariate analyses. Surprisingly, and contrary to previous studies, cough was not significantly associated with influenza, even in the univariate analysis in our study, as this symptom was present in 77% of influenza virus-infected children, but also in 71% of control children.
Likelihood ratios are increasingly recommended to be used for the evaluation of diagnostic tests [23]. Unlike positive and negative predictive values that are conventionally and most frequently reported, likelihood ratios are not dependent on the prevalence of the illness in the population, and, hence, they provide a more robust tool for decision-making. With knowledge of the prevalence of any condition in the population (pre-test probability), likelihood ratios can be used in calculating the probability of that condition in patients with either a positive or a negative test result (post-test probability). As shown in our application of likelihood ratios of different levels of fever to the diagnosis of influenza, fever-associated likelihood ratios appear to be a useful and valuable aid in the clinical diagnosis of influenza in children.
Although the presence of high fever substantially increases the probability of influenza in children, an important limitation is that only a minority of children’s influenza-like illnesses are caused by influenza viruses, even during the peak weeks of influenza activity in the community. Several follow-up studies among unselected outpatient infants and children have demonstrated that influenza virus infections account for a maximum of 25–30% of medically attended respiratory illnesses during influenza epidemics [8, 10, 13, 14]. An additional challenge for the clinical diagnosis of influenza arises from young children’s inability to describe their subjective symptoms. Because the reliability of such symptoms is questionable in young children [24], we did not analyze any subjective symptoms in children <3 years of age.
A limitation of our study is that, because the diagnosis of influenza was based on viral culture alone, some children with influenza may have remained false-negative and, therefore, may have been misclassified as controls. It should be noted, however, that our viral culture method included also subsequent immunoperoxidase staining with monoclonal antibodies [22]. In previous studies, this method has yielded a sensitivity of approximately 90% when compared with polymerase chain reaction (PCR)-based assays for the detection of influenza [10, 25]. Furthermore, because the controls were selected in a blinded manner from a very large database of influenza virus-negative children, the probability for any individual child who may have been false-negative for influenza to end up in the control group was low. Therefore, we consider it unlikely that the viral detection method used would have caused a significant bias to our results.
Taken together, the evidence from the present and previous studies appears to underscore the importance of the virologic confirmation of influenza, particularly in the youngest children. Several rapid test kits that can provide results within 15 min are available. The performance of these tests varies [26, 27], but is usually good in children and during the early course of the illness when, also, the benefits of the antiviral treatment of influenza are greatest [10, 25, 28, 29].
References
Heikkinen T, Booy R, Campins M et al (2006) Should healthy children be vaccinated against influenza? A consensus report of the Summits of Independent European Vaccination Experts. Eur J Pediatr 165:223–228
Jhung MA, Swerdlow D, Olsen SJ et al (2011) Epidemiology of 2009 pandemic influenza A (H1N1) in the United States. Clin Infect Dis 52(Suppl 1):S13–S26
Shrestha SS, Swerdlow DL, Borse RH et al (2011) Estimating the burden of 2009 pandemic influenza A (H1N1) in the United States (April 2009–April 2010). Clin Infect Dis 52(Suppl 1):S75–S82
Neuzil KM, Mellen BG, Wright PF et al (2000) The effect of influenza on hospitalizations, outpatient visits, and courses of antibiotics in children. N Engl J Med 342:225–231
Izurieta HS, Thompson WW, Kramarz P et al (2000) Influenza and the rates of hospitalization for respiratory disease among infants and young children. N Engl J Med 342:232–239
Thompson WW, Shay DK, Weintraub E et al (2004) Influenza-associated hospitalizations in the United States. JAMA 292:1333–1340
Heikkinen T, Silvennoinen H, Peltola V et al (2004) Burden of influenza in children in the community. J Infect Dis 190:1369–1373
Poehling KA, Edwards KM, Weinberg GA et al (2006) The underrecognized burden of influenza in young children. N Engl J Med 355:31–40
Whitley RJ, Hayden FG, Reisinger KS et al (2001) Oral oseltamivir treatment of influenza in children. Pediatr Infect Dis J 20:127–133
Heinonen S, Silvennoinen H, Lehtinen P et al (2010) Early oseltamivir treatment of influenza in children 1–3 years of age: a randomized controlled trial. Clin Infect Dis 51:887–894
Hedrick JA, Barzilai A, Behre U et al (2000) Zanamivir for treatment of symptomatic influenza A and B infection in children five to twelve years of age: a randomized controlled trial. Pediatr Infect Dis J 19:410–417
Peltola V, Reunanen T, Ziegler T et al (2005) Accuracy of clinical diagnosis of influenza in outpatient children. Clin Infect Dis 41:1198–1200
Zambon MC, Stockton JD, Clewley JP et al (2001) Contribution of influenza and respiratory syncytial virus to community cases of influenza-like illness: an observational study. Lancet 358:1410–1416
Heikkinen T, Ziegler T, Peltola V et al (2003) Incidence of influenza in Finnish children. Pediatr Infect Dis J 22:S204–S206
Bonner AB, Monroe KW, Talley LI et al (2003) Impact of the rapid diagnosis of influenza on physician decision-making and patient management in the pediatric emergency department: results of a randomized, prospective, controlled trial. Pediatrics 112:363–367
Friedman MJ, Attia MW (2004) Clinical predictors of influenza in children. Arch Pediat Adol Med 158:391–394
Ohmit SE, Monto AS (2006) Symptomatic predictors of influenza virus positivity in children during the influenza season. Clin Infect Dis 43:564–568
Sočan M, Prosenc K, Nagode M (2010) Differences in clinical predictors of influenza in adults and children with influenza-like illness. Cent Eur J Med 5:41–48
Heikkinen T (2006) Influenza in children. Acta Paediatr 95:778–784
Silvennoinen H, Peltola V, Lehtinen P et al (2009) Clinical presentation of influenza in unselected children treated as outpatients. Pediatr Infect Dis J 28:372–375
Heikkinen T, Marttila J, Salmi AA et al (2002) Nasal swab versus nasopharyngeal aspirate for isolation of respiratory viruses. J Clin Microbiol 40:4337–4339
Waris M, Ziegler T, Kivivirta M et al (1990) Rapid detection of respiratory syncytial virus and influenza A virus in cell cultures by immunoperoxidase staining with monoclonal antibodies. J Clin Microbiol 28:1159–1162
Hayden SR, Brown MD (1999) Likelihood ratio: a powerful tool for incorporating the results of a diagnostic test into clinical decisionmaking. Ann Emerg Med 33:575–580
Andrasik F, Powers SW, McGrath PJ (2005) Methodological considerations in research with special populations: children and adolescents. Headache 45:520–525
Heinonen S, Silvennoinen H, Lehtinen P et al (2011) Feasibility of diagnosing influenza within 24 hours of symptom onset in children 1–3 years of age. Eur J Clin Microbiol Infect Dis 30:387–392
Grijalva CG, Poehling KA, Edwards KM et al (2007) Accuracy and interpretation of rapid influenza tests in children. Pediatrics 119:e6–e11
Uyeki TM, Prasad R, Vukotich C et al (2009) Low sensitivity of rapid diagnostic test for influenza. Clin Infect Dis 48:e89–e92
Steininger C, Redlberger M, Graninger W et al (2009) Near-patient assays for diagnosis of influenza virus infection in adult patients. Clin Microbiol Infect 15:267–273
Stripeli F, Sakkou Z, Papadopoulos N et al (2010) Performance of rapid influenza testing in hospitalized children. Eur J Clin Microbiol Infect Dis 29:683–688
Acknowledgment
Supported by: Turku University Hospital Foundation; Foundation for Paediatric Research, Finland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Heinonen, S., Peltola, V., Silvennoinen, H. et al. Signs and symptoms predicting influenza in children: a matched case–control analysis of prospectively collected clinical data. Eur J Clin Microbiol Infect Dis 31, 1569–1574 (2012). https://doi.org/10.1007/s10096-011-1479-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-011-1479-4