Abstract
Background
No epidemiological data is yet available on Avoidant/Restrictive Food Intake Disorder (ARFID) in Arab countries, which may in part be due to the lack of measures available in Arabic language. This constitutes a major obstacle to further progress of our understanding of the nature, aetiology, course, treatment, and prevention of ARFID, especially as some evidence suggested that ARFID may vary across cultures and food environments. We aimed to contribute to the literature in the eating disorders field by examining the psychometric properties of an Arabic translation of the Nine Item ARFID Screen (NIAS).
Method
This was a cross-sectional, web-based study. A total of 515 Lebanese community adults (mean age of 27.55 ± 10.92 years, 69.9% females) participated. The forward–backward method was adopted to translate the NIAS from English to Arabic.
Results
Confirmatory Factor Analyses provided evidence for the adequate fit indices for the three-factor model (i.e., Picky eating, Fear, and Appetite) and the 9-item version of the NIAS. An adequate reliability of the Arabic NIAS was achieved, with McDonald’s ω ranging from .75 to .90 for the total score and all three subscores. Multi-group analyses demonstrated measurement invariance by sex (males vs. females) and weight groups (underweight/healthy weight [BMI ≤ 25] vs. overweight/obese [BMI > 25]) at the configural, metric, and scalar levels. Adequate patterns of correlations between the NIAS and measures of disordered eating symptoms, psychological distress and well-being were seen. In particular, fear was significantly associated with non-ARFID disordered eating symptoms. Appetite and Picky eating, but not Fear, were inversely correlated with well-being. All three NIAS subscores and the total score were positively correlated with psychological distress.
Conclusion
Findings provided evidence that the Arabic NIAS is a short, valid and reliable self-report measure to screen for ARFID symptoms. In light of these findings, we recommend its use for clinical and research purposes among Arabic-speaking adults.
Plain English summary
Avoidant/restrictive food intake disorder (ARFID) is an eating disorder characterized by food avoidance or dietary restriction associated with at least one of four consequences––weight loss, nutritional deficiency, nutritional supplement dependence, and/or psychosocial impairment. The Nine Item ARFID Screen (NIAS) was developed as a screening measure to detect ARFID symptoms and has nine items with three subscales that map onto symptoms of each ARFID presentation. The NIAS have been translated into multiple languages but not yet validated in Arabic. To that end, we aimed to translate and validate the Arabic version of the NIAS in the present study, which would in turn facilitate improved research and clinical practices related to ARFID in Arabic-speaking nations. The present findings provide support for the psychometric properties of the Arabic version of the NIAS in examining ARFID in Arabic-speaking adults in Lebanon.
Similar content being viewed by others
Background
Avoidant/Restrictive Food Intake Disorder (ARFID) is a debilitating eating/feeding disorder that has a broad range of presentations and can be diagnosed at any age. It has been added as a new diagnostic category to the DSM-5 [1] to identify individuals with eating problems that are not driven by distorted body image or fear of weight gain and that can cause significant impairment in psychosocial functioning. Three patterns of eating behaviours that can lead to ARFID symptoms are described: (a) avoidance of foods (e.g., fruits, vegetables, meats) based on their sensory properties (“picky” or selective/neophobic eating); (b) limited interest in eating and/or low appetite; and (c) fear of aversive consequences (e.g., vomiting, choking) from eating [2]. Accordingly, individuals diagnosed with ARFID often fail to meet appropriate energy and/or nutritional needs without the support of nutritional supplements or enteral feeding, thus exhibiting weight loss and substantial nutritional deficiencies [2]. Without an intervention, ARFID may run a chronic course [3], place a significant burden on the patient and their families, and evolve into various medical complications including bradycardia, electrolyte abnormalities, prolonged QT interval, amenorrhoea, lower bone mineral density [4, 5], scurvy [6], loss of vision [7]. Besides, ARFID cases showed high rates of current and lifetime psychiatric comorbidities, including conduct disorders, anxiety and depressive disorders, as well as bipolar-related disorders [8,9,10].
As ARFID has only recently been introduced to psychiatric nosology, very little is known about the nature of its clinical phenotypic heterogeneity [2]. This has in turn led to limited knowledge about its prevalence estimates [11], as well as the optimal approaches to diagnosis and treatment [12]. A recent systematic review [13] that included 30 studies (including 23 from Western countries) showed that prevalence estimates of ARFID in children and adolescents varied widely, ranging from 0.3 to 15.5% in non-clinical samples, 5–22.5% in clinical samples from specialised paediatric eating disorders treatment settings, and 32–64% in clinical samples from specialised tertiary care services for feeding problems. It is of note, however, that research on the epidemiology of ARFID in adult populations has been until recently “non-existent or highly inconsistent” [14]. Population‐based studies reported prevalence estimates of 0.3–4.8% in general adult populations in Western countries and South‐East Asia [15,16,17,18], and of 6.3–11% in clinical adult populations [19, 20]. The effective gathering of prevalence data has long been hindered by the lack of consistent self-report screening and assessment measures to assess ARFID eating patterns in different world languages. Having such measurement instruments is crucial for a timely detection of individuals at-risk for ARFID in clinical contexts, and for enabling to gain a clearer insight into the epidemiology of ARFID in different countries and populations.
Throughout the last few years, some research efforts have been directed at designing and validating measurement instruments that capture ARFID behavioural symptoms. A systematic review published in 2020 [12] could identify a total of four measures that showed promising psychometric properties: (1) the Eating Disturbances in Youth Questionnaire (EDY-Q) [21], (2) the Pica, ARFID and Rumination Disorder Interview (PARDI) [22] and a most updated version the PARDI ARFID Questionnaire [PARDI-AR-Q]) [23], (3) the Eating Disorder Examination (ChEDE) [24], and (4) the Nine Item Avoidant/Restrictive Food Intake Disorder Screen (NIAS) [14]. Among these measures, the NIAS is the briefest self-report measure that has been exclusively designed and validated to explicitly detect the DSM-5-based presentations of ARFID (i.e., sensory sensitivity, fear of aversive consequences, lack of interest) in a community-based adult population [14]. The NIAS demonstrated strong psychometric qualities in terms of divergent, convergent, and discriminant validity in English-speaking adults in the United States [14], in addition to valid cut-off scores to screen for ARFID with good specificity and sensitivity [25]. The NIAS has recently been selected as a recommended measure for ARFID by the International Consortium for Health Outcomes Measurement (ICHOM) [26]. Since its development in 2018, the NIAS has been translated and validated in a few other languages (including Chinese [27] and Spanish [28]) and in different populations (including transgender and non-binary youth and young adults aged 12–23 years [29]). To the best of our knowledge, no Arabic version of the NIAS exists to date. In addition, no epidemiological data is yet available on ARFID in Arab countries. This may constitute a major obstacle to further progress of our understanding of the nature, aetiology, course, treatment, and prevention of ARFID, especially as some evidence suggested that ARFID may vary across cultures and food environments [27, 30]. Therefore, existing data that mostly came from western backgrounds cannot be assumed to apply to other cultural contexts. For instance, some studies showed that ARFID in patients from Eastern backgrounds showed interesting differences in the prevalence and clinical presentation from that in samples from the West (e.g. [20, 31, 32]), which are possibly due to cross-cultural determinants.
To date, there is relatively limited research on disordered eating in Arab populations. A recent literature review on the topic indicated that about one-third of Arab females had restrained eating behaviour [33]. Some studies reported a highly unexpected prevalence of orthorexia nervosa in samples of non-clinical Arab adults [34, 35]. Additionally, cross-cultural research has shown that Arab teenagers were significantly more likely to report anorexia nervosa compared to those from Western cultures [36]. The Arabic culture is expected to shape ARFID symptom manifestations as well as the subsequent experienced problems and impairment for several reasons. The vast majority of Arab people are of Muslim faith, whereas dietary restriction and starvation that may potentially harm the human body are prohibited in Islam (e.g., “Do not throw yourselves with your own hands into destruction”; Surah Al-Baqarah 2: 195). In addition, Arab countries’ traditional social norms and values endorse overeating, as food is closely linked to social/religious events and celebrations. A main characteristic of Arab culture, i.e. hospitality toward a guest, is enacted through food-sharing rituals [37], with interactional moves of insisting and refusing being more conventionalized and more likely to occur between the host and guest in Arab cultures than in Western cultures [38]. Food is treated by Arab people “with the highest respect as it is a sacred blessing with an entrenched social, religious, and cultural meaning” [39]. As such, having ARFID-related eating restrictions in Arab culture and environment, where food plays a central role in people lives, is likely to be problematic and impairing. This underscores the strong need to provide valid and reliable measures that assess ARFID in Arabic-speaking populations. To advance our understanding of ARFID, researchers have also called for more attention to be afforded to adult populations [2] and the subclinical level [27].
For all these reasons, we sought through this study to examine the psychometric properties of an Arabic translation of the NIAS. We hypothesized that the Arabic NIAS will: (1) replicate the originally proposed three-factor structure, (2) show good composite reliability and measurement invariance by sex (males vs. females) and weight groups (underweight/healthy weight [BMI ≤ 25] vs. overweight/obese [BMI > 25]), and (3) demonstrate adequate patterns of correlations between the NIAS and measures of disordered eating symptoms, psychological distress and well-being. In particular, we expected that all three NIAS scales will be positively correlated with disordered eating symptoms. Indeed, although symptoms related to ARFID are theorized to be distinct from “traditional” disordered eating symptoms related to anorexia nervosa and bulimia nervosa [1], research has suggested a potential overlap between these two conditions [40]. ARFID symptoms have been proposed to “share endophenotypes with symptoms of other eating disorders, simultaneously increasing risk for all forms of disordered eating”, and/or “precipitate additional eating pathology” [40]. A previous psychometric study [25] demonstrated that the NIAS is an effective tool in distinguishing between individuals with ARFID and those with other eating disorders symptoms, albeit with a high overlap between the two groups on the NIAS-fear and NIAS-appetite subscales. Authors suggested that ARFID and other eating disorders appear to share transdiagnostic features [25]. Furthermore, we expected that ARFID symptoms will be positively associated with psychological distress and negatively associated with well-being. We also predicted to replicate Zickgraf and Ellis’ findings that only Appetite will be negatively related to BMI.
Methods
Translation and adaptation procedures
Before their use in the current study, the ARFID scale was translated and adapted to the Arabic language and context. To this end, it was translated to the literary Arabic language (i.e., Modern Standard Arabic), which represents the official language of all Arab countries, and is used to communicate between speakers of different groups. The purpose of achieving semantic equivalence between measures in their original and Arabic versions following international norms and recommendations [41]. For this, the forward and backward translation method was applied. The English version was translated to Arabic by a Lebanese translator who was completely unrelated to the study. Afterwards, a Lebanese psychologist with a full working proficiency in English, translated the Arabic version back to English. The translation team ensured that any specific and/or literal translation was balanced. The initial and translated English versions were compared to detect/eliminate any inconsistencies and guarantee the accuracy of the translation by a committee of experts composed of two psychiatrists and one psychologist, in addition to the research team and the two translators [42]. An adaptation of the measure to our specific context was performed, and sought to determine any misunderstanding of the items wording as well as the ease of items interpretation; and, therefore, ensure the conceptual equivalence of the original and Arabic scales in both contexts [43]. After the translation and adaptation of the scale, a pilot study was done on 30 patients to ensure all questions were well understood; no changes were applied after the pilot study.
Measures
Avoidant/Restrictive Food Intake Disorder screen (NIAS)
This scale was designed to screen for ARFID. It is composed of 9 items, scored on a 6-point Likert scale, “Strongly disagree,” “Disagree,” “Slightly disagree,” “Slightly agree,” “Agree,” and “Strongly agree” [e.g. I am a picky eater (item1); I dislike most foods that other people eat easily (item 2)] [14]. It yields three subscales composed of 3 items each as follows: Picky eating, Appetite and Fear. Higher scores indicate more avoidant/restrictive eating. Cutoff values of ≥ 10, ≥ 9, and/or ≥ 10 have been proposed for capturing individuals who fit the NIAS dimensions Picky eating, Appetite, and Fear, respectively [25].
Eating Attitude Test (EAT-7)
This scale is the Arabic shortened version of the Eating Attitude Test-26 (EAT-26) [44, 45]. It is composed of 7 items scored on a 6-point Likert scale [46] [e.g. Aware of the energy content of foods that I eat (item2); Avoid foods with sugar in them (item 5)]. Higher scores reflect more severe disordered eating symptoms related to anorexia nervosa and bulimia nervosa (ω = 0.84).
Depression anxiety and stress scale-8 items (DASS-8)
Validated in Arabic [47], this scale is composed of 8 items that measure depression (3 items), anxiety (3 items) and stress (2 items) [e.g. I felt that I was using a lot of nervous energy (item 1); I felt down-hearted and blue (item 5)]. Questions are rated on a 4-point Likert scale (“0 = does not apply to me to “3 = always applies to me”). Higher scores reflect more psychological distress (ω = 0.89).
WHO-wellbeing scale
Validated in Arabic [48, 49], this scale is composed of 5 items [e.g. I have felt cheerful in good spirit, in the last 2 weeks (item 1)], scored on a 6-point Likert scale (“0 = at none time to 5 = all of time”), with higher scores reflecting better wellbeing [50] (ω = 0.93).
Demographics
Participants were asked to provide their demographic details consisting of age, sex, and education level. Weight and height were self-reported by participants to calculate the Body Mass Index (BMI); the latter was later subdivided into underweight/normal (Body Mass Index [BMI] ≤ 25) and overweight/obese (BMI > 25) [51].
Procedures
All data were collected via a Google Forms link; the sample was recruited conveniently between February and March 2023. The survey link was sent using social media applications (WhatsApp, Instagram, Messenger) and included an estimated duration. Inclusion criteria for participation included: (1) being of a resident and citizen of Lebanon, (2) aged 18 years and above, (3) having access to the Internet, and (4) willing to participate in the study. Excluded were those who refused to fill out the questionnaire. Internet protocol (IP) addresses were examined to ensure that no participant took the survey more than once. After providing digital informed consent, participants were asked to complete the instruments described above, which were presented in a pre-randomised order to control for order effects. The survey was anonymous and participants completed the survey voluntarily and without remuneration, in approximately 20 min on average [52].
Analytic strategy
Confirmatory factor analysis (CFA)
There were no missing responses in the dataset. We used data from the total sample to conduct a CFA using the SPSS AMOS v.29 software. As a rule of thumb, simulation studies show that with normally distributed indicator variables and no missing data, a reasonable sample size for a simple confirmatory factor analysis model is about N = 150 [53], which was exceeded in our sample. Our intention was to test the original model of the ARFID scale (i.e., three-factor model). Parameter estimates were obtained using the maximum likelihood method and fit indices. For this purpose, the normed model chi-square (χ2/df), the Steiger-Lind root mean square error of approximation (RMSEA), the Tucker-Lewis Index (TLI) and the comparative fit index (CFI). Values ≤ 5 for χ2/df, and ≤ 0.05 for RMSEA, and 0.95 for CFI and TLI indicate good fit of the model to the data [54]. Additionally, evidence of convergent validity was assessed in this subsample using the Fornell-Larcker criterion, with average variance extracted (AVE) values of ≥ 0.50 considered adequate [55]. The absence of multicollinearity was verified through tolerance values > 0.2 and variance inflation factor (VIF) values < 5. Multivariate normality was not verified at first (Bollen-Stine bootstrap p = 0.002); therefore, we performed non-parametric bootstrap** procedure (available in AMOS).
Sex and weight invariance
To examine sex and weight invariance of ARFID scores, we conducted multi-group CFA [56] using the total sample. Measurement invariance was assessed at the configural, metric, and scalar levels [57]. Following the recommendations of Cheung and Rensvold [58] and Chen [56], we accepted ΔCFI ≤ 0.010 and ΔRMSEA ≤ 0.015 or ΔSRMR ≤ 0.010 (0.030 for factorial invariance) as evidence of invariance. The Student t test was used to compare two means in case of evidence of measurement invariance.
Further analyses
Composite reliability in both subsamples was assessed using McDonald’s ω, with values greater than 0.70 reflecting adequate composite reliability [59]. McDonald’s ω was selected as a measure of composite reliability because of known problems with the use of Cronbach’s α (e.g., [60]). The social support total score was considered normally distributed since the skewness (= 0.406) and kurtosis (= − 0.270) values varied between ± 1 [61]. We examined bivariate correlations between the ARFID and the DASS-8 and WHO-5 using the Pearson test. Based on Cohen [62], values ≤ 0.10 were considered weak, ~ 0.30 were considered moderate, and ~ 0.50 were considered strong correlations.
Results
Participants
Five hundred fifteen participants participated in this study, with a mean age of 27.55 ± 10.92 years, 69.9% females and 83.7% with a university level of education. Moreover, the mean BMI was 24.27 ± 4.54 kg/m2; 189 (36.7%) were overweight/obese. Moreover, 56 (10.9%) had NIAS-picky eating scores ≥ 10, 112 (21.7%) NIAS-appetite scores ≥ 9 and 49 (9.5%) NIAS-fear scores ≥ 10. Finally, 17 (3.3%) had positive screen on any NIAS subscale (≥ 10 NIAS-picky eating, ≥ 9 NIAS-appetite, and ≥ 10 NIAS-fear).
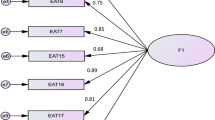
Confirmatory factor analysis of the ARFID scale
CFA indicated that fit of the three-factor model of the ARFID scale was acceptable: χ2 = 75.55, df = 24 (p < 0.001), RMSEA = 0.065 (90% CI 0.049, 0.081), SRMR = 0.036, CFI = 0.978, TLI = 0.967. The standardised estimates of factor loadings were all adequate (see Table 1). The convergent validity for this model was good, as AVE = 0.61.
Measurement invariance
As reported in Table 2, all indices suggested that configural, metric, and scalar invariance was supported across sex and weight. The results showed that there was no statistically significant difference between males and females in all ARFID dimensions. Furthermore, no significant difference was found between participants with underweight/healthy weight vs overweight/obese except for the appetite subscale score where non-overweight participants scored higher than those who are overweight/obese (Table 3).
Composite reliability
Composite reliability of scores was adequate in the total sample for the ARFID total scale (ω = 0.88), picky eating (ω = 0.75), appetite (ω = 0.80) and fear (ω = 0.90) subscales.
Associations of NIAS with other measures
Higher NIAS scores and sub-scores were significantly correlated with higher psychological distress, lower wellbeing. The NIAS fear subscale was significantly associated with more disordered eating as measured by the EAT-7 (Table 4).
Discussion
No data exists to date on ARFID in Arab countries, which may in part be due to the lack of measures available in Arabic language. We aimed to contribute to the literature in the eating disorders field by validating the Arabic version of the NIAS in a sample of non-clinical Arabic-speaking adults (N = 515) from Lebanon. As expected, analyses revealed that the Arabic NIAS yielded a three-factor solution, which showed excellent levels of reliability. In addition, the Arabic NIAS demonstrated measurement invariance across gender and BMI, as well as good correlations with the other measures. In light of these findings, we recommend its use among Arabic-speaking adults. Offering this psychometrically sound Arabic version of the NIAS may help to provide accurate epidemiological data on ARFID in Arab countries, increase the awareness of ARFID screening and diagnosis in Arab settings, and inform the development of culturally-tailored, evidence‐informed interventions.
CFA provided evidence for the adequate fit indices for the three-factor model (i.e., Picky eating, Fear, and Appetite) and the 9-item version of the NIAS, which further supports the DSM-5-oriented ARFID subdomains proposed in the original scale [2]. Other linguistic validations of the NIAS, including the Chinese version [27] in college students and the Spanish version [28] in a Mexican adolescent and young adult population. More recently, Zickgraf et al. [29] could also replicate the original factorial structure in English-speaking sexual minority youth. Furthermore, an adequate reliability of the Arabic NIAS was achieved, with McDonald’s ω ranging from 0.75 to 0.90 for the total score and all three subscores. Similarly, a good reliability of the NIAS was demonstrated in the original [14] and subsequent validations (e.g., Cronbach’s α of 0.73–0.86 in Chinese college students [27], McDonald’s ω of 0.70–0.90 in Mexican youth [28]).
Another finding of our study is that the factor loadings of the Arabic NIAS remained invariant by gender and weight groups at the three levels (configural, metric, and scalar). Evidence for invariance reflects that across-group comparisons of NIAS subscale means is valid. In other words, individuals of both genders and different weight groups understand and interpret the meaning of NIAS items in the same way. In line with our findings, Medina‐Tepal et al. [28] provided evidence supporting measurement invariance across sex. Between-sex comparisons revealed no statistically significant differences in all three ARFID presentations in our sample. The previous literature on sex difference in ARFID manifestations has yielded conflicting results. In Chinese college students, no significant sex differences were found except for the subscale “Appetite”, with males scoring significantly higher than females [27]. In American transgender and non-binary youth, assigned females at birth displayed greater scores in Fear and Appetite subscales than assigned males at birth [29]. Previous data in children and adolescent samples also showed mixed results, with rates of ARFID being higher either in males [63,64,65] or females [66,67,68]. As for comparisons across weight groups, findings showed no significant differences between individuals belonging to underweight/healthy weight and overweight/obese groups, except for Appetite scores which were lower in the latter group. These findings were expected, and were consistent with those of the original validation study [14], thus suggesting that the NIAS captures eating behavioural patterns related to significant and/or prolonged inadequate intake which ultimately results in weight loss or lack of weight gain. Different findings were reported by He et al. [27], who found that underweight Chinese students exhibited significantly higher scores in Appetite, Picky eating and NIAS total scores. These differences were explained by cultural factors, as authors suggested that adult picky eating might have protective effect against overweight/obesity in China, a cultural context where there is lower prevalence of and fewer environmental contributors to overweight/obesity than Western contexts (e.g., the United states [US]) [27]. All these controversial data indicate the need for more investigations of ARFID characteristics across sex and weight groups in different settings and countries.
Similar to the original validation [14], we used the EAT as a measure of non-ARFID disordered eating to explore divergent validity. Findings indicated that only Fear was significantly associated with disordered eating symptoms. It is of note that there is scant research to date on how disordered eating (such as anorexia nervosa, bulimia nervosa and binge eating) relates to ARFID symptoms. Some evidence suggests that picky eaters are at an increased risk of develo** anorexia nervosa [69], although a lack of association between the two entities has also been observed [70]. In the original validation study, the NIAS Fear and Picky eating (but not Appetite) subscores were independently correlated with EAT-26 scores [14]. A positive relationship between picky eating and disordered eating symptoms has also been previously observed among adults (e.g. [71, 72]). Burton Murray et al. [25] also found a significant overlap between ARFID and traditional eating disorders symptoms related to anorexia nervosa and bulimia nervosa, as these two disorders involve shared manifestations. Indeed, the ARFID Fear of aversive consequences may share overlap** presentations with other disordered eating symptoms, as both often include gastrointestinal symptoms [19, 73].
Our findings also revealed that Appetite and Picky eating, but not Fear were inversely correlated with well-being. In addition, all three NIAS subscores and the total score were positively correlated with psychological distress. Consistently, Zickgraf and Ellis [14] found a positive association between Fear and anxiety as well as between Appetite and depression in the US validation sample. He et al. [27] showed that Fear and Appetite were each independently associated with psychological distress in the Chinese validation sample. The lack of significant correlation between Fear and well-being in our sample may be partly explained by cultural factors. The way how individuals perceive aversive consequences of eating (such as vomiting or choking) may be influenced by cultural factors, and can therefore differently affect well-being across cultural backgrounds. In collectivistic cultures, such as Arab countries, somatic symptoms seem to reflect a “constructive response” to distress; where, generally, individuals “explicitly exhibit somatization in response to life stressors” [74]. Indeed, the prevalence of medically unexplained somatic symptoms is consistently reported to be higher in Arab people than globally, with gastrointestinal symptoms being among the most commonly reported [75].
Study limitations and research perspectives
Certain limitations should be considered when interpreting the findings and conclusions of this study. Our data were gathered using a convenience (non-probabilistic) and web-based sampling methods, which may limit the generalization of the present findings. We did not implement practices to ensure the integrity of the data (embedding attention checks throughout the survey) and did not have the option to check the response time of participants with Google forms. In addition, we used a self-report survey, meaning the answers could be affected by recall or social desirability biases. Another limitation is that our sample was disproportionate in terms of sex and educational levels (with the majority of participants being females of a high educational level), which may have impacted the findings. Also, our study relied on an adult non-clinical sample to validate the NIAS. Additional studies are required to test its psychometric properties in clinical samples (e.g., patients with eating disorders) and across the lifespan. As cross-national cultural differences may also exist between Arab countries, one should be cautious in generalizing the findings to the broader Arabic-speaking community in other parts of the world. To address this limitation, future validations in contexts other than Lebanon are needed to further confirm the robustness of the scale across various Arab backgrounds. Other important psychometric characteristics of the NIAS (e.g., test–retest reliability) have not been explored in the present study, and still need to be considered in future studies. Finally, further research still needs to identify clinical cut-offs on the Arabic NIAS, in order to enable to define individuals at-risk for ARFID and determine prevalence rates of ARFID in Arab populations.
Conclusion
The present study is the first to investigate ARFID symptoms in an Arab population from a develo** country of the Middle East and North Africa (MENA) region. Findings provided evidence that the Arabic NIAS is a short, valid and reliable self-report measure to screen for ARFID among Arabic-speaking adults from the general population. Pending larger scale studies in other settings, countries and age groups, we recommend its use to screen for ARFID symptoms, at least among Arabic-speaking adults in non-clinical settings and the Lebanese context. We hope that by providing a psychometrically sound Arabic version of the NIAS we can aid in fostering cross-cultural research on ARFID by including under-represented populations from non-Western non-developed countries, and furthering the understanding of this new diagnostic entity.
Availability of data and materials
All data generated or analyzed during this study are not publicly available due the restrictions from the ethics committee, but are available upon a reasonable request from the corresponding author (SH).
References
Association AP. Diagnostic and statistical manual of mental disorders: DSM-5. 2013. Washington, DC: American psychiatric association; 2013.
Strand M, von Hausswolff-Juhlin Y, Welch E. A systematic sco** review of diagnostic validity in avoidant/restrictive food intake disorder. Int J Eat Disord. 2019;52(4):331–60.
Thomas JJ, et al. Avoidant/restrictive food intake disorder: a three-dimensional model of neurobiology with implications for etiology and treatment. Curr Psychiatry Rep. 2017;19:1–9.
Alberts Z, et al. Bone mineral density in anorexia nervosa versus avoidant restrictive food intake disorder. Bone. 2020;134: 115307.
Katzman DK, Norris ML, Zucker N. Avoidant restrictive food intake disorder. Psychiatr Clin. 2019;42(1):45–57.
Sharp WG, et al. Scurvy as a sequela of avoidant-restrictive food intake disorder in autism: a systematic review. J Dev Behav Pediatr. 2020;41(5):397–405.
Chiarello F, et al. Optic neuropathy due to nutritional deficiency in a male adolescent with Avoidant/Restrictive Food Intake Disorder: a case report. Eat Weight Disord Stud Anorex Bulim Obes. 2018;23:533–5.
Kambanis PE, et al. Prevalence and correlates of psychiatric comorbidities in children and adolescents with full and subthreshold avoidant/restrictive food intake disorder. Int J Eat Disord. 2020;53(2):256–65.
Cooney M, et al. Clinical and psychological features of children and adolescents diagnosed with avoidant/restrictive food intake disorder in a pediatric tertiary care eating disorder program: a descriptive study. J Eat Disord. 2018;6:7.
Bryson AE, Scipioni AM, Ornstein RM. Avoidant/restrictive food intake disorder: categorization of subtypes and longitudinal outcomes after day hospitalization. J Adolesc Health. 2017;60(2):S45–6.
Bryant-Waugh R. Avoidant/restrictive food intake disorder. Child Adolesc Psychiatr Clin. 2019;28(4):557–65.
Bourne L, et al. Avoidant/restrictive food intake disorder: a systematic sco** review of the current literature. Psychiatry Res. 2020;288: 112961.
Sanchez-Cerezo J, et al. What do we know about the epidemiology of avoidant/restrictive food intake disorder in children and adolescents? A systematic review of the literature. Eur Eat Disord Rev. 2023;31(2):226–46.
Zickgraf HF, Ellis JM. Initial validation of the Nine Item Avoidant/Restrictive Food Intake disorder screen (NIAS): a measure of three restrictive eating patterns. Appetite. 2018;123:32–42.
Fitzsimmons-Craft EE, et al. Results of disseminating an online screen for eating disorders across the US: reach, respondent characteristics, and unmet treatment need. Int J Eat Disord. 2019;52(6):721–9.
Hilbert A, et al. Psychometric evaluation of the Eating Disorders in Youth-Questionnaire when used in adults: prevalence estimates for symptoms of avoidant/restrictive food intake disorder and population norms. Int J Eat Disord. 2021;54(3):399–408.
Chua SN, et al. Estimated prevalence of eating disorders in Malaysia based on a diagnostic screen. Int J Eat Disord. 2022;55(6):763–75.
Hay P, et al. Burden and health-related quality of life of eating disorders, including Avoidant/Restrictive Food Intake Disorder (ARFID), in the Australian population. J Eat Disord. 2017;5(1):1–10.
Murray HB, et al. Prevalence and characteristics of avoidant/restrictive food intake disorder in adult neurogastroenterology patients. Clin Gastroenterol Hepatol. 2020;18(9):1995–2002.
Nakai Y, et al. Clinical presentation and outcome of avoidant/restrictive food intake disorder in a Japanese sample. Eat Behav. 2017;24:49–53.
Kurz S, et al. Early-onset restrictive eating disturbances in primary school boys and girls. Eur Child Adolesc Psychiatry. 2015;24:779–85.
Bryant-Waugh R, et al. Development of the Pica, ARFID, and Rumination Disorder Interview, a multi-informant, semi-structured interview of feeding disorders across the lifespan: a pilot study for ages 10–22. Int J Eat Disord. 2019;52(4):378–87.
Bryant-Waugh R, et al. Preliminary validation of the pica, ARFID and rumination disorder interview ARFID questionnaire (PARDI-AR-Q). J Eat Disord. 2022;10(1):179.
Schmidt R, et al. Interview-based assessment of avoidant/restrictive food intake disorder (ARFID): a pilot study evaluating an ARFID module for the eating disorder examination. Int J Eat Disord. 2019;52(4):388–97.
Burton Murray H, et al. Validation of the nine item ARFID screen (NIAS) subscales for distinguishing ARFID presentations and screening for ARFID. Int J Eat Disord. 2021;54(10):1782–92.
ICHOM. Eating disorders data collection reference guide. 2022.
He J, et al. Chinese version of the nine item ARFID screen: psychometric properties and cross-cultural measurement invariance. Assessment. 2020;28(2):537–50.
Medina-Tepal KA, et al. Cross-cultural adaptation and validation of the Nine Item ARFID Screen (NIAS) in Mexican youths. Int J Eat Disord. 2022;56:721–6.
Zickgraf HF, et al. Validation of the nine-item avoidant/restrictive food intake disorder screen among transgender and nonbinary youth and young adults. Transgender Health. 2023;8(2):159–67.
Schermbrucker J, et al. Avoidant/restrictive food intake disorder in an 11-year old South American boy: medical and cultural challenges. J Can Acad Child Adolesc Psychiatry/Journal de l’Académie canadienne de psychiatrie de l’enfant et de l’adolescent. 2017;26:110.
Nakai Y, et al. Characteristics of avoidant/restrictive food intake disorder in a cohort of adult patients. Eur Eat Disord Rev. 2016;24(6):528–30.
Zickgraf HF, et al. Characteristics of outpatients diagnosed with the selective/neophobic presentation of avoidant/restrictive food intake disorder. Int J Eat Disord. 2019;52(4):367–77.
Melisse B, de Beurs E, van Furth EF. Eating disorders in the Arab world: a literature review. J Eat Disord. 2020;8(1):1–19.
Haddad C, et al. Correlates of orthorexia nervosa among a representative sample of the Lebanese population. Eat Weight Disord. 2019;24(3):481–93.
Farchakh Y, Hallit S, Soufia M. Association between orthorexia nervosa, eating attitudes and anxiety among medical students in Lebanese universities: results of a cross-sectional study. Eat Weight Disord. 2019;24(4):683–91.
Al-Adawi S, et al. Presence and severity of anorexia and bulimia among male and female Omani and non-Omani adolescents. J Am Acad Child Adolesc Psychiatry. 2002;41(9):1124–30.
Sobh R et al. Home and commercial hospitality rituals in Arab Gulf countries. ACR North American Advances; 2012.
Grainger K, et al. Offering and hospitality in Arabic and English. J Politeness Res. 2015;11(1):41–70.
Chammas G, Yehya NA. Lebanese meal management practices and cultural constructions of food waste. Appetite. 2020;155: 104803.
Becker KR, et al. Co-occurrence of avoidant/restrictive food intake disorder and traditional eating psychopathology. J Am Acad Child Adolesc Psychiatry. 2020;59(2):209–12.
Van Widenfelt BM, et al. Translation and cross-cultural adaptation of assessment instruments used in psychological research with children and families. Clin Child Fam Psychol Rev. 2005;8(2):135–47.
Fenn J, Tan C-S, George S. Development, validation and translation of psychological tests. BJPsych Adv. 2020;26(5):306–15.
Ambuehl B, Inauen J. Contextualized measurement scale adaptation: a 4-step tutorial for health psychology research. Int J Environ Res Public Health. 2022;19(19):12775.
Haddad C, et al. Validation of the Arabic version of the Eating Attitude Test in Lebanon: a population study. Public Health Nutr. 2021;24(13):4132–43.
Garner DM, Garfinkel PE. The eating attitudes test: an index of the symptoms of anorexia nervosa. Psychol Med. 1979;9(2):273–9.
Fekih-Romdhane F, et al. Validation of a shortened version of the Eating Attitude Test (EAT-7) in the Arabic language. J Eat Disord. 2022;10(1):127.
Ali AM, et al. The Depression Anxiety Stress Scale 8-items expresses robust psychometric properties as an ideal shorter version of the Depression Anxiety Stress Scale 21 among healthy respondents from three continents. Front Psychol. 2022;13: 799769.
Fekih-Romdhane F et al. Cross-country validation of the Arabic version of the WHO-5 well-being index in non-clinical young adults from six Arab countries. 2023.
Sibai AM, et al. Validation of the Arabic version of the 5-item WHO Well Being Index in elderly population. Int J Geriatr Psychiatry. 2009;24(1):106–7.
Heun R, et al. Internal and external validity of the WHO Well-Being Scale in the elderly general population. Acta Psychiatr Scand. 1999;99(3):171–8.
World Health Organization. Body mass index (BMI). https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/body-mass-index
Swami V, et al. Psychometric properties of an Arabic translation of the Functionality Appreciation Scale (FAS) in Lebanese adults. Body Image. 2022;42:361–9.
Muthén LK, Muthén BO. How to use a Monte Carlo study to decide on sample size and determine power. Struct Equ Model. 2002;9(4):599–620.
Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. 1999;6(1):1–55.
Malhotra N, Dash S. Marketing research: an applied orientation. Delhi: Pearson, Ed.; 2011.
Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equ Model. 2007;14(3):464–504.
Vadenberg R, Lance C. A review and synthesis of the measurement in variance literature: suggestions, practices, and recommendations for organizational research. Organ Res Methods. 2000;3:4–70.
Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Model. 2002;9(2):233–55.
Dunn TJ, Baguley T, Brunsden V. From alpha to omega: a practical solution to the pervasive problem of internal consistency estimation. Br J Psychol. 2014;105(3):399–412.
McNeish D. Thanks coefficient alpha, we’ll take it from here. Psychol Methods. 2018;23(3):412.
Hair JF Jr, et al. Advanced issues in partial least squares structural equation modeling. Sage publications; 2017.
Cohen J. Quantitative methods in psychology: a power primer. In: Psychological bulletin. 1992. Citeseer.
Eddy KT, et al. Prevalence of DSM-5 avoidant/restrictive food intake disorder in a pediatric gastroenterology healthcare network. Int J Eat Disord. 2015;48(5):464–70.
Norris ML, et al. Exploring avoidant/restrictive food intake disorder in eating disordered patients: a descriptive study. Int J Eat Disord. 2014;47(5):495–9.
Nicely TA, et al. Prevalence and characteristics of avoidant/restrictive food intake disorder in a cohort of young patients in day treatment for eating disorders. J Eat Disord. 2014;2(1):1–8.
Fisher MM, et al. Characteristics of avoidant/restrictive food intake disorder in children and adolescents: a “new disorder” in DSM-5. J Adolesc Health. 2014;55(1):49–52.
Katzman DK, et al. Incidence and age-and sex-specific differences in the clinical presentation of children and adolescents with avoidant restrictive food intake disorder. JAMA Pediatr. 2021;175(12):e213861–e213861.
Wong L, Goh LG, Ramachandran R. Evolution of paediatric eating disorders in Singapore: a historical cohort study. Arch Dis Child. 2022;107(11):1046–8.
Marchi M, Cohen P. Early childhood eating behaviors and adolescent eating disorders. J Am Acad Child Adolesc Psychiatry. 1990;29(1):112–7.
Kotler LA, et al. Longitudinal relationships between childhood, adolescent, and adult eating disorders. J Am Acad Child Adolesc Psychiatry. 2001;40(12):1434–40.
Ellis JM, et al. Recollections of pressure to eat during childhood, but not picky eating, predict young adult eating behavior. Appetite. 2016;97:58–63.
Kauer J, et al. Adult picky eating. Phenomenology, taste sensitivity, and psychological correlates. Appetite. 2015;90:219–28.
Burton Murray H, et al. Avoidant/restrictive food intake disorder symptoms are frequent in patients presenting for symptoms of gastroparesis. Neurogastroenterol Motil. 2020;32(12): e13931.
El Halabi S, Founouni, ZN, Arawi T. Social construction of Arab masculinity and its effects on mental health. In: Handbook of healthcare in the Arab World. Springer. p. 3295–3305; 2021.
Okasha A, Okasha T. Somatoform disorders—an Arab perspective. In: Somatoform disorders: a worldwide perspective. Springer; 1999.
Acknowledgements
The authors would like to thank all participants.
Funding
None.
Author information
Authors and Affiliations
Contributions
FFR, SO and SH designed the study; FFR drafted the manuscript; SH carried out the analysis and interpreted the results; FS, MD and DM collected the data. RH and TS reviewed the paper for intellectual content; all authors reviewed the final manuscript and gave their consent.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethics approval for this study was obtained from the ethics committee of the School of Pharmacy at the Lebanese International University (2023RC-014-LIUSOP). Written informed consent was obtained from all subjects; the online submission of the soft copy was considered equivalent to receiving a written informed consent. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fekih-Romdhane, F., Hallit, R., Malaeb, D. et al. Psychometric properties of an Arabic translation of the Nine Item Avoidant/Restrictive Food Intake Disorder Screen (NIAS) in a community sample of adults. J Eat Disord 11, 143 (2023). https://doi.org/10.1186/s40337-023-00874-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40337-023-00874-0