Abstract
Background
Reliable biomarkers of frontotemporal dementia (FTD) are currently lacking. FTD may be associated with chronic immune dysfunction, microglial activation and raised inflammatory markers, particularly in progranulin (GRN) mutation carriers. Levels of soluble triggering receptor expressed on myeloid cells 2 (sTREM2) are elevated in Alzheimer’s disease (AD), but they have not been fully explored in FTD.
Methods
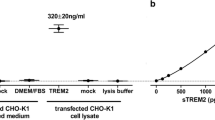
We investigated whether cerebrospinal fluid (CSF) sTREM2 levels differ between FTD and controls, across different clinical and genetic subtypes of FTD, or between individuals with FTD due to AD versus non-AD pathology (based on CSF neurodegenerative biomarkers). We also assessed relationships between CSF sTREM2 and other CSF biomarkers (total tau [T-tau], tau phosphorylated at position threonine-181 [P-tau] and β-amyloid 1–42 [Aβ42]) and age and disease duration. Biomarker levels were measured using immunoassays in 17 healthy controls and 64 patients with FTD (behavioural variant FTD, n = 20; primary progressive aphasia, n = 44). Ten of 64 had familial FTD, with mutations in GRN (n = 3), MAPT (n = 4), or C9orf72 (n = 3). Fifteen of 64 had neurodegenerative biomarkers consistent with AD pathology (11 of whom had logopenic variant PPA). Levels were compared using multivariable linear regressions.
Results
CSF sTREM2 levels did not differ between FTD and controls or between clinical subgroups. However, GRN mutation carriers had higher levels than controls (mean ([SD] = 9.7 [2.9] vs. 6.8 [1.6] ng/ml; P = 0.028) and MAPT (3.9 [1.5] ng/ml; P = 0.003] or C9orf72 [4.6 [1.8] ng/ml; P = 0.006) mutation carriers. Individuals with AD-like CSF had higher sTREM2 levels than those with non-AD-like CSF (9.0 [3.6] vs. 6.9 [3.0] ng/ml; P = 0.029). CSF sTREM2 levels were associated with T-tau levels in control and FTD groups and also with P-tau in those with FTD and AD-like CSF. CSF sTREM2 levels were influenced by both age and disease duration in FTD.
Conclusions
Although CSF sTREM2 levels are not raised in FTD overall or in a particular clinical subtype of FTD, levels are raised in familial FTD associated with GRN mutations and in FTD syndromes due to AD pathology. Because CSF sTREM2 levels correlate with a marker of neuronal injury (T-tau), sTREM2 should be explored as a biomarker of disease intensity in future longitudinal studies of FTD.
Similar content being viewed by others
Background
Frontotemporal dementia (FTD) is a common cause of early-onset dementia, presenting with behavioural change (behavioural variant FTD [bvFTD]) or language impairment (primary progressive aphasia [PPA]). Around one-third of cases are familial, associated most commonly with mutations in progranulin (GRN), microtubule-associated protein tau (MAPT) or chromosome 9 open reading frame 72 (C9orf72) [1]. Pathologically, the majority of individuals have frontotemporal lobar degeneration (FTLD) with inclusions containing tau or transactive response DNA binding protein 43 (TDP-43), although some, particularly those with the logopenic variant of PPA (lvPPA), have Alzheimer’s disease (AD) pathology [2]. Reliable biomarkers that differentiate the pathological changes underlying sporadic FTD in vivo or that predict disease onset, severity or progression in sporadic and familial FTD are currently lacking. There is growing evidence that neuroinflammation and microglial dysfunction play a role in FTD, particularly in familial FTD secondary to GRN mutations [3, 4]. Inflammatory markers are variably altered in blood or cerebrospinal fluid (CSF) of patients with neurodegenerative disease, including across the clinical, genetic and pathological spectrum of FTD, and they could be useful as disease biomarkers in future clinical trials.
The protein triggering receptor expressed on myeloid cells 2 (TREM2) is an innate immune receptor expressed on microglia and on myeloid cells outside the brain [5, 6]. TREM2 is upregulated on activated microglia and involved in microglial phagocytosis [7,8,9,21, 23,24,25], although significantly higher levels [22] or a trend towards higher levels [26] have been observed in males. Although it remains unclear whether sex affects sTREM2, we adjusted all analyses for sex.
A limitation of our study is that some of the FTD clinical and genetic subgroups were rather small, which may have limited our power to detect significant differences between groups. However, this is inherent to a disease such as FTD, where rarer subtypes exist, and it is difficult to avoid when analysing biomarker levels across a broad clinical and pathological spectrum of disease and when employing CSF collection and biomarker analysis at one centre in order to minimise inter-centre variation. Other studies with multi-centre CSF sources have shown significant variability in sTREM2 levels between centres [25], which we were keen to avoid. Our dementia group contained individuals with a diagnosis of an FTD syndrome, including those typically associated with FTLD-TDP or FTLD-tau (bvFTD, svPPA and nfvPPA) and those associated with AD pathology (lvPPA), which in theory could have differentially affected sTREM2 levels within the group as a whole. However, we were able to dissect out any differences in sTREM2 linked to differing pathologies through stratification of all patients with dementia by their CSF biomarker profile. Although most cases of dementia were not pathologically confirmed, all met recent diagnostic criteria for bvFTD [27] or PPA [28], and our CSF ratio cut-off was intentionally stringent to minimise misclassification of cases into the wrong pathology subgroup. Our dementia group combined individuals with a wide range of disease durations, which we showed was independently associated with sTREM2 levels. However, we adjusted analyses for disease duration wherever possible to account for this. We did not include any individuals with mild cognitive impairment, because this is typically a ‘pre-AD’ rather than a ‘pre-FTD’ state, nor did we analyse longitudinal CSF samples or samples from pre-symptomatic mutation carriers at risk of familial FTD. This means we cannot definitively conclude whether CSF sTREM2 levels change over the disease course, and therefore reflect disease proximity, intensity or progression in FTD, or how sTREM2 relates to changes in other CSF biomarkers such as T-tau over time.
Conclusions
Although CSF sTREM2 does not seem useful for differentiating between individuals with FTD and healthy controls, or for delineating a particular clinical subtype of FTD, levels are higher in familial FTD associated with GRN mutations (albeit within a small preliminary cohort) and in individuals with a clinical syndrome consistent with FTD but underlying AD, rather than FTLD, pathology. Because CSF sTREM2 levels correlate with a measure of neuronal injury (T-tau), they may reflect disease intensity in FTD, but this requires further exploration.
Future studies should analyse CSF sTREM2 levels within larger cohorts of individuals with FTD, across a variety of clearly defined clinical subgroups, and ideally in pathologically confirmed cases. Inclusion of a larger number of familial FTD cases with mutations in GRN, MAPT and C9orf72 (which have known pathology) would be helpful in this regard and would enable confirmation of our preliminary observations of higher levels in symptomatic GRN mutation carriers. Assessment of CSF sTREM2 levels in pre-symptomatic individuals at risk of familial FTD could establish if and when levels change prior to expected symptom onset. This would help to elucidate whether CSF sTREM2 levels may be useful as a biomarker of disease proximity in FTD, which, if validated, may be useful for guiding timely initiation of treatments or assessing treatment response in clinical trials. This would maximise the chance of benefitting individuals before significant neurodegeneration occurs. Exploration of relationships between baseline and longitudinal measurements of CSF sTREM2 levels and other markers of disease intensity (such as serum or CSF neurofilament light levels or frontal lobe atrophy rate) would also enable determination of whether CSF sTREM2 can be used as a biomarker of disease intensity in sporadic or familial FTD.
Abbreviations
- Aβ42:
-
β-Amyloid 1–42
- AD:
-
Alzheimer’s disease
- BSA:
-
Bovine serum albumin
- bvFTD:
-
Behavioural variant frontotemporal dementia
- C9orf72 :
-
Chromosome 9 open reading frame 72 (gene)
- CSF:
-
Cerebrospinal fluid
- FTD:
-
Frontotemporal dementia
- FTLD:
-
Frontotemporal lobar degeneration
- GRN :
-
Progranulin (gene)
- lvPPA:
-
Logopenic variant primary progressive aphasia
- MAPT :
-
Microtubule-associated protein tau (gene)
- nfvPPA:
-
Non-fluent variant primary progressive aphasia
- PPA:
-
Primary progressive aphasia
- PPA-NOS:
-
Primary progressive aphasia not otherwise specified
- P-tau:
-
tau phosphorylated at position threonine-181
- sTREM2:
-
soluble triggering receptor expressed on myeloid cells 2
- svPPA:
-
Semantic variant primary progressive aphasia
- TDP-43:
-
Transactive DNA response binding protein 43
- TREM2:
-
Triggering receptor expressed on myeloid cells 2
- T-tau:
-
Total tau
References
Woollacott IOC, Rohrer JD. The clinical spectrum of sporadic and familial forms of frontotemporal dementia. J Neurochem. 2016;138(Suppl.1):6–31.
Lashley T, Rohrer JD, Mead S, Revesz T. Review: an update on clinical, genetic and pathological aspects of frontotemporal lobar degenerations. Neuropathol Appl Neurobiol. 2015;41:858–81.
Lui H, Zhang J, Makinson SR, Cahill MK, Kelley KW, Huang HY, et al. Progranulin deficiency promotes circuit-specific synaptic pruning by microglia via complement activation. Cell. 2016;165:921–35.
Chitramuthu BP, Bennett HPJ, Bateman A. Progranulin: a new avenue towards the understanding and treatment of neurodegenerative disease. Brain. 2017;140(12):3081–104.
Schmid CD, Sautkulis LN, Danielson PE, Cooper J, Hasel KW, Hilbush BS, et al. Heterogeneous expression of the triggering receptor expressed on myeloid cells-2 on adult murine microglia. J Neurochem. 2002;83:1309–20.
Hickman SE, Kingery ND, Ohsumi TK, Borowsky ML, Wang L, Means TK, et al. The microglial sensome revealed by direct RNA sequencing. Nat Neurosci. 2013;16:1896–905.
Takahashi K, Rochford CDP, Neumann H. Clearance of apoptotic neurons without inflammation by microglial triggering receptor expressed on myeloid cells-2. J Exp Med. 2005;201:647–57.
N’Diaye EN, Branda CS, Branda SS, Nevarez L, Colonna M, Lowell C, et al. TREM-2 (triggering receptor expressed on myeloid cells 2) is a phagocytic receptor for bacteria. J Cell Biol. 2009;184:215–23.
Kleinberger G, Yamanishi Y, Suarez-Calvet M, Czirr E, Lohmann E, Cuyvers E, et al. TREM2 mutations implicated in neurodegeneration impair cell surface transport and phagocytosis. Sci Transl Med. 2014;6:243ra86.
Kleinberger G, Brendel M, Mracsko E, Wefers B, Groeneweg L, **ang X, et al. The FTD-like syndrome causing TREM2 T66M mutation impairs microglia function, brain perfusion, and glucose metabolism. EMBO J. 2017;36:1837–53.
**ang X, Werner G, Bohrmann B, Liesz A, Mazaheri F, Capell A, et al. TREM2 deficiency reduces the efficacy of immunotherapeutic amyloid clearance. EMBO Mol Med. 2016;8:992–1004.
Wang Y, Cella M, Mallinson K, Ulrich JD, Young KL, Robinette ML, et al. TREM2 lipid sensing sustains the microglial response in an Alzheimer’s disease model. Cell. 2015;160:1061–71.
Mazaheri F, Snaidero N, Kleinberger G, Madore C, Daria A, Werner G, et al. TREM2 deficiency impairs chemotaxis and microglial responses to neuronal injury. EMBO Rep. 2017;18:1186–98.
Paloneva J, Kestilä M, Wu J, Salminen A, Böhling T, Ruotsalainen V, et al. Loss-of-function mutations in TYROBP (DAP12) result in a presenile dementia with bone cysts. Nat Genet. 2000;25:357–61.
Chouery E, Delague V, Bergougnoux A, Koussa S, Serre JL, Mégarbané A. Mutations in TREM2 lead to pure early-onset dementia without bone cysts. Hum Mutat. 2008;29:E194–204.
Giraldo M, Lopera F, Siniard AL, Corneveaux JJ, Schrauwen I, Carvajal J, et al. Variants in triggering receptor expressed on myeloid cells 2 are associated with both behavioral variant frontotemporal lobar degeneration and Alzheimer’s disease. Neurobiol Aging. 2013;2077(34):e11–8.
Guerreiro R, Bilgic B, Guven G, Brás J, Rohrer J, Lohmann E, et al. A novel compound heterozygous mutation in TREM2 found in a Turkish frontotemporal dementia-like family. Neurobiol Aging. 2013;34:2890.e1–5.
Le Ber I, De Septenville A, Guerreiro R, Bras J, Camuzat A, Caroppo P, et al. Homozygous TREM2 mutation in a family with atypical frontotemporal dementia. Neurobiol Aging. 2014;35:2419.e23–5.
Piccio L, Buonsanti C, Cella M, Tassi I, Schmidt RE, Fenoglio C, et al. Identification of soluble TREM-2 in the cerebrospinal fluid and its association with multiple sclerosis and CNS inflammation. Brain. 2008;131:3081–91.
Öhrfelt A, Axelsson M, Malmeström C, Novakova L, Heslegrave A, Blennow K, et al. Soluble TREM-2 in cerebrospinal fluid from patients with multiple sclerosis treated with natalizumab or mitoxantrone. Mult Scler J. 2016;22:1587–95.
Heslegrave A, Heywood W, Paterson R, Magdalinou N, Svensson J, Johansson P, et al. Increased cerebrospinal fluid soluble TREM2 concentration in Alzheimer’s disease. Mol Neurodegener. 2016;11:3.
Piccio L, Deming Y, Del-Aquila JL, Ghezzi L, Holtzman DM, Fagan AM, et al. Cerebrospinal fluid soluble TREM2 is higher in Alzheimer disease and associated with mutation status. Acta Neuropathol. 2016;131:925–33.
Henjum K, Almdahl IS, Årskog V, Minthon L, Hansson O, Fladby T, et al. Cerebrospinal fluid soluble TREM2 in aging and Alzheimer’s disease. Alzheimers Res Ther. 2016;8:17.
Gispert JD, Suárez-Calvet M, Monté GC, Tucholka A, Falcon C, Rojas S, et al. Cerebrospinal fluid sTREM2 levels are associated with gray matter volume increases and reduced diffusivity in early Alzheimer’s disease. Alzheimers Dement. 2016;12:1259–72.
Suárez-Calvet M, Kleinberger G, Araque Caballero MÁ, Brendel M, Rominger A, Alcolea D, et al. sTREM2 cerebrospinal fluid levels are a potential biomarker for microglia activity in early-stage Alzheimer’s disease and associate with neuronal injury markers. EMBO Mol Med. 2016;8:466–76.
Suárez-Calvet M, Araque Caballero MÁ, Kleinberger G, Bateman RJ, Fagan AM, Morris JC, et al. Early changes in CSF sTREM2 in dominantly inherited Alzheimer’s disease occur after amyloid deposition and neuronal injury. Sci Transl Med. 2016;8:369ra178.
Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134:2456–77.
Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011;76:1006–14.
Paterson RW, Heywood WE, Heslegrave AJ, Magdalinou NK, Andreasson U, Sirka E, et al. A targeted proteomic multiplex CSF assay identifies increased malate dehydrogenase and other neurodegenerative biomarkers in individuals with Alzheimer’s disease pathology. Transl Psychiatry. 2016;6:e952.
Meeter LH, Dopper EG, Jiskoot LC, Sanchez-Valle R, Graff C, Benussi L, et al. Neurofilament light chain: a biomarker for genetic frontotemporal dementia. Ann Clin Transl Neurol. 2016;3:623–36.
Rohrer JD, Woollacott IOC, Dick KM, Brotherhood E, Gordon E, Fellows A, et al. Serum neurofilament light chain protein is a measure of disease intensity in frontotemporal dementia. Neurology. 2016;87:1329–36.
Bossù P, Salani F, Alberici A, Archetti S, Bellelli G, Galimberti D, et al. Loss of function mutations in the progranulin gene are related to pro-inflammatory cytokine dysregulation in frontotemporal lobar degeneration patients. J Neuroinflammation. 2011;8:65.
Miller ZA, Rankin KP, Graff-Radford NR, Takada LT, Sturm VE, Cleveland CM, et al. TDP-43 frontotemporal lobar degeneration and autoimmune disease. J Neurol Neurosurg Psychiatry. 2013;84:956–62.
Galimberti D, Bonsi R, Fenoglio C, Serpente M, Cioffi SMG, Fumagalli G, et al. Inflammatory molecules in frontotemporal dementia: cerebrospinal fluid signature of progranulin mutation carriers. Brain Behav Immun. 2015;49:182–7.
Takahashi H, Klein ZA, Bhagat SM, Kaufman AC, Kostylev MA, Ikezu T, et al. Opposing effects of progranulin deficiency on amyloid and tau pathologies via microglial TYROBP network. Acta Neuropathol. 2017;133:785–807.
Zhong L, Chen XF, Wang T, Wang Z, Liao C, Wang Z, et al. Soluble TREM2 induces inflammatory responses and enhances microglial survival. J Exp Med. 2017;214:597–607.
Yin F, Banerjee R, Thomas B, Zhou P, Qian L, Jia T, et al. Exaggerated inflammation, impaired host defense, and neuropathology in progranulin-deficient mice. J Exp Med. 2009;207:117–28.
Yin F, Dumont M, Banerjee R, Ma Y, Li H, Lin MT, et al. Behavioral deficits and progressive neuropathology in progranulin-deficient mice: a mouse model of frontotemporal dementia. FASEB J. 2010;24:4639–47.
Martens LH, Zhang J, Barmada SJ, Zhou P, Kamiya S, Sun B, et al. Progranulin deficiency promotes neuroinflammation and neuron loss following toxin-induced injury. J Clin Invest. 2012;122:3955–9.
Tanaka Y, Matsuwaki T, Yamanouchi K, Nishihara M. Exacerbated inflammatory responses related to activated microglia after traumatic brain injury in progranulin-deficient mice. Neuroscience. 2013;231:49–60.
Minami SS, Shen V, Le D, Krabbe G, Asgarov R, Perez-Celajes L, et al. Reducing inflammation and rescuing FTD-related behavioral deficits in progranulin-deficient mice with α7 nicotinic acetylcholine receptor agonists. Biochem Pharmacol. 2015;97:454–62.
Piccio L, Buonsanti C, Mariani M, Cella M, Gilfillan S, Cross AH, et al. Blockade of TREM-2 exacerbates experimental autoimmune encephalomyelitis. Eur J Immunol. 2007;37:1290–301.
Sjögren M, Vanderstichele H, Agren H, Zachrisson O, Edsbagge M, Wikkelsø C, et al. Tau and Aβ42 in cerebrospinal fluid from healthy adults 21–93 years of age: establishment of reference values. Clin Chem. 2001;47:1776–81.
Paternicò D, Galluzzi S, Drago V, Bocchio-Chiavetto L, Zanardini R, Pedrini L, et al. Cerebrospinal fluid markers for Alzheimer’s disease in a cognitively healthy cohort of young and old adults. Alzheimers Dement. 2012;8:520–7.
Forabosco P, Ramasamy A, Trabzuni D, Walker R, Smith C, Bras J, et al. Insights into TREM2 biology by network analysis of human brain gene expression data. Neurobiol Aging. 2013;34:2699–714.
Lue LF, Schmitz CT, Serrano G, Sue LI, Beach TG, Walker DG. TREM2 protein expression changes correlate with Alzheimer’s disease neurodegenerative pathologies in post-mortem temporal cortices. Brain Pathol. 2015;25:469–80.
Funding
This work was funded by the Medical Research Council (MRC) UK. The authors acknowledge the support of the National Institute for Health Research (NIHR) Queen Square Dementia Biomedical Research Unit and the University College London Hospitals Biomedical Research Centre, the Leonard Wolfson Experimental Neurology Centre, the MRC Dementias Platform UK and the UK Dementia Research Institute. The Dementia Research Centre is an Alzheimer’s Research UK (ARUK) coordinating centre and is supported by ARUK, the Brain Research Trust and the Wolfson Foundation. IOCW is funded by an MRC Clinical Research Training Fellowship (MR/M018288/1). KMD is supported by an Alzheimer’s Society PhD Studentship. RWP is funded by an NIHR Clinical Lectureship. AK is the recipient of a PhD Fellowship awarded by the Wolfson Foundation and a grant from the Weston Brain Institute. JDW has received funding support from the Alzheimer’s Society. JMS acknowledges the support of the Engineering and Physical Sciences Research Council (EP/J020990/1), MRC Dementias Platform UK (MR/L023784/1), ARUK (ARUK-Network 2012-6-ICE, ARUK-PG2017-1946, ARUK-PG2017-1946), Brain Research UK (UCC14191), the Weston Brain Institute (UB170045) and the European Union’s Horizon 2020 research and innovation programme (grant 666992). HZ is a Wallenberg Academy Fellow. JDR is an MRC Clinician Scientist (MR/M008525/1) and has received funding from the NIHR Rare Diseases Translational Research Collaboration (BRC149/NS/MH), the Bluefield Project and the Association for Frontotemporal Degeneration.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
IOCW and JDR conceptualised and designed the study and drafted the initial manuscript. IOCW collected CSF samples and clinical data, performed sTREM2 immunoassays, analysed data, interpreted results, produced tables and figures, and revised the initial manuscript based on edits and comments from other authors. JMN assisted with study design; provided statistical advice; and assisted in data analysis, production of figures and interpretation of results. AH developed the sTREM2 immunoassay, provided technical advice for assays, and contributed to the initial draft of the “Methods” section. CH and MSF processed CSF samples and performed INNOTEST immunoassays for quantification of CSF T-tau, P-tau and Aβ42 levels. KMD and LLR assisted with patient recruitment and collection of clinical data. RWP and AK assisted in patient recruitment and collection of CSF samples and clinical data. HZ assisted in study conceptualisation and design. All authors edited the manuscript, but JMN, AH, NCF, JDW, JMS, HZ and JDR provided major contributions to edits. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in line with ethics applications approved by the Health Research Authority and NHS Research Ethics Service Committee, London, Queen Square. All individuals gave written informed consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Woollacott, I.O.C., Nicholas, J.M., Heslegrave, A. et al. Cerebrospinal fluid soluble TREM2 levels in frontotemporal dementia differ by genetic and pathological subgroup. Alz Res Therapy 10, 79 (2018). https://doi.org/10.1186/s13195-018-0405-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-018-0405-8