Abstract
Background
The incidence of lumbar spinal stenosis (LSS) continues to rise, with both conservative and surgical management representing options for its treatment. The timing of surgery for LSS varies from shortly after the onset of symptoms to several months or years after conservative treatment. The aim of this study was to investigate the association between the duration of pre-operative conservative treatment and the ultimate outcome following surgical interventions for LSS.
Methods
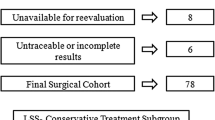
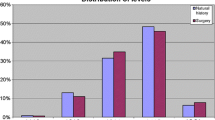
The study was based on prospective multicentre registry data (Spine Tango). Cases of LSS with a documented duration of conservative treatment, undergoing spinal decompression with at least one post-operative patient assessment between 3 and 30 months, were included in the study. Cases of LSS with spondylolisthesis, additional spinal pathology or previous spinal surgery were excluded. Interrogation of the Spine Tango Registry listed 3478 patients meeting the prescribed inclusion criteria. This cohort was stratified into four groups: (1) no previous treatment (n = 497; 14.3%), (2) conservative treatment <6 months (n = 965; 27.8%), (3) conservative treatment between 6 and 12 months (n = 758; 21.8%), and (4) conservative treatment >12 months (n = 1258; 36.1%). Group 4 reference group in regression analysis. The inverse probability of treatment weighting (IPTW) was applied using the propensity score to balance the groups for their characteristics. Outcome measures included achievement of the minimum clinically important change (MCIC) score of 2 points for (a) back pain, (b) leg pain and (c) Core Outcome Measures Index (COMI), and (d) surgical complications, (e) general complications and (f) operation time >2 h.
Results
Patient group (“duration of conservative therapy”) was not associated with achievement of the MCIC for post-operative relief of leg pain (p = 0.22), achievement of MCIC for the COMI score (p = 0.054), surgical complications (p = 0.11) or general complications (p = 0.14). Only MCIC for post-operative relief of back pain (p = 0.021) and operation time were significantly associated with patient group (p = 0.038). However, compared with the reference group of >12 months of conservative treatment there was no significant difference in the likelihood of achieving the MCIC for those with none, <6 or 6–12 months of conservative treatment.
Conclusions
The duration of pre-operative conservative treatment was not associated with the ultimate outcome of decompression surgery. Further research is required to investigate optimal thresholds/indications for surgery and its appropriate timing in individual patients.


Similar content being viewed by others
References
Sobottke R, Herren C, Siewe J, Mannion AF, Roder C, Aghayev E (2015) Predictors of improvement in quality of life and pain relief in lumbar spinal stenosis relative to patient age: a study based on the Spine Tango Registry. Eur Spine J. doi:10.1007/s00586-015-4078-8
Joaquim AF, Sansur CA, Hamilton DK, Shaffrey CI (2009) Degenerative lumbar stenosis: update. Arq Neuropsiquiatr 67:553–558
Benoist M (2002) The natural history of lumbar degenerative spinal stenosis. Joint Bone Spine 69:450–457
Kalff R, Ewald C, Waschke A, Gobisch L, Hopf C (2013) Degenerative lumbar spinal stenosis in older people: current treatment options. Deutsch Arztebl Int 110:613–623. doi:10.3238/arztebl.2013.0613 (quiz 624)
Katz JN, Losina E (2008) Cost-effectiveness of spine surgery: the jury is out. Ann Intern Med 149:901–903
Sobottke R, Aghayev E, Roder C, Eysel P, Delank SK, Zweig T (2012) Predictors of surgical, general and follow-up complications in lumbar spinal stenosis relative to patient age as emerged from the Spine Tango Registry. Eur Spine J 21:411–417. doi:10.1007/s00586-011-2016-y
Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE (2005) Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the maine lumbar spine study. Spine 30:936–943
Malmivaara A, Slatis P, Heliovaara M, Sainio P, Kinnunen H, Kankare J, Dalin-Hirvonen N, Seitsalo S, Herno A, Kortekangas P, Niinimaki T, Ronty H, Tallroth K, Turunen V, Knekt P, Harkanen T, Hurri H, Finnish Lumbar Spinal Research G (2007) Surgical or nonoperative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine 32:1–8. doi:10.1097/01.brs.0000251014.81875.6d
Amundsen T, Weber H, Nordal HJ, Magnaes B, Abdelnoor M, Lilleas F (2000) Lumbar spinal stenosis: conservative or surgical management?: a prospective 10-year study. Spine 25:1424–1435 (discussion 1435–1426)
Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Blood E, Hanscom B, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H, Investigators S (2008) Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 358:794–810. doi:10.1056/NEJMoa0707136
Fritsch CG, Ferreira ML, Maher CG, Herbert RD, Pinto RZ, Koes B, Ferreira PH (2016) The clinical course of pain and disability following surgery for spinal stenosis: a systematic review and meta-analysis of cohort studies. Eur Spine J. doi:10.1007/s00586-016-4668-0
Radcliff KE, Rihn J, Hilibrand A, DiIorio T, Tosteson T, Lurie JD, Zhao W, Vaccaro AR, Albert TJ, Weinstein JN (2011) Does the duration of symptoms in patients with spinal stenosis and degenerative spondylolisthesis affect outcomes?: analysis of the Spine Outcomes Research Trial. Spine 36:2197–2210. doi:10.1097/BRS.0b013e3182341edf
Weinstein JN, Lurie JD, Tosteson TD, Zhao W, Blood EA, Tosteson AN, Birkmeyer N, Herkowitz H, Longley M, Lenke L, Emery S, Hu SS (2009) Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Jt Surg Am 91:1295–1304. doi:10.2106/JBJS.H.00913
Staub LP, Ryser C, Roder C, Mannion AF, Jarvik JG, Aebi M, Aghayev E (2016) Total disc arthroplasty versus anterior cervical interbody fusion: use of the Spine Tango registry to supplement the evidence from randomized control trials. Spine J 16:136–145. doi:10.1016/j.spinee.2015.11.056
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ 85:867–872
Melloh M, Staub L, Aghayev E, Zweig T, Barz T, Theis JC, Chavanne A, Grob D, Aebi M, Roeder C (2008) The international spine registry SPINE TANGO: status quo and first results. Eur Spine J 17:1201–1209. doi:10.1007/s00586-008-0665-2
Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Semmer NK, Jacobshagen N, Dvorak J, Boos N (2005) Outcome assessment in low back pain: how low can you go? Eur Spine J 14:1014–1026. doi:10.1007/s00586-005-0911-9
Mannion AF, Porchet F, Kleinstuck FS, Lattig F, Jeszenszky D, Bartanusz V, Dvorak J, Grob D (2009) The quality of spine surgery from the patient’s perspective. Part 1: the Core Outcome Measures Index in clinical practice. Eur Spine J 18(Suppl 3):367–373. doi:10.1007/s00586-009-0942-8
Monticone M, Ferrante S, Maggioni S, Grenat G, Checchia GA, Testa M, Teli MG, Mannion AF (2014) Reliability, validity and responsiveness of the cross-culturally adapted Italian version of the core outcome measures index (COMI) for the neck. Eur Spine J 23:863–872. doi:10.1007/s00586-013-3092-y
Genevay S, Cedraschi C, Marty M, Rozenberg S, De Goumoens P, Faundez A, Balague F, Porchet F, Mannion AF (2012) Reliability and validity of the cross-culturally adapted French version of the Core Outcome Measures Index (COMI) in patients with low back pain. Eur Spine J 21:130–137. doi:10.1007/s00586-011-1992-2
Ferrer M, Pellise F, Escudero O, Alvarez L, Pont A, Alonso J, Deyo R (2006) Validation of a minimum outcome core set in the evaluation of patients with back pain. Spine 31:1372–1379. doi:10.1097/01.brs.0000218477.53318.bc (discussion 1380)
Storheim K, Brox JI, Lochting I, Werner EL, Grotle M (2012) Cross-cultural adaptation and validation of the Norwegian version of the Core Outcome Measures Index for low back pain. Eur Spine J 21:2539–2549. doi:10.1007/s00586-012-2393-x
Damasceno LH, Rocha PA, Barbosa ES, Barros CA, Canto FT, Defino HL, Mannion AF (2012) Cross-cultural adaptation and assessment of the reliability and validity of the Core Outcome Measures Index (COMI) for the Brazilian-Portuguese language. Eur Spine J 21:1273–1282. doi:10.1007/s00586-011-2100-3
Qiao J, Zhu F, Zhu Z, Xu L, Wang B, Yu Y, Qian BP, Ding Y, Qiu Y (2013) Validation of the simplified Chinese version of the Core Outcome Measures Index (COMI). Eur Spine J 22:2821–2826. doi:10.1007/s00586-013-2761-1
Miekisiak G, Kollataj M, Dobrogowski J, Kloc W, Libionka W, Banach M, Latka D, Sobolewski T, Sulewski A, Nowakowski A, Kiwic G, Pala A, Potaczek T (2013) Cross-cultural adaptation and validation of the Polish version of the core outcome measures index for low back pain. Eur Spine J 22:995–1001. doi:10.1007/s00586-012-2607-2
Klemencsics I, Lazary A, Valasek T, Szoverfi Z, Bozsodi A, Eltes P, Fekete TF, Varga PP (2016) Cross-cultural adaptation and validation of the Hungarian version of the Core Outcome Measures Index for the back (COMI Back). Eur Spine J 25:257–264. doi:10.1007/s00586-014-3750-8
Definitions of the degenerativ diagnosis groups. EUROSPINE, Spine Tango committee. http://www.eurospine.org/cm_data/def_of_degen_patho.pdf. August 2016
Citrome L (2008) Compelling or irrelevant? Using number needed to treat can help decide. Acta Psychiatr Scand 117:412–419. doi:10.1111/j.1600-0447.2008.01194.x
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 46:399–424. doi:10.1080/00273171.2011.568786
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Zweig, T., Enke, J., Mannion, A.F. et al. Is the duration of pre-operative conservative treatment associated with the clinical outcome following surgical decompression for lumbar spinal stenosis? A study based on the Spine Tango Registry. Eur Spine J 26, 488–500 (2017). https://doi.org/10.1007/s00586-016-4882-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4882-9