Abstract
Objectives
In the latest World Health Organization classification 2021, grade 4 adult diffuse gliomas can be diagnosed with several molecular features even without histological evidence of necrosis or microvascular proliferation. We aimed to explore whole tumor histogram-derived apparent diffusion coefficient (ADC) histogram profiles for differentiating between the presence (Mol-4) and absence (Mol-2/3) of grade 4 molecular features in histologically lower-grade gliomas.
Methods
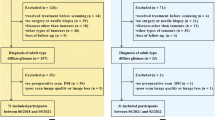
Between June 2019 and October 2022, 184 adult patients with diffuse gliomas underwent MRI. After excluding 121 patients, 18 (median age, 64.5 [range, 37–84 years]) Mol-4 and 45 (median 40 [range, 18–73] years) Mol-2/3 patients with histologically lower-grade gliomas were enrolled. Whole tumor volume-of-interest-derived ADC histogram profiles were calculated and compared between the two groups. Stepwise logistic regression analysis with Akaike’s information criterion using the ADC histogram profiles with p values < 0.01 and age at diagnosis was used to identify independent variables for predicting the Mol-4 group.
Results
The 90th percentile (p < 0.001), median (p < 0.001), mean (p < 0.001), 10th percentile (p = 0.014), and entropy (p < 0.001) of normalized ADC were lower, and kurtosis (p < 0.001) and skewness (p = 0.046) were higher in the Mol-4 group than in the Mol-2/3 group. Multivariate logistic regression analysis revealed that the entropy of normalized ADC and age at diagnosis were independent predictive parameters for the Mol-4 group with an area under the curve of 0.92.
Conclusion
ADC histogram profiles may be promising preoperative imaging biomarkers to predict molecular grade 4 among histologically lower-grade adult diffuse gliomas.
Clinical relevance statement
This study highlighted the diagnostic usefulness of ADC histogram profiles to differentiate histologically lower grade adult diffuse gliomas with the presence of molecular grade 4 features and those without.
Key Points
• ADC histogram profiles to predict molecular CNS WHO grade 4 status among histologically lower-grade adult diffuse gliomas were evaluated.
• Entropy of ADC and age were independent predictive parameters for molecular grade 4 status.
• ADC histogram analysis is useful for predicting molecular grade 4 among histologically lower-grade gliomas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gliomas are the most frequent primary brain tumors in adults with an overall age-adjusted population incidence rate of 4.67–5.73 per 100,000, without remarkable change over the past two decades [1, 2]. Adult diffuse gliomas are graded as CNS WHO grades 2, 3, or 4 according to the degree of malignancy; the higher the grade, the more malignant, and the poorer the prognosis. The primary treatment for IDH-mutant grade 2 and 3 diffuse gliomas is maximal safe resection followed by active surveillance, or radiation followed by procarbazine, lomustine, and vincristine, while radiation with adjuvant temozolomide is often used in the treatment of IDH-mutant astrocytoma, grade 4 and IDH-wildtype glioblastomas (grade 4) [3]. Despite the development of therapeutics, the prognosis for grade 4 gliomas remains unfavorable. The reported median survival of grades 2, 3, and 4 gliomas are approximately 5–17 years, 2–8 years, and <1 year, respectively [1].
Recent advances in molecular genetics have allowed for a more concise definition of CNS tumors based on molecular genetic features. The diagnostic criteria for adult diffuse gliomas now rely on the presence or absence of an isocitrate dehydrogenase (IDH) gene mutation and 1p/19q codeletion, which were adopted in the 2016 edition of WHO classification [4], with the addition of several updates in the latest WHO classification in 2021 (WHO CNS5) [5]. For example, a diagnosis of IDH-wildtype grade 4 diffuse glioma (glioblastoma) includes 3 new molecular genetic criteria: concurrent gain of the whole chromosome 7 and loss of the whole chromosome 10 (+7/−10), telomerase reverse transcriptase (TERT) promoter mutation, and epidermal growth factor receptor (EGFR) amplification. Meanwhile, oligodendrogliomas are classified only into grade 2 or 3 [6]. Due to its rarity, an IDH-wildtype lower-grade (grade 2 or 3) astrocytoma is no longer regarded as a distinct tumor type in WHO CNS5 [6].
Due to these recent revisions and reclassifications of WHO criteria, a diagnosis of grade 4 adult diffuse gliomas should be made even if there is no histological evidence of necrosis or microvascular proliferation. The presence of grade 4 diffuse glioma among tumors diagnosed as lower-grade glioma in previous criteria evokes a challenging problem in radiological diagnosis. Traditionally, a rim-enhancing mass with central necrosis has been considered a typical appearance for grade 4 diffuse glioma, including IDH-wildtype glioblastomas and grade 4 IDH-mutant astrocytomas [7, 8]. However, even tumors without imaging evidence of necrosis could be diagnosed as grade 4 diffuse gliomas according to WHO CNS5 [5].
Despite the difficulty of imaging diagnosis, it is meaningful to diagnose these “molecular” grade 4 diffuse gliomas because these updates are based on advances in molecular genetic findings that revealed histologically lower-grade gliomas with these molecular abnormalities have a prognosis similar to those of histological grade 4 diffuse gliomas [9,10,11]. Moreover, these molecular genetic features are potential targets for molecularly targeted therapies currently under development, although the results have not yet been satisfactory [12, 13]. Therefore, imaging biomarkers on preoperative MRI for predicting molecular grade 4 diffuse glioma have been warranted to formulate a treatment strategy. Significant efforts have been made to differentiate grade 4 and lower-grade diffuse gliomas, and DWI has provided useful imaging biomarkers including ADC [1 and Fig. 2, respectively.
An 84-year-old man with IDH-wildtype histologically lower-grade astrocytic glioma with molecular evidence of CNS WHO grade 4 (concurrent gain of the whole chromosome 7 and loss of the whole chromosome 10 and TERT promoter mutation). The tumor shows hyperintensity on the fluid-attenuated inversion recovery image (a), and the median and entropy of the normalized apparent diffusion coefficient are 1.28 and 6.19, respectively (b). No evidence of necrosis or contrast enhancement is found on the subtraction T1-weighted image (c)
A 26-year-old woman with IDH-mutant histologically lower-grade astrocytoma without homozygous deletions of CDKN2A/B. The tumor shows hyperintensity on the fluid-attenuated inversion recovery image (a), and the median and entropy of the normalized apparent diffusion coefficient are 2.37 and 6.89, respectively (b). No evidence of necrosis or contrast enhancement is found on the subtraction T1-weighted image (c)
Subclass analyses between the Mol-4 and Mol-2/3 astrocytomas
The demographic and pathological findings and the results of ADC histogram analyses are summarized in Supplementary Tables 1 and 2, respectively. Age at diagnosis was significantly higher, and the rate of IDH-mutant tumors was significantly lower in the Mol-4 astrocytomas compared with the Mol-2/3 counterparts (median 64.5 [range, 37–84] years vs. 33 [18–60] years, p < 0.001; IDH-mutant vs. IDH-wildtype: 1:17 vs. 24:3, p < 0.001). The age at diagnosis and median of ADC were selected for the stepwise multivariate logistic regression analysis, and the AUC of the model was 0.98 (0.94–1) (Supplementary Table 3). The mean precision, recall, and F1 score using LOOCV and 1000-bootstrap** (mean (95%CI)) were 0.86 (0.86–0.87), 0.85 (0.85–0.86), and 0.86 (0.85–0.86), respectively. Although the median of ADC tended to be lower in the Mol-4 astrocytomas, the p-value did not reach statistical significance.
Discussion
In this study, we compared ADC histogram profiles in histologically lower-grade adult diffuse gliomas between the presence (the Mol-4 group) and absence (the Mol-2/3 group) of molecular evidence for CNS WHO grade 4 in accordance with WHO CNS5. Many ADC histogram profiles were significantly different between the two groups, and the entropy of normalized ADC and age at diagnoses were found as independent predictive factors for the Mol-4 group with an AUC of 0.92. On the other hand, while several ADC histogram profiles were significantly different between the groups, only age at diagnosis was the independent predictive factor for the Mol-4 astrocytoma group in the comparison between the Mol-4 and Mol-2/3 astrocytomas.
In the present study, we found that 1st-order ADC histogram profiles (i.e., maximum, 90th percentile, median, mean, and 10th percentile) were significantly lower in the Mol-4 group than in the Mol-2/3 group. These results were similar to the results of the subclass analyses of astrocytomas. Traditionally, a lower ADC has been considered to be associated with increased cellularity [26]. Furthermore, many studies have reported that lower ADC is a negative prognostic biomarker in gliomas independent of the grade. In the meta-analysis of studies published between 2006 and 2010, Zulfigar et al. [27] demonstrated that a low minimum ADC was associated with a shorter survival rate in patients with grades III and IV diffuse glioma when cases were stratified according to the grades. Cuccarini et al. [28] reported that a low minimum ADC was associated with a shorter overall survival in patients with grades II and III diffuse glioma when cases were stratified according to the grades. Hilario et al. [29] found that older age and a low median ADC were associated with shorter overall survival independent of tumor grade in their study including patients with grades II, III, and IV diffuse gliomas. Despite the consistency of the results, it should be noted that diffuse gliomas in these studies were diagnosed according to the previous WHO classifications without the latest molecular updates; thus, histologically lower-grade molecular grade 4 diffuse gliomas (i.e., the Mol-4 group) were likely included in their grades II or III diffuse glioma groups [26,27,28,29]. Therefore, the variations in ADC and prognosis among the “same” grade diffuse gliomas in these studies may have been affected, at least in part, by the differences in the presence or absence of the molecular features of grade 4, as shown in the present study.
The multivariate stepwise logistic regression analysis revealed that age at diagnosis and the entropy of normalized ADC were independent parameters for predicting the Mol-4 group. The second-order parameters derived from the whole tumor ADC histograms, namely kurtosis, skewness, and entropy, have been evaluated for tumor grading and for estimating the proliferative potential of the tumors [30,31,32]. Kurtosis represents the distribution peakedness of the intensity for the parameter within the tissue. Skewness represents the distribution asymmetry. Entropy represents the intensity predictability of the parameter and reflects textural variation. Differences in the entropy of normalized ADC in the present study may have reflected the difference in microstructural heterogeneity between the two groups. Although the p-value of the entropy of ADC did not reach statistical significance and only age at diagnosis was an independent predictive factor for the Mol-4 astrocytoma group in the subclass analysis without oligodendrogliomas, the entropy of ADC was also selected in the stepwise selection. The higher patient age in the Mol-4 group compared with the Mol-2/3 group was in line with the study by Reuss et al. [33], although they did not compare the patient age statistically. Further studies with a larger number of cases are warranted to verify these results.
While ADC histogram profiles were shown to be promising imaging biomarkers in differentiating Mol-4 group from Mol-2/3 group, we could not verify the difference in the frequency of the gyriform infiltration on FLAIR imaging between the two groups. The gyriform infiltration was reported to be present in 16/31 patients (51.6%) in the Mol-4 group and 0/151 patients (0%) in the Mol-2/3 group with a statistically significant difference in the frequency by a French group [18]. The discrepancy between the results of their study and the present study should be further investigated by another group since other than one study by the same French group with the patients from the same institution [34] and the present study, no study has examined the frequency of the gyriform infiltration in the Mol-4 group. It should be noted that although all of their Mol-4 group tumors corresponded to lower-grade IDH-wildtype astrocytomas in the previous WHO 2016 classification [18], the high frequency of gyriform infiltration in lower-grade IDH-wildtype astrocytomas has not been reported from other groups.
We recognize several limitations in the present study. First, this was a single institutional retrospective study, which limited the number of patients. Second, MRI examinations were performed using multiple scanners at different field strengths. However, to minimize the influence of the machine differences, we normalized ADC parameters. Further, ADC is theoretically insensitive to the difference in field strength, even though a higher field strength may benefit from a higher contrast-to-noise ratio [35]. Third, most of the Mol-4 group consisted of IDH-wildtype diffuse gliomas in the present study. However, this reflects the real-world frequency because we included consecutive patients, and the similar frequency of IDH-wildtype diffuse gliomas has been reported in other studies [18, 33]. Finally, we could not evaluate the correlation between histogram profiles and patient survival. The association with prognosis needs to be investigated in future studies.
Conclusion
Whole tumor histogram-derived ADC profiles may be promising imaging biomarkers on preoperative brain MRI with significant differences between the presence and absence of molecular features for grade 4 in histologically lower-grade adult diffuse gliomas.
Abbreviations
- +7/-10:
-
Concurrent gain of the whole chromosome 7 and loss of the whole chromosome 10
- AUC:
-
Area under the receiver operating characteristic curve
- EGFR:
-
Epidermal growth factor receptor
- FDR:
-
False discovery rate
- IDH:
-
Isocitrate dehydrogenase
- TERT:
-
Telomerase reverse transcriptase
References
Ostrom QT, Cioffi G, Waite K et al (2021) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2014–2018. Neuro Oncol 23:iii1–iii105
Ostrom QT, Bauchet L, Davis FG et al (2014) The epidemiology of glioma in adults: a “state of the science” review. Neuro Oncol 16:896–913
Weller M, van den Bent M, Preusser M et al (2021) EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat Rev Clin Oncol 18:170–186
Louis DN, Perry A, Reifenberger G et al (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820
Louis DN, Perry A, Wesseling P et al (2021) The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol 23:1231–1251
Gritsch S, Batchelor TT, Nicolas Gonzalez Castro L (2022) Diagnostic, therapeutic, and prognostic implications of the 2021 World Health Organization classification of tumors of the central nervous system. Cancer 128:47–58
Roux A, Tran S, Edjlali M et al (2021) Prognostic relevance of adding MRI data to WHO 2016 and cIMPACT-NOW updates for diffuse astrocytic tumors in adults. Working toward the extended use of MRI data in integrated glioma diagnosis. Brain Pathol 31:e12929
Nelson SJ, Cha S (2003) Imaging glioblastoma multiforme. Cancer J 9:134–145
Brat DJ, Aldape K, Colman H et al (2018) cIMPACT-NOW update 3: recommended diagnostic criteria for “Diffuse astrocytic glioma, IDH-wildtype, with molecular features of glioblastoma, WHO grade IV.” Acta Neuropathol 136:805–810
Brat DJ, Aldape K, Colman H et al (2020) cIMPACT-NOW update 5: recommended grading criteria and terminologies for IDH-mutant astrocytomas. Acta Neuropathol 139:603–608
Shirahata M, Ono T, Stichel D et al (2018) Novel, improved grading system(s) for IDH-mutant astrocytic gliomas. Acta Neuropathol 136:153–166
Rezaei V, Rabiee A, Khademi F (2020) Glioblastoma multiforme: a glance at advanced therapies based on nanotechnology. J Chemother 32:107–117
Yang K, Wu Z, Zhang H et al (2022) Glioma targeted therapy: insight into future of molecular approaches. Mol Cancer 21:39
**e Y, Li S, Shen N et al (2021) Assessment of isocitrate dehydrogenase 1 genotype and cell proliferation in gliomas using multiple diffusion magnetic resonance imaging. Front Neurosci 15:783361
Gezer B, Mutlukan A, Sahinoglu M et al (2020) Comparison of immunogenetic properties of glial tumors with advanced magnetic resonance imaging findings. Turk Neurosurg 30:422–427
Liu T, Cheng G, Kang X et al (2018) Noninvasively evaluating the grading and IDH1 mutation status of diffuse gliomas by three-dimensional pseudo-continuous arterial spin labeling and diffusion-weighted imaging. Neuroradiology 60:693–702
Leu K, Ott GA, Lai A et al (2017) Perfusion and diffusion MRI signatures in histologic and genetic subtypes of WHO grade II-III diffuse gliomas. J Neurooncol 134:177–188
Mesny E, Barritault M, Izquierdo C et al (2022) Gyriform infiltration as imaging biomarker for molecular glioblastomas. J Neurooncol 157:511–521
Cho NS, Hagiwara A, Sanvito F, Ellingson BM (2022) A multi-reader comparison of normal appearing white matter normalization techniques for perfusion and diffusion MRI in brain tumors. Neuroradiology
Hagiwara A, Oughourlian TC, Cho NS et al (2022) Diffusion MRI is an early biomarker of overall survival benefit in IDH wild-type recurrent glioblastoma treated with immune checkpoint inhibitors. Neuro Oncol 24:1020–1028
Ellingson BM, Kim HJ, Woodworth DC et al (2014) Recurrent glioblastoma treated with bevacizumab: contrast-enhanced T1-weighted subtraction maps improve tumor delineation and aid prediction of survival in a multicenter clinical trial. Radiology 271:200–210
Hagiwara A, Yao J, Raymond C et al (2021) “Aerobic glycolytic imaging” of human gliomas using combined pH-, oxygen-, and perfusion-weighted magnetic resonance imaging. Neuroimage Clin 32:102882
Chowdhury MZI, Turin TC (2020) Variable selection strategies and its importance in clinical prediction modelling. Fam Med Community Health 8:e000262
Yan L-F, Sun Y-Z, Zhao S-S et al (2019) Perfusion, diffusion, or brain tumor barrier integrity: which represents the glioma features best? Cancer Manag Res 11:9989–10000
Hagiwara A, Tatekawa H, Yao J et al (2022) Visualization of tumor heterogeneity and prediction of isocitrate dehydrogenase mutation status for human gliomas using multiparametric physiologic and metabolic MRI. Sci Rep 12:1078
Sugahara T, Korogi Y, Kochi M et al (1999) Usefulness of diffusion-weighted MRI with echo-planar technique in the evaluation of cellularity in gliomas. J Magn Reson Imaging 9:53–60
Zulfiqar M, Yousem DM, Lai H (2013) ADC values and prognosis of malignant astrocytomas: does lower ADC predict a worse prognosis independent of grade of tumor?–a meta-analysis. AJR Am J Roentgenol 200:624–629
Cuccarini V, Erbetta A, Farinotti M et al (2016) Advanced MRI may complement histological diagnosis of lower grade gliomas and help in predicting survival. J Neurooncol 126:279–288
Hilario A, Sepulveda JM, Perez-Nuñez A et al (2014) A prognostic model based on preoperative MRI predicts overall survival in patients with diffuse gliomas. AJNR Am J Neuroradiol 35:1096–1102
Gihr G, Horvath-Rizea D, Hekeler E et al (2021) Diffusion weighted imaging in high-grade gliomas: A histogram-based analysis of apparent diffusion coefficient profile. PLoS One 16:e0249878
Han X, Suo S, Sun Y et al (2017) Apparent diffusion coefficient measurement in glioma: Influence of region-of-interest determination methods on apparent diffusion coefficient values, interobserver variability, time efficiency, and diagnostic ability. J Magn Reson Imaging 45:722–730
Just N (2014) Improving tumour heterogeneity MRI assessment with histograms. Br J Cancer 111:2205–2213
Reuss DE, Kratz A, Sahm F et al (2015) Adult IDH wild type astrocytomas biologically and clinically resolve into other tumor entities. Acta Neuropathol 130:407–417
Izquierdo C, Barritault M, Poncet D et al (2019) Radiological characteristics and natural history of adult IDH-wildtype astrocytomas with TERT promoter mutations. Neurosurgery 85:E448–E456
Hagiwara A, Fujita S, Ohno Y, Aoki S (2020) Variability and standardization of quantitative imaging: monoparametric to multiparametric quantification, radiomics, and artificial intelligence. Invest Radiol 55:601–616
Funding
Open access funding provided by The University of Tokyo. The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Toshio Moritani.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
We obtained our institutional review board exemption for including cases from University of Michigan.
Study subjects or cohorts overlap
No study subjects or cohorts have been previously reported.
Methodology
• retrospective
• case-control study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kurokawa, R., Hagiwara, A., Kurokawa, M. et al. Diffusion histogram profiles predict molecular features of grade 4 in histologically lower-grade adult diffuse gliomas following WHO classification 2021. Eur Radiol 34, 1367–1375 (2024). https://doi.org/10.1007/s00330-023-10071-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10071-x