Abstract
Background
Sustaining multiple concussions over one’s lifetime may be associated with behavioral and mood changes beyond the acute phase of injury. The present cross-sectional study examined the relationship between concussion history, the incidence of current moderate-severe psychological distress, and lifetime adolescent hazardous gambling in high school students.
Methods
Four-hundred fifty-nine high school students from southern Sweden (age: 16.81 ± 0.83, 58.2% male) completed a survey assessing concussion history (0,1,2…>8), psychological distress using the Kessler-6 scale, and lifetime hazardous gambling using the NODS-CLiP scale.
Results
Participants who self-reported three or more concussions were more likely to endorse moderate-severe symptoms of psychological distress than those with no concussion history while controlling for covariates, OR = 2.71, 95% CI [1.19, 6.18]. In contrast, concussion history was not associated with hazardous gambling after controlling for confounding variables.
Conclusions
Self-reporting three or more concussions was associated with increased current psychological distress beyond the acute phase of injury among high school students. Adolescents who have sustained multiple concussions should undergo mental health evaluations beyond the acute phase of injury to identify and treat psychological distress, but probing for hazardous gambling may not be clinically relevant in this previously concussed adolescent population.
Similar content being viewed by others
Background
Up to 30 million brain injuries occur worldwide each year [1]. Concussion, often used interchangeably with mild traumatic brain injury (mTBI), is a brain injury caused by a direct or indirect blow to the head, neck, or body that transmits significant biomechanical force to the head and brain [2]. This force precipitates a cascade of neurobiological changes and subsequent neurologic dysfunction lasting for days to weeks following injury [3]. In contrast to our well-established understanding of concussion symptomology in the acute phase of injury (< 1 month), the long-term consequences of concussion on cognitive, physical, and psychological health are still the subject of intense debate and remain at the forefront of research [4]. Recent research, despite a lack of consensus, suggests a dose-dependent relationship between concussion, specifically sports-related concussion (SRC), and the later development of depression, emotional disturbance, sleep abnormalities, and addictive behaviors [5,6,7,8,9,10,11,12,13].
Depression and anxiety, sometimes grouped and defined as psychological distress, are among the most common mood-related symptoms reported by adolescents post-concussion [14]. These symptoms often spontaneously resolve within a month, but many patients continue to present with symptoms beyond the acute phase of injury [15, 16], or these symptoms slowly reemerge after a period of remission. A meta-analysis of 89,114 children with concussion by Gornall and colleagues [5] found that pediatric concussion was associated with increased odds of exhibiting internalizing symptoms, such as depression and anxiety beyond three months post-injury. Additionally, a recent retrospective cohort study conducted by Ledoux and colleagues [8] compared 152,321 children with concussion to 296,482 age and gender-matched controls with orthopedic injuries. Their study revealed that both single and multiple concussions were linked to a higher risk of receiving a mental health diagnosis over time compared to sustaining an orthopedic injury. Despite these large-scale studies, there is a dearth of high-quality studies demonstrating how this relationship is influenced by individual factors in, specifically, older adolescent student populations who are more likely to begin experiencing symptoms of depression and anxiety [17].
Research on behavioral addictions, specifically gambling for money, has expanded tremendously since the addition of non-substance-related disorders in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [18]. Gambling disorder (GD), is an addictive disorder characterized by a “persistent and recurrent problematic gambling behavior leading to clinically significant impairment or distress” [18 pp. 585], which affects approximately 5.8% of adolescents and 7.0% of elite athletes in Sweden [19, 20]. In Sweden, gambling for money is forbidden for individuals under the age of 18, though many minors find avenues to engage in gambling activities [19]. Due to its prohibition for minors, prevalence metrics may underestimate the occurrence of adolescent gambling behavior and GD.
GD is characterized by tolerance, an inability to abstain from gambling activities, preoccupation with gambling, chasing losses, lying to conceal gambling activity, and reliance on others for financial support due to gambling [21]. In addition to significant psychosocial and financial distress, those with GD have a lower quality of life and a higher suicide risk [21]. The etiology and course of GD are complex, and researchers have only recently begun to uncover the role that brain injury and concussion play in the development of GD. As emphasized in Olsen and Corrigan’s examination of TBI as a precursor to substance use and substance use disorders [13], there exists a significant increase in risky substance use after the initial stage of TBI-injury. They posit that TBI fosters risky substance use through physiological mechanisms linked to persistent alterations in neuroplasticity, neuroimmune signaling, and network connectivity, all of which could potentially be generalized to non-substance use addictive disorders, such as GD. In fact, researchers have taken an interest in measuring how TBI may first engender hazardous gambling, a pattern of gambling that resembles and often precedes GD, albeit not at the severity required to satisfy criteria for a GD diagnosis [22]. Previous studies have demonstrated that moderate-to-severe TBI independently predicts subsequent hazardous gambling in Canadian adults and adolescents [23,24,25,26], as well as American veterans [27] which may be attributable to TBI-induced impaired risk-based decision-making and increased motor impulsivity as evidenced by preclinical trials using rodent models [28, 29]. For instance, Shaver and colleagues [29] conducted a preclinical experiment where they exposed 4-month-old rats to either a controlled cortical impact or a sham procedure. They then monitored the rats’ performance in a task resembling the Iowa Gambling Task over the course of 12 weeks. Their findings revealed that rats subjected to the cortical impact opted for suboptimal alternatives more often than sham controls, indicating impaired risk-based decision-making. Despite growing evidence linking more severe forms of TBI and later hazardous gambling in various age-groups and demographics, no study hitherto has assessed the relationship between concussion history and adolescent hazardous gambling.
Adolescence is a critical stage of physical and psychosocial development during which high-risk behaviors, like gambling, are popular and pervasive among certain subgroups [30,31,32]. Hazardous gambling during this stage may lead to a myriad of immediate consequences that hinder development and ultimately have a negative impact on the individual long-term. For example, adolescents who exhibit hazardous gambling are more likely to have poorer school performance and drop out, have familial issues at home, have weakened intimate relationships, engage in illicit substance use, and experience career disruptions that are at least partially attributable to the consequences of earlier adolescent hazardous gambling [33, 34]. Attenuating the burden of adolescent gambling on the individual and society is therefore of high priority.
Aims and hypotheses
Based on previous research indicating that multiple concussions in an individual’s lifetime leads to poorer mental health outcomes [5,6,7,8,9], that adolescence is a transitional period when critical development and risky behavior (i.e., illicit gambling) occur [30,31,32], and that GD is associated with poorer quality of life and suicide [21], understanding the genesis of hazardous gambling and psychological distress in adolescent populations and its relationship to concussion is essential. Thus, the purpose of the present study is to assess the impact of concussion history on psychological distress and hazardous gambling behavior in youth populations while controlling for known covariates, namely age, sex, body mass index (BMI), athlete status, sport type, current and previous parental gambling, as well as previous diagnosis of attention deficit hyperactivity disorder (ADHD), autism spectrum disorder (ASD), and learning disorders (LD). The inclusion of these variables was based on existing literature indicating that older adolescents, males, those with higher BMI, athletes, those with parents who have a history of gambling, and those with psychiatric disorders are more likely to exhibit hazardous gambling behavior [35,36,37,38]. Several of these factors are also associated with increased odds of sustaining concussion and develo** persisting concussive symptoms [5, 16, 39, 40]. We hypothesize that (1) students reporting more previous concussions will be more likely to report greater psychological distress and exhibit hazardous gambling behavior (2) that these relationships will remain significant when controlling for individual differences. Results will contribute to the literature map** the potential post-acute effects of concussion on mental health and addictive behavior.
Methods
Participants
Each of the twenty high schools with at least one sports-tailored program located in Skåne county, Sweden were invited to participate. Eleven of twenty principals (55%) agreed to distribute the survey link to students through their respective instructors in class. A total of 661 participants consented and continued onto the survey, of which 463 (70%) provided a response to at least half of items. Four participants reported sustaining a concussion in the previous month and were excluded from further analysis to avoid assessing the consequences of acute concussion symptoms on outcome measures, leading to a final sample size of 459 participants.
Procedure
The present observational study utilized a cross-sectional survey design. High school principals representing a school district in Skåne County, Sweden offering both traditional and sports-tailored curriculums were contacted via email and telephone. In Sweden, sports-tailored high school programs integrate the traditional high school curriculum with the training and competition schedules of student-athletes. Student-athletes can apply to tailored programs at the national, regional, and local levels, with the level of competition and demand on student-athletes depending on the program’s level [41]. All students attending these high schools were invited to participate, regardless of whether they were enrolled in tailored or traditional curricula or competed at the national, regional, or local levels. Students typically enter high school at the age of 16 and complete their studies within three years. Students were informed of the goals of the study and that their participation was voluntary and anonymous before entering the survey. Data collection took place between January 16th and February 17th, 2023. A reminder to participating principals was sent two weeks prior to closing the survey. Ethical approval for the present project was sought through the Swedish Ethical Review Authority, who came to the decision that formal ethical approval was not required because no personal identifiable data were to be collected (#DNr: 2022-04648-01, October 30th, 2022). In accordance with Swedish Law concerning the ethical review of research involving humans (SFS 2003:460 [42]), only students 15 years or older were invited to participate. Study procedures adhered to the Declaration of Helsinki and participants provided digital informed consent prior to proceeding to the survey.
Measures
Psychological distress
Non-specific psychological distress was assessed using the Swedish-translated Kessler-6 scale (K6) [43], which is the short-form of the K10 scale whose Danish translation has been validated [44]. The K6 scale consists of six items pertaining to how often an individual has experienced depression- and anxiety-related symptoms over the past six months. Responses were given on a five-point Likert-type scale ranging from “not at all” (0) to “all the time” (4). Item scores were summed (0–24) and grouped based on Furukawa and colleagues’ [45] suggestions: no/low distress (0–7), moderate distress (8–12), and severe distress (13–24). Internal consistency of the scale in the present study was high (Cronbach’s α = 0.87).
Hazardous gambling
Lifetime hazardous gambling was assessed using the three-item version of the National Opinion Research Center DSM-IV Screen for Gambling Problems – Control, Lying, and Preoccupation (NODS-CLiP) [46, 47]. The screen includes three items probing for the incidence of loss of control, lying, and preoccupation associated with gambling during the participant’s lifetime, to which they respond on a binary “Yes” or “No” scale. Endorsing one of the three behaviors in relation to one’s gambling results in a positive screening for lifetime hazardous gambling. The NODS-CLiP has ample sensitivity and is preferable to other iterations of the original NODS scale, such as the NODS-PERC, in general population samples where the prevalence rate of hazardous gambling is low [47].
Individual differences
Demographics pertaining to age, sex, height, weight, athlete status, sport type, current and previous parental gambling, as well as previous ADHD, ASD, or LD diagnoses were collected to serve as covariates based on prior research [35,36,37,38, 48]. Height and weight were used to calculate participant BMI. Athlete status was coded on a binary scale based on student enrollment in sports-tailored academic programs. Reporting of at least one current or prior ADHD, ASD, or LD diagnosis was coded on a binary scale. Parental gambling behavior was assessed with two items, “Has your mother/father gambled in the last 12 months” (No, never; Yes, occasionally; Yes, often; Do not know). Responses were transformed to be binary. If participants reported that either of their parents gambled occasionally or gambled often, responses were coded as positive (1), while those that indicated that their parents did not gamble or did not know were coded as negative (0).
Concussion history
Participants were presented with the following commonly used definition of concussion to assess concussion history, “A concussion is an injury occurring typically, but not necessarily, from a blow to the head, followed by a variety of symptoms that may include any of the following: headache, dizziness, loss of balance, blurred vision, ‘seeing stars,’ feeling in a fog or slowed down, memory problems, poor concentration, nausea, throwing up, and loss of consciousness. Getting ‘knocked out’ or being unconscious does not always occur from a concussion” [49, pp.2]. Participants were asked based on this definition how many times they had sustained a concussion, both diagnosed and undiagnosed. Reponses were given on an interval scale (0, 1, 2… 8+), but were ultimately stratified into 0, 1–2, and 3+ concussions, as was predetermined based on contemporary concussion research [50, 51]. Participants were also asked when their latest concussion occurred to control for the acute effects of concussion injury on outcome measures.
Statistical analyses
Missing data were processed using both simple and multiple imputation strategies. Missing data for K6 items were imputed with participants’ scale median, while missing demographic data were imputed via logistic regression for binary variables (e.g., sex) and linear regression for continuous variables (e.g., height and weight) through multiple imputation by chained equations with the mice() package. Assumptions of multicollinearity and linearity were assessed using VIF values and scatterplots of the log odds of the dependent variable against continuous predictor variables, respectively. BMI was not related to hazardous gambling nor psychological distress logits and was therefore not included in our logistic regression models. The assumption of no outliers was met as assessed by Cook’s distance. Age and BMI were not normally distributed, as assessed by Shapiro-Wilk’s tests (p < .05). Therefore, demographic variables were compared across concussion groups using the non-parametric alternative to analysis of variance, Kruskal-Wallis H test, for continuous variables and Chi-square (χ2) analyses for binary variables. The Benjamini-Hochberg procedure was carried out on p-values to account for increased risk of Type I error from multiple comparison across groups [52].
Thereafter, we conducted a series of binary logistic regressions predicting psychological distress with concussion history independently in Model 1a and alongside important covariates in Model 2a (age, BMI, sex, athlete status, and psychiatric history). We then conducted penalized logistic regressions with Firth’s bias reduction method [53] and post hoc intercept adjustments [54] to predict NODS-CLiP results with concussion history as an independent predictor in Model 1b as well as when controlling for important covariates in Model 2b (age, BMI, sex, athlete status, psychiatric history, parental gambling). A Firth regression was preferred due to the rareness of hazardous gambling in this population, which can lead to separation in logistic regression [55]. Rv4.2.1 was used to conduct all analyses, including the logistf() [56], stats(), and car() packages.
Results
Participants
Missing data for participants were minimal (2.2%, 613/27,317) and deemed missing at random based on visual inspection of missing data patterns. Participants were 16.81 ± 0.83 years old with a BMI of 22.08 ± 2.88 \(\frac{kg}{{m}^{2}}\). Most were male (n = 267, 58.2%), in their first year of secondary school (n = 219, 47.8%), enrolled in a sports-tailored high school curriculum (n = 242, 52.7%), and lived at home with parents, step-parents, or caregivers (n = 437, 95.2%). Fifteen students reported an ADHD diagnosis, four students reported an ASD diagnosis, and 37 students reported having a LD (e.g., dyslexia). Approximately half (47.3%) of all students reported any form of gambling across their lifetime, while 24.6% reported gambling in the past 30 days. The most popular gambling types were in-person cards or poker (30.3%lifetime, 10.0%current), online sports betting (20.7%lifetime, 9.6%current), and within computer game gambling (i.e., to win real money or play the game; 20.0%lifetime, 7.2%current).
Overall, participant mean K6 scores were 7.52 ± 4.87 (0–24), with 113 (24.6%) participants endorsing moderate symptoms and 69 (15.0%) endorsing severe symptoms of psychological distress. On the other hand, 41 (8.9%) participants were identified as hazardous gamblers according to NODS-CLiP results, with 24 (5.2%) reporting loss of control over their gambling, 17 (3.7%) reporting lying to conceal their gambling, and 22 (4.8%) reporting preoccupation of gambling-related thoughts. A similar percentage of students enrolled in sports-tailored programs and traditional curricula were identified as hazardous gamblers (8.3%sports−tailored vs. 9.7%traditional). Of participants enrolled in a sports-tailored high school curriculum, there was no difference in the prevalence of hazardous gambling between team sport athletes (n = 14, 8.0%) and individual sport athletes (n = 6, 9.0%), χ2(1) = 0.058, p = .81, padj = 0.99.
Most participants reported no previous concussions (n = 311, 67.8%), while 120 (26.1%) reported 1–2 previous concussions, and 28 (6.1%) reported 3 or more concussions. Of participants enrolled in a sport preparatory program, the majority participated in team sports (72.0%), with soccer (32.1%) and handball (30.9%) being most common. Sociodemographic variables stratified by concussion group are presented in Table 1.
Chi-square analyses indicated that there were differences in the percentages of participants diagnosed with ADHD, ASD, or LD across concussion groups χ2(2) = 11.965, p = .003, padj = 0.038, V = 0.161. Post hoc pairwise comparisons revealed that fewer participants with no concussion history reported a diagnosis than those with three or more concussions, χ2(1) = 8.645, p = .003, padj = 0.025, V = 0.160, and those with 1–2 concussions, χ2(1) = 6.894, p = .009, padj = 0.043, V = 0.126. The percentage of participants with a diagnosis did not differ between participants with 1–2 concussions and those with three or more, χ2(1) = 1.057, p = .30, padj = 0.57, V = 0.085.
Effect of concussion history on psychological distress and hazardous gambling
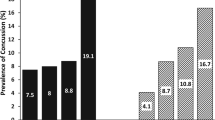
Binomial logistic regressions were performed to ascertain the effect of concussion history on the likelihood that participants were to report moderate to severe psychological distress. In the crude model only including concussion history as a predictor (Model 1a), only those sustaining three or more concussions were more likely to exhibit moderate to severe psychological distress, having 2.78 times greater odds than those with no concussion history. In the adjusted model including age, sex, athlete status, and psychiatric history as covariates (Model 1b), sustaining three or more concussions remained a significant predictor of moderate to severe psychological distress, having 2.71 higher odds than those with no concussion history. Additional binomial logistic regressions were performed to assess the crude effect of concussion history on the likelihood that participants were to exhibit hazardous gambling. In both the crude model only including concussion history as a predictor (Model 1b) and the adjusted model including age, sex, athlete status, psychiatric history, and lifetime parental gambling as covariates (Model 2b), concussion history was not predictive of hazardous gambling. Model parameters are presented in Table 2. Crude models of the effect of concussion history on the percentage of participants screening positively for moderate to severe psychological distress and hazardous gambling are illustrated in Fig. 1A, while odds ratios for adjusted models including covariates predicting positive screenings (Model 2a & 2b) are illustrated in Fig. 1B.
Moderate-Severe Psychological Distress and Hazardous Gambling Across Concussion Group. Note. Concussion history as a predictor of psychological distress (K6) and hazardous gambling (NODS-CLiP). A: Crude differences in proportions between concussion groups screening positive for moderate to severe psychological distress and hazardous gambling. The proportion of participants with 3 + more concussions reporting moderate to severe psychological distress was significantly higher than those with no concussion history. No differences were found in hazardous gambling across concussion groups. Dotted lines illustrate linear fitted model. B: Adjusted odds ratios with 95% confidence intervals (CI) for logistic regression models predicting outcome variables while controlling for covariates (Model 2a & 2b). Firth regression used for hazardous gambling model. The odds ratio predicting moderate to severe psychological distress from concussion history was significant for those with 3 + concussions. Psychological Distress = positive K6 screen. Hazardous Gambling = positive NODS-CLiP screen. *p < .05
Discussion
Concussion and TBI have been linked to the development of long-term mental health issues and addictive behaviors [5,6,7,8,9, 23, 25,26,27], yet little research has targeted psychological distress in adolescent students nor examined the relationship between concussion and adolescent hazardous gambling. Accordingly, the present study evaluated how concussion history was associated with psychological distress and hazardous gambling while controlling for important individual differences. Assessing this relationship is essential for (a) accurately informing individuals of the risks involved in activities that expose them to biomechanical impacts (sports, military service, etc.), (b) informing clinicians of potential sequelae of concussive injuries to better meet their patients’ needs, and (c) providing a better picture for how we can proactively reduce the risk and severity of concussion.
Controlling for important covariates associated with concussion, psychological distress, and hazardous gambling, we found that concussion history was associated with increased psychological distress for students reporting three or more previous concussions, but not associated of hazardous gambling, which partially supports our hypotheses (Fig. 1). According to Models 1a and 2a, only in students that self-reported three or more concussions was there an increase in odds of moderate to severe psychological distress. These findings are in line with a growing body of literature highlighting that concussions can lead to increases in psychological distress over time [5, 9]. Non-significant results regarding associations between concussion and hazardous gambling contrasts studies indicating that TBI or concussion is associated with hazardous gambling [23,24,25,26,27]. Including covariates proved to be essential in more accurately assessing the effects of concussion history on outcomes. As expected, age and gender were important confounders to account for. Being 18 years or older was associated with greater odds of endorsing hazardous gambling, while identifying as female was associated with greater psychological distress but lower odds of hazardous gambling, which is consistent with similar studies in adolescent populations [19, 31, 41].
There are several possible explanations as to why only students with three or more concussions were more likely to endorse moderate to severe levels of psychological distress. Sustaining multiple concussions can be psychologically traumatic and have a lasting negative impact on an individual. For example, the increased likelihood of sustaining an additional concussion after the initial injury [40, 57] can contribute to the fear and anxiety an individual experiences returning to the modality where the injury occurred (e.g., sport, military duty, driving) [58, 59]. In addition, being forcibly sidelined and subjected to recovery procedures multiple times can be stressful and depressing for individuals that rely heavily on, for example, sports for social connection, physical conditioning, structure, and overall well-being [58]. Similarly, there are several possible explanations as to why hazardous gambling was not associated with concussion history. Primarily, gambling is a restricted activity for people under the age of eighteen in Sweden [60], and therefore less accessible and available to a large proportion of the students who participated in the present study. Secondly, despite evidence from preclinical research suggesting potential mechanisms for a causal link between brain injury and hazardous gambling [28, 29], no brain imaging studies in the clinical context testing this theory exist currently. Likewise, whether gambling is a common strategy to cope with concussion-induced chronic symptoms has not been explored. Lastly, previous studies demonstrating a relationship largely recruited participants who had sustained moderate-to-severe TBI injuries or recruited participants who were older [23,24,25,26,27]. It may be that gambling behavior is not affected by TBIs of lower severity. Future research detailing how neurobiological changes and psychological responses to concussion contribute to changes in gambling behavior may aid in elucidating this relationship and yield more conclusive results.
Limitations
The current study’s findings must be interpreted carefully considering its limitations. Most importantly, causation cannot be assessed due to the cross-sectional design of the study. The onset of psychological distress and hazardous gambling behavior may have occurred prior to concussion, or the time required for symptoms to manifest after concussion was insufficient. Concerning our recruitment strategy, we cannot report an accurate overall response rate from students, as it behooved principals to distribute the survey link to instructors. Despite more than half of the schools agreeing to participate, the exclusion of students from both non-participating schools and, likely, a portion of students from participating schools who were not invited for unknown reasons introduces a degree of sampling bias. In relation to the measures used in the present study, the NODS-CLiP questionnaire used is a brief form that has the potential of being overly sensitive, meaning that recreational, non-problematic gamblers may screen positively, possibly leading to spurious results [47]. In addition, our assessment of concussion history did not evaluate the severity of previous concussive injuries, which may have contributed to greater variation in the relative burden of injury sustained across concussions. Similarly, concussion history as well as other measures were self-reported and subject to bias. However, self-reported concussion history was preferred in the present study to avoid the underreporting associated with requiring that concussions had to have been diagnosed by a medical professional [61]. Furthermore, the present study was unable to account for all known comorbid and pre-morbid covariates (history of depression, alcohol use, sleep disturbance) associated with the development of hazardous gambling and psychological distress. Lastly, the sample size may have not yielded sufficient statistical power to assess these relationships accurately considering the inherent heterogeneity of concussive injuries. Future research would benefit from having larger sample sizes which would enable far more comprehensive models to assess the relationships between concussion, gambling behavior, and psychological distress.
Conclusions
In sum, our findings imply that mental health evaluations beyond the acute phase of injury in adolescents and young adults who have sustained multiple concussions may be of relevance to clinicians in identifying and managing post-acute concussion sequelae. Additionally, these preliminary data do not provide support probing for hazardous gambling in adolescents who have sustained multiple mild brain injuries. The nature of this connection will be better understood by subsequent research conducted with larger samples.
Data availability
Data can be made available upon request.
References
James SL, Theadom A, Ellenbogen RG, Bannick MS, Montjoy-Venning W, Lucchesi LR, et al. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet Neurol. 2019;18(1):56–87. https://doi.org/10.1016/S1474-4422(18)30415-0.
Patricios JS, Schneider KJ, Dvorak J, Ahmed OH, Blauwet C, Cantu RC, Davis GA, Echemendia RJ, Makdissi M, McNamee M, Broglio S. Consensus statement on concussion in sport: the 6th International Conference on Concussion in Sport–Amsterdam, October 2022. Br J Sports Med. 2023;57(11):695–711. https://doi.org/10.1136/bjsports-2023-106898.
Giza CC, Hovda DA. The new neurometabolic cascade of concussion. Neurosurg. 2014;75(suppl4):S24–33. https://doi.org/10.1227/NEU.0000000000000505.
McAllister T, McCrea M. Long-term cognitive and neuropsychiatric consequences of repetitive concussion and head-Impact exposure. J Athl Train. 2017;52(3):309–17. https://doi.org/10.4085/1062-6050-52.1.14.
Gornall A, Takagi M, Morawakage T, Liu X, Anderson V. Mental health after paediatric concussion: a systematic review and meta-analysis. Br J Sports Med. 2021;55(18):1048–58. https://doi.org/10.1136/bjsports-2020-103548.
Gouttebarge V, Kerkhoffs GM. Sports career-related concussion and mental health symptoms in former elite athletes. Neurochirurgie. 2021;67(3):280–2. https://doi.org/10.1016/j.neuchi.2020.01.001.
Kilic Ö, Hopley P, Kerkhoffs GM, Lambert M, Verhagen E, Viljoen W, Wylleman Gouttebarge V. Impact of concussion and severe musculoskeletal injuries on the onset of mental health symptoms in male professional rugby players: a 12-month study. BMJ Open Sport Exerc Med. 2019;5(1):e000693. https://doi.org/10.1136/bmjsem-2019-000693.
Ledoux AA, Webster RJ, Clarke AE, Fell DB, Knight BD, Gardner W, Cloutier P, Gray C, Tuna M, Zemek R. Risk of Mental Health problems in children and youths following concussion. JAMA Net. 2022;5(3):e221235. https://doi.org/10.1001/jamanetworkopen.2022.1235.
Rice SM, Parker AG, Rosenbaum S, Bailey A, Mawren D, Purcell R. Sport-related concussion and mental health outcomes in elite athletes: a systematic review. Sports Med. 2018;48(2):447–65. https://doi.org/10.1007/s40279-017-0810-3.
Tjønndal A. NHL heavyweights: narratives of violence and masculinity in ice hockey. Phys Cult Sport Stud Res. 2016;70(1):55–68.
Corrigan JD, Bogner J, Mellick D, Bushnik T, Dams-O’Connor K, Hammond FM, et al. Prior history of traumatic brain Injury among persons in the traumatic brain Injury Model Systems National Database. Arch Phys Med Rehabil. 2013;94(10):1940–50. https://doi.org/10.1016/j.apmr.2013.05.018.
Cottler LB, Ben Abdallah A, Cummings SM, Barr J, Banks R, Forchheimer R. Injury, pain, and prescription opioid use among former National Football League (NFL) players. Drug Alcohol Depend. 2011;116(1):188–94. https://doi.org/10.1016/j.drugalcdep.2010.12.003.
Olsen CM, Corrigan JD. Does traumatic Brain Injury cause Risky Substance Use or Substance Use Disorder? Biol Psychiatry. 2022;91(5):421–37. https://doi.org/10.1016/j.biopsych.2021.07.013.
Kontos AP, Sufrinko A, Sandel N, Emami K, Collins MW. Sport-related Concussion Clinical profiles: clinical characteristics, targeted treatments, and preliminary evidence. Curr Sports Med Rep. 2019;18(3):82. https://doi.org/10.1249/JSR.0000000000000573.
Broglio SP, Collins MW, Williams RM, Mucha A, Kontos AP. Current and emerging Rehabilitation for Concussion: a review of the evidence. Clin Sports Med. 2015;34(2):213–31. https://doi.org/10.1016/j.csm.2014.12.005.
Iverson GL, Gardner AJ, Terry DP, Ponsford JL, Sills AK, Broshek DK, et al. Predictors of clinical recovery from concussion: a systematic review. Br J Sports Med. 2017;51(12):941–8. https://doi.org/10.1136/bjsports-2017-097729.
Cummings CM, Caporino NE, Kendall PC. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychol Bull. 2014;140:816–45. https://doi.org/10.1037/a0034733.
American Psychiatric Association DS, American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American psychiatric association; 2013. https://doi.org/10.1176/appi.books.9780890425596.
Gerdner A, Håkansson A. Prevalence and comorbidity in a Swedish adolescent community sample – gambling, gaming, substance use, and other psychiatric disorders. BMC Psychiatry. 2022;22(1):594. https://doi.org/10.1186/s12888-022-04218-1.
Håkansson A, Kenttä G, Åkesdotter C. Problem gambling and gaming in elite athletes. Addict Behav Rep. 2018;8:79–84. https://doi.org/10.1016/j.abrep.2018.08.003.
Potenza MN, Balodis IM, Derevensky J, Grant JE, Petry NM, Verdejo-Garcia A, et al. Gambling disorder. Nat Rev Dis Primers. 2019;5(1):1–21. https://doi.org/10.1038/s41572-019-0099-7.
World Health Organization. International Classification of Diseases, Eleventh Revision (ICD-11). 2019/2021. https://icd.who.int/browse11.
Bhatti JA, Thiruchelvam D, Redelmeier DA. Traumatic brain injury as an independent risk factor for problem gambling: a matched case-control study. Soc Psychiatry Psychiatr Epidemiol. 2019;54(4):517–23. https://doi.org/10.1007/s00127-018-1583-1.
Hodgins DC, Holub A. Components of Impulsivity in Gambling Disorder. Int J Ment Health Addict. 2015;13(6):699–711. https://doi.org/10.1007/s11469-015-9572-z.
Turner NE, McDonald AJ, Ialomiteanu AR, Mann RE, McCready J, Millstone D, et al. Moderate to severe gambling problems and traumatic brain injury: a population-based study. Psychiatry Res. 2019;272:692–7. https://doi.org/10.1016/j.psychres.2018.12.170.
Turner NE, Cook S, Shi J, Elton-Marshall T, Hamilton H, Ilie G, et al. Traumatic brain injuries and problem gambling in youth: evidence from a population-based study of secondary students in Ontario, Canada. PLoS ONE. 2020;15(10):e0239661. https://doi.org/10.1371/journal.pone.0239661.
Whiting SW, Potenza MN, Park CL, McKee SA, Mazure CM, Hoff RA. Investigating veterans’ Pre-, Peri-, and Post-deployment experiences as potential risk factors for Problem Gambling. J Behav Addictions. 2016;5(2):213–20. https://doi.org/10.1556/2006.5.2016.027.
Ozga-Hess JE, Whirtley C, O’Hearn C, Pechacek K, Vonder Haar C. Unilateral parietal brain injury increases risk-taking on a rat gambling task. Exp Neurol. 2020;327:113217. https://doi.org/10.1016/j.expneurol.2020.113217.
Shaver TK, Ozga JE, Zhu B, Anderson KG, Martens KM, Vonder Haar C. Long-term deficits in risky decision-making after traumatic brain injury on a rat analog of the Iowa gambling task. Brain Res. 2019;1704:103–13. https://doi.org/10.1016/j.brainres.2018.10.004.
Calado F, Alexandre J, Griffiths MD. Prevalence of adolescent Problem Gambling: a systematic review of recent research. J Gambl Stud. 2017;33(2):397–424. https://doi.org/10.1007/s10899-016-9627-5.
Claesdotter-Knutsson E, André F, Fridh M, Delfin C, Håkansson A, Lindström M. Gender differences and Associated Factors Influencing Problem Gambling in adolescents in Sweden: cross-sectional investigation. JMIR Pediatr Parent. 2022;5(1):e35207. https://doi.org/10.2196/35207.
Huang JH, Boyer R. Epidemiology of youth gambling problems in Canada: A National Prevalence Study. Can J Psychiatry. 2007;52(10):657–65. https://doi.org/10.1177/070674370705201006.
Delfabbro P, King DL, Derevensky JL. Adolescent gambling and Problem Gambling: prevalence, current issues, and concerns. Curr Addict Rep. 2016;3(3):268–74. https://doi.org/10.1007/s40429-016-0105-z.
Livazović G, Bojčić K. Problem gambling in adolescents: what are the psychological, social and financial consequences? BMC Psychiatry. 2019;19(1):308. https://doi.org/10.1186/s12888-019-2293-2.
Algren MH, Ekholm O, Davidsen M, Larsen CVL, Juel K. Health Behaviour and Body Mass Index among Problem gamblers: results from a Nationwide Survey. J Gambl Stud. 2015;31(2):547–56. https://doi.org/10.1007/s10899-013-9437-y.
Chamberlain SR, Aslan B, Quinn A, Anilkumar A, Robinson J, Grant JE, et al. Autism and gambling: a systematic review, focusing on neurocognition. Neurosci Biobehavioral Reviews. 2023;147:105071. https://doi.org/10.1016/j.neubiorev.2023.105071.
Parker JDA, Summerfeldt LJ, Taylor RN, Kloosterman PH, Keefer KV. Problem gambling, gaming and internet use in adolescents: relationships with emotional intelligence in clinical and special needs samples. Pers Indiv Differ. 2013;55(3):288–93. https://doi.org/10.1016/j.paid.2013.02.025.
Theule J, Hurl KE, Cheung K, Ward M, Henrikson B. Exploring the relationships between Problem Gambling and ADHD: a Meta-analysis. J Atten Disord. 2019;23(12):1427–37. https://doi.org/10.1177/1087054715626512.
Covassin T, Savage JL, Bretzin AC, Fox ME. Sex differences in sport-related concussion long-term outcomes. Int J Psychophysiol. 2018;132:9–13. https://doi.org/10.1016/j.ijpsycho.2017.09.010.
Putukian M, Riegler K, Amalfe S, Bruce J, Echemendia R. Preinjury and Postinjury factors that Predict sports-related concussion and clinical recovery time. Clin J Sport Med. 2021;31(1):15. https://doi.org/10.1097/JSM.0000000000000705.
Andersson MJ, Kenttä G, Moesch K, Borg E, Claesdotter-Knutsson E, Håkansson A. Depression and anxiety symptoms in elite high school student-athletes in Sweden during the covid-19 pandemic: a repeated cross-sectional. J Sports Sci. 2023;41(9):874–83. https://doi.org/10.1080/02640414.2023.2241783.
Law Concerning the Ethical Review of Research Involving. Humans (lag om etikprövning av forskning som avser människor) (SFS 2003:460). Stockholm: Ministry of Education and Research.
Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–76. https://doi.org/10.1017/S0033291702006074.
Thelin C, Mikkelsen B, Laier G, Turgut L, Henriksen B, Olsen LR, et al. Danish translation and validation of Kessler’s 10-item psychological distress scale – K10. Nord J Psychiatry. 2017;71(6):411–6. https://doi.org/10.1080/08039488.2017.1312517.
Furukawa TA, Kawakami N, Saitoh M, Ono Y, Nakane Y, Nakamura Y, et al. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int J Methods Psychiatr Res. 2008;17(3):152–8. https://doi.org/10.1002/mpr.257.
Toce-Gerstein M, Gerstein DR, Volberg RA. The NODS–CLiP: a Rapid screen for adult pathological and Problem Gambling. J Gambl Stud. 2009;25(4):541–55. https://doi.org/10.1007/s10899-009-9135-y.
Volberg RA, Munck IM, Petry NM. A quick and simple screening method for pathological and Problem Gamblers in Addiction Programs and practices. Am J Addictions. 2011;20(3):220–7. https://doi.org/10.1111/j.1521-0391.2011.00118.x.
Brett BL, Kuhn AW, Yengo-Kahn AM, Solomon GS, Zuckerman SL. Risk factors associated with sustaining a sport-related concussion: an initial synthesis study of 12,320 student-athletes. Arch Clin Neuropsychol. 2018;33(8):984–92. https://doi.org/10.1093/arclin/acy006.
McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in High School Football players: implications for Prevention. Clin J Sport Med. 2004;14(1):13.
Brett BL, Walton SR, Kerr ZY, Nelson LD, Chandran A, Defreese JD, et al. Distinct latent profiles based on neurobehavioural, physical and psychosocial functioning of former National Football League (NFL) players: an NFL-LONG study. J Neurol Neurosurg Psychiatry. 2021;92(3):282–90. https://doi.org/10.1136/jnnp-2020-324244.
Kerr ZY, Walton SR, Brett BL, Chandran A, DeFreese JD, Mannix R, et al. Measurement implications on the association between self-reported concussion history and depression: an NFL-LONG study. Clin Neuropsychol. 2022;0(0):1–18. https://doi.org/10.1080/13854046.2022.2094834.
Benjamini Y, Hochberg Y. Controlling the false Discovery rate: a practical and powerful Approach to multiple testing. J Roy Stat Soc: Ser B (Methodol). 1995;57(1):289–300. https://doi.org/10.1111/j.2517-6161.1995.tb02031.x.
Firth D. Bias reduction of maximum likelihood estimates. 1993;80(1):27–38. https://doi.org/10.1093/biomet/80.1.27.
Puhr R, Heinze G, Nold M, Lusa L, Geroldinger A. Firth’s logistic regression with rare events: accurate effect estimates and predictions? Stat Med. 2017;36(14):2302–17. https://doi.org/10.1002/sim.7273.
Heinze G, Schemper M. A solution to the problem of separation in logistic regression. Stat Med. 2002;21(16):2409–19. https://doi.org/10.1002/sim.1047.
Heinze G, Ploner M, Dunkler D, Southworth H, Heinze M. Package ‘logistf’. 2022.
van Ierssel J, Osmond M, Hamid J, Sampson M, Zemek R. What is the risk of recurrent concussion in children and adolescents aged 5–18 years? A systematic review and meta-analysis. Br J Sports Med. 2021;55(12):663–9. https://doi.org/10.1136/bjsports-2020-102967.
Bloom GA, Trbovich AM, Caron JG, Kontos AP. Psychological aspects of sport-related concussion: an evidence-based position paper. J Appl Sport Psychol. 2022;34(3):495–517. https://doi.org/10.1080/10413200.2020.1843200.
Schneider JC, Hendrix-Bennett F, Beydoun HA, Johnstone B. A retrospective study of demographic, medical, and psychological predictors of readiness in service members with mild traumatic brain Injury. Mil Med. 2021;186(3–4):e401–9. https://doi.org/10.1093/milmed/usaa274.
Swedish Gambling Act SFS. 2018:1138. https://www.spelinspektionen.se/globalassets/dokument/engelsk/oversatt-spellagen/gambling-act-2018_1138-uppdate-sfs-2022_1674.pdf.
Wojtowicz M, Iverson GL, Silverberg ND, Mannix R, Zafonte R, Maxwell B, et al. Consistency of self-reported concussion history in adolescent athletes. J Neurotrauma. 2017;34(2):322–7. https://doi.org/10.1089/neu.2016.4412.
Acknowledgements
We would like to thank the principals and instructors who agreed to participate and distribute the survey, as well as the students who participated in the present study.
Funding
Open access funding provided by Lund University. This work was supported by the Skåne County Administrative Board and the Swedish Research Council for Health, Working life and Welfare (FORTE) [2021 − 01696].
Open access funding provided by Lund University.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. AH, SK, and ECK secured funding for the present project. MA, SK, and ECK were responsible for data collection. MA performed all data analyses and drafted the first version of the manuscript. All authors revised the original manuscript and have approved the submission in its current form.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for the present project was sought through the Swedish Ethical Review Authority, who came to the decision that formal ethical approval was not required because no personal identifiable data were to be collected (#DNr: 2022-04648-01, October 30th, 2022). In accordance with Swedish Law concerning the ethical review of research involving humans (2003:460 [42]), only students 15 years or older were invited to participate. Study procedures adhered to the Declaration of Helsinki and participants provided digital informed consent before proceeding to the survey.
Consent for publication
Not applicable.
Competing interests
AH receives funding from AB Svenska Spel, a Swedish state-owned gambling provider, and the state-owned alcohol monopoly, Systembolaget. Neither were involved in the planning, execution, or publication decision for this piece. The remaining authors report there are no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Andersson, M.J., Kapetanovic, S., Håkansson, A. et al. Concussion history associated with adolescent psychological distress but not hazardous gambling: a cross-sectional study. BMC Psychol 12, 329 (2024). https://doi.org/10.1186/s40359-024-01830-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40359-024-01830-6