Abstract
The gradual deterioration of the supporting periodontal tissues caused by periodontitis, a chronic multifactorial inflammatory disease, is thought to be triggered by the colonization of dysbiotic plaque biofilms in a vulnerable host. One of the most prevalent dental conditions in the world, periodontitis is now the leading factor in adult tooth loss. When periodontitis does develop, it is treated by scra** the mineralized deposits and dental biofilm off the tooth surfaces. Numerous studies have shown that non-surgical treatment significantly improves clinical and microbiological indices in individuals with periodontitis. Although periodontal parameters have significantly improved, certain bacterial reservoirs often persist on root surfaces even after standard periodontal therapy. Periodontitis has been treated with local or systemic antibiotics as well as scaling and root planning. Since there aren't many brand-new antibiotics on the market, several researchers are currently concentrating on creating alternate methods of combating periodontal germs. There is a delay in a study on the subject of nanoparticle (NP) toxicity, which is especially concerned with mechanisms of action, while the area of nanomedicine develops. The most promising of them are metal NPs since they have potent antibacterial action. Metal NPs may be employed as efficient growth inhibitors in a variety of bacteria, making them useful for the treatment of periodontitis. In this way, the new metal NPs contributed significantly to the development of efficient anti-inflammatory and antibacterial platforms for the treatment of periodontitis. The current therapeutic effects of several metallic NPs on periodontitis are summarized in this study. This data might be used to develop NP-based therapeutic alternatives for the treatment of periodontal infections.
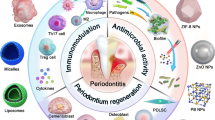
Graphical Abstract

Similar content being viewed by others
Introduction
Before the turn of the century, people often used the word “pyorrhea” to describe periodontal disease, which is characterized by pus, periodontal pockets, bone loss, and tooth loss. It was generally accepted that pyorrhea and the subsequent tooth loss were natural consequences of becoming older. Periodontal disease has become more important as a root cause of tooth loss in recent years, especially while the prevalence of dental caries has decreased in the general population. As the number of teeth lost to caries declines, the number of teeth at risk of periodontal disease rises [1]. Deterioration of periodontal ligaments (PDLs), the development of periodontal pockets, and the resorption of alveolar bone are hallmarks of periodontitis, an inflammatory disease of the gums that destroys the foundation on which teeth rest. Pockets may get infected with periodontitis because of the proliferation of microflora, especially anaerobes, which produce toxins, enzymes, and immune system stimulation [2]. This is often linked to a variety of clinical diseases, including gum inflammation (gingivitis), PDL and dental cementum deterioration, and loss of alveolar bone. The disease's early stage, gingivitis, may evolve into periodontitis, a more serious illness that manifests as the growth of cavities, a loss of clinical connection, and the deterioration of alveolar bone [3]. The use of pharmacological medicines, mechanical therapy, and surgical intervention are only a few of the several methods used to treat illness. Antimicrobials that alter the microbial flora in the periodontal milieu and host response modulating agents that alter host responses like lowering excessive enzyme levels, cytokines, prostaglandins, and osteoclast activity are among the medications specifically used for improving the management of periodontitis [4]. Osteoclasts, osteoblasts, and bone marrow stromal cells were traditionally considered to regulate bone loss in periodontitis. In addition to starting the physiological bone remodeling, osteocytes have recently been discovered to help in inflammation-related bone remodeling [5]. Evidence from recent case–control and cross-sectional studies suggests that periodontitis may raise the chance of having a prematurely born baby with a low birth weight by a factor of seven, and the risk of cardiovascular disease by a factor of two. These preliminary studies suggest a possible connection between general and oral health. Evidence from this research also lends credence to the idea that periodontal disease is the result of an inflammatory response from the host on both the local and systemic levels [6]. Without treatment, periodontitis, an inflammatory condition caused by bacteria, destroys the tissues around your teeth and eventually forces you to lose them. An imbalance between the host's immunological protection and immune destruction processes is a major contributor to periodontal tissue deterioration. To restore the physiological structure and function of the periodontium, periodontal treatment seeks to reduce inflammation, and repair and regenerate hard and soft tissues. Thanks to recent developments in nanotechnology, immunomodulatory nanoparticles (NPs) may now be used in regenerative dental procedures [7].
NPs can efficiently enter biological organisms due to their very tiny size. The effective and targeted delivery of medications, genes, and therapeutic chemicals to specific organs or cells, imaging, and precise identification of viruses at early stages are only a few examples of the many applications of nano biomedical expertise. NPs also play a crucial role in antiviral therapy by improving the efficacy of medicine use and facilitating the transfer of hydrophobic drugs [8,9,10]. Due to their small size (1–100 nm), NPs can easily pass through even the smallest blood capillaries and avoid being phagocytized, which increases their plasma half-life and allows for a more gradual release of the drug. The NPs may be classified as either “organic” or “inorganic”. Polymers, dendrimers, micelles, liposomes, and lipids are all examples of organic materials; silver (Ag), gold (Au), iron oxide, zinc oxide (ZnO), and silica are all examples of inorganic materials [9]. NPs have several uses, including medication delivery at a precise point, sensors, pharmaceuticals to combat cancer, antioxidants, larvicides, Nanofluids, antibacterial agents in dentistry, mouthwashes, the treatment of white spot lesions during orthodontic therapy, and more. Since the size reduction limits the electron movements, NPs have superior optical characteristics compared to bulk metals. They are less hazardous and have a high surface-to-volume ratio because of their very tiny size. Therefore, quicker absorption and a relatively greater drug loading arise from interactions at the surface. NPs' increased antibacterial action may be attributed to their huge surface area and high charge density, which allows them to interact with the negatively charged surface of bacterial cells [11]. Nanotechnology has a wide variety of potential dental applications. Nano-products, regenerative dentistry, periodontics, implantology, periodontal therapy, endodontics, prosthodontics, conservative and cosmetic dentistry, orthodontics, and endodontics are all part of the dental care industry. Dental equipment, such as LED light curing units, dental hard tissue protection against acid-containing meals, dental material characterization, and dental hard tissue characterization, all rely heavily on nanotechnology [12]. Biomineralization is sparked by metallic NPs, which promote the remineralization of demineralized (caries-ridden) dental tissues. In addition, because of their ion balance in oral fluid, metallic NP may triumph over obstacles under a wide variety of oral circumstances. Many different nano-formulations have been studied by academics and clinicians for their ability to reduce caries [13]. In addition, there's evidence that metal NPs may inhibit the growth of harmful germs. Numerous studies have been conducted so far on the efficacy of various metal NPs against pathogenic microorganisms [14]. Metal NPs, according to several studies, are an appealing new approach to treating periodontitis because of their ability to enhance the photothermal characteristics and anti-inflammatory action of materials [15]. Metal NPs, which have antibacterial and anti-inflammatory characteristics, are also being considered as potential periodontitis treatments. For instance, a dose- and time-dependent increase in cytotoxicity was seen in human periodontal fibroblasts exposed to silver NPs (AgNPs) smaller than 20 nm [16, 17]. In this paper, we discussed metal NPs, which are useful in the treatment of periodontitis.
Development factors of periodontitis
It was predicted that by 2020, almost 62% of dentate individuals will have periodontitis, with a further 23.6% suffering from severe periodontitis. When compared to estimates provided between 1990 and 2010, these findings reveal an alarmingly high frequency of periodontitis [18]. Inflammation of the gums and loss of alveolar bone that supports teeth characterize periodontitis, the most prevalent oral illness. Plaque biofilm on the dental and gingival surfaces is the primary cause of periodontal disease, which in turn is governed by unclean behavioral factors, the internal milieu of the oral cavity, and the production of dental and gingival plaque. Inducing host immune responses that harm gingival tissues and resorb bone, Porphyromonas gingivalis (P. gingivalis) is the main keystone pathogen of the periodontal biofilm [19]. Demineralization and destruction of tooth hard tissues characterize dental caries, also known as tooth decay, which may advance to inflame and destroy the soft tissues around the teeth, leading to periodontitis. There are several potential causes of dental caries and periodontal disease. The oral microbiome has been examined extensively, both in healthy people and those with diseases. The oral cavity is home to bacteria from at least 13 distinct phyla: Actinobacteria, Bacteroidetes, Chloroflexi, Firmicutes, Fusobacteria, Proteobacteria, Spirochaetes, Synergistetes, Tenericutes, and the as-yet-unnamed SR1 and TM7 [20]. It indicates that the number of spirochetes present in subgingival plaque is proportional to the clinical stage of periodontal disease. The exact number of spirochetal species that colonize the plaque is unknown, but we can tell that there are three sizes of spirochetes: tiny, medium, and giant. Among the four cultivable species of tiny spirochetes, Treponema denticola (T. denticola) is the only one that has been proven to contain proteolytic and keratinolytic enzymes, as well as factors or processes that reduce lymphocyte blastogenesis and inhibit fibroblast and polymorphonuclear leukocyte (PMNL) activity. Periodontal tissue injury may result from any or all of these factors [21]. An individual’s reaction to periodontal infection is significantly influenced by risk factors. Lifestyle variables, such as smoking and alcohol intake, are examples of these separate but changeable risk factors for periodontal disease. Conditions including diabetes mellitus, obesity, metabolic syndrome, osteoporosis, and inadequate calcium and vitamin D intake are also included. The modern treatment of many periodontal patients includes the control of these modifiable risk factors. Because of the role played by genetic variables, it is possible to target people for periodontal disease prevention and early diagnosis. Aggressive periodontitis has a definite hereditary component. Despite widespread speculation that some genes may play a role in the development of chronic adult periodontitis, no definitive evidence linking these two conditions has been found [22].
Periodontitis treatment methods
In most cases, opportunistic infections are the root cause of periodontal disease. Due to the infection caused by bacteria in a biofilm that is resistant to antimicrobials and the body’s natural defenses, periodontal disease is difficult to treat. It is a time-consuming process to eliminate the germs from the periodontal cavity, and the bacteria persist after treatment. The germs present and the host's reaction both play major roles in determining the severity of the illness [23]. Gingival swelling, bleeding gums, and bad breath are all symptoms of periodontitis, which begins as a gingival (gingivitis) inflammation and progresses into deeper tissues. Pockets arise when alveolar bone resorbs, gingival epithelial tissue migrates, and degenerating collagen in the periodontium provides less support for the teeth. Therefore, the progression of the condition determines the therapeutic approach that will be used [24]. Teeth might become loose and fall out if this condition is not corrected. Inflammation and degeneration of the gums, PDL, and cementum (the substance that holds teeth in place) are hallmarks of this condition. Periodontal pockets are created when gingival epithelium migrates along the tooth surface. These pockets are a fertile breeding ground for bacteria. The teeth get loose and eventually fall out in the latter stages. Local delivery offers the benefit of producing larger medication concentrations at the desired site of action while requiring lower dosages, which results in a decrease in harmful and side effects. For instance, syringes, irrigation tools, dental gels, mouthwashes, and gentrifiers. Due to the drug's brief interaction with tissues and inadequate penetration into the periodontal pocket, mouth rinses, and dental treatments are regarded as ineffective. Dental irrigation aids in the decrease of dental plaque and subgingival bacteria [25]. The primary objective of periodontitis treatment is to halt the progression of the disease, thereby decreasing the likelihood of tooth loss, alleviating symptoms and the perception of the disease, potentially restoring lost periodontal tissue, and offering guidance on maintaining a healthy periodontium. Therapeutic intervention encompasses the implementation of strategies aimed at modifying behavior, including personalized oral hygiene instructions, smoking cessation programs, dietary modifications, subgingival instrumentation for plaque and calculus removal, local and systemic pharmacotherapy, as well as diverse surgical procedures. There is no definitive evidence to support the superiority of any specific treatment option, and nearly all forms of mechanical periodontal treatment experience positive effects when combined with adjunctive antimicrobial chemotherapy [26]. By stop** the chronic inflammatory process that leads to the loss of periodontal attachment, alveolar bone, and the development of periodontal pockets, periodontal treatment aims to retain the natural dentition. Periodontitis' etiology and pathogenesis are now understood to be the consequence of a complex interaction between bacterial aggressiveness and host defense, which is influenced by behavioral and systemic risk factors. Since only treatments that mechanically disrupt subgingival biofilms are effective, maintaining periodontal health requires that patients adequately manage their plaque and that professionals do periodic professional prophylaxis [27]. Fluorides are often utilized, and their antiseptic qualities help lessen gingivitis and bacterial buildup. Antibiotic usage may lessen periodontal disease occurrence and severity [28]. Chlorhexidine (CHX) gluconate is a frequently employed antimicrobial compound that is utilized in conjunction with mechanical periodontal therapy. Typically, it is administered in the form of an oral rinse; however, alternative applications include gel, varnish, and subgingival chip formulations. The utilization of CHX, in conjunction with routine tooth brushing, has the potential to result in a decrease in the accumulation of dental plaque, thereby offering significant advantages in the management of chronic periodontitis. Pharmacotherapy for periodontal disease has witnessed a recent emergence as a notable advancement. The CHX gluconate chip is introduced into the periodontal pocket after the completion of the cleaning procedure, facilitating a protracted and controlled discharge of CHX gluconate within the targeted region. Systemic antibiotics are occasionally necessary, however, they are uncommon, as in the case of chronic deep periodontal pockets. Tetracyclines, penicillin, macrolides, quinolones, cephalosporins, and nitroimidazole compounds are the most often prescribed antimicrobial drugs. These pharmaceutical treatments can be provided to patients with a variety of susceptible germs, including some that are resistant to antibiotics, and they all have different mechanisms of action. These medications can also be administered separately or in combination to increase their potential uses [29, 30]. Following invasive periodontal operations, patients are frequently prescribed antibiotics as a preventative measure. Antibiotic resistance has, however, recently grown in patients with periodontal disease, in line with the general trend of rising antimicrobial resistance in human pathogens. These bacteria are less vulnerable to antibiotics because of the particular periodontal environment and biofilm production. To treat periodontal disorders, new treatment approaches are required [31, 32]. In addition to controlling supragingival plaque, manual, sonic, and/or ultrasonic instrumentation is another non-surgical periodontal therapy option. It was discovered that subgingival debridement was a successful therapy for lowering the depth of the probing pocket and raising the clinical attachment level. Treatment reduces the depth of the pocket because the gingiva recedes and the clinical attachment level rises. The therapy is deemed effective when a pocket depth of less than or equal to 5mm is attained. Periodontal treatment is negatively impacted by patient-related variables like smoking status and the severity of the illness. Endodontic therapy and tooth type are two site-specific variables that may affect the result. There is a distinction between single-rooted and multi-rooted teeth with the potential for furcation involvement about tooth type, which is a challenge for the effective treatment of molars [33]. In addition, the removal of the periodontal pocket and the clearing of the subgingival infection are regarded as essential in the treatment of periodontitis. It seems that periodontal disease can be treated well in as little as one to three days, albeit this does not prevent the illness from being recolonized and returning. It's possible that utilizing many modes of administration simultaneously yields the best results. The utilization of a short-acting biodegradable system as an initial treatment may prove advantageous in delivering a bactericidal concentration of the antibacterial agent directly to the periodontal pocket. The continued and extended administration of antibacterial agents to the vicinity surrounding the opening of the pocket can potentially hinder the re-establishment of bacteria in the pocket from the oral cavity by suppressing the formation of plaque at the margins [27, 34].
Periodontitis would be brought on by the oral pathogenic bacteria' biofilm, which is brought on by their coaggregation and growth. Individual bacteria are encased in biofilms by extracellular polymeric substances (EPS), acting as a barrier to keep them safe from harm. Disrupting the EPS of pathogenic bacteria is essential and problematic for the treatment of periodontal disease. Researchers assumed that our specially developed cationic dextrans may be effective in treating periodontitis based on their ability to sufficiently disorganize EPS. Researchers confirmed that cationic dextrans may cause EPS biofilms, particularly those containing P. gingivalis, a major periodontal pathogen, to undergo a phase shift, thereby eliminating the biofilm in vitro. More significantly, a rat model of periodontal disease had a favorable in vivo therapy. In conclusion, the research took use of the substantial biofilm-controlling ability of cationic dextrans to treat periodontitis practically and successfully [35]. Despite being the Au standard for treating periodontal disease, non-surgical periodontal therapy (NSPT) might nevertheless provide subpar outcomes because of anatomical and microbiological restrictions. Probiotic usage as a supplement to non-surgical periodontal therapy may be able to enhance periodontal clinical parameters for up to three months, according to limited data [36]. Nevertheless, the current dental materials, instruments, and procedures exhibit limitations in terms of their efficacy and precision in targeting microbial pathogens, particularly in reaching deep periodontal pockets. Nano-drug delivery systems present a sophisticated approach to drug delivery in the context of periodontitis, exhibiting efficacy against pathogens that have developed resistance. NPs have been widely utilized in diverse dental applications owing to the distinctive characteristics that render them appropriate for drug delivery purposes. The small dimensions of NPs enable targeted drug delivery to specific tissues, cells, or pathogens within the periodontal pockets. Furthermore, they exhibit antimicrobial properties through the disruption of bacterial cell membranes, resulting in the eradication of bacteria. The utilization of inorganic NPs offers several benefits, including their notable surface-to-volume ratios, diverse shapes, numerous structural defects, such as irregularities in the crystal lattice of nanostructured bismuth oxide, and their nanoscale dimensions. These attributes enable a greater number of active sites for interaction with various biological systems, such as bacteria, fungi, and viruses. The primary distinction between NPs and conventional organic molecular antimicrobial agents lies in their significance, as it has the potential to mitigate the emergence of antimicrobial resistance [37,38,39,40]. In Fig. 1, we have shown the provoking factors of periodontal disease and the methods of non-surgical treatment of periodontitis.
Factors that stimulate periodontal disease, such as biofilm dysbiosis, uncontrolled gingival and periodontal inflammatory reactions, psychological stress paralleled by increased cortisol discharge, and harmful foods defined by high carbohydrate consumption. Dental plaque and calculus accumulate at the tooth-gingiva margin and extend subgingivally. The activities of subgingival plaque and host protection result in inflammation and tissue injury. The gingiva becomes detached from the root surface, creating a periodontal pocket, which is extremely anaerobic and allows additional expansion and development of subgingival plaque. Increasingly severe destruction of tissues results in the gradual recession of the supporting alveolar bone [41, 42]
Metal nanoparticles in periodontitis
Generally, smaller NPs tend to be more effective in killing germs. However, bigger NPs have been proven to be more effective in other trials, suggesting that size is not the primary determinant of toxicity. The formulation procedure, the surrounding conditions, the bacterial resistance mechanism, and the NP’s physical properties are all additional variables [43]. The antibacterial effect of distinct transient metal and metal oxide NPs has been shown against a wide range of Gram-negative and Gram-positive bacteria, including pathogens and those resistant to standard antibacterial drugs. Therefore, NPs may be used in nanotechnology to inhibit bacterial development and in biomedicine to remedy a wide range of illnesses [44]. There has been a lot of interest in the possible antibacterial properties of various NPs and their derivatives. Antimicrobial activity in metal NPs was discovered, including gold Au, Ag, Ag oxide (Ag2O), titanium dioxide (TiO2), silicon (Si), copper oxide (CuO), ZnO, Au, calcium oxide (CaO), and magnesium oxide (MgO) [45]. The reactive oxygen species (ROS) generated by these NPs are toxic to microbes because they may degrade DNA, RNA, and proteins. Since their antibacterial action does not rely on ROS, it seems that Au NPs are less toxic to mammalian cells than the other nanometals. Additionally, the great functionalization potential of these NPs makes them suitable nanomaterials for use as targeted antibacterial agents. In addition, the antibacterial efficacy of ZnONPs is enhanced by their excellent photocatalytic activities. ROS are also produced by ZnONPs when exposed to UV radiation [46]. To do their part, metal NPs eliminate the biofilm. An essential contributor to the resurgence of drug-resistant bacteria that has resulted in a dramatic rise in mortality and morbidity and a drawn-out treatment cycle is the development of biofilms [47, 48]. Furthermore, the metal ions released by these NPs kill bacterial DNA and protein. In the case of metal NPs, the positive metal ions interact with the negative membrane charges of microorganisms. Metal ions can cross the membrane of bacteria and enter the cells. They prevent protein and nucleic acid production by reacting with the sulfhydryl group (–SH) on microbial proteins. NPs’ antibacterial efficacy is dependent on their size and surface charge. Excellent antibacterial effects are achieved with no degradation of the material's mechanical qualities because of their reduced particle size and higher surface-to-volume ratio. The release of the loaded antibacterial chemical is another way for killing bacteria, in addition to the one described above that involves direct contact with NPs [48]. The antibacterial mechanisms of metal NPs are summarized in Fig. 2. In addition to being a leading cause of adult tooth loss, periodontitis has been linked to the chronic activation of the host immune system and has been shown to have bidirectional effects with various systemic disorders such as diabetes, cardiovascular disease, digestive disease, and cancer. Therefore, protecting and restoring periodontal health is crucial to overall wellness. Therefore, it is crucial to find a way to treat periodontitis that is both more successful and less intrusive [122, 123]. In a few investigations, NiNPs were shown to exhibit anti-microbial properties against bacteria like S. aureus and E. coli. In this investigation, researchers used S. epidermidis clinical isolates to test the hemolytic impact of NiNPs on human red blood cells (RBC) and the inhibitory effect of NiNPs on biofilm development. All S. epidermidis clinical isolates were shown to be capable of biofilm generation in this investigation. The production of biofilm was shown to be suppressed by NiNPs. The coagulase-negative staphylococci group includes S. epidermidis, a Gram-positive coccus. It is the main source of infection in artificial heart valves, prosthetic joints, vascular grafts, intra-cardiac devices, and cerebrospinal fluid shunts. The ability to form biofilms, polysaccharide intercellular adhesion (PIA), biofilm-associated protein, poly-glutamic acid (PGA), staphylococcal enterotoxin-like toxin L (SEIL), and C3 enterotoxin (SEC3), phenol-soluble modulins (PSMs), Clpxp, and extracellular matrix-binding protein are all examples of virulence factors [124]. Biofilms are multicellular, surface-attached collections of bacteria that exhibit unique physiologic and architectural features, making them resistant to several types of antibiotics, including penicillin, aminoglycosides, quinolones, and various host defense mechanisms. The concentration of antibiotics needed to kill bacteria in a biofilm is one thousand times greater than the concentration needed to kill the same bacterium in a planktonic form [125]. However, NiNPs' potential for inhibiting biofilm formation has never been studied. This research set out to determine whether Ni-NPs might inhibit biofilm formation in S. epidermidis from a clinical setting. Furthermore, the equivalent hemolytic impact on human RBC was examined to ascertain the dangers of NiNPs for systemic application in live beings. While NiNPs' antimicrobial efficacy has been shown elsewhere, their potential to disrupt biofilms has not yet been explored. In patients with catheters or other surgical implants, S. epidermidis is a prevalent source of hospital-acquired infection. S. epidermidis’s ability to form biofilm is likely a contributing element to its infectiousness. Since S. epidermidis's capacity to form biofilms on viable and non-viable surfaces, notably on plastic devices, is its key virulence factor, the current research aimed to ascertain whether or not NiNPs might suppress the biofilm formation of S. epidermidis clinical isolates [61]. A novel Ni(II)-containing coordination complex has been successfully created by researchers via a solvothermal process. According to the findings, the substance significantly inhibits the growth of P. gingivalis biofilm. In conclusion, the substance effectively combats periodontal disease by preventing the growth of P. gingivalis biofilm [126]. The commonly used standard human pathogens S. aureus and E. coli were utilized to investigate the antibacterial activity of copper (Cu), Ni, and bimetallic Cu-Ni NPs. These NPs were further examined against the dental pathogen S. mutans. When it comes to S. aureus, E. coli, and S. mutans, CuNPs demonstrate a bactericidal impact whereas NiNPs and bimetallic Cu-Ni NPs only have a bacteriostatic effect. Cu-Ni-NPs are anticipated to demonstrate unique effectiveness against periodontitis-related bacteria or to prevent the production of biofilm [127].
Bismuth nanoparticle
Despite the well-documented therapeutic usage of the bismuthcomplex, very few investigations have focused on the medicinal uses of bismuth NPs (BiNPs). Bactericidal, fungicidal, antiparasitic, and antibiofilm characteristics of metallic bismuth NPs have also been investigated. Toxicological data on these NPs have been acquired, however, they are not yet adequate to warrant their use in human clinical trials [128, 129]. Numerous publications discuss the creation of non-metallic BiNPs such as bismuth oxide, bismuth sulfide, bismuth selenide, and bismuth telluride as well as its use in biomedicine [130]. Therefore, due to their unique features, Bi2O3 NPs may have uses in the medical, dental, and aesthetic fields. Among them are their affordability and scalability, high stabilization, chemical inertness, nontoxicity, compatibility with biological systems, and active characteristics [131]. The emergence of a new strategy for the treatment of dental caries, oral infection, and infection related to the oral cavity, such as endocarditis and septicemia, is crucial and essential due to the high side effect of routine drugs used for oral infection, low efficacy, drug resistance, and use as a mouthwash, which could cause sensitivity and have low efficacy. To get around this issue, researchers used BiNPs. A recent study suggests that BiNPs might replace existing drugs or be used as a mouthwash to treat oral infections due to their low MIC, good effectiveness, and cheap cost [132]. BiNPs’ ability to stop S. mutans, the bacteria responsible for most cases of tooth decay, from forming biofilms is one of its defining features. Due to the electrostatic interaction between a negatively charged cell membrane and the positively charged NPs, it has been shown that positive charges on the metal ion are essential for antimicrobial activity. DNA damage, changes in gene expression, and effects on membrane-bound respiratory enzymes are among the other negative effects of AgNPs that have been documented [133]. Bismuth combined with a lipophilic dithiol (3-dimercapto-1-propanol, BAL) in a 2:1 molar ratio strongly inhibited the production of EPS by Brevundimonas diminuta (B. diminuta) in suspended cultures at concentrations slightly below the MIC. After 5 days of exposure to bismuth-BAL chelate (BisBAL) at near MIC (12 M), total polysaccharides and proteins released by B. diminuta reduced by nearly 95%. The suppression of carbohydrate O-acetylation was hypothesized to be one mechanism by which BisBAL disrupts biofilms using Fourier-transform infrared spectroscopy (FTIR). FTIR analysis also showed striking similarities between EPS samples treated and untreated with BisBAL, with protein, polysaccharide, and peptide expression levels being the main difference [134]. Nanomaterials have recently been used in the area of dentistry and medicine as a novel, alternative antibacterial agents. Bismuth subsalicylate (BSS) has been utilized as an antibacterial agent, but its potential efficacy against the bacteria that cause periodontal disease has not been specifically studied in the form of NPs (BSS-nano). This research aimed to analyze the safety of BSS-nano by analyzing their cytotoxicity in HGF-1 cells and the antibacterial efficacy of BSS-nano against oral anaerobic bacteria. It was shown that BSS-nano has a polygonal form and a main size of 4–22 nm. Dental materials and antiseptic solutions may use BSS-nano as an antibacterial agent [135]. Zerovalent BiNPs’ antibacterial effects have been the subject of preliminary but encouraging studies. They were just as successful in halting the spread of S. mutans as CHX. It is critical to keep in mind that zero-valent BiNPs have a 0.5 mM MIC for the inhibition of bacterial growth when thinking about including them in mouthwash. In the tests that have been done, CHX, the industry standard for oral antiseptics, has been demonstrated to have similar effects to these NPs. The introduction of zerovalent BiNPs completely stopped S. mutans from producing biofilm. This result was surprising since zero-valent BiNPs were anticipated to have an inhibitory effect on cell growth but not a complete block. Researchers hypothesized that because 69% of the cells were rendered inactive by NPs, there wouldn’t be enough cells left to form a biofilm. The majority of the experimental evidence points to these NPs as a potential treatment for bacterial infections based on biofilms [62].
To create innovative medicinal molecules with antibacterial capabilities for the treatment of various mouth illnesses, such as periodontal disorders, nanotechnology is now helpful. In this study, the laser ablation of solids in liquids (LASL)-created BSS-NPs were tested for their ability to kill bacteria on samples of subgingival biofilm from patients with periodontal disorders. The findings of the characterization demonstrated that both the triclinic crystallographic structure and the vibrational modes of the BSS functional groups were preserved in the synthesized BSS-NPs made by laser ablation of solids in liquids. When exposed to BSS-NPs, more than 30% of the total number of cultivable bacteria from the oral biofilm samples were suppressed. Because of this, BSS-NPs have the potential to be utilized as a novel alternative antibacterial in the treatment of periodontal disorders, lowering the usage of antibiotics without a prescription and halting the rise of antibiotic resistance [136]. This study investigated the effects of BiNPs on Enterococcus faecalis, the bacteria responsible for most chronic root canal infections. All samples were first cultured in Enterococcosel broth. After incubation, the PCR test was repeated on the samples that had shown signs of growth on blood agar plates. Powdered NPs were dissolved in ultrapure water, and the spectrophotometer was used to calculate the final concentration of BiNPs. The microbroth dilution technique was used to evaluate the MIC of BiNPs against E. faecalis by standard procedures for antimicrobial susceptibility testing. The quantity of BiNPs that resulted in a 99.9 percent reduction in the number of live bacteria was also determined using bactericidal experiments performed in the Mueller–Hinton broth medium. In light of the benefits of BiNPs, such as their ability to prevent biofilm formation from S. mutans and their greater antibacterial activity compared to CHX, it is suggested that they be used in a variety of dental settings to combat E. faecalis [63].
BiNPs have been shown effective in the treatment of H. pylori ulcers in people, and their antimicrobial properties have been demonstrated in several laboratory trials. One study (NCT04209933) aims to compare the safety and efficacy of three different forms of Bi (pectin BiNPs, Bi potassium citrate, and pectin Bi capsules) for the first treatment of H. pylori infection [137]. Since BiNPs have more antibacterial action and fewer adverse effects than CHX, they may be a more appealing choice to employ in various dental settings in the fight against S. salivarius and E. faecalis. BiNPs, however, need in-depth research. More extensive research with a bigger sample size is needed in this area. More research is needed to determine the toxicity and short- and long-term impact of these NPs on live cells [132]. Although BiNPs show promise as a means of preventing several infectious illnesses, they still need further testing to guarantee their safety for use in people. Over the last century, there have been reports of human Bi intoxication and even fatalities associated with the use of Bi pharmaceuticals. A hazardous dosage of Bi compounds causes acute renal impairment. Bi encephalopathy was a treatable neurological condition that emerged in the 1970s among patients who had taken excessive amounts of Bi over extended time periods. Since many people who had taken large amounts of Bi had not experienced these symptoms, the dose–response relationship between Bi intake and these symptoms remains unexplained. BiNPs' dose must also be carefully examined. Hence, it is imperative to conduct additional investigations to ascertain the potential cytotoxicity of BiNPs to identify any detrimental impacts on human health. The underlying mechanism by which BiNPs operate remains inadequately comprehended. The absence of a reliable in vitro analysis technique, coupled with the complexities associated with the bacterial membrane, presents challenges in obtaining a comprehensive understanding of the precise antimicrobial mechanism of BiNPs. To accurately evaluate the therapeutic capabilities of BiNPs and uncover the microbial response to these elements, it is imperative to conduct in vivo studies. In the context of biological systems, in vivo, investigations are considered essential for providing a comprehensive understanding of their application. Therefore, it is imperative to conduct further investigations into the activity of BiNPs at the structural, genetic, and proteomic levels [138].
Cobalt nanoparticles
Co oxide NPs are put to use in a wide variety of industries, from the medical sector to the production of sensors and magnetic materials to electrochemical systems and smart absorbers and catalysts. The colony formation of the gram-positive and gram-negative bacteria investigated was significantly reduced during the assessment of the antibacterial capabilities of the synthesized Co oxide NPs. An advantageous antibacterial activity against gram-negative bacteria is shown by a chemical contacting Co oxide NPs. As yet, no particular mechanism has been proposed to explain how the Co oxide NPs kill the bacteria. The synthesized Co oxide NPs have excellent antibacterial characteristics, making them suitable for application in the production of antibacterial dental and medical devices [139]. The objective of this study was to incorporate antibacterial properties into pits and fissure sealant (PFS) as a means to address the significant clinical issues associated with PFS, including microleakage and secondary caries. The pH-dependent incorporation of minocycline (MNC@CO) into cobalt oxide NPs was carried out by researchers, who subsequently characterized the resulting composite material. The purpose of this investigation was to assess the antibacterial efficacy of MNC@CO against S. sobrinus. The experimental groups with concentrations of 2.5% and 5.0% have demonstrated a statistically significant antimicrobial effect against S. sobrinus when compared to the control group (p < 0.05). The MNC@CO doped PFS with a concentration of 5.0% exhibited the greatest release of MNC at various pH levels, particularly at pH 5.0 and 3.5. The PFS incorporated with 2.5% MNC@CO exhibited the highest compressive strength of 110 MPa during a 70-day testing period, surpassing the compressive strengths of the PFS doped with 5.0% MNC@CO (75 MPa) and the control sample (80 MPa). The flexural strength of both experimental groups was lower for both time points (24 h and 30 days) than for control. In conclusion, the present study found that 2.5% MNC@CO doped PFS showed considerable anti-biofilm potential without compromising mechanical properties [140].
One of the most affordable transition metals is co, however, its antibacterial properties in its nano form have not been well investigated. It is also inadequate to compare CoNPs with bulk Co and conventional antibacterial. Investigations demonstrated that from 0.125 to 128.0 g/ml, Co NPs were shown to affect S. aureus and E. coli. E. coli was more successfully inhibited by the CoNPs zone of inhibition than S. aureus. Compared to bulk Co, oxytetracycline, and gentamicin, CoNPs performed noticeably better. At the majority of concentrations, the activity index and fold rise of CoNPs were greater. In conclusion, CoNPs showed superior antibacterial activity against S. aureus and E. coli compared to other investigated substances, especially at lower doses. Their usage may be expanded in many biomedical domains in the future. In conclusion, the CoNPs are superior to traditional antibacterials in their bulk form when it comes to fighting S. aureus and E. coli, especially at lower doses. Future uses of Co NPs' robust antibacterial properties might expand into other industries and bring about a significant transformation in the medical area [64]. A novel low-dimensional Co(II) coordination complex was synthesized using solvothermal reaction conditions by integrating an unsymmetrical tetracarboxylic acid based on a semi-rigid ether with the auxiliary dipyridyl ligand 4,4′-bipyridine (bipy). Both its therapeutic efficacy and the mechanism by which it works against chronic periodontitis were assessed. Real-time RT-PCR findings revealed that the chemical may dose-dependently reduce the relative expression levels of the survival genes expression in P. gingivalis. Inhibiting the expression of P. gingivalis survival genes, the chemical shows promise as a potential therapy for chronic periodontitis [141].
Because of their unique antioxidant, antibacterial, antifungal, anticancer, larvicidal, antileishmanial, anticholinergic, wound-healing, and antidiabetic capabilities, cobalt and cobalt oxide, NPs have a wide range of medicinal uses. To further complicate matters, cobalt, and cobalt oxide NPs have been synthesized using a variety of chemical and physical processes, some of which may be related to eco-toxicity, cost-effectiveness, high energy, and time consumption. The utilization of biotic resources including plant extract, microbes, algae, and other biomolecules like starch and gelatin has led to the development of a new approach that is safe for the environment, straightforward, simple, and quick. More benefits may be gained by using biogenic cobalt and cobalt oxide NPs than by using conventional physicochemical synthesis techniques [142]. However, there has been a dearth of research on the efficacy of CoNPs for periodontitis therapy. As a result, it is important to study CoNPs in depth to cure to cure periodontitis.
Copper nanoparticles
Copper (Cu) NPs have a high level of biological activity, are very inexpensive, are environmentally benign, and have the potential to be effective multifunctional antibacterial agents. Other metals, ceramics, and polymers may easily mix and bond with CuNPs, and the products show physiochemical stability. CuNPs are thus among the metal NPs that are often employed in dentistry. Dental products including dental amalgam, restorative types of cement, adhesives, resins, endodontic-irrigation solutions, obturation materials, dental implants, and orthodontic archwires and brackets have all benefited from the usage of CuNPs to improve their physical and chemical qualities [143]. CuNPs have various metallic qualities connected to dental uses as well as antibacterial activity. These NP composites are simple to produce with currently available dental materials and are reportedly physiochemically stable. However, they only have very limited clinical use. CuNPs have mostly been investigated in dentistry as a modifier in amalgam and antibacterial agents. Recent studies on a wide range of dental materials have shown that CuNPs may be incorporated into several different settings. Research has shown that the carboxyl group of bacterial lipoproteins contains a negative charge, which attracts positive Cu ions. Cu ions interact with bacterial cell membranes, changing the membrane's permeability and enabling Cu ions to enter the cells. Cu ions modify cellular structures and proteins when they combine with phosphorus- and sulfur-containing macromolecules (such as DNA). The cell's biochemical functions are hampered and eventually die as a result of this modification. Enzyme activity is hampered, however, by Cu ions. They interfere with DNA or protein synthesis, render their enzymes inactive, and stimulate the generation of hydrogen peroxide. Furthermore, NPs interact with the sulfhydryl group of protein molecules, causing the molecules to become denatured. At the same time, the bacterial cell membrane becomes damaged, allowing DNA, ribonucleic acid, proteins, and cytoplasm to escape. In the evolution of dental material characteristics, CuNPs serve a dual function. Incorporating CuNPs into dental materials has the potential to boost their physio-mechanical characteristics and introduce or boost their antibacterial activity. This will provide light on the advantages and disadvantages of using CuNPs in dental practice, and open up a new avenue for dental biomaterials research [144].
The research set out to develop an antibiotic release system for periodontal treatment using chitosan and CuNPs, and then evaluate its efficacy against A. actinomycetemcomitans in a laboratory setting. A biocompatible system including CuNPs was synthesized out of chitosan, starch, and ascorbic acid. Solid sponges and gel spheres with a Cu concentration of 100 g/mL were made using CuNPs/chitosan gel nanocomposites. Nanometric Cu particles were proven to produce sponges and gel spheres out of chitosan. The development of A. Actinomycetemcomitans were stymied by these substances. The sphere nanocomposites were more stable in saliva and showed a prolonged release of Cu at amounts effective against bacteria. Nanocomposites containing CuNPs and chitosan show promise as a platform for develo** targeted treatments for periodontitis [65].
Biologically synthesized AgNPs and CuNPs with the potential to display antibacterial action against several multidrug-resistant (MDR) microorganisms have been extracted from the fungus Shizophyllum commune. TEM, FTIR, dynamic light scattering, and ultraviolet–visible spectroscopy was used to determine the characterization. It was determined that the NPs were uniform in size and shape. Furthermore, the agar well diffusion technique was used to test the NPs' antibacterial activity against multidrug-resistant bacteria such as Salmonella abony, Klebsiella pneumoniae, E. coli, and S. aureus. These biosynthesized NPs have been shown to have a variety of biological uses, including the elimination of harmful bacteria and the bio-control of fungal strains [145]. Dental restorative materials are greatly impacted by pathogenicity due to improper adhesion and colonization by bacteria in the oral cavity. Therefore, scientists find that including tiny CuONPs into the sodium aluminosilicate ceramic material makes for an effective anti-S. mutans material investigation demonstrates that the composite ceramic is very biocompatible and effective against S. mutans (up to 99.99% antibacterial rate). The Cu ions in the composite ceramic prevent S. mutans from replicating its DNA, damage its respiratory system, and prevent its cell membrane from functioning properly, killing the bacterium. The antimicrobial properties of the composite ceramics correlated with the concentration of CuNPs present, and Cu ions were continuously released from the ceramics' interior to kill S. mutans within 10 days by altering membrane permeability, impeding respiratory chain activity, and interfering with gene replication [66] (Table 2).
Advantages and the perspective of comparison of metal nanoparticles for the development of therapeutic methods
Traditional antibacterial medications are ineffective against the biofilm that accumulates on human wounds, but multiple studies have demonstrated that nanomaterials may help fight bacterial drug resistance. Among the various chemotherapeutic medications, metal ions including Au, Ag, Zn, and Cu have been studied extensively for their effectiveness against periodontal and peri-implant bacteria [146]. Benefits of using NPs as antibacterial agents include their effectiveness against antibiotic-resistant bacteria, their ability to target diverse microbes, and their use as effective antibiotic transporters. The potential applications of NPs in the treatment of periodontal diseases are vast. Antimicrobial research has shown that NPs may break apart bacterial biofilms and spread them. Biofilm-encased periodontal bacteria are likely to be eliminated by NPs. However, clinical investigations are needed to confirm whether or not NPs can disperse biofilms produced by periodontal bacteria [147]. They work well against the gram-negative and gram-positive bacteria that cause periodontitis and peri-implantitis, including Prevotella intermedia, F. nucleatum, and P. gingivalis. The large surface area of the biosynthesized AgNPs increased interactions between flavonoids and the cell surface or bacteria, hence amplifying the flavonoids' physiological effects. By boosting contacts between flavonoids and the cell surface or bacteria, the biosynthesized AgNPs improved the flavonoids' biological effects [86, 148]. There is a direct correlation between AgNP size and their bactericidal action, stability, and biocompatibility. The optimal size for AgNPs is between 10 and 15 nm, with activity peaking at 15 nm. Since smaller AgNPs have a greater surface area to NP volume ratio, they are better able to interact with cell membranes. In addition, S. mutans growth, adhesion, and biofilm generation have all been shown to be inhibited by AgNPs, as shown in in vitro investigations [149]. Using methods that remove the plant material may allow for the cheap, sustainable, and ecologically responsible production of AgNPs. Plants, because of their phytochemical components, offer a superior, non-toxic, and more cost-effective alternative to both physical and chemical methods. Since the effectiveness and toxicity of AgNP rely on both their size and shape, synthesis methods and procedures have lately been the focus of a considerable amount of scientific interest. AgNPs may be made by physical, chemical, or biological means. Physical techniques need a lot of energy to maintain the high pressure and temperature necessary for the reaction, while the chemical method is dangerous and costly. The disadvantages of nanomaterials have inspired the development of biochemical techniques or biosynthesis, such as the use of biomolecular extracts from plants, to overcome issues including toxicity towards bone cells, varying biocompatibility depending on size, surface, and composition, and high cost [150]. Because of their adaptability and versatility, AuNP may be altered to improve their stability, biocompatibility, and antibacterial characteristics. The antibacterial properties of loaded antibacterial medicines may be enhanced by using AuNPs as drug carriers. Meanwhile, the use of AuNPs in oral biology is on the rise. Dental disease is only one area that might benefit from AuNPs' unique qualities, such as their adaptability in size, shape, surface properties, optical properties, biocompatibility, low cytotoxicity, high stability, and multi-functional potential. Because of their ability to inhibit the growth of fungi and bacteria, AuNPs may be introduced into certain biological materials to increase their use by providing such materials with antibacterial capabilities [7].
When compared to AgNPs, the most commonly commercially utilized ZnONPs offer several benefits, including a cheaper price and a whiter look. Toxic heavy metals react with proteins, binding their molecules. Heavier metals have a powerful interaction with the thiol groups of essential enzymes, rendering them useless. Proteins are thought to be deactivated and denatured once metal NPs like Ag attach to their functional groups. Researchers revealed that exposure to surface-functionalized TiO2NPs and UV light did not affect ALP activity in intact heterotrophic biofilms. However, at concentrations of ZnONPs far lower than those seen in complete biofilms, the ALP enzyme that is secreted by E. coli is severely inhibited [151, 152]. Indeed, in in vivo toxicity experiments, both ZnONPs and TiO2NPs have shown considerable antibacterial efficacy against oral bacteria at non-toxic doses. This means that ZnO and TiO2NPs might potentially be used as nano-antibiotics in the creation of various oral hygiene products including mouthwashes and dental pastes. Dental biofilms and oral planktonic bacteria may be managed with fewer adverse effects and less antibiotic resistance if these NPs are used as an alternative [153]. When compared to their metallic, semiconducting, silica- or carbon-based counterparts designed for pharmacological and biological applications, MNPs offer additional desirable features. By applying a magnetic field externally, magnetic NPs might be remotely directed to specific locations. Furthermore, the application of a varying magnetic field causes MNPs to waste energy as heat, leading to a localized rise in temperature. All of these methods seem to be successful, but MNPs are among the most promising concerning clinical translation in the area of antibiotic treatment. MNPs are designed for pharmaceutical and biological applications due to their unusual physical features and their ability to work at the cellular and molecular levels. Furthermore, MNP drug delivery methods enhance localization, reducing the dosage of medications required to achieve the desired effect. These benefits result from the antibacterial qualities present in the bulk form of some metals, such as Zn, Ag, and Cu [154]. Many advances have been made, but the fight against tooth disease is far from over. To create MNPs with sufficient biocompatibility, new synthesis processes, and methodologies are still required. MNPs-based composites with fine microstructures and superior biomedical capabilities need more efficient ways of preparation [155]. A summary of the performance of various types of metal NPs in the treatment of periodontitis is shown in Fig. 6.
Cu's antibacterial qualities and low toxicity make it a desirable research material in the fields of medicine and dentistry. Copper's metal ions or the oxidized Cu ions produced by CuNPs (1–100 nm) are responsible for the antibacterial actions. Moreover, since Cu may be produced either naturally or via chemical synthesis, CuNPs are processed at a low cost. In addition, CuO NPs may be readily formed by oxidation in air or water. Cu particles, like other metal NPs used in dentistry, have a wide range of nano-sizes and shapes, a one-of-a-kind distribution, and a high surface-to-volume ratio. These characteristics improve the NPs’ antibacterial efficacy, biocompatibility, and bio-physiochemical functionalization. CuONPs have been demonstrated to be antibacterial and to prevent the production of biofilms. The antimicrobial activity of Cu NPs is improved by their high surface area/volume ratio. Despite extensive research, the precise method by which CuNPs kill microorganisms remains unclear. The bactericidal activity of CuNPs against E. coli, B. subtilis, and S. aureus is superior to that of AgNPs, another kind of NP often employed in biomedical research. Antimicrobial and other metallic characteristics of interest for dental applications are present in CuNPs. It is simple to create these NPs composites using standard dental materials, and they are reported to be physiochemically stable. However, their use in the clinic is quite restricted. As a modifier in amalgam and an antibacterial agent, CuNPs have received the majority of the research attention in the dental field. Dental cement, restorative materials, adhesives, resins, irrigating solutions, obturations, orthodontic archwires and brackets, implant surface coatings, and the bone regeneration process are all reported to benefit from the addition of CuNPs, the subject of recent research. CuONPs are less expensive, chemically stable, and safe for the environment than AgNPs [144].
However, their use in the clinic is quite restricted. As a modifier in amalgam and an antibacterial agent, CuNPs have received the majority of the research attention in the dental field. Dental cement, restorative materials, adhesives, resins, irrigating solutions, obturations, orthodontic archwires and brackets, implant surface coatings, and the bone regeneration process are all reported to benefit from the addition of CuNPs, the subject of recent research. In comparison to AgNPs, CuONPs are more environmentally friendly, less costly, and more stable chemically. Cu and NiNPs have been found to exhibit bactericidal action in laboratory studies. They have not been synthesized in aqueous solution, however, since their characteristics may be compromised by the addition of stabilizers such as polymers, ligands, salts, etc. Furthermore, Cu-Ni bimetallic NPs' antibacterial activities have not been investigated till recently. To synthesize the desired NPs, several variables, including pH and reducing agent concentration, are used. Despite claims that nickel oxide nanotubes may be synthesized with potent antibacterial properties, the present study demonstrated that NiNPs have neither bactericidal nor bacteriostatic activity. Finally, the antibacterial action of bimetallic Cu-Ni NPs has not been reported before. Nickel’s bacteriostatic activity and the fact that bimetallic Cu-Ni particles are bigger than CuNPs and NiNPs may both be to blame for this behavior. When creating NPs, the experimental settings used are crucial. To create stoichiometric metal nanoalloy (bimetallic) NPs, pH plays a crucial role. The redox potential of the metals is what decides this. Successfully characterizing the NPs. Since the sample is exposed to the atmosphere during characterization, oxides develop, making the study of zero-valent metal compounds challenging. The produced NPs have a polydispersity of less than 5% and a size of less than 25 nm [127]. The research and refinement of metal NP production technologies for use in periodontitis therapy are crucial. These NPs are useful in the treatment of this condition thanks to their antibacterial and anti-inflammatory capabilities, as well as their simple and inexpensive manufacturing procedure.
Metal NPs are being employed for periodontitis therapy and other dental applications due to their unique properties; nevertheless, these NPs should be thoroughly investigated for any harmful side effects to guarantee their safe usage. Furthermore, the cost of raw materials and processing, their availability, their sustainability towards end-use, and their recyclability are all factors that must be addressed when using the circular economy idea [156, 157]. When it comes to treating periodontitis, the major antibacterial mechanism underlying the activity of various metal NPs, such BiNPs, and CoNPs, is still not fully known. In vivo, studies are crucial for accurately gauging the therapeutic potential of metal NPs and uncovering the microbial response to these variables. In-vivo studies are crucial for providing a complete explanation of their function in living systems [116]. In addition, the journals discussed here contain evidence that suggests research into the use of metal NPs to treat periodontitis is still in its early stages. A large proportion of the studies reviewed here are technically focused investigations that often lack a principal expense/advantage analysis and specifications of the primary steps of each investigation. The mechanisms of metal NPs’ cellular absorption and their antibacterial effects in periodontitis therapy need further investigation. It's worth noting that most mechanisms for site-specific transfer perform well in vitro but poorly in vivo testing. Therefore, in vivo, testing for periodontitis therapy might benefit this study.
Conclusion
Several traditional treatments for periodontitis exist, each targeting different aspects of the disease's etiology and pathophysiology. Antibiotic and antimicrobial drug treatment is widely used. However, traditional approaches are rendered useless due to medication resistance and the emergence of unwanted effects. Metal NPs are the most promising antibacterial material because of their high specific surface area to volume ratio, prolonged shelf life, and biocompatibility. Researchers' interest in metal NPs growing as a result of the creation of strains that are resistant to drugs and the improvement of microbial resistance to antibiotics. Due to the NPs' tiny size, they may enter the biofilm matrix and make direct contact with the bacterial cells, which inhibits the biofilm. As we move closer to practical applications, it's expected that antibacterial research will improve further. Metal NPs have efficient antibacterial capabilities. Given the recent advancements and ongoing efforts in improving particle synthesis efficiency and examining their biomedical applications, it is hoped that the implementation of our strategy on a large scale and their commercial applications in medicine and health care will be very helpful in the upcoming years. It is anticipated that antimicrobial research would advance more as we get closer to real-world applications. The antibacterial properties of metal NPs are very effective. With recent and ongoing improvements to particle synthesis efficiency and research into their biomedical applications, it is hoped that widespread implementation of investigation strategy and their commercial applications in medicine and health care will prove immensely beneficial in the years to come.
Availability of data and materials
Not applicable.
References
Glickman I, Carranza FA. Glickman’s clinical periodontology. Philadelphia: WB Saunders Company; 1990.
Amato M, et al. Local delivery and controlled release drugs systems: a new approach for the clinical treatment of periodontitis therapy. Pharmaceutics. 2023;15(4):1312.
Ryan ME. Nonsurgical approaches for the treatment of periodontal diseases. Dent Clin. 2005;49(3):611–36.
Krayer JW, Leite RS, Kirkwood KL. Non-surgical chemotherapeutic treatment strategies for the management of periodontal diseases. Dent Clin. 2010;54(1):13–33.
Sadek KM, et al. Molecular basis beyond interrelated bone resorption/regeneration in periodontal diseases: a concise review. Int J Mol Sci. 2023;24(5):4599.
Fowler EB, Breault LG, Cuenin MF. Periodontal disease and its association with systemic disease. Mil Med. 2001;166(1):85–9.
Abdelghany TM, et al. Phytofabrication of zinc oxide nanoparticles with advanced characterization and its antioxidant, anticancer, and antimicrobial activity against pathogenic microorganisms. Biomass Conv Biorefinery. 2023;13(1):417–30.
Yasamineh S, et al. An overview on nanoparticle-based strategies to fight viral infections with a focus on COVID-19. J Nanobiotechnology. 2022;20(1):440.
Yasamineh S, et al. A state-of-the-art review on the recent advances of niosomes as a targeted drug delivery system. Int J Pharm. 2022;624:121878.
Norouzi M, et al. Recent advances on nanomaterials-based fluorimetric approaches for microRNAs detection. Mater Sci Eng, C. 2019;104: 110007.
Solanki LA, Sundari KS, Rajeshkumar S. In-vitro cytotoxicity evaluation of green synthesized gold nanoparticles and its indigenous mouthwash. J Pure Appl Microbiol. 2021;15(2):735–42.
Jandt KD, Watts DC. Nanotechnology in dentistry: present and future perspectives on dental nanomaterials. Dent Mater. 2020;36(11):1365–78.
Nizami MZI, et al. Metal and metal oxide nanoparticles in caries prevention: a review. Nanomaterials. 2021;11(12):3446.
Shanmuganathan R, et al. Core/shell nanoparticles: synthesis, investigation of antimicrobial potential and photocatalytic degradation of Rhodamine B. J Photochem Photobiol, B. 2020;202: 111729.
Wang H, et al. Branched AuAg nanoparticles coated by metal–phenolic networks for treating bacteria-induced periodontitis via photothermal antibacterial and immunotherapy. Mater Des. 2022;224: 111401.
Hernández-Sierra JF, et al. In vitro cytotoxicity of silver nanoparticles on human periodontal fibroblasts. J Clin Pediatr Dent. 2011;36(1):37–42.
Steckiewicz KP, et al. Silver nanoparticles as chlorhexidine and metronidazole drug delivery platforms: their potential use in treating periodontitis. Int J Nanomedicine. 2022;17:495–517.
Trindade D, et al. Prevalence of periodontitis in dentate people between 2011 and 2020: a systematic review and meta-analysis of epidemiological studies. J Clin Periodontol. 2023. https://doi.org/10.1111/jcpe.13769.
Ray RR. Periodontitis: an oral disease with severe consequences. Appl Biochem Biotechnol. 2023;195(1):17–32.
Khan ST, et al. Application of nanoparticles in oral hygiene. Biomater Tissue Eng Bull. 2016;3:35–49.
Loesche WJ. The role of spirochetes in periodontal disease. Adv Dent Res. 1988;2(2):275–83.
Genco RJ, Borgnakke WS. Risk factors for periodontal disease. Periodontology 2020. 2013;62(1):59–94.
Tariq M, et al. Treatment modalities and evaluation models for periodontitis. Int J Pharm Investig. 2012;2(3):106.
Jain N, et al. Dental therapeutic systems. Recent Pat Drug Deliv Formul. 2008;2(1):58.
Harini G, Kaarthikeyan G. Advanced drug delivery systems in treating periodontal diseases-a review. J Dental Med Sci. 2014;13(1):27–32.
Graziani F, et al. Nonsurgical and surgical treatment of periodontitis: how many options for one disease? Periodontology 2000. 2017;75(1):152–88.
Sanz I, et al. Nonsurgical treatment of periodontitis. J Evid Based Dent Pract. 2012;12(3):76–86.
Page R. Oral health status in the United States: prevalence of inflammatory periodontal diseases. J Dent Educ. 1985;49:354–67.
Gasner NS, Schure RS. Periodontal disease. In: Gasner NS, editor. StatPearls. Treasure Island: StatPearls Publishing; 2022.
Belibasakis GN, et al. Periodontal microbiology and microbial etiology of periodontal diseases: historical concepts and contemporary perspectives. Periodontology 2000. 2023. https://doi.org/10.1111/prd.12473.
Haque MM, et al. Advances in novel therapeutic approaches for periodontal diseases. BMC Oral Health. 2022;22(1):1–23.
Muñoz Navarro C, et al. Analysis of the oral microbiome in a patient with cardiofaciocutaneous syndrome and severe periodontal disease: impact of systemic antibiotic therapy. Antibiotics. 2022;11(12):1754.
Van der Weijden G, Dekkers GJ, Slot DE. Success of non-surgical periodontal therapy in adult periodontitis patients: a retrospective analysis. Int J Dental Hygiene. 2019;17(4):309–17.
Jain N, et al. Recent approaches for the treatment of periodontitis. Drug Discov Today. 2008;13(21–22):932–43.
Li Y, et al. Disruption of biofilms in periodontal disease through the induction of phase transition by cationic dextrans. Acta Biomater. 2023. https://doi.org/10.1016/j.actbio.2023.01.008.
Butera A, et al. Evaluation of the efficacy of probiotics domiciliary protocols for the management of periodontal disease, in adjunction of non-surgical periodontal therapy (NSPT): a systematic literature review. Appl Sci. 2023;13(1):663.
Mercado N, et al. Application of nanoparticles in treating periodontitis: preclinical and clinical overview. In: Pathak YV, editor., et al., Surface modification of nanoparticles for targeted drug delivery. Cham: Springer; 2019. p. 467–80.
Hernández-Venegas PA, et al. Bactericidal activity of silver nanoparticles on oral biofilms related to patients with and without periodontal disease. J Funct Biomater. 2023;14(6):311.
Oveili E, et al. The potential use of mesenchymal stem cells-derived exosomes as microRNAs delivery systems in different diseases. Cell Commun Signal. 2023;21(1):1–26.
Assefi M, et al. A state-of-the-art review on solid lipid nanoparticles as a nanovaccines delivery system. J Drug Deliv Sci Technol. 2023;86:104623.
Sedghi LM, Bacino M, Kapila YL. Periodontal disease: the good, the bad, and the unknown. Front Cell Infect Microbiol. 2021;11:1210.
Cheng Z, et al. Periodontal disease and periodontal bacteria as triggers for rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2017;31(1):19–30.
Slavin YN, et al. Metal nanoparticles: understanding the mechanisms behind antibacterial activity. Journal of nanobiotechnology. 2017;15:1–20.
Gabrielyan L, Trchounian A. Antibacterial activities of transient metals nanoparticles and membranous mechanisms of action. World J Microbiol Biotechnol. 2019;35(10):162.
Priyadarsini S, Mukherjee S, Mishra M. Nanoparticles used in dentistry: a review. J Oral Biol Craniofac Res. 2018;8(1):58–67.
Dizaj SM, et al. Antimicrobial activity of the metals and metal oxide nanoparticles. Mater Sci Eng, C. 2014;44:278–84.
Rattanata N, et al. Gallic acid conjugated with gold nanoparticles: antibacterial activity and mechanism of action on foodborne pathogens. Int J Nanomed. 2016;11:3347.
Zhang S, et al. Antimicrobial properties of metal nanoparticles and their oxide materials and their applications in oral biology. J Nanomater. 2022;2022:1.
**n Y, et al. A robust ROS generation nanoplatform combating periodontitis via sonodynamic/chemodynamic combination therapy. Chem Eng J. 2023;451: 138782.
Bruna T, et al. Silver nanoparticles and their antibacterial applications. Int J Mol Sci. 2021;22(13):7202.
Lengert EV, et al. Influence of the new formulation based on silver alginate microcapsules loaded with tannic acid on the microcirculation of the experimental periodontitis in rats. Mater Sci Eng, C. 2021;126: 112144.
Zhang S, et al. L-cysteine-modified chiral gold nanoparticles promote periodontal tissue regeneration. Bioact Mater. 2021;6(10):3288–99.
Dong Z, et al. NIR-triggered tea polyphenol-modified gold nanoparticles-loaded hydrogel treats periodontitis by inhibiting bacteria and inducing bone regeneration. Mater Des. 2023;225: 111487.
Mohandoss S, et al. Ulvan as a reducing agent for the green synthesis of silver nanoparticles: a novel mouthwash. Inorganics. 2023;11(1):5.
Halkai KR, et al. Biosynthesis, characterization and antibacterial efficacy of silver nanoparticles derived from endophytic fungi against P. gingivalis. J Clin Diagn Res. 2017;11(9):92.
Zhang M, et al. Biological safe gold nanoparticle-modified dental aligner prevents the Porphyromonas gingivalis biofilm formation. ACS Omega. 2020;5(30):18685–92.
Holden MS, et al. Antibacterial activity of partially oxidized Ag/Au nanoparticles against the oral pathogen Porphyromonas gingivalis W83. J Nanomater. 2016;2016:53–53.
Seo N, et al. Effect of zinc oxide nanoparticle addition to polycaprolactone periodontal membranes on antibacterial activity and cell viability. J Nanosci Nanotechnol. 2021;21(7):3683–8.
Yeniyol S, et al. Antibacterial activity of As-annealed TiO2 nanotubes doped with Ag nanoparticles against periodontal pathogens. Bioinorg Chem Appl. 2014;2014:1.
Sun X, et al. Nanoparticles having amphiphilic silane containing Chlorin e6 with strong anti-biofilm activity against periodontitis-related pathogens. J Dent. 2019;81:70–84.
Vahedi M, et al. Evaluation of anti-bacterial effects of nickel nanoparticles on biofilm production by Staphylococcus epidermidis. Iran J Microbiol. 2017;9(3):160.
Hernandez-Delgadillo R, et al. Zerovalent bismuth nanoparticles inhibit Streptococcus mutans growth and formation of biofilm. Int J Nanomedicine. 2012;7:2109–13.
Azad A, et al. Assessment of the antibacterial effects of bismuth nanoparticles against Enterococcus faecalis. BioMed Res Int. 2020;2020:1.
Gupta V, et al. Comparative assessment of antibacterial efficacy for cobalt nanoparticles, bulk cobalt and standard antibiotics: a concentration dependant study. Haнocиcтeмы физикa, xимия, мaтeмaтикa. 2020;11(1):78–85.
González J, et al. Design of antimicrobial release systems based on chitosan and copper nanoparticles for localized periodontal therapy. J Dent Oral Disord. 2016;2(7):1035.
Fu R, et al. A Nano-CuO doped sodium aluminosilicate composite ceramic with high efficiency against streptococcus mutans for dental restorative materials. Ceram Int. 2022;48(19):28578–85.
Anwar AA, Sumaryono B, Budhy TI. An insight of epigallocatechin-3-gallate-loaded gold nanoparticles as an oral mucosal cancer adjuvant therapy by modulating intrinsic apoptosis pathway: a narrative. Malays J Med Health Sci. 2023;19:187–93.
Ifijen IH, et al. A concise review of the antibacterial action of gold nanoparticles against various bacteria. In: Ifijen IH, editor., et al., TMS 2023 152nd annual meeting and exhibition supplemental proceedings. Cham: Springer; 2023.
Bapat RA, et al. Recent advances of gold nanoparticles as biomaterial in dentistry. Int J Pharm. 2020;586: 119596.
Ni C, et al. Gold nanoparticles modulate the crosstalk between macrophages and periodontal ligament cells for periodontitis treatment. Biomaterials. 2019;206:115–32.
Wang Q, et al. Gold nanoparticles enhance proliferation and osteogenic differentiation of periodontal ligament stem cells by PINK1-mediated mitophagy. Arch Oral Biol. 2023;150:105692.
Zhang Y, et al. Gold nanoparticles promote the bone regeneration of periodontal ligament stem cell sheets through activation of autophagy. Int J Nanomed. 2021;16:61.
Yin Y, et al. Gold nanoparticles targeting the autophagy–lysosome system to combat the inflammation-compromised osteogenic potential of periodontal ligament stem cells: from mechanism to therapy. Biomaterials. 2022;288: 121743.
Chi M, et al. Novel bioactive and therapeutic dental polymeric materials to inhibit periodontal pathogens and biofilms. Int J Mol Sci. 2019;20(2):278.
Ma Y-C, et al. Au nanoparticles with enzyme-mimicking activity-ornamented ZIF-8 for highly efficient photodynamic therapy. Biomater Sci. 2019;7(7):2740–8.
Deng X, et al. Yolk–shell structured Au nanostar@ metal–organic framework for synergistic chemo-photothermal therapy in the second near-infrared window. Nano Lett. 2019;19(10):6772–80.
Qi M, et al. Novel nanomaterial-based antibacterial photodynamic therapies to combat oral bacterial biofilms and infectious diseases. Int J Nanomedicine. 2019;14:6937–56.
Darabpour E, et al. Fast and effective photodynamic inactivation of 4-day-old biofilm of methicillin-resistant Staphylococcus aureus using methylene blue-conjugated gold nanoparticles. J Drug Deliv Sci Technol. 2017;37:134–40.
Turcheniuk K, et al. Highly effective photodynamic inactivation of E. coli using gold nanorods/SiO 2 core–shell nanostructures with embedded verteporfin. Chem Commun. 2015;51(91):16365–8.
Bapat RA, et al. An overview of application of silver nanoparticles for biomaterials in dentistry. Mater Sci Eng, C. 2018;91:881–98.
Tsuzuki T, McCormick PG. Mechanochemical synthesis of nanoparticles. J Mater Sci. 2004;39:5143–6.
Mallineni SK, et al. Silver nanoparticles in dental applications: a descriptive review. Bioengineering. 2023;10(3):327.
Afkhami F, et al. Silver nanoparticles and their therapeutic applications in endodontics: a narrative review. Pharmaceutics. 2023;15(3):715.
Craciunescu O, et al. Biosynthesis of silver nanoparticles in collagen gel improves their medical use in periodontitis treatment. Part Sci Technol. 2019;37(6):757–63.
Li W, et al. Novel dental adhesive containing silver exchanged EMT zeolites against cariogenic biofilms to combat dental caries. Microporous Mesoporous Mater. 2020;299: 110113.
Prapaipittayakhun J, et al. Biologic effects of biosynthesized Oroxylum indicum/silver nanoparticles on human periodontal ligament stem cells. OpenNano. 2023;9: 100117.
Wong PY, et al. A novel antimicrobial hydrogel for the management of periodontal diseases. Int Dental J. 2023. https://doi.org/10.1016/j.identj.2023.01.002.
Mendes CR, et al. Antibacterial action and target mechanisms of zinc oxide nanoparticles against bacterial pathogens. Sci Rep. 2022;12(1):2658.
Toledano M, et al. Polymeric zinc-doped nanoparticles for high performance in restorative dentistry. J Dent. 2021;107: 103616.
Ziaei M, et al. Effects of incorporating zinc oxide and graphene oxide nanoparticles on abrasion, translucency, and microhardness of flowable composite resin: in vitro. Dental Res J. 2023;20(1):6.
Pasquet J, et al. The contribution of zinc ions to the antimicrobial activity of zinc oxide. Colloids Surf A. 2014;457:263–74.
Rani N, et al. Characterization and investigation of antioxidant and antimicrobial activity of zinc oxide nanoparticles prepared using leaves extract of Nyctanthes arbor-tristis. Inorg Chem Commun. 2023;150: 110516.
Naqvi QU, et al. Size-dependent inhibition of bacterial growth by chemically engineered spherical ZnO nanoparticles. J Biol Phys. 2019;45:147–59.
Raj NB, et al. Harnessing ZnO nanoparticles for antimicrobial and photocatalytic activities. J Photochem Photobiol. 2021;6: 100021.
Bahrami R, et al. Anti-biofilm and bystander effects of antimicrobial photo-sonodynamic therapy against polymicrobial periopathogenic biofilms formed on coated orthodontic mini-screws with zinc oxide nanoparticles. Photodiagn Photodyn Ther. 2023;41: 103288.
Delfani S, et al. Potent effects of green synthesized zinc nanoparticles against some cariogenic bacteria (Streptococcus mutans and Actinomyces viscosus). Glob J Med Pharm Biomed Update. 2022;17:11.
Mou J, et al. Hydrogel containing minocycline and zinc oxide-loaded serum albumin nanopartical for periodontitis application: preparation, characterization and evaluation. Drug Deliv. 2019;26(1):179–87.
Talalabd S, et al. Comparison the activity of ALT enzyme in saliva of periodontitis patients with control and determine the effect of ZnONPs on its activity. IJSR. 2017;6(1):2197–200.
Osorio R, et al. Bioactive polymeric nanoparticles for periodontal therapy. PLoS ONE. 2016;11(11): e0166217.
Pushpalatha C, et al. Zinc oxide nanoparticles: a review on its applications in dentistry. Front Bioeng Biotechnol. 2022;10: 917990.
Münchow EA, et al. Development and characterization of novel ZnO-loaded electrospun membranes for periodontal regeneration. Dent Mater. 2015;31(9):1038–51.
Prado-Prone G, et al. Antibacterial composite membranes of polycaprolactone/gelatin loaded with zinc oxide nanoparticles for guided tissue regeneration. Biomed Mater. 2020;15(3): 035006.
Sun J, et al. Improving performance of dental resins by adding titanium dioxide nanoparticles. Dent Mater. 2011;27(10):972–82.
Nadeem M, et al. The current trends in the green syntheses of titanium oxide nanoparticles and their applications. Green Chem Lett Rev. 2018;11(4):492–502.
Ziental D, et al. Titanium dioxide nanoparticles: prospects and applications in medicine. Nanomaterials. 2020;10(2):387.
Holban AM, Grumezescu AM, Andronescu E. Inorganic nanoarchitectonics designed for drug delivery and anti-infective surfaces. In: Surface chemistry of nanobiomaterials. Amsterdam: Elsevier; 2016. p. 301–27.
Mansoor A, et al. Medical and dental applications of titania nanoparticles: an overview. Nanomaterials. 2022;12(20):3670.
Chen X, et al. Effects of tricalcium phosphate-titanium nanoparticles on mechanical performance after friction stir processing on titanium alloys for dental applications. Mater Sci Eng B. 2023;293: 116492.
Qi M, et al. Novel nanotechnology and near-infrared photodynamic therapy to kill periodontitis-related biofilm pathogens and protect the periodontium. Dent Mater. 2019;35(11):1665–81.
Ali BG. The effect of titanium dioxide nanoparticles on the activity of salivary alkaline phosphatase and peroxidase in chronic periodontitis patients. World J Dent. 2019. https://doi.org/10.5005/jp-journals-10015-1593.
Kim D-H, et al. Titanium dioxide nanoparticles induce COX-2 expression through ROS generation in human periodontal ligament cells. J Toxicol Sci. 2019;44(5):335–45.
Li Z, Zhang Y. An efficient and user-friendly method for the synthesis of hexagonal-phase NaYF4: Yb, Er/Tm nanocrystals with controllable shape and upconversion fluorescence. Nanotechnology. 2008;19(34): 345606.
Grande F, Tucci P. Titanium dioxide nanoparticles: a risk for human health? Mini Rev Med Chem. 2016;16(9):762–9.
Mathew DM, Pushpalatha C, Anandakrishna L. Magnetic nanoparticles: a novel adjunct for dentistry. Mater Today Proc. 2022;50:173–80.
Li Z, et al. An overview of synthesis and structural regulation of magnetic nanomaterials prepared by chemical coprecipitation. Metals. 2023;13(1):152.
Yazdanian M, et al. The potential application of green-synthesized metal nanoparticles in dentistry: a comprehensive review. Bioinorg Chem Appl. 2022;2022:1.
Moraes G, Zambom C, Siqueira WL. Nanoparticles in dentistry: a comprehensive review. Pharmaceuticals. 2021;14(8):752.
Guo C, et al. Engineering magnetically induced antibacterial organic/inorganic hybrid nanoparticles for the treatment of periodontitis. Giant. 2023;13:100145.
Guo X, et al. The preventive effect of a magnetic nanoparticle-modified root canal sealer on persistent apical periodontitis. Int J Mol Sci. 2022;23(21):13137.
Wang Y, et al. Protective effect of iron oxide nanoparticles on periodontal injury in rats by inhibiting collagenase-1 and alkaline phosphatase expression. J Biomed Nanotechnol. 2022;18(4):1131–7.
Habibi N, Jazani NH, Yousefi S. Evaluation of the antibacterial effects of nickel nanoparticles on biofilm production by Streptococcus mutans. J Med Bacteriol. 2017;6(1–2):8–14.
Loberto JCS, et al. Staphylococcus spp. in the oral cavity and periodontal pockets of chronic periodontitis patients. Braz J Microbiol. 2004;35:64–8.
O’Connor AM, et al. Significant enrichment and diversity of the staphylococcal arginine catabolic mobile element ACME in Staphylococcus epidermidis isolates from subgingival peri-implantitis sites and periodontal pockets. Front Microbiol. 2018;9:1558.
Buttner H, Mack D, Rohde H. Structural basis of Staphylococcus epidermidis biofilm formation: mechanisms and molecular interactions. Front Cell Infect Microbiol. 2015;5:14. https://doi.org/10.3389/fcimb.2015.00014.
Ceri H, et al. The calgary biofilm device: new technology for rapid determination of antibiotic susceptibilities of bacterial biofilms. J Clin Microbiol. 1999;37(6):1771–6.
Gan J-C, et al. A new Ni (II)-containing coordination complex based on the multiple N-donor ligand: crystal structure and application of its nanoparticle as a P. gingivalis biofilm inhibitor for periodontitis treatment. J Struct Chem. 2020;61:330–5.
Argueta-Figueroa L, et al. Synthesis, characterization and antibacterial activity of copper, nickel and bimetallic Cu–Ni nanoparticles for potential use in dental materials. Prog Nat Sci Mater Int. 2014;24(4):321–8.
Neamati F, et al. Bismuth nanoparticles against microbial infections. Nanomedicine. 2023. https://doi.org/10.2217/nnm-2022-0153.
Tiekink ER. Antimony and bismuth compounds in oncology. Crit Rev Oncol Hematol. 2002;42(3):217–24.
Gomez C, et al. Medical applications of metallic bismuth nanoparticles. Pharmaceutics. 2021;13(11):1793.
El-Batal AI, et al. Melanin-gamma rays assistants for bismuth oxide nanoparticles synthesis at room temperature for enhancing antimicrobial, and photocatalytic activity. J Photochem Photobiol B. 2017;173:120–39.
Rostamifar S, et al. New strategy of reducing biofilm forming bacteria in oral cavity by bismuth nanoparticles. BioMed Res Int. 2021;2021:1.
Hernandez-Delgadillo R, et al. Bismuth oxide aqueous colloidal nanoparticles inhibit Candida albicans growth and biofilm formation. Int J Nanomedicine. 2013;8:1645–52.
Badireddy AR, et al. Bismuth dimercaptopropanol (BisBAL) inhibits the expression of extracellular polysaccharides and proteins by Brevundimonas diminuta: implications for membrane microfiltration. Biotechnol Bioeng. 2008;99(3):634–43.
Vega-Jiménez A, et al. Bismuth subsalicylate nanoparticles with anaerobic antibacterial activity for dental applications. Nanotechnology. 2017;28(43): 435101.
Reyes-Carmona L, et al. Antimicrobial evaluation of bismuth subsalicylate nanoparticles synthesized by laser ablation against clinical oral microorganisms. Opt Laser Technol. 2023;158: 108930.
Cao Y, et al. The efficacy and safety of different bismuth agents in Helicobacter pylori first-line eradication: a multicenter, randomized, controlled clinical trial. Medicine. 2021;100(50): e27923.
Salari Sedigh S, et al. The role of bismuth nanoparticles in the inhibition of bacterial infection. World J Microbiol Biotechnol. 2023;39(7):1–18.
Moradpoor H, et al. Optimisation of cobalt oxide nanoparticles synthesis as bactericidal agents. Open Access Maced J Med Sci. 2019;7(17):2757.
Alkheraif AA, et al. Minocycline incorporated cobalt oxide nanoparticles in dental sealants: an in vitro study. Microsc Res Tech. 2022;85(7):2558–66.
Hao W-J, et al. A new Co (II)-coordination complex: application values against chronic periodontitis through regulating Porphyromonas gingivalis survival genes expression. Inorg Nano Metal Chem. 2021;51(11):1507–11.
Waris A, et al. Green fabrication of Co and Co3O4 nanoparticles and their biomedical applications: a review. Open Life Sci. 2021;16(1):14–30.
Holubnycha V et al. Antibacterial activity of the new copper nanoparticles and Cu NPs/chitosan solution. In: 2017 IEEE 7th international conference nanomaterials: application and properties (NAP). 2017: IEEE.
Xu VW, et al. Application of copper nanoparticles in dentistry. Nanomaterials. 2022;12(5):805.
Fatima F, Wahid I. Eco-friendly synthesis of silver and copper nanoparticles by Shizophyllum commune fungus and its biomedical applications. Int J Environ Sci Technol. 2022;19(8):7915–26.
Goudouri O-M, et al. Antibacterial properties of metal and metalloid ions in chronic periodontitis and peri-implantitis therapy. Acta Biomater. 2014;10(8):3795–810.
Das V, et al. An update on possible alternative therapeutics for future periodontal disease management. J Appl Microbiol. 2023;134(1):lxac039.
Reidy B, et al. Mechanisms of silver nanoparticle release, transformation and toxicity: a critical review of current knowledge and recommendations for future studies and applications. Materials. 2013;6(6):2295–350.
Talapko J, et al. Antibacterial activity of silver and its application in dentistry, cardiology and dermatology. Microorganisms. 2020;8(9):1400.
Hossain N, Islam MA, Chowdhury MA. Synthesis and characterization of plant extracted silver nanoparticles and advances in dental implant applications. Heliyon. 2022;8: e12313.
Ibrahim L, et al. Estimation of ZnO nanoparticles effect on salivary alp activity in chronic periodontitis patients: in vitro study. Int J Adv Res Biol Sci. 2016;3(4):152–9.
Schug H, et al. Effect of TiO2 nanoparticles and UV radiation on extracellular enzyme activity of intact heterotrophic biofilms. Environ Sci Technol. 2014;48(19):11620–8.
Khan ST, Al-Khedhairy AA, Musarrat J. ZnO and TiO 2 nanoparticles as novel antimicrobial agents for oral hygiene: a review. J Nanopart Res. 2015;17:1–16.
Rodrigues GR, et al. Antimicrobial magnetic nanoparticles based-therapies for controlling infectious diseases. Int J Pharm. 2019;555:356–67.
Li X, et al. Current investigations into magnetic nanoparticles for biomedical applications. J Biomed Mater Res Part A. 2016;104(5):1285–96.
Kumar S, et al. Advantages and disadvantages of metal nanoparticles. In: Tiwari SK, Kumar V, Thomas S, editors., et al., Nanoparticles reinforced metal nanocomposites: mechanical performance and durability. Singapore: Springer; 2023. p. 209–35.
Priyadarsini S, et al. Application of nanoparticles in dentistry Current trends. In: Shukla AK, editor., et al., Nanoparticles in Medicine. Singapore: Springer; 2020. p. 55–8.
Acknowledgements
The authors thank all researchers who contributed to the advancement of science.
Funding
There is no funding.
Author information
Authors and Affiliations
Contributions
SY, and OG: writing—original draft. KN, SM, SA, MG, MT, AG, and MA: writing—review and editing. OG, and MC: conceptualization, supervision, writing—review and editing. All authors participated in the manuscript in the critical review process of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nasiri, K., Masoumi, S.M., Amini, S. et al. Recent advances in metal nanoparticles to treat periodontitis. J Nanobiotechnol 21, 283 (2023). https://doi.org/10.1186/s12951-023-02042-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12951-023-02042-7