Abstract
The diagnosis of multiple myeloma requires detection of paraproteinemia and confirmation of monoclonal bone marrow infiltration, along with signs of end-organ damage. Despite the increasing prevalence, serum paraproteinemia is not routinely measured. We examined the relationship between alterations in routine hematological parameters and the development of paraproteinemia in a case-control study. Data was retrieved from a laboratory database in the capital region of Denmark between 01/01/2012 and 31/12/2022. Patients were included if they had a test for paraproteinemia (n = 134,740) and at least one prior hematological parameter (white blood cells, hemoglobin and platelet count) with a minimum follow-up of 1 year.
Between 96,999 and 103,590 patients were included in each of the three hematological groups. We found white blood cell count and the presence of paraproteinemia followed an inverse J-shaped curve, with the highest presence below 3 × 109/L and above > 9 × 109/L. The adjusted OR below and above the nadir of 4 × 109/L was 1.61 (95% CI 1.25; 2.08, p < 0.0001) and 1.03 (95% CI 1.03; 1.04, p < 0.0001). Hemoglobin levels were inversely associated the presence of paraproteinemia, with the highest association below 6 mmol/L with an OR of 1.30 (95% CI 1.28; 1.32, p < 0.0001) adjusted for age and gender. Platelet count followed a U-shaped curve with the highest association at < 100 × 109/L. The adjusted OR below and above the nadir of 250 × 109/L was 1.13 (95% CI 1.10; 1.17, p < 0.0001) and 1.10 (95% CI 1.08; 1.12, p < 0.0001) respectively. In conclusion, all three parameters showed significant association with later paraproteinemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple Myeloma (MM) is a malignant hematological cancer characterized by abnormal plasma cell proliferation in the bone marrow [1]. The global incidence of MM is rising with a current incidence of 2.1/100,000 and 1.4/100,000 for men and women respectively, and even higher regional incidences in Australia, Western Europe and United States of America [2]. In total, MM constitutes 10% of all hematological malignancies and 1% of all cancers [3, 4]. The diagnosis of overt MM requires the presence of ≥ 10% clonal plasma cells in the bone marrow and the development of at least one myeloma defining event, such as CRAB criteria (calcium elevation, renal insufficiency, anemia, bone disease) or one or more myeloma-defining biomarkers: ≥60% clonal plasma cells in the bone marrow, a serum light free chain (FLC) ratio of ≥ 100 in combination with a concentration of FLC above 10 mg/dL or > 1 focal lesions (> 5 mm) on MRI [5, 6].
MM is typically preceded by one or both of its two asymptomatic precursor conditions: Monoclonal Gammopathy of Undetermined Significance (MGUS) or Smoldering Multiple Myeloma (SMM) [7]. The defining diagnostic criteria between MGUS and SMM is based on the concentration of serum paraprotein and monoclonal plasma cells in the bone marrow; MGUS is characterized by less than 10% monoclonal plasma cells in the bone marrow, while more than 10% are present in SMM [7, 8]. MGUS prevalence is up to 5.3% in the general population over 70 years old [9], and presents a constant annual risk of progression to MM of 1%, which increases to a cumulative 10% in SMM [5, 8, 10].
Despite MM being a life-threatening condition with a 5 year survival of 53.9% in the US and 62.4% in Germany, the prognosis and overall survival have improved remarkably over the last decades [2, 11]. Importantly, early detection of premalignant gammopathies has been correlated with increased overall survival in MM through increased monitoring and timely treatment [12, 13]. Nonetheless, current MGUS and SMM diagnosis remain incidental and specific paraprotein measures are not routinely conducted as part of the standard of care hematological investigations. In order to accurately predict survival and prognosis of various cancer types, the Hemoglobin, Albumin, Lymphocytes and Platelets Score (HALP) has been effectively used [14]. In MM, the HALP score has been proven as a prognostic marker for overall and progression-free survival in MM [4], but the association between routinely measured serum biomarkers and premalignant gammopathies remains unknown. Therefore, the aim of this retrospective case-control study is to examine the relationship between alterations in blood hemoglobin, white blood cell and platelet count, and the development of paraproteinemia.
Methods
Patient population and data collection
This study includes data from patients who had a diagnostic blood sample taken for potential monoclonal gammopathies, identified using the NPU17675 code for Plasma M protein, the NPU19606 code for Kappa light chain monoclonal gammopathy or the NPU19607 code for Lambda light chain monoclonal gammopathy, between 01/01/2012 and 31/12/2022. Patients were referred to the analysis according to national guidelines [15]. Inclusion criteria also required data availability for prior hematological parameters, including hemoglobin, white blood cells and/or platelet count. The data was extracted from LAKBA II, a database containing blood test results from patients in hospitals and general practices in the Capital Region of Denmark.
Only patients with a minimum follow-up of 1 year between hematological parameters and M protein/free light chain testing were included. If a patient had multiple hematological assessments during the 11-year study period, their mean was used in the further analyses. If a patient had a positive M protein or free light chain test result, this result was used in the analyses. Otherwise, if multiple negative test results were present, only the first was included in this study.
A total of 134,740 patients who had a test for monoclonal gammopathy were identified. In this group, 133,792 patients also had hemoglobin values available. Likewise, 133,612 patients had available white blood cell data, and 133,303 had platelet count data. Patients with a test for monoclonal gammopathy taken before the respective hematological parameters were excluded. Further information can be found in the supplementary Figs. 1–3.
Measurements of hematological parameters, M protein and free light chains
The analysis of the hemoglobin, white blood cell and platelet count was performed by all laboratories located in the capital region of Denmark. The analyses of M protein (NPU17675), Kappa light chain monoclonal gammopathies (NPU19606) and Lambda light chain monoclonal gammopathies (NPU19607) were performed by four specialized laboratories in the region. The majority of the M-protein samples, 94.4%, were analyzed by capillary electrophoresis using the Capillarys platform from Sebia (Lisses, France). The remaining 5.6% were analyzed using agarose gel electrophoresis. According to the national guideline [15], when the M-protein analysis (NPU17675) was negative, the samples were screened for light chain monoclonal gammopathies. In the included laboratories, this was performed on the Atellica platform from Siemens Healthineers (Erlangen, Germany), on the SPAPLUS platform from Binding Site or on the Optilite platform from Binding Site.
The test was considered positive for Kappa light chain monoclonal gammopathy at concentrations above 22.4 mg/L. For Lambda light chain monoclonal gammopathy, the cut-off used was 27.0 mg/L.
All included laboratories participated in external quality programs during the study period to confirm the reliability of the assays over time.
Statistical analyses
Differences between continuous variables were tested using unpaired t-tests or Mann Whitney U tests as appropriate while differences in the distribution of categorical variables were tested using Chi-square tests.
In order to investigate the shape of the association between the hematological parameters and the development of monoclonal gammopathy, we plotted rounded values of the mean concentration of white blood cells, hemoglobin and platelets on the x-axis versus the percentage of patients with monoclonal gammopathy on the Y-axis. For white blood cells and platelets, the association was approximately inverse J-shaped and U-shaped, respectively. The nadir of the two curves was therefore used to split the data into below and above this value for further analyses.
Unadjusted and adjusted for covariates (i.e. age and gender) proportional hazards regression analyses were used to investigate the relationship between monoclonal gammopathy and the three hematological parameters.
All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). For all the statistical analyses, p < 0.05 was considered statistically significant.
Ethics
The data from the laboratory information system was anonymized before analysis. In Denmark, no approval from the Ethics Committee is required for this type of register-based study.
Results
A total of 99,766 patients with an M protein/free light chain test result and at least one white blood cell count in the study period between 01/01/2012 and 31/12/2022 were included. Likewise, 103,590 with a hemoglobin sample and M protein/free light chain, and 96,999 patients with a platelet count and M protein/free light chain were included.
Table 1 shows the basic characteristics of the study population according to the hematological and monoclonal gammopathy status. In all the three groups with monoclonal gammopathy, the mean age at the time of the first hematological measurement was significantly higher, compared with the groups without monoclonal gammopathy. The follow-up period between the measurements of the hematological parameters and the M protein/free light chain test was significantly longer in all of the groups with monoclonal gammopathy. Concerning the gender distribution, paraproteinemia was more prevalent in males than females.
The association between white blood cell count and the presence of monoclonal gammopathy during the follow-up period is illustrated in Fig. 1. The curve is reversed J-shaped with increasing presence (up to 30%) of monoclonal gammopathy below a mean white blood cell count of 4 × 109/L and above a mean count of 12 × 109/L the presence of monoclonal gammopathy was 35%.
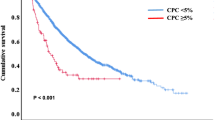
For hemoglobin, the presence of monoclonal gammopathy was inversely correlated with blood hemoglobin levels (Fig. 2). The presence of monoclonal gammopathy was highest (44%) at hemoglobin levels below 6 mmol/L, and decreased to a minimum of 26% correlating to hemoglobin levels between 8.5 and 10 mmol/L.
Lastly, the association between platelet count and the presence of monoclonal gammopathy followed a U-shape (Fig. 3), with the highest presence (> 40%) at platelet counts < 100 × 109/L. The presence of monoclonal gammopathy decreased with increasing platelet counts, with nadir at 250 × 109/L correlating to a presence of monoclonal gammopathy of 28%. After the nadir, the presence increased towards > 500 × 109/L.
The unadjusted Odds Ratios (OR) for the three hematological parameters as well as the ORs of each parameter adjusted for gender and age were also calculated (Table 2). The white blood cell count followed a reversed J-shaped curve, and therefore separate OR were calculated for each side of the nadir at 4 × 109/L. Below the nadir, the unadjusted OR was found to be 1.68 (95% CI 1.32; 2.14, p < 0.0001) and above the nadir the OR was 1.04 (95% CI 1.04; 1.05 p < 0.0001). When adjusted for age and gender, the ORs for the descending and ascending parts of the curve were 1.61 (95% CI 1.25; 2.08, p < 0.0001) and 1.03 (95% CI 1.03; 1.04, p < 0.0001), respectively. The relation between hemoglobin levels and the presence of monoclonal gammopathy showed a linearly descending curve, with an unadjusted OR of 1.25 (95% CI 1.24; 1.27, p < 0.0001). When adjusted for gender and age the OR was 1.30 (95% CI 1.28; 1.32, p < 0.0001). Finally, the OR for platelet count was calculated and as for the association between white blood cells and the presence of monoclonal gammopathy, the curve was split and two separate ORs were calculated as the curve followed a U-shape. The unadjusted OR of the descending part below the nadir of 250 × 109/L was 1.26 (95% CI 1.22; 1.29, p < 0.0001) and the unadjusted OR above the nadir was 1.10 (95% CI 1.09; 1.12, p < 0.0001). Similarly, the ORs for platelets were adjusted for gender and age, resulting in OR 1.13 (95% CI 1.10; 1.17, p < 0.0001) below the nadir and 1.10 (95% CI 1.08; 1.12, p < 0.0001) above.
Additionally, the white blood cell/platelet count ratio was estimated, but did not show greater predictive value compared to the three hematological parameters separately, and was therefore not included in further analyses (data not shown).
Discussion
MM remains an incurable disease, but early detection and monitoring of its premalignant precursors have been associated with greater overall survival due to timely treatment intervention [12]. In this retrospective case-control study, we found that the results of routine hematological parameters may warrant further evaluation of potential paraproteinemia utmost importance to improve early detection and diagnosis. The goal of this study was to evaluate the association between blood hemoglobin, platelet and white blood cell counts and serum paraproteinemia in retrospective Danish data collected between 2012 and 2022. Our study found a significant relationship between hematological parameters and the presence of monoclonal gammopathy. Male gender led to a significant increase in paraproteinemia OR compared to female gender, and age was found to increase OR in all the analyses.
The relationship between hematological parameters and the later development of MGUS or MM has previously been investigated by Li et al. [16]. In a case-control study, they examined the whole blood count of 21 MM patients and 21 healthy controls at time of enrollment in the study. They found a significant reduction in both hemoglobin, platelet count and white blood cell count in MM patients. This data is in line with our findings of increased risk for monoclonal gammopathy development at low hemoglobin levels and low platelet counts, and also a greater OR at low white blood cell count compared to higher levels.
An observational cohort-study of Danish patients without prior cancer diagnosis by Boennelykke et al. [17] sought to determine the effect of new-onset anemia on predicting a later cancer development within a follow-up of 12 months. The study found a significant relationship between all types of anemias and the incidence ratio of cancer, primarily of the gastrointestinal or respiratory systems. Among patients with unclassified anemia, hematological cancers had the highest standardized incidence ratio between both genders. The study further found that risk of cancer development increased continuously with age and also with the severity of anemia. This relationship between degree of anemia and risk of cancer development follows the same relationship as found between hemoglobin concentration and risk of monoclonal gammopathy in our study.
White blood cell count has been investigated in several studies as a prognostic biomarker for the development of various cancers. A study by Margolis et al. [18] investigated the incidence and mortality of breast, colorectal, endometrial and lung cancer in a prospective cohort with baseline measures of several hematological parameters collected at study initiation, including white blood cell counts. The outcomes were the incidence of cancer and cancer mortality. The study found that with increasing white blood cell count, the incidence of all four cancers also rose, suggesting a significant association between cancer development and systemic immunoreactivity. A study on the relationship between white blood cells and cancer incidence was conducted by Wong et al. [19], where data from patients in the UK biobank database was analyzed. The study found that increasing white blood cell count was associated with an increase in the incidence of lung cancer with an average follow-up of 7 years. While both of these studies showed a rising incidence in cancer development with increased white blood cell count, our study found a reversed J-shape relationship between white blood cell count and serum paraproteinemia. Importantly, both of the aforementioned studies used white blood cell data divided in quartiles, compared to our study in which white blood cell count was analyzed as a continuous variable, which may explain the differences across studies. Moreover, our study focused on patients with potential hematological cancer development, which may affect hematological parameters more acutely than solid cancers contained in organs compared to cancers in the bone marrow. Nonetheless rising white blood cell count has been shown to correlate to the development of several cancers.
Finally, the relationship between cancer incidence and platelet count has been examined in a study Jensvoll et al. [20]. The study examined the risk of develo** cancer and the risk of venous thromboembolisms in a Norwegian prospective population-study with cancer-free participants, and found no relation between platelet count and the risk of develo** cancer. This is in contrast with our results, where thrombocytes and monoclonal gammopathy presented an U-shape association.
Several studies have examined the importance of the combination of hemoglobin, lymphoctyte count, platelet count and albumin in the HALP score in relation to prognosis and severity of several cancers, including MM [4, 14, 21, 22]. The value of the HALP scores as a prognostic biomarker of MGUS or MM development has yet to be examined, but the data from our study showed that all three hematological parameters had a predictive value, and the addition of albumin and lymphocyte count to this might yield interesting results. Future studies will investigate whether the addition of albumin and lymphocyte data will clarify the prognostic value of HALP in the development of monoclonal gammopathies.
Strengths and weaknesses
An important limitation of our study is that the population only included patients who in their lifetime had a blood test taken for M protein/free light chains; all patients without this test were excluded. Serum paraprotein is tested on suspected development of MGUS or MM, and these patients typically present themselves with symptoms including fatigue, bone pain or anemia, amongst others [5]. Asymptomatic patients are therefore more unlikely to have a test for M protein/free light chains taken, and this large group of patients are missing from the dataset of this study. This could potentially result in selection bias of the study population. Sigurbergsdóttir et al. thus found that patients with a clinical diagnosis of MGUS have a higher mean number of comorbidities and are more likely to have been diagnosed with certain medical conditions compared to a screening population [23]. Furthermore, the prevalence of MM differs greatly between races and countries [2]. This information is not incorporated in the patient population of our study, and therefore it is not possible to take that into account in our statistical models. Additionally, given the long-term course of monoclonal gammopathies, it is possible that MGUS or even MM was already present at the time of blood test of the hematological parameters. This study only describes the biochemical status in the years prior to the positive M-protein/FLC test and cannot, therefore, specify the predictive value of the investigated parameters.
Our study was designed to analyze the association between routine hematological parameters and the later presence of paraproteinemia development a large population of Danish patients. We found that decreased hemoglobin, platelet and white blood cell count are all associated with increased presence of paraproteinemia, suggesting that these routine biomarkers can be utilized to inform the early and easy screening of potential MGUS, SMM and MM patients. The Iceland Screens, Treats, or Prevents Multiple Myeloma (iStopMM) study is a nationwide ongoing screening program for multiple myeloma (MM) and its precursors including 75,422 participants [24]. Rögnvaldsson et al. seek to determine the effect of follow-up on the survival of MGUS-patients. This includes continuous blood sampling in the study period, and the results to come from this study might corroborate the results of our study on the importance of routine blood samples in hematological malignancies and gammopathies [24].
Conclusion
In conclusion, our study found a relationship between blood levels of hemoglobin, white blood cell and platelet count and the later presence of paraproteinemia. All three parameters showed a higher association with the presence of monoclonal gammopathy at low levels. Furthermore, both platelet count and white blood cell count were similarly associated with a higher presence of monoclonal gammopathy at higher levels. Overall, our results suggest that alterations in these routine hematological parameters can be clinically used to inform serum M protein and FLC testing and may promote the early detection of abnormal plasma cell growth.
Data availability
Data is not publicly available.
References
Kyle RA, Rajkumar SV (2008) Multiple myeloma. Blood 111(6):2962–2972. https://doi.org/10.1182/blood-2007-10-078022
Padala SA, Barsouk A, Barsouk A, Rawla P, Vakiti A, Kolhe R, Kota V, Ajebo GH (2021) Epidemiology, staging, and management of multiple myeloma. Med Sci 9(1):3. https://doi.org/10.3390/medsci9010003
Rajkumar SV (2019) Multiple myeloma: every year a new standard? Hematol Oncol 37(S1):62–65. https://doi.org/10.1002/hon.2586
Solmaz S, Uzun O, Sevindik OG, Demirkan F, Ozcan MA, Ozsan GH, Alacacıoglu I (2023) The effect of haemoglobin, albumin, lymphocyte and platelet score on the prognosis in patients with multiple myeloma. Int J Lab Hematol 45(1):13–19. https://doi.org/10.1111/ijlh.13958
Cowan AJ, Green DJ, Kwok M, Lee S, Coffey DG, Holmberg LA, Tuazon S, Gopal AK, Libby EN (2022) Diagnosis and management of multiple myeloma. JAMA 327(5):464. https://doi.org/10.1001/jama.2022.0003
Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos M-V, Kumar S, Hillengass J, Kastritis E, Richardson P, Landgren O, Paiva B, Dispenzieri A, Weiss B, Leleu X, Zweegman S, Lonial S, Rosinol L, Zamagni E, Jagannath S, Sezer O, Kristinsson SY, Caers J, Usmani SZ, Lahuerta JJ, Johnsen HE, Beksac M, Cavo M, Goldschmidt H, Terpos E, Kyle RA, Anderson KC, Durie BGM, Miguel JFS (2014) International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 15(12):e538–e548. https://doi.org/10.1016/s1470-2045(14)70442-5
Landgren O, Waxman AJ (2010) Multiple myeloma Precursor Disease. JAMA 304(21):2397. https://doi.org/10.1001/jama.2010.1713
Kyle RA, Therneau TM, Rajkumar SV, Larson DR, Plevak MF, Offord JR, Dispenzieri A, Katzmann JA, Melton LJ (2006) Prevalence of Monoclonal Gammopathy of undetermined significance. N Engl J Med 354(13):1362–1369. https://doi.org/10.1056/nejmoa054494
Kyle RA, Larson DR, Therneau TM, Dispenzieri A, Kumar S, Cerhan JR, Rajkumar SV (2018) Long-term follow-up of Monoclonal Gammopathy of undetermined significance. N Engl J Med 378(3):241–249. https://doi.org/10.1056/nejmoa1709974
Rajkumar SV (2016) Updated diagnostic criteria and staging system for multiple myeloma. Am Soc Clin Oncol Educational Book 36e418–e423. https://doi.org/10.1200/edbk_159009
Eisfeld C, Kajüter H, Möller L, Wellmann I, Shumilov E, Stang A (2023) Time trends in survival and causes of death in multiple myeloma: a population-based study from Germany. BMC Cancer 23(1). https://doi.org/10.1186/s12885-023-10787-5
Goyal G, Rajkumar SV, Lacy MQ, Gertz MA, Buadi FK, Dispenzieri A, Hwa YL, Fonder AL, Hobbs MA, Hayman SR, Zeldenrust SR, Lust JA, Russell SJ, Leung N, Kapoor P, Go RS, Gonsalves WI, Kourelis TV, Warsame R, Kyle RA, Kumar SK (2019) Impact of prior diagnosis of monoclonal gammopathy on outcomes in newly diagnosed multiple myeloma. Leukemia 33(5):1273–1277. https://doi.org/10.1038/s41375-019-0419-7
Sigurdardottir EE, Turesson I, Lund SH, Lindqvist EK, Mailankody S, Korde N, Björkholm M, Landgren O, Kristinsson SY (2015) The role of diagnosis and clinical follow-up of Monoclonal Gammopathy of undetermined significance on Survival in multiple myeloma. JAMA Oncol 1(2):168–174. https://doi.org/10.1001/jamaoncol.2015.23
Farag CM, Antar R, Akosman S, Ng M, Whalen MJ (2023) What is hemoglobin, albumin, lymphocyte, platelet (HALP) score? A comprehensive literature review of HALP’s prognostic ability in different cancer types. Oncotarget 14(1):153–172. https://doi.org/10.18632/oncotarget.28367
DMSG (2022) M-komponent analyser ved myelomatose. https://www.dmcg.dk/siteassets/kliniske-retningslinjer---skabeloner-og-vejledninger/kliniske-retningslinjer-opdelt-pa-dmcg/dmsg/dmsg_m-komponent-analyser_v.1.1_admgodk100123.pdf. Accessed 28 february 2024
Li L, Roest M, Sang Y, Remijn JA, Fijnheer R, Smit K, Huskens D, Wan J, De Laat B, Konings J (2022) Patients with multiple Myeloma have a Disbalanced Whole Blood Thrombin Generation Profile. Front Cardiovasc Med 9. https://doi.org/10.3389/fcvm.2022.919495
Boennelykke A, Jensen H, Østgård LSG, Falborg AZ, Hansen AT, Christensen KS, Vedsted P (2022) Cancer risk in persons with new-onset anaemia: a population-based cohort study in Denmark. BMC Cancer 22(1):805. https://doi.org/10.1186/s12885-022-09912-7
Margolis KL (2007) Prospective study of Leukocyte Count as a predictor of incident breast, colorectal, endometrial, and Lung Cancer and Mortality in Postmenopausal Women. Arch Intern Med 167(17):1837. https://doi.org/10.1001/archinte.167.17.1837
Wong JYY, Bassig BA, Loftfield E, Hu W, Freedman ND, Ji B-T, Elliott P, Silverman DT, Chanock SJ, Rothman N, Lan Q (2020) White Blood Cell Count and Risk of Incident Lung Cancer in the UK Biobank. JNCI Cancer Spectr 4(2). https://doi.org/10.1093/jncics/pkz102
Jensvoll H, Blix K, Brækkan SK, Hansen J-B (2014) Platelet count measured prior to Cancer Development is a risk factor for future symptomatic venous thromboembolism: the Tromsø Study. PLoS ONE 9(3):e92011. https://doi.org/10.1371/journal.pone.0092011
Guo Y, Shi D, Zhang J, Mao S, Wang L, Zhang W, Zhang Z, ** L, Yang B, Ye L, Yao X (2019) The Hemoglobin, Albumin, lymphocyte, and platelet (HALP) score is a novel significant prognostic factor for patients with metastatic prostate Cancer Undergoing Cytoreductive Radical Prostatectomy. J Cancer 10(1):81–91. https://doi.org/10.7150/jca.27210
Vlatka P, Marko L, Stefan M, Dorian L (2022) The hemoglobin, albumin, lymphocyte, and platelet (HALP) score is a novel prognostic factor for patients with diffuse large B-cell lymphoma. J Cancer Res Ther 18(3):725–732. https://doi.org/10.4103/jcrt.jcrt_174_21
Sigurbergsdóttir AÝ, Rögnvaldsson S, Thorsteinsdóttir S, Sverrisdóttir I, Sigurðardóttir GÁ, Viðarsson B, Önundarson PT, Agnarsson BA, Sigurðardóttir M, Þorsteinsdóttir I, Ólafsson Í, Þórðardóttir ÁR, Gíslason GK, Ólafsson A, Hultcrantz M, Durie BGM, Harding S, Landgren O, Löve TJ, Kristinsson SY (2023) Disease associations with monoclonal gammopathy of undetermined significance can only be evaluated using screened cohorts: results from the population-based iStopMM study. Haematologica 108(12):3392–3398. https://doi.org/10.3324/haematol.2023.283191
Rögnvaldsson S, Love TJ, Thorsteinsdottir S, Reed ER, Óskarsson JÞ, Pétursdóttir Í, Sigurðardóttir GÁ, Viðarsson B, Önundarson PT, Agnarsson BA, Sigurðardóttir M, Þorsteinsdóttir I, Ólafsson Í, Þórðardóttir ÁR, Eyþórsson E, Jónsson Á, Björnsson AS, Gunnarsson GÞ, Pálsson R, Indriðason ÓS, Gíslason GK, Ólafsson A, Hákonardóttir GK, Brinkhuis M, Halldórsdóttir SL, Ásgeirsdóttir TL, Steingrímsdóttir H, Danielsen R, Dröfn Wessman I, Kampanis P, Hultcrantz M, Durie BGM, Harding S, Landgren O, Kristinsson SY (2021) Iceland screens, treats, or prevents multiple myeloma (iStopMM): a population-based screening study for monoclonal gammopathy of undetermined significance and randomized controlled trial of follow-up strategies. Blood Cancer J 11(5). https://doi.org/10.1038/s41408-021-00480-w
Funding
This study received no funding from any organizations.
Open access funding provided by Copenhagen University
Author information
Authors and Affiliations
Contributions
JRL, AEE, AMH and HLJ contributed to the design, objectives and the review of the study. AEE and HLJ extracted the data and performed the statistical analyses as well as construction of tables and figures. MDC reviewed the study with critical insights.
Corresponding author
Ethics declarations
Ethics approval
No ethical approval was required for this study.
Conflict of interest
None of the authors have any conflicts of interest to disclose in regard to the content of this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 1
: Flowchart of the in- and exclusion process of the study for patients with a white blood cell count (WBC).
Supplementary Fig. 2
: Flowchart of the in- and exclusion process of the study for patients with a hemoglobin measurement.
Supplementary Fig. 3
: Flowchart of the in- and exclusion process of the study for patients with a platelet count.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Røllum-Larsen, J., Engell, A.E., Diaz-delCastillo, M. et al. Association of routine hematological parameters with the development of monoclonal gammopathies: a case-control study of 134,740 patients. Ann Hematol (2024). https://doi.org/10.1007/s00277-024-05822-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00277-024-05822-9