Abstract
Background
Transvaginal suspension procedures often use the sacrospinous ligament (SSL), which attaches onto the ischial spine (IS). However, nerve-related sequelae (e.g., sciatic nerve injury) following such procedures have been reported. Therefore, the current anatomical study was performed to better understand these relationships. Additionally, three case illustrations of patients with injury to the sciatic nerve following sacrospinous ligament suspension procedures are included to exemplify the significance of a thorough knowledge of this anatomy.
Methods
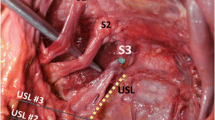
In 20 human adult cadavers (40 sides), a gluteal dissection was performed to expose the IS and SSL and regional nerves near the greater sciatic foramen. Measurements between the IS and SSL were made between these structures and surrounding nerves.
Results
The average distance between the IS and sciatic nerve was 1.4 cm. From this bony part, the average distance to the S1 and S2 ventral rami was 3.1 cm and 1.9 cm, respectively. From the IS to the lumbosacral trunk, pudendal nerve, nerve to obturator internus, and superior gluteal nerve, the mean distance was 4 cm, 0.5 cm, 0.7 cm, and 4.5 cm, respectively. From the SSL to the lumbosacral trunk, S1 ventral ramus, and S2 ventral ramus, there was an average distance of 4.2 cm, 1.6 cm, and 0.8 cm, respectively. Statistically, in females, the distances from the IS and SSL to the sciatic nerve, lumbosacral trunk, superior gluteal nerve, and S1 and S2 ventral rami were shorter when compared to males.
Conclusion
An improved understanding of the relationship between the SSL and IS and nerves near the greater sciatic foramen can lead to fewer intraoperative complications during approaches to various peripheral nerves in this region. Lastly, these relationships might help better understand the nerve injuries following pelvic suspension procedures that use the SSL.





Similar content being viewed by others
Data Availability
Data used in this study are not available.
References
Estrade JP, Agostini A, Roger V, Dallay D, Blanc B, Cravello L (2004) Sacrospinous colpopexy complications. Gynecologie, Obstetrique Fertilite 32:850–854
Ferrando CA, Walters MD (2018) A randomized double-blind placebo-controlled trial on the effect of local analgesia on postoperative gluteal pain in patients undergoing sacrospinous ligament colpopexy. Am J Obstet Gynecol 218:599.e1-599.e8. https://doi.org/10.1016/j.ajog.2018.03.033
Florian-Rodriguez ME, Hare A, Chin K, Phelan JN, Rippenda CM, Corton MM (2016) Inferior gluteal and other nerves associated with sacrospinous ligament: a cadaver study. Am J Obstet Gynecol 215:646e1–6.
Iwanaga J, Puffer RC, Watanabe K, Spinner RJ, Tubbs RS (2019) Division of Sacrospinous and Sacrotuberous Ligaments Expands Access Through Greater Sciatic Foramen: Anatomic Study with Application to Resection of Greater Sciatic Foramen Tumors. World Neurosurg 128:e970–e974. https://doi.org/10.1016/j.wneu.2019.05.045
Iwanaga J, Singh V, Takeda S et al (2022) Standardized statement for the ethical use of human cadaveric tissues in anatomy research papers: Recommendations from Anatomical Journal Editors-in-Chief. Clin Anat 35:526–528. https://doi.org/10.1002/ca.23849
Jelovesk JE, Barber MD, Brubaker L et al (2018) Effect of uterosacral ligament suspension vs. sacrospinous ligament fixation with or without perioperative behavioral therapy for pelvic organ vaginal prolapse on surgical outcomes and prolapse symptoms at 5 years in the OPTIMAL randomized clinical trial. JAMA 319:1554–1565
Katrikh AZ, Ettarh R, Kahn MA (2017) Cadaveric nerve and artery proximity to sacrospinous ligament fixation sutures placed by a suture-capturing device. Obstet Gynecol 130:1033–1038
Lee TG, Unlu BS (2020) Sacrospinous ligament suspension and uterosacral ligament suspension in the treatment of apical prolapse. Gynecol Pelvic Med 3:39
Netter, FH, Hansen JT, Lambert DR. Netter's Clinical Anatomy. Carlstadt, N.J: Icon Learning Systems, 2005.
Rane A, Frazer M, Jain A, Kannan K, Iyer J (2011) The sacrospinous ligament: conveniently effective or effectively convenient? J Obstet Gynaecol 31:366–370. https://doi.org/10.3109/01443615.2011.578225
Sagsoz N, Ersoy M, Kamaci M, Tekdemir I (2022) Anatomical landmarks regarding sacrospinous colpopexy operations performed for vaginal vault prolapse. Eur J Obstet Gynecol Reprod Biol 101:74–78. https://doi.org/10.1016/s0301-2115(01)00507-3
Siddiqui N, Edenfield AL (2014) Clinical challenges in the management of vaginal prolapse. Int J Women’s Health 6:83–94
Acknowledgements
The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase mankind’s overall knowledge that can then improve patient care. Therefore, these donors and their families deserve our highest gratitude. The authors state that every effort was made to follow all local and international ethical guidelines and laws that pertain to the use of human cadaveric donors in anatomical research [5] .
Funding
None.
Author information
Authors and Affiliations
Contributions
LAS: writing—original draft, formal analysis, NI: writing—original draft, ŁO: investigation, writing—review and editing, JI: investigation, writing—review and editing, ASD: writing—review and editing, KKA: resources, methodology, investigation, writing—review and editing, RJS: resources, conceptualization, methodology, investigation, writing—review and editing, RST: resources, conceptualization, methodology, investigation, writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The protocol of the study did not require approval by the ethical committees or informed consent. The study followed the Declaration of Helsinki (64th WMA General Assembly, Fortaleza, Brazil, October 2013).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Seltzer, L.A., Ibrahim, N., Olewnik, Ł. et al. Nerve relationships to the sacrospinous ligament: application to suspension procedures and transgluteal approaches for nerve repair and tumor removal with three case illustrations. Surg Radiol Anat 45, 693–698 (2023). https://doi.org/10.1007/s00276-023-03142-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-023-03142-7