Abstract
Parkinson’s disease (PD), a neurodegenerative disorder with an unknown etiology, is primarily characterized by the degeneration of dopamine (DA) neurons. The prevalence of PD has experienced a significant surge in recent years. The unidentified etiology poses limitations to the development of effective therapeutic interventions for this condition. Helicobacter pylori (H. pylori) infection has affected approximately half of the global population. Mounting evidences suggest that H. pylori infection plays an important role in PD through various mechanisms. The autotoxin produced by H. pylori induces pro-inflammatory cytokines release, thereby facilitating the occurrence of central inflammation that leads to neuronal damage. Simultaneously, H. pylori disrupts the equilibrium of gastrointestinal microbiota with an overgrowth of bacteria in the small intestinal known as small intestinal bacterial overgrowth (SIBO). This dysbiosis of the gut flora influences the central nervous system (CNS) through microbiome-gut-brain axis. Moreover, SIBO hampers levodopa absorption and affects its therapeutic efficacy in the treatment of PD. Also, H. pylori promotes the production of defensins to regulate the permeability of the blood-brain barrier, facilitating the entry of harmful factors into the CNS. In addition, H. pylori has been found to induce gastroparesis, resulting in a prolonged transit time for levodopa to reach the small intestine. H. pylori may exploit levodopa to facilitate its own growth and proliferation, or it can inflict damage to the gastrointestinal mucosa, leading to gastrointestinal ulcers and impeding levodopa absorption. Here, this review focused on the role of H. pylori infection in PD from etiology, pathogenesis to levodopa bioavailability.
Similar content being viewed by others
Introduction
Parkinson’s disease (PD) is the second most prevalent neurodegenerative disorder, following Alzheimer’s disease (AD) [1]. It is projected that by 2040, the global PD population will exceed 14 million individuals [2]. Numerous studies have demonstrated that the older adult has a higher susceptibility to PD [3]. PD is characterized by a progressive degeneration of neurons in the brain, leading to their eventual demise and disruption of normal dopamine (DA) neuronal activity [4]. Notably, two prominent neuropathological manifestations of PD are the death of nigrostriatal DA neurons and the abnormal aggregation of α-synuclein (α-syn) with the formation of Lewy vesicles [5]. The clinical symptoms of PD can be categorized into motor and non-motor symptoms. Motor symptoms mainly encompass dyskinesia, tremor, rigidity and postural instability [6], whereas non-motor symptoms predominantly consist of depression, anxiety, sensory disturbances, sleep disturbances, gastrointestinal dysfunction, amnesia, olfactory loss, and dementia [7, 8]. Previous studies indicated that non-motor symptoms manifested earlier than motor symptoms [9]. Moreover, PD patients frequently reported experiencing gastrointestinal disorders prior to the onset of motor symptoms. Gastrointestinal symptoms in PD have a significantly high prevalence globally [7]. Typically, the symptoms of PD exhibit a gradual deterioration as the disease progresses [6]. Regrettably, there is currently no medical intervention capable of completely eradicating PD. Clinical management of PD primarily relies on the administration of levodopa to alleviate motor symptoms [10].
Helicobacter pylori (H. pylori), a Gram-negative, spiral-shaped, microaerophilic and flagellated bacterium, is widely prevalent worldwide, infecting approximately half of the global population [11, 12]. It predominantly colonizes the gastric mucosa in humans and predisposes individuals to various gastric mucosal diseases, including gastric ulcers and gastric cancer [11]. H. pylori can enter the brain via two distinct pathways: the oral-nasal olfactory pathway and the gastrointestinal tract associated retrograde axonal transport pathway [13]. Monocytes infected with H. pylori traverse the blood-brain barrier (BBB), which is compromised due to chronic infection and the release of pro-inflammatory cytokines. Consequently, this process leads to the occurrence of neurodegeneration [14]. Extensive evidences have demonstrated the association between H. pylori and various central nervous system (CNS) disorders, such as depression, anxiety, PD, AD, Multiple sclerosis (MS), Green-Barré syndrome (GBS), and Bickerstaff brainstem encephalitis (BBE), among others [13, 15]. The mechanisms by which H. pylori contributes to PD are believed to involve the production of toxins, disruption of the delicate equilibrium of intestinal microbes, stimulation of pro-inflammatory cytokines production, and interference with the effectiveness of PD medications [16, 17]. This review aimed to summarize the association between H. pylori infection and PD, focusing on the etiology, pathogenesis, and levodopa bioavailability, to provide new insights into the treatment of PD.
Microbiome-gut-brain axis: H. Pylori infection and PD
H. pylori infection has been observed to disrupt the delicate equilibrium of the microbiota within the gastrointestinal tract [18]. It is widely acknowledged that the maintenance of human health heavily depends on the dynamic balance of the gastrointestinal microbiota [19]. When this equilibrium is disrupted, the body becomes vulnerable to various associated diseases [20]. H. pylori primarily influences the intestinal microbiota by means of virulence factors, such as cytotoxin-related gene A (CagA), vacuolar cytotoxin A (VacA), urease (Ure), arginase (Arg), lipopolysaccharide (LPS), and neutrophil activating protein (NAP) [11]. This phenomenon involves the fascinating concept of the microbiome-gut-brain axis, which encompasses various signaling pathways, including neuronal, metabolic, endocrine, and immune pathways, through which the gut microbiome communicates with the brain [15, 21]. Importantly, the gut microbiota can up-regulate inflammation both locally and systemically [21]. Dysregulation of the intestinal ecological and heightened intestinal permeability leads to overstimulation of the innate immune system, inducing systemic and CNS inflammation [21]. In addition, H. pylori has the potential to indirectly affect the microbiome-gut-brain axis through its influence on the intestinal microbiota, consequently resulting in the development of CNS disorders [13].
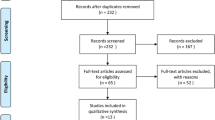
Abnormal folding and aggregation of α-syn in the enteric nervous system (ENS) of PD patients causes the formation Lewy bodies and neuritis [22]. Furthermore, Lewy bodies are discerned in the gastrointestinal tract of numerous PD patients who do not exhibit PD symptoms [23]. These discoveries have fostered an increasing recognition that the origin of PD might lie within the intestine. Consequently, a hypothesis has been put forth suggesting that the misfolding and aggregation of α-syn initially occurs in the intestine and subsequently spreads to brain via the vagus nerve [24]. This hypothesis was expeditiously validated through the administration of human brain PD lysate containing α-syn into the intestinal wall of rats, which resulted in the rapid transportation of α-syn via the vagus nerve into the brainstem, specifically in the dorsal motor nucleus of the vagus nerve [25]. The pivotal role of the vagus nerve in this process becomes evident. As one of the largest nerves connecting the gastrointestinal tract to the brain, the vagus nerve has been observed to diminish the risk of PD when subjected to vagotomy, especially for full truncal vagotomy [24]. This substantiates the notion that PD and the gut are inextricably linked [26]. On the other hand, it has been demonstrated that a significant proportion of the impacts exerted by the gut microbiota on brain function are contingent upon vagal activation. This finding serves to reinforce the notion that the gastrointestinal tract and CNS could establish a reciprocal relationship via the brain-gut axis. At the beginning of the 20th century, the association between infection and PD was widely regarded as highly consequential [27]. Since then, increasing evidence focused their attention towards investigating the correlation between viral and bacterial infections and PD. Subsequently, in 1960, the association of H. pylori infection and PD was initially discovered [28]. Moreover, various studies have reported a prevalence range of 26.4–87.9% for H. pylori infection in PD patients. These patients were older and had worse motor function, suggesting a potential association between H. pylori infection and PD pathophysiology (Table 1). Additionally, the effect of H. pylori infection on PD motor results varied according to age [40]. Various viewpoints exist regarding the factors that influence PD pathogenesis upon H. pylori infection, with particular emphasis placed on toxin production by H. pylori (Fig. 1A), disruption of intestinal flora, release of massive pro-inflammatory cytokines, activation of microglia and astrocyte, and dysfunction of BBB [17].
Potential mechanisms of the association of H. pylori infection with PD. (A) H. pylori virulence factors, such as LPS, CagA, VacA, and CGs, activate NF-kB or PI3K-AKT pathway to induce the production of pro-inflammatory factors of the T cells, which further stimulate glial cells, leading to neuronal injury. (B) VacA monomers assemble into oligomers and then translocate to the membranes of LEs, facilitating the entry of chloride ions into the lumen, which in turn enhances the activity of v-ATPase proton pump and reduces the intraluminal pH. Additionally, VacA induces apoptosis of epithelial cells that leads to “leaky gut” and increases the permeability of the blood-brain barrier, eventually impact nerve cells. (C) H. pylori infection cause SIBO, leading to the impairment of mitochondrial function and subsequent hindrance of ATP production and calcium influx, which are crucial for maintaining neuronal activity. Moreover, its virulence factor, VacA, can enter mitochondria and stimulate the release of cytochrome c from these organelles, further leading to mitochondrial impairment. Abbreviations: PD: Parkinson’s disease; CagA: Cytotoxin-related gene A; VacA: Vacuolar cytotoxin A; Ure: Urease; LPS: Lipopolysaccharide; TLR4: Toll-like receptor 4; LBP: Lipopolysaccharide binding protein; CG: Cholesterol glucosides; LEs: Late endonuclear bodies
H. Pylori infection in PD pathogenesis
H. Pylori virulence factors and PD
LPS
LPS, a group of phosphorylated lipoglycans, is primarily found in the outer membrane of Gram-negative bacteria [41]. The influence of H. pylori on the pathogenesis of PD has been reported to occur through the production of LPS [42, 43]. The detrimental effects of LPS on DA neurons are mainly attributed to its ability to trigger an inflammatory response [42]. This hypothesis was supported by a mouse model experiment conducted in 2017 and 2022, wherein the intraperitoneal injection of LPS elicited a robust pro-inflammatory response in mice, leading to the loss of nigrostriatal DA neurons [44, 45]. LPS treatment was administered subsequent to the successful establishment of the mouse model, and the cessation of LPS-induced damage to DA neurons was observed [45]. Moreover, LPS activates immune cells, such as T cells, in the gut and substantia nigra, thereby triggering a systemic inflammatory response by interacting with Toll-like receptor 4 (TLR4) located on the gut surface [46,47,48]. Among the entire TLR family, TLR4 exhibits a distinctive ability to recognize LPS derived from Gram-negative bacterial [48]. The process of LPS attachment involves the cluster of differentiation (CD14) in two forms [49]. Specifically, LPS is presented to membrane CD14 and TLR4 via the mediation of lipopolysaccharide binding protein (LBP). Additionally, it has been demonstrated that soluble CD14 and LBP play crucial roles in activating TLR upon LPS stimulation [50,51,52]. The activation of TLR4 by LPS can initiate various downstream pathways, including myeloid differentiation primary response 88 (MyD88) and NF-κB, which play critical roles in production of multiple pro-inflammatory cytokines (e.g., TNF-α, IL-1β, and IL-6) and oxidative stress molecules that contribute to neuroinflammation [53,54,55].
The pathology of PD is characterized by the misfolding and aggregation of α-syn, which activate microglia and astrocytes in the nigrostriatal region [6, 56, 57]. Lipid structures present in LPS induce the aggregation of α-syn [26, 58], and these lipid structures are mainly located in the outer membrane of Gram-negative bacteria. Furtherly, nuclear magnetic resonance (NMR) semi-quantitative analysis demonstrates that intact helical α-syn structures adopt a specific helical conformation in order to bind to the lipid surface [58, 59]. There are substantial evidences supporting this theory. In addition, α-syn monomers exhibited intense thioflavin T fluorescence after incubation with LPS [59]. When these α-syn protofibrils were injected into the mouse striatum, phosphorylated α-syn was observed throughout various regions of the brain including the striatum, substantia nigra, amygdala, and auditory cortex. This finding suggests that α-syn protofibrils induced by LPS possess toxic properties [58]. The neurotoxicity of these protofibrils is related to their structural and post-translational modifications, such as phosphorylation and nitration at Ser129 [59,60,61]. Also, LPS regulates α-syn in a concentration-dependent manner [58, 60]. Meanwhile, the presence of these pathological proteins hinders normal physiological functions of α-syn, while also exerting toxicity as an environmental stressor, thereby promoting inflammation, oxidative stress, and disruption of other physiological processes [62, 63]. Furthermore, this cascade of events triggers the release of pro-inflammatory and neurotoxic molecules by immune cells in the brain, ultimately leading to chronic neuroinflammation and neuronal death [64].
Besides, the induction of PD by LPS involves in the activation of glial cells, which in turn produce various stimulatory and regulatory factors [65, 66]. One notable effect is the excessive production of nitric oxide (NO) by microglia, which leads to DA neurodegeneration. Meanwhile, LPS up-regulates the expression of inducible nitric oxide synthase (iNOS) to promote NO release from microglia and astrocytes [64]. In addition, LPS can influence the activation of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase enzymes, resulting in the production of reactive oxygen species (ROS) in microglia [67]. Interestingly, these ROS released from microglia not only directly damage DA neurons, but also up-regulate the expression of TNF-α [68], IL-1β and cyclooxygenase-2 (COX-2), leading to enhanced collective inflammatory damage to DA neurons [69, 70]. Among various cytokines released by LPS-activated glial cells, the pro-inflammatory factors, such as IL-1β and TNF-α, are believed to be the primary cytokines involved in LPS-induced DA neurodegeneration [69,70,71]. Furthermore, TNF-α increases the surface expression of tumor necrosis factor receptor 1 (TNFR1), thereby exacerbating LSP-induced DA neurotoxicity [64].
Cholesterol glucoside
H. pylori infection leads to the production of cholesterol glucosides (CGs) that have a detrimental effect on nerve cells, thereby initiating the degeneration of neurons and ultimately triggering PD [72]. CGs, which are lipid components of H. pylori, play a crucial role in enabling it to adapt to environmental changes. The synthesis of CGs necessitates the presence of cholesterol, which H. pylori cannot produce on its own and therefore relies on the consumption of host cholesterol [73]. Enzyme responsible to produce CGs is cholesterol-based glycosyltransferase (CGT), which is encoded by the HP0421 gene [74]. This gene is required for H. pylori evasion of host immune cells [75]. AKT, a crucial protein kinase with anti-apoptotic properties, is believed to exert a protective function in neuronal injury by phosphorylating and inhibiting downstream regulators of apoptosis [76, 72]. Activation of AKT occurs in response to oxidative and hypoxia, enabling it to effectively process various types of stressful stimuli [77, 72]. The cytoprotective effect associated with AKT is abolished when its upstream activator, PI3K, is blocked, indicating the significance of the PI3K/AKT pathway in promoting cell survival [72]. This notion is further supported by the elimination of cytoprotective effect, when PI3K is inhibited during CG preconditioning [72]. The AKT pathway plays an important role in inhibiting cell death induced by various cytotoxic stress stimuli [77, 78]. In addition, impairment of AKT signaling has been implicated in neuronal death observed in various neurodegenerative disease animal models [72]. For instance, the absence of AKT signaling was identified as a potential contributor to cell death in motor neurons lacking adequate nutritional support, and interference with the PI3K/AKT pathway by CGs in T cells was implicated in the pathogenesis of PD [72, 79].
Cytotoxin
The cytotoxins, CagA and VacA, are considered as the main pathogenic factors in H. pylori infection [80]. CagA, a virulence factor of H. pylori, can be translocated by the type IV secretion system (T4SS) after attaching to cells, then activate T cells that result in chronic inflammation of gastric epithelial cells [81, 82]. It has the ability to activate transcription factor, NFAT, independent of its phosphorylation [82, 83]. Lipid rafts are cholesterol-rich membrane microstructural domains that provide entry points for many bacterial pathogens or their virulence factors. H. pylori utilizes host externalized phosphatidylserine (PS) to deliver CagA via T4SS [84], and CGT participates in this process by promoting H. pylori adhesion to host cells in a raft-dependent manner [68, 85].
VacA possesses the ability to form anion-selective channels within planar lipid bilayers, allowing for the conduction of chloride, bicarbonate, and organic molecules. This ability to stimulate intracellular acidic vesicle formation and disrupt cellular homeostasis ultimately leads to apoptosis (Fig. 1B) [74, 84, 86]. VacA monomers assemble into oligomers and then translocate to the membranes of late endonuclear bodies (LEs), where they form an anion-selective channel, enabling the entry of chloride ion into the lumen [87, 88]. This process subsequently enhances the activity of the v-ATPase proton pump and reduces the intraluminal pH [74]. Weak bases that can pass through the membrane diffuse into the LEs, in which they are protonated and trapped in an acidic environment [74]. LEs develops osmotic swelling, leading to cellular vacuolation [89, 90]. Additionally, VacA increases the permeability of the cell membrane, allowing for the influx of various anions and small molecules, such as chloride, urea and bicarbonate, into the extracellular space [91]. VacA induces vacuolation and apoptosis of epithelial cells, inducing disruption of tight junction integrity in the epithelium and resulting in increased permeability (“leaky gut”). This increased permeability allows various toxins to cross BBB and enter the brain, where they can impact nerve cells [74].
VacA activates p38MAPK in T cells, a crucial regulator of multiple cellular stresses. The activated form of p38MAPK then regulates several downstream transcription factors, including NF-κB, which up-regulates inflammatory molecules, such as COX-2 and iNOS, and promotes the development and progression of inflammatory response [74, 92, 93]. The p38MAPK signaling pathway participates in the neuroinflammatory responses mediated by microglia and astrocytes [94]. Activation of the p38 signaling pathway by VacA also induces the activation of activating transcription factor 2 (ATF-2) [95]. Furthermore, VacA can modulate the function of a variety of immune cells, including lymphocytes, macrophages, eosinophils, mast cells, and dendritic cells. In B cells, VacA has been observed to disrupt antigen presentation [18]. In macrophages, VacA contributes to the formation of macrovesicular bodies and hinders the maturation and functionality of vesicle compartments [96]. In addition, VacA modulates various signaling pathways in macrophages and induces apoptosis in these cells [97,98,99]. Consequently, these VacA-mediated effects might compromise the phagocytic ability of macrophages towards H. pylori [87], thereby exacerbating the effects of H. pylori on PD.
H. Pylori, small intestinal bacterial overgrowth and PD
An abundance of bacteria in the small intestine, resulting in gastrointestinal symptoms, is referred to as small intestinal bacterial overgrowth (SIBO) [100]. It is widely acknowledged that constipation, a representative non-motor symptom of PD, exhibits a high prevalence. In 2021, a connection between SIBO and PD was first established through the presence of constipation, suggesting that the severity of constipation might increase the likelihood of SIBO [101]. In addition, elevated gastric pH and gastric mucosal atrophy could contribute to the development of SIBO [102]. H. pylori is capable of hydrolyzing urea to produce ammonia and carbonic acid in the stomach, where ammonia by-products serve to buffer gastric acid, causing an increase in gastric pH and the development of gastric mucosal atrophy. Moreover, proton pump inhibitors (PPIs), which are commonly used to treat H. pylori infection, further elevate gastric pH. Antibiotics utilized in the treatment of H. pylori infection disrupt the balance of intestinal flora, potentially leading to SIBO [102, 103]. In 2017 and 2018, two studies were conducted to investigate the relationship between SIBO and H. pylori. The pilot study conducted in 2017 examined a cohort of 109 patients diagnosed with both H. pylori infection and SIBO, revealing that 52.8% patients with H. pylori infection also presented with SIBO [104]. Conversely, only 21.9% patients without H. pylori infection met the criteria for SIBO [103]. These data suggested that the incidence of SIBO was twice as high in patients infected with H. pylori compared to those uninfected patient [105]. This conclusion was further supported by a separate study conducted in 2018, which reported that 53% patients with concurrent H. pylori infection and SIBO were identified [106].
It is noteworthy that H. pylori infection causes mitochondria impairment, and the coexistence of H. pylori and damaged mitochondria synergistically contribute to the progression of SIBO [107, 105] (Fig. 1C). Its virulence factor, VacA, can enter mitochondria and stimulate the release of cytochrome c from these organelles, further leading to mitochondrial impairment [104, 108, 109]. The emergence of SIBO further exacerbates mitochondrial dysfunction, and chronic infection at the large mucosal interface intensifies mitochondrial damage [107, 105]. Impaired mitochondrial function impedes adenosine triphosphate (ATP) synthesis and calcium regulation, both of which are crucial for neuronal activity [110, 111]. In addition, the impact of mitochondria on PD is mediated through its interaction with PD-related proteins. The intricated nature of mitochondria and its involvement in various pathogenic pathways associated with PD underscores its significant influence on several processes, such as energy supply, calcium buffering, and ROS production [111]. For instance, PINK1 actively recruits Parkin to mitochondria and phosphorylates it, leading to the disruption of mitochondria. This disruption allows for their encapsulation by autophagosomes and subsequent transportation to lysosomes [110]. Animal models with PINK1 and Parkin mutations presented structural and functional alterations in mitochondria, which were frequently implicated in the degeneration of DA neurons in these models [100].
A synergistic effect has been identified between the coexistence of H. pylori and SIBO with a diminished effectiveness of PD medications and subsequently exacerbating motor fluctuations [100]. H. pylori infection was more closely associated with wear phenomena, whereas SIBO was primarily correlated with delayed opening and non-opening. The simultaneous presence of H. pylori and SIBO resulted in the most severe motion fluctuations [100]. PD patients with comorbid SIBO experienced more severe dyskinesia, including prolonged rest time, delayed on-time and off-time, compared to those without SIBO [18]. This suggests a close association between SIBO and deterioration in motor function [18]. Another evidence showed that motor fluctuations in PD patients were improved after the eradication of SIBO, further supporting the association between SIBO and motor fluctuations in PD [88]. Several speculations have been proposed to explain this association, including the potential impact of SIBO on drug absorption by altering chyme composition [18]. Malabsorption can be attributed to the loss of brush border disaccharidase activity caused by mucosal damage, bacterial fermentation of sugars, and bacterial uncoupling of bile acids [112, 113]. SIBO may induce detrimental inflammatory effects on enterochromaffin cells and further impede gastric emptying [114]. Recently, given that levodopa is primarily absorbed in the duodenum, SIBO may hinder drug absorption due to intestinal mucosal inflammation [13, 100, 32].
H. Pylori, BBB and PD
H. pylori has been found to disrupt BBB, leading to an increase of harmful substances entry into the brain and subsequent neuronal damage (Fig. 2) [114]. This disruption is attributed to the promotion of pro-inflammatory cytokines, IFN-γ and TNF-α, release from bone marrow-derived mast cells (BMD-MCs) by H. pylori infection, with TNF-α activating matrix metalloproteinases that compromise the integrity of BBB [13]. In addition, H. pylori may contribute to BBB disruption through the release of defensins, particularly those that are uniquely distributed at the site of BBB [115]. Simultaneously, H. pylori infection triggers the activation of granulocytes and prompts the release of defensins from these cells. The defensins, once secreted by the activated granulocytes, are capable of breaching BBB and gaining access to brain, potentially resulting in neurodegeneration [116]. On the other hand, the inflammatory factors instigated by H. pylori can disrupt the neuroendocrine immune system and impair brainstem function, leading to the prolonged secretion of pro-inflammatory cytokines that compromise the integrity of BBB [13]. Consequently, this compromised barrier permits the entry of more detrimental substances into the brain, thereby causing damage to DA neurons and inducing PD.
H. pylori infection disrupt the BBB to contribute to the development of PD. H. pylori infection can stimulate the release of pro-inflammatory cytokines and defensins from BMD-MCs and granulocytes, respectively, resulting in the compromised integrity of the BBB. Consequently, compromised BBB facilitates the infiltration of additional inflammatory factors into the brain, leading to neuronal damage
H. pylori and levodopa bioavailability
As previously mentioned, the primary approach to managing PD involves alleviating motor symptoms, with levodopa being a crucial medication for addressing these symptoms [116, 117]. Extensive studies have been conducted in recent years, particularly focusing on the in vivo metabolism of levodopa. It is widely recognized that oral administration of levodopa causes its absorption into the bloodstream at the duodenum and subsequent passage through the BBB to reach the pathological area for therapeutic purposes. Numerous factors influence the bioavailability of levodopa during this process, and among them, H. pylori has been found to exert a significant impact on the efficacy of levodopa [118, 119]. H. pylori interferes with the efficacy of levodopa treatment, leading to motor fluctuations [120]. This phenomenon has been substantiated by a study conducted in Korea, wherein a notable reduction of 25.9% in levodopa “onset” time and an increase of 11.9% in levodopa “on time” were observed after successful eradication of H. pylori infection in 34 patients with PD. Notably, there was no significant alteration in symptom scores, as evaluated by the unified-PD rating scale III, before and after eradication [121]. Consequently, the eradication of H. pylori infection could serve as a preventive measure and improve the clinical condition of PD patients experiencing motor fluctuations [34]. The impact of H. pylori on levodopa pharmacokinetics in PD is multifaceted (Fig. 3).
Effect of H. pylori infection on levodopa absorption. (1) H. pylori infection induces gastroparesis by regulating the SCF/c-kit pathway, hereby further impeding levodopa absorption. (2) H. pylori infection obstructs the dissolution of levodopa under elevated pH conditions. (3) H. pylori infection leads to duodenal enterocolitis, which hampers levodopa absorption through LATs. Abbreviations: ICC: Interstitial cells of Cajal; SCF: stem cell factor. DGE: Delayed gastric emptying; LAT: L-type amino acid transporter
H. Pylori and gastroparesis
Pathological alterations of the intragastric milieu during H. pylori infection in PD affect the process of drug absorption [34]. Among gastrointestinal disorder in PD, gastroparesis is the most prevalent [122]. In addition, there is evidence suggesting a correlation between the severity of dyskinesia in PD patients and the gastroparesis [9]. Clinically, gastroparesis, also namely delayed gastric emptying (DGE), is characterized by slowing or stop** the food movement from stomach to small intestine, even though there is no blockage in the stomach or intestines, and H. pylori infection influences DGE and hampers the absorption of levodopa [118, 34, 123]. The main feature is reduced by gastric motility in the absence of mechanical obstruction [124]. The pathogenic mechanisms of mild paralysis may encompass autonomic and intrinsic neuropathy of the excitatory and inhibitory systems of the gastrointestinal tract, including impairment of the Vagus nerves and interstitial cells of Cajal (ICCs), which govern the contractility of smooth muscle cells [122]. ICCs serve as pacemakers, generating slow waves within the gastrointestinal tract, thereby dictating the frequency of rhythmic contractions in the smooth muscle [125,126,127]. ICCs are ubiquitously distributed throughout the entire gastrointestinal tract, spanning from the esophagus to the internal anal sphincter [125]. They act as mediators of muscle innervation in motor activity, and the proliferation, differentiation and functionality of ICCs are intricately associated with the activation of c-kit receptors present on their surface [128]. The activation of c-kit is contingent upon the presence of the endogenous ligand, stem cell factor (SCF) [129, 130]. Previous investigations have demonstrated that SCF mutations or deletions precipitate a decrease of ICCs number or disrupt the integrity of the ICC network, thereby giving rise to gastrointestinal motility disorders [131,132,133]. Alterations in SCF levels can consequently induce changes in the number of ICCs, leading to gastrointestinal motility disorders [134]. Hence, it is evident that the SCF/c-kit pathway plays a crucial role in the proper functioning of ICCs. In addition, increasing studies have demonstrated that H. pylori infection affects the SCF level, leading to a reduction in the number of ICCs and subsequently causing DGE. Recent findings conducted in 2021 revealed a significant decrease in gastric emptying rates among H. pylori-infected mice compared to uninfected mice [123]. Moreover, the expression of SCF in gastric tissues of H. pylori infection was obviously lower compared to the H. pylori-uninfected group. Also, submucosa and intramuscular ICCs numbers were reduced in the H. pylori-infected group. These findings suggest that H. pylori infection is highly associated with a decrease in SCF levels and ICCs numbers in gastric tissue, eventually leading to DGE. Furtherly, the entry of levodopa into the duodenum is affected by this phenomenon [125].
H. Pylori and stomach pH
Influence of stomach pH on levodopa dissolution has been observed, indicating that levodopa exhibits optimal solubility in highly acidic environments [34, 123]. However, the regulation of stomach pH by H. pylori complicates this process. Specifically, H. pylori produces urease in the stomach, which hydrolyzes urea into ammonia and carbonic acid. The ammonia by-products act as buffers for gastric acid, thereby regulating stomach pH [102, 123]. Consequently, the presence of H. pylori hinders the dissolution of the drug in higher pH conditions. In addition, H. pylori infection causes chronic inflammation of the gastric mucosa, resulting in the inhibition of gastric acid secretion by the mural cells [121, 135]. Pro-inflammatory cytokine, such as IL-1β, a key mediator in H. pylori-associated disease, inhibits gastric acid secretion in vitro and in vivo [136]. Prolonged injury from H. pylori could cause an obvious loss of mural cells, leading to atrophy of the oxidative glands and a subsequent decrease in gastric juice acidity [135].
Furthermore, it has been discovered that H. pylori possesses several types of receptors that enable it to directly utilize levodopa for growth [118, 39]. The proliferation of H. pylori necessitates specific amino acids, including arginine, histidine, isoleucine, leucine, methionine, valine, and phenylalanine. Notably, the demand for phenylalanine presents the potential for bacterial consumption of levodopa within the stomach. Various animal studies have substantiated this assertion [137, 138]. In a speculative study published in 2010, it was indicated that H. pylori colony-forming units had a direct reliance on levodopa for their growth [136]. Time- and concentration-dependent incubation studies indicated an apparent decrease in levodopa levels upon contact with H. pylori [122]. Moreover, an inverse relationship between the concentration of H. pylori and levodopa was observed as time progressed. H. pylori exhibited the enhanced growth in media containing higher level of levodopa compared to media simulating the normal gastric environment [138].
H. Pylori and duodenum
Levodopa is primarily absorbed in the duodenum, making it a crucial site for modulating the efficacy of levodopa treatment. Extensive studies have documented the impact of duodenal enterocolitis on levodopa absorption, with multiple studies demonstrating the association between H. pylori infection and duodenal enterocolitis [118, 123]. Activation of human phagocytes by H. pylori leads to the production of reactive oxygen metabolites (ROM), which inflict damage upon the duodenal mucosa. This process plays an important role in the development of enterocolitis and subsequently affects levodopa absorption [139]. Absorption of levodopa in the small intestine is believed to be facilitated by a significant neutral amino acid transport mechanism, potentially involving the L-type amino acid transporter protein (LATs) [140]. This transporter is closely involved in the transportation of various amino acids. To minimize competition for carrier-mediated intestinal transport, it is advisable to avoid the simultaneous. Once absorbed into the blood stream, levodopa traverses BBB with the assistance of LATs. However, the presence of duodenal inflammation hinders the functional absorption of levodopa by LATs [39].
Conclusions
Recent studies have identified numerous factors that are associated with the onset and progression of PD, thereby presenting a significant challenge in treatment due to the diversity of these influencing factors. Consequently, approach to treating PD symptoms has not solely focused on addressing the symptoms themselves, but rather encompasses the management of other factors that impact PD. Notably, H. pylori alone could exert multiple effects on PD, thereby exacerbating the complexity of treatment. Eradication of H. pylori infection might improve clinical status of patients with PD, especially on bradykinesia, or improve levodopa bioavailability. However, some studies pointed out H. pylori eradication did not improve clinical outcomes in PD. Therefore, identification and subsequent targeted treatment of the underlying cause of PD have emerged as the paramount concerns and the optimal therapeutic choice presently. Moreover, this simultaneous treatment approach presents several discernible drawbacks. Primarily, the amalgamation of various drugs is likely to result in a diverse range of side effects, thereby detrimentally impacting the patient’s overall health. Secondly, this approach imposes a substantial financial burden on the individual. Finally, the aforementioned factors significantly compromise the physical and psychological well-being of patients.
Data availability
Not applicable.
Abbreviations
- α-syn:
-
α-synuclein
- ATF-2:
-
Activating transcription factor 2
- ATP:
-
Adenosine triphosphate
- AD:
-
Alzheimer’s disease
- BBE:
-
Bickerstaff brainstem encephalitis
- BBB:
-
Blood-brain barrier
- BMD-MCs:
-
Bone marrow-derived mast cells
- CagA:
-
Cytotoxin-related gene A
- CG:
-
Cholesterol glucosides
- CGT:
-
Cholesterol-based glycosyltransferase
- CNS:
-
Central nervous system
- COX-2:
-
Cyclooxygenase-2
- DA:
-
Dopamine
- DGE:
-
Delayed gastric emptying
- ENS:
-
Enteric nervous system
- GBS:
-
Green-Barré syndrome
- H. Pylori :
-
Helicobacter pylori
- iNOS:
-
Inducible nitric oxide synthase
- ICCs:
-
Interstitial cajal cells
- LATs:
-
L-type amino acid transporter
- LBP:
-
Lipopolysaccharide binding protein
- LEs:
-
Late endonuclear bodies
- LPS:
-
Lipopolysaccharide
- MS:
-
Multiple sclerosis
- NADPH:
-
Nicotinamide adenine dinucleotide phosphate
- NAP:
-
Neutrophil activating protein
- NMR:
-
Nuclear magnetic resonance
- NO:
-
Nitric oxide
- PD:
-
Parkinson’s disease
- ROS:
-
Reactive oxygen species
- ROM:
-
Reactive oxygen metabolites
- PPIs:
-
Proton pump inhibitors
- SCF:
-
Stem cell factor
- SIBO:
-
Small intestinal bacterial overgrowth
- TLR4:
-
Toll-like receptor 4
- TNFR1:
-
Tumor necrosis factor receptor 1
- Ure:
-
Urease
- VacA:
-
Vacuolar cytotoxin A
References
Lampela P, Tolppanen AM, Kaarniranta K, Hokkinen K, Hartikainen S. Incidence of cataract surgeries in relation to diagnosis of Parkinson’s Disease. Arch Gerontol Geriatr. 2023;104:104842.
Hiller BM, Marmion DJ, Thompson CA, Elliott NA, Federoff H, Brundin P, et al. Optimizing maturity and dose of iPSC-derived dopamine progenitor cell therapy for Parkinson’s Disease. NPJ Regen Med. 2022;7(1):24.
Reeve A, Simcox E, Turnbull D. Ageing and Parkinson’s Disease: why is advancing age the biggest risk factor? Ageing Res Rev. 2014;14(100):19–30.
Sharma S, Awasthi A, Singh S. Altered gut microbiota and intestinal permeability in Parkinson’s Disease: pathological highlight to management. Neurosci Lett. 2019;712:134516.
Su A, Gandhy R, Barlow C, Triadafilopoulos G. A practical review of gastrointestinal manifestations in Parkinson’s Disease. Parkinsonism Relat Disord. 2017;39:17–26.
Chen ZJ, Liang CY, Yang LQ, Ren SM, **a YM, Cui L, et al. Association of Parkinson’s Disease with microbes and microbiological therapy. Front Cell Infect Microbiol. 2021;11:619354.
Bisaglia M. Mediterranean diet and Parkinson’s Disease. Int J Mol Sci. 2022;24(1):42.
Fan HX, Sheng S, Zhang F. New hope for Parkinson’s Disease treatment: targeting gut microbiota. CNS Neurosci Ther. 2022;28(11):1675–88.
Ivan IF, Irincu VL, Diaconu Ș, Falup-Pecurariu O, Ciopleiaș B, Falup-Pecurariu C. Gastro-intestinal dysfunctions in Parkinson’s Disease (review). Exp Ther Med. 2021;22(4):1083.
Fox SH, Katzenschlager R, Lim SY, Barton B, de Bie RMA, Seppi K, et al. International Parkinson and movement disorder society evidence-based medicine review: update on treatments for the motor symptoms of Parkinson’s Disease. Mov Disord. 2018;33(8):1248–66.
Deng R, Zheng H, Cai H, Li M, Shi Y, Ding S. Effects of helicobacter pylori on Tumor microenvironment and immunotherapy responses. Front Immunol. 2022;13:923477.
Sijmons D, Guy AJ, Walduck AK, Ramsland PA. Helicobacter pylori and the role of lipopolysaccharide variation in innate immune evasion. Front Immunol. 2022;13:868225.
Baj J, Forma A, Flieger W, Morawska I, Michalski A, Buszewicz G, et al. Helicobacter pylori Infection and extragastric diseases-A focus on the central nervous system. Cells. 2021;10(9):2191.
Kountouras J, Zavos C, Polyzos SA, Deretzi G, Vardaka E, Giartza-Taxidou E, et al. Helicobacter pylori Infection and Parkinson’s Disease: apoptosis as an underlying common contributor. Eur J Neurol. 2012;19(6):e56.
Gorlé N, Bauwens E, Haesebrouck F, Smet A, Vandenbroucke RE. Helicobacter and the potential role in neurological disorders: there is more than Helicobacter pylori. Front Immunol. 2020;11:584165.
Noto JM, Peek RM Jr. The gastric microbiome, its interaction with Helicobacter pylori, and its potential role in the progression to Stomach cancer. PLoS Pathog. 2017;13(10):e1006573.
Shen S, Zhang C, Xu YM, Shi CH. The role of pathogens and anti-infective agents in Parkinson’s Disease, from etiology to therapeutic implications. J Parkinsons Dis. 2022;12(1):27–44.
Lubomski M, Davis RL, Sue CM. Gastrointestinal dysfunction in Parkinson’s Disease. J Neurol. 2020;267(5):1377–88.
Li Z, Liang H, Hu Y, Lu L, Zheng C, Fan Y, et al. Gut bacterial profiles in Parkinson’s Disease: a systematic review. CNS Neurosci Ther. 2023;29(1):140–57.
Grenham S, Clarke G, Cryan JF, Dinan TG. Brain-gut-microbe communication in health and Disease. Front Physiol. 2011;2:94.
Mulak A, Bonaz B. Brain-gut-microbiota axis in Parkinson’s Disease. World J Gastroenterol. 2015;21(37):10609–20.
Travagli RA, Browning KN, Camilleri M. Parkinson Disease and the gut: new insights into pathogenesis and clinical relevance. Nat Rev Gastroenterol Hepatol. 2020;17(11):673–85.
Sun X, Xue L, Wang Z, **e A. Update to the treatment of Parkinson’s Disease based on the gut-brain axis mechanism. Front Neurosci. 2022;16:878239.
Braak H, Del Tredici K, Rüb U, de Vos RA, Jansen Steur EN, Braak E. Staging of brain pathology related to sporadic Parkinson’s Disease. Neurobiol Aging. 2003;24(2):197–211.
Holmqvist S, Chutna O, Bousset L, Aldrin-Kirk P, Li W, Björklund T, et al. Direct evidence of Parkinson pathology spread from the gastrointestinal tract to the brain in rats. Acta Neuropathol. 2014;128(6):805–20.
Chen QQ, Haikal C, Li W, Li JY. Gut inflammation in association with pathogenesis of Parkinson’s Disease. Front Mol Neurosci. 2019;12:218.
Shannon KM. Infections and changes in commensal bacteria and the pathogenesis of Parkinson’s Disease. J Parkinsons Dis. 2022;12(s1):45–S51.
Shamsdin SA, Khazraei H, Rahimi Jaberi A, Zamani M, Rafiee Monjezi M. Evaluation of inflammatory cytokine and anti Helicobacter pylori antibodies in the pathogenesis of Parkinson’s Disease. Middle East J Dig Dis. 2022;14(1):96–102.
Dobbs RJ, Charlett A, Dobbs SM, Weller C, MA AI, Iguodala O, et al. Leukocyte-subset counts in idiopathic parkinsonism provide clues to a pathogenic pathway involving small intestinal bacterial overgrowth. A surveillance study. Gut Pathog. 2012;4(1):12.
Rahne KE, Tagesson C, Nyholm D. Motor fluctuations and Helicobacter pylori in Parkinson’s Disease. J Neurol. 2013;260(12):2974–80.
Hashim H, Azmin S, Razlan H, Yahya NW, Tan HJ, Manaf MR, et al. Eradication of Helicobacter pylori Infection improves levodopa action, clinical symptoms and quality of life in patients with Parkinson’s Disease. PLoS ONE. 2014;9(11):e112330.
Tan AH, Mahadeva S, Marras C, Thalha AM, Kiew CK, Yeat CM, et al. Helicobacter pylori Infection is associated with worse severity of Parkinson’s Disease. Parkinsonism Relat Disord. 2015;21(3):221–5.
Efthymiou G, Dardiotis E, Liaskos C, Marou E, Tsimourtou V, Rigopoulou EI, et al. Immune responses against Helicobacter pylori-specific antigens differentiate relapsing remitting from secondary Progressive multiple sclerosis. Sci Rep. 2017;7(1):7929.
Liu H, Su W, Li S, Du W, Ma X, ** Y, et al. Eradication of Helicobacter pylori Infection might improve clinical status of patients with Parkinson’s Disease, especially on bradykinesia. Clin Neurol Neurosurg. 2017;160:101–4.
Mridula KR, Borgohain R, Chandrasekhar Reddy V, Bandaru V, Suryaprabha T. Association of Helicobacter pylori with Parkinson’s Disease. J Clin Neurol. 2017;13(2):181–6.
Roshan T, Bijani A, Hosseini SR, Bagherzade M, Saadat P, Zamani M. The association between Helicobacter pylori Infection and Parkinson’s Disease: a case-control study. J Clin Diagn Res. 2018;12:OC05–8.
Görgün S, Yılmaz A, ÖZgan E, Çalık M. Helicobacter pylori Infection is an avoidable risk factor for Parkinson s Disease. Turk J Geriatr. 2019;22:340–5.
Tan AH, Lim SY, Mahadeva S, Loke MF, Tan JY, Ang BH, et al. Helicobacter pylori eradication in Parkinson’s Disease: a randomized placebo-controlled trial. Mov Disord. 2020;35(12):2250–60.
Lolekha P, Sriphanom T, Vilaichone RK. Helicobacter pylori eradication improves motor fluctuations in advanced Parkinson’s Disease patients: a prospective cohort study (HP-PD trial). PLoS ONE. 2021;16(5):e0251042.
Çamcı G, Oğuz S. Association between Parkinson’s Disease and Helicobacter pylori. J Clin Neurol. 2016;12(2):147–50.
Yu CK, Wang CJ, Chew Y, Wang PC, Yin HS, Kao MC. Functional characterization of Helicobacter pylori 26695 sedoheptulose 7-phosphate isomerase encoded by hp0857 and its association with lipopolysaccharide biosynthesis and adhesion. Biochem Biophys Res Commun. 2016;477(4):794–800.
Beier EE, Neal M, Alam G, Edler M, Wu LJ, Richardson JR. Alternative microglial activation is associated with cessation of Progressive dopamine neuron loss in mice systemically administered lipopolysaccharide. Neurobiol Dis. 2017;108:115–27.
Park AM, Tsunoda I. Helicobacter pylori infection in the stomach induces neuroinflammation: the potential roles of bacterial outer membrane vesicles in an animal model of Alzheimer’s disease. Inflamm Regen. 2022;42(1):39.
Yang QY, Li XW, Yang R, Qin TY, Long H, Zhang SB, et al. Effects of intraperitoneal injection of lipopolysaccharide-induced peripheral inflammation on dopamine neuron damage in rat midbrain. CNS Neurosci Ther. 2022;28(10):1624–36.
Alhasson F, Das S, Seth R, Dattaroy D, Chandrashekaran V, Ryan CN, et al. Altered gut microbiome in a mouse model of Gulf War Illness causes neuroinflammation and intestinal injury via leaky gut and TLR4 activation. PLoS ONE. 2017;12(3):e0172914.
Perez-Pardo P, Dodiya HB, Engen PA, Forsyth CB, Huschens AM, Shaikh M, et al. Role of TLR4 in the gut-brain axis in Parkinson’s Disease: a translational study from men to mice. Gut. 2019;68(5):829–43.
Gray MT, Woulfe JM. Striatal blood-brain barrier permeability in Parkinson’s Disease. J Cereb Blood Flow Metab. 2015;35(5):747–50.
Figueroa-Hall LK, Paulus MP, Savitz J. Toll-like receptor signaling in depression. Psychoneuroendocrinology. 2020;121:104843.
Muta T, Takeshige K. Essential roles of CD14 and lipopolysaccharide-binding protein for activation of toll-like receptor (TLR)2 as well as TLR4 reconstitution of TLR2- and TLR4-activation by distinguishable ligands in LPS preparations. Eur J Biochem. 2001;268(16):4580–9.
Pahwa R, Devaraj S, Jialal I. The effect of the accessory proteins, soluble CD14 and lipopolysaccharide-binding protein on toll-like receptor 4 activity in human monocytes and adipocytes. Int J Obes. 2016;40(6):907–11.
Moreno C, Merino J, Ramírez N, Echeverría A, Pastor F, Sánchez-Ibarrola A. Lipopolysaccharide needs soluble CD14 to interact with TLR4 in human monocytes depleted of membrane CD14. Microbes Infect. 2004;6(11):990–5.
Smith SM, Freeley M, Moynagh PN, Kelleher DP. Differential modulation of Helicobacter pylori lipopolysaccharide-mediated TLR2 signaling by individual pellino proteins. Helicobacter 2017; 22(1).
Fellner L, Irschick R, Schanda K, Reindl M, Klimaschewski L, Poewe W, et al. Toll-like receptor 4 is required for α-synuclein dependent activation of microglia and astroglia. Glia. 2013;61(3):349–60.
Zhao Z, Ning J, Bao XQ, Shang M, Ma J, Li G, et al. Fecal microbiota transplantation protects rotenone-induced Parkinson’s Disease mice via suppressing inflammation mediated by the lipopolysaccharide-TLR4 signaling pathway through the microbiota-gut-brain axis. Microbiome. 2021;9(1):226.
Alexoudi A, Alexoudi I, Gatzonis S. Parkinson’s Disease pathogenesis, evolution and alternative pathways: a review. Rev Neurol. 2018;174(10):699–704.
Mukherjee A, Biswas A, Das SK. Gut dysfunction in Parkinson’s Disease. World J Gastroenterol. 2016;22(25):5742–52.
Bussell R Jr., Eliezer D. A structural and functional role for 11-mer repeats in alpha-synuclein and other exchangeable lipid binding proteins. J Mol Biol. 2003;329(4):763–78.
Bhattacharyya D, Mohite GM, Krishnamoorthy J, Gayen N, Mehra S, Navalkar A, et al. Lipopolysaccharide from gut microbiota modulates α-synuclein aggregation and alters its biological function. ACS Chem Neurosci. 2019;10(5):2229–36.
Arawaka S, Sato H, Sasaki A, Koyama S, Kato T. Mechanisms underlying extensive Ser129-phosphorylation in α-synuclein aggregates. Acta Neuropathol Commun. 2017;5(1):48.
He Y, Yu Z, Chen S. Alpha-synuclein nitration and its implications in Parkinson’s Disease. ACS Chem Neurosci. 2019;10(2):777–82.
Xu B, Wu SW, Lu CW, Deng Y, Liu W, Wei YG, et al. Oxidative stress involvement in manganese-induced alpha-synuclein oligomerization in organotypic brain slice cultures. Toxicology. 2013;305:71–8.
Collins LM, Toulouse A, Connor TJ, Nolan YM. Contributions of central and systemic inflammation to the pathophysiology of Parkinson’s Disease. Neuropharmacology. 2012;62(7):2154–68.
Wang L, Zhao Z, Zhao L, Zhao Y, Yang G, Wang C, et al. Lactobacillus plantarum DP189 reduces α-SYN aggravation in MPTP-induced Parkinson’s Disease mice via regulating oxidative damage, inflammation, and gut microbiota disorder. J Agric Food Chem. 2022;70(4):1163–73.
Dutta G, Zhang P, Liu B. The lipopolysaccharide Parkinson’s Disease animal model: mechanistic studies and drug discovery. Fundam Clin Pharmacol. 2008;22(5):453–64.
Liu B, Gao HM, Wang JY, Jeohn GH, Cooper CL, Hong JS. Role of nitric oxide in inflammation-mediated neurodegeneration. Ann N Y Acad Sci. 2002;962:318–31.
He JY, Li DD, Wen Q, Qin TY, Long H, Zhang SB, et al. Synergistic effects of lipopolysaccharide and rotenone on dopamine neuronal damage in rats. CNS Neurosci Ther. 2023;29(8):2281–91.
Li J, Baud O, Vartanian T, Volpe JJ, Rosenberg PA. Peroxynitrite generated by inducible nitric oxide synthase and NADPH oxidase mediates microglial toxicity to oligodendrocytes. Proc Natl Acad Sci U S A. 2005;102(28):9936–41.
Sanlioglu S, Williams CM, Samavati L, Butler NS, Wang G, McCray PB Jr., et al. Lipopolysaccharide induces Rac1-dependent reactive oxygen species formation and coordinates Tumor necrosis factor-alpha secretion through IKK regulation of NF-kappa B. J Biol Chem. 2001;276(32):30188–98.
Sawada M, Kondo N, Suzumura A, Marunouchi T. Production of Tumor necrosis factor-alpha by microglia and astrocytes in culture. Brain Res. 1989;491(2):394–7.
Hetier E, Ayala J, Denèfle P, Bousseau A, Rouget P, Mallat M, et al. Brain macrophages synthesize interleukin-1 and interleukin-1 mRNAs in vitro. J Neurosci Res. 1988;21(2–4):391–7.
Tombola F, Oregna F, Brutsche S, Szabò I, Del Giudice G, Rappuoli R, et al. Inhibition of the vacuolating and anion channel activities of the VacA toxin of Helicobacter pylori. FEBS Lett. 1999;460(2):221–5.
Ly PT, Pelech S, Shaw CA. Cholesteryl glucoside stimulates activation of protein kinase B/Akt in the motor neuron-derived NSC34 cell line. Neurobiol Lipids. 2008;7(4):620081.
Hsu CY, Yeh JY, Chen CY, Wu HY, Chiang MH, Wu CL, et al. Helicobacter pylori cholesterol-α-glucosyltransferase manipulates cholesterol for bacterial adherence to gastric epithelial cells. Virulence. 2021;12(1):2341–51.
Foegeding NJ, Caston RR, McClain MS, Ohi MD, Cover TL. An overview of Helicobacter pylori VacA toxin biology. Toxins 2016; 8(6).
Kunimoto S, Kobayashi T, Kobayashi S, Murakami-Murofushi K. Expression of cholesteryl glucoside by heat shock in human fibroblasts. Cell Stress Chaperones. 2000;5(1):3–7.
Kandel ES, Hay N. The regulation and activities of the multifunctional serine/threonine kinase Akt/PKB. Exp Cell Res. 1999;253(1):210–29.
Han H, Wang H, Long H, Nattel S, Wang Z. Oxidative preconditioning and apoptosis in L-cells. Roles of protein kinase B and mitogen-activated protein kinases. J Biol Chem. 2001;276(28):26357–64.
Alvarez-Tejado M, Naranjo-Suarez S, Jiménez C, Carrera AC, Landázuri MO, del Peso L. Hypoxia induces the activation of the phosphatidylinositol 3-kinase/Akt cell survival pathway in PC12 cells: protective role in apoptosis. J Biol Chem. 2001;276(25):22368–74.
Beigier-Bompadre M, Moos V, Belogolova E, Allers K, Schneider T, Churin Y. Modulation of the CD4 + T-cell response by Helicobacter pylori depends on known virulence factors and bacterial cholesterol and cholesterol α-glucoside content. J Infect Dis. 2011;204(9):1339–48.
de Brito BB, da Silva FAF, Soares AS, Pereira VA, Santos MLC, Sampaio MM, et al. Pathogenesis and clinical management of Helicobacter pylori gastric Infection. World J Gastroenterol. 2019;25(37):5578–89.
Chatterjee R, Chowdhury AR, Mukherjee D, Chakravortty D. Lipid Larceny: channelizing host lipids for establishing successful pathogenesis by bacteria. Virulence. 2021;12(1):195–216.
Yokoyama K, Higashi H, Ishikawa S, Fujii Y, Kondo S, Kato H, et al. Functional antagonism between Helicobacter pylori CagA and vacuolating toxin VacA in control of the NFAT signaling pathway in gastric epithelial cells. Proc Natl Acad Sci U S A. 2005;102(27):9661–6.
Backert S, Tegtmeyer N. The versatility of the Helicobacter pylori vacuolating cytotoxin vacA in signal transduction and molecular crosstalk. Toxins. 2010;2(1):69–92.
Czajkowsky DM, Iwamoto H, Cover TL, Shao Z. The vacuolating toxin from Helicobacter pylori forms hexameric pores in lipid bilayers at low pH. Proc Natl Acad Sci U S A. 1999;96(5):2001–6.
Wang HJ, Cheng WC, Cheng HH, Lai CH, Wang WC. Helicobacter pylori cholesteryl glucosides interfere with host membrane phase and affect type IV secretion system function during Infection in AGS cells. Mol Microbiol. 2012;83(1):67–84.
Tombola F, Carlesso C, Szabò I, de Bernard M, Reyrat JM, Telford JL, et al. Helicobacter pylori vacuolating toxin forms anion-selective channels in planar lipid bilayers: possible implications for the mechanism of cellular vacuolation. Biophys J. 1999;76(3):1401–9.
Iwamoto H, Czajkowsky DM, Cover TL, Szabo G, Shao Z. VacA from Helicobacter pylori: a hexameric chloride channel. FEBS Lett. 1999;450(1–2):101–4.
Szabò I, Brutsche S, Tombola F, Moschioni M, Satin B, Telford JL, et al. Formation of anion-selective channels in the cell plasma membrane by the toxin VacA of Helicobacter pylori is required for its biological activity. Embo j. 1999;18(20):5517–27.
Ricci V, Sommi P, Fiocca R, Romano M, Solcia E, Ventura U. Helicobacter pylori vacuolating toxin accumulates within the endosomal-vacuolar compartment of cultured gastric cells and potentiates the vacuolating activity of ammonia. J Pathol. 1997;183(4):453–9.
Morbiato L, Tombola F, Campello S, Del Giudice G, Rappuoli R, Zoratti M, et al. Vacuolation induced by VacA toxin of Helicobacter pylori requires the intracellular accumulation of membrane permeant bases, Cl(-) and water. FEBS Lett. 2001;508(3):479–83.
Forsyth MH, Atherton JC, Blaser MJ, Cover TL. Heterogeneity in levels of vacuolating cytotoxin gene (vacA) transcription among Helicobacter pylori strains. Infect Immun. 1998;66(7):3088–94.
Hisatsune J, Yamasaki E, Nakayama M, Shirasaka D, Kurazono H, Katagata Y, et al. Helicobacter pylori VacA enhances prostaglandin E2 production through induction of cyclooxygenase 2 expression via a p38 mitogen-activated protein kinase/activating transcription factor 2 cascade in AZ-521 cells. Infect Immun. 2007;75(9):4472–81.
Bohush A, Niewiadomska G, Filipek A. Role of mitogen activated protein kinase signaling in Parkinson’s disease. Int J Mol Sci 2018; 19(10).
Nakayama M, Kimura M, Wada A, Yahiro K, Ogushi K, Niidome T, et al. Helicobacter pylori VacA activates the p38/activating transcription factor 2-mediated signal pathway in AZ-521 cells. J Biol Chem. 2004;279(8):7024–8.
Nakayama M, Hisatsune J, Yamasaki E, Isomoto H, Kurazono H, Hatakeyama M, et al. Helicobacter pylori VacA-induced inhibition of GSK3 through the PI3K/Akt signaling pathway. J Biol Chem. 2009;284(3):1612–9.
Tombola F, Morbiato L, Del Giudice G, Rappuoli R, Zoratti M, Papini E. The Helicobacter pylori VacA toxin is a urea permease that promotes urea diffusion across epithelia. J Clin Invest. 2001;108(6):929–37.
Weiss G, Forster S, Irving A, Tate M, Ferrero RL, Hertzog P, et al. Helicobacter pylori VacA suppresses Lactobacillus acidophilus-induced interferon beta signaling in macrophages via alterations in the endocytic pathway. mBio. 2013;4(3):e00609–00612.
Hisatsune J, Nakayama M, Isomoto H, Kurazono H, Mukaida N, Mukhopadhyay AK, et al. Molecular characterization of Helicobacter pylori VacA induction of IL-8 in U937 cells reveals a prominent role for p38MAPK in activating transcription factor-2, cAMP response element binding protein, and NF-kappaB activation. J Immunol. 2008;180(7):5017–27.
Menaker RJ, Ceponis PJ, Jones NL. Helicobacter pylori induces apoptosis of macrophages in association with alterations in the mitochondrial pathway. Infect Immun. 2004;72(5):2889–98.
Fasano A, Bove F, Gabrielli M, Petracca M, Zocco MA, Ragazzoni E, et al. The role of small intestinal bacterial overgrowth in Parkinson’s Disease. Mov Disord. 2013;28(9):1241–9.
Dănău A, Dumitrescu L, Lefter A, Tulbă D, Popescu BO. Small intestinal bacterial overgrowth as potential therapeutic target in Parkinson’s Disease. Int J Mol Sci. 2021;22(21):11663.
Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG Clinical Guideline: treatment of Helicobacter pylori Infection. Am J Gastroenterol. 2017;112(2):212–39.
Enko D, Kriegshäuser G. Functional (13)C-urea and glucose hydrogen/methane breath tests reveal significant association of small intestinal bacterial overgrowth in individuals with active Helicobacter pylori Infection. Clin Biochem. 2017;50(1–2):46–9.
Liu W, Chen Y, Lu G, Sun L, Si J. Down-regulation of HSP70 sensitizes gastric epithelial cells to apoptosis and growth retardation triggered by H. Pylori. BMC Gastroenterol. 2011;11:146.
Dharan M, Wozny D. Helicobacter pylori Infection and small intestinal bacterial overgrowth-more than what meets the eye. World J Clin Cases. 2022;10(21):7209–14.
Konrad P, Chojnacki J, Gąsiorowska A, Rudnicki C, Kaczka A, Chojnacki C. Therapeutic efficacy of Amoxicillin and Rifaximin in patients with small intestinal bacterial overgrowth and Helicobacter pylori Infection. Prz Gastroenterol. 2018;13(3):213–7.
Pan I, Issac PK, Rahman MM, Guru A, Arockiaraj J. Gut-brain axis a key player to control gut dysbiosis in neurological Diseases. Mol Neurobiol 2023.
Machado AM, Figueiredo C, Seruca R, Rasmussen LJ. Helicobacter pylori Infection generates genetic instability in gastric cells. Biochim Biophys Acta. 2010;1806(1):58–65.
Chiozzi V, Mazzini G, Oldani A, Sciullo A, Ventura U, Romano M, et al. Relationship between Vac A toxin and ammonia in Helicobacter pylori-induced apoptosis in human gastric epithelial cells. Biochim Biophys Acta. 2009;60(3):23–30.
Chen C, Turnbull DM, Reeve AK. Mitochondrial dysfunction in Parkinson’s disease-cause or consequence? Biology. 2019;8(2):38.
McWilliams TG, Muqit MM. PINK1 and parkin: emerging themes in mitochondrial homeostasis. Curr Opin Cell Biol. 2017;45:83–91.
Wanitschke R, Ammon HV. Effects of dihydroxy bile acids and hydroxy fatty acids on the absorption of oleic acid in the human jejunum. J Clin Invest. 1978;61(1):178–86.
Nucera G, Gabrielli M, Lupascu A, Lauritano EC, Santoliquido A, Cremonini F, et al. Abnormal breath tests to lactose, fructose and sorbitol in irritable bowel syndrome may be explained by small intestinal bacterial overgrowth. Aliment Pharmacol Ther. 2005;21(11):1391–5.
Lomax AE, Linden DR, Mawe GM, Sharkey KA. Effects of gastrointestinal inflammation on enteroendocrine cells and enteric neural reflex circuits. Auton Neurosci. 2006;126–127:250–7.
Kountouras J, Deretzi G, Gavalas E, Zavos C, Polyzos SA, Kazakos E, et al. A proposed role of human defensins in Helicobacter pylori-related neurodegenerative disorders. Med Hypotheses. 2014;82(3):368–73.
Richmond AM, Lyons KE, Pahwa R. Safety review of current pharmacotherapies for levodopa-treated patients with Parkinson’s Disease. Expert Opin Drug Saf. 2023;22(7):563–79.
Si Q, Gan C, Zhang H, Cao X, Sun H, Wang M, et al. Altered dynamic functional network connectivity in levodopa-induced dyskinesia of Parkinson’s Disease. CNS Neurosci Ther. 2023;29(1):192–201.
Nyholm D, Hellström PM. Effects of Helicobacter pylori on Levodopa Pharmacokinetics. J Parkinsons Dis. 2021;11(1):61–9.
Zhong R, Chen Q, Zhang X, Li M, Lin W. Helicobacter pylori Infection is associated with a poor response to levodopa in patients with Parkinson’s Disease: a systematic review and meta-analysis. J Neurol. 2022;269(2):703–11.
Lee WY, Yoon WT, Shin HY, Jeon SH, Rhee PL. Helicobacter pylori Infection and motor fluctuations in patients with Parkinson’s Disease. Mov Disord. 2008;23(12):1696–700.
Lahner E, Virili C, Santaguida MG, Annibale B, Centanni M. Helicobacter pylori Infection and Drugs malabsorption. World J Gastroenterol. 2014;20(30):10331–7.
Niehues M, Hensel A. In-vitro interaction of L-dopa with bacterial adhesins of Helicobacter pylori: an explanation for clinicial differences in bioavailability? J Pharm Pharmacol. 2009;61(10):1303–7.
Liu B, Dong J, Wang S, Yu H, Li Z, Sun P, et al. Helicobacter pylori causes delayed gastric emptying by decreasing interstitial cells of Cajal. Exp Ther Med. 2021;22(1):663.
Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L. Clinical guideline: management of gastroparesis. Am J Gastroenterol. 2013;108(1):18–37. quiz 38.
Yan S, Yue YZ, Wang XP, Dong HL, Zhen SG, Wu BS et al. Aqueous extracts of herba cistanche promoted intestinal motility in loperamide-induced constipation rats by ameliorating the interstitial cells of Cajal. Evid Based Complement Alternat Med 2017; 2017:6236904.
Blair PJ, Hwang SJ, Shonnard MC, Peri LE, Bayguinov Y, Sanders KM, et al. The role of prostaglandins in disrupted gastric motor activity associated with type 2 Diabetes. Diabetes. 2019;68(3):637–47.
Yang S, Wu B, Sun H, Sun T, Han K, Li D, et al. Impaired insulin/IGF-1 is responsible for diabetic gastroparesis by damaging myenteric cholinergic neurones and interstitial cells of Cajal. Biosci Rep. 2017;37(5):BSR20170776.
Zhao J, An J, Liu S. Electroacupuncture at ST36 increases bone marrow-derived interstitial cells of Cajal via the SDF-1/CXCR4 and mSCF/Kit-ETV1 pathways in the stomach of diabetic mice. Evid Based Complement Alternat Med 2018; 2018:7878053.
** QH, Shen HX, Wang H, Shou QY, Liu Q. Curcumin improves expression of SCF/c-kit through attenuating oxidative stress and NF-κB activation in gastric tissues of diabetic gastroparesis rats. Diabetol Metab Syndr. 2013;5(1):12.
Zhou J, O’Connor MD, Ho V. The potential for gut organoid derived interstitial cells of Cajal in replacement therapy. Int J Mol Sci. 2017;18(10):2059.
Tan YY, Ji ZL, Zhao G, Jiang JR, Wang D, Wang JM. Decreased SCF/c-kit signaling pathway contributes to loss of interstitial cells of Cajal in gallstone Disease. Int J Clin Exp Med. 2014;7(11):4099–106.
Gao J, Wang Q, Tang YD, Zhai J, Hu W, Zheng C. When ferroptosis meets pathogenic Infections. Trends Microbiol. 2023;31(5):468–79.
Feng J, Gao J, Zhou S, Liu Y, Zhong Y, Shu Y, et al. Role of stem cell factor in the regulation of ICC proliferation and detrusor contraction in rats with an underactive bladder. Mol Med Rep. 2017;16(2):1516–22.
El-Omar EM. Mechanisms of increased acid secretion after eradication of Helicobacter pylori Infection. Gut. 2006;55(2):144–6.
McNamara D, El-Omar E. Helicobacter pylori Infection and the pathogenesis of gastric cancer: a paradigm for host-bacterial interactions. Dig Liver Dis. 2008;40(7):504–9.
Lyte M. Microbial endocrinology as a basis for improved L-DOPA bioavailability in Parkinson’s patients treated for Helicobacter pylori. Med Hypotheses. 2010;74(5):895–7.
Doherty NC, Tobias A, Watson S, Atherton JC. The effect of the human gut-signalling hormone, norepinephrine, on the growth of the gastric pathogen Helicobacter pylori. Helicobacter. 2009;14(3):223–30.
Pfeiffer RF, Isaacson SH, Pahwa R. Clinical implications of gastric Complications on levodopa treatment in Parkinson’s Disease. Parkinsonism Relat Disord. 2020;76:63–71.
Fotiadis D, Kanai Y, Palacín M. The SLC3 and SLC7 families of amino acid transporters. Mol Aspects Med. 2013;34(2–3):139–58.
Jost WH. Gastrointestinal dysfunction in Parkinson’s Disease. J Neurolo Sci. 2010;289(1):69–73.
Funding
This study was supported by the National Natural Science Foundation of China (No. 82160690), Science and Technology Foundation of Guizhou Province (No. ZK[2021]-014) and Collaborative Innovation Center of Chinese Ministry of Education (No. 2020-39).
Author information
Authors and Affiliations
Contributions
WBR and ZF designed the review. WBR drafted the manuscript. CYF and HC designed the figures. ZYJ and ZF revised the review. All authors approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wei, Br., Zhao, Yj., Cheng, Yf. et al. Helicobacter pylori infection and Parkinson’s Disease: etiology, pathogenesis and levodopa bioavailability. Immun Ageing 21, 1 (2024). https://doi.org/10.1186/s12979-023-00404-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12979-023-00404-1