Abstract
Background
To determine whether concurrent chemotherapy is necessary during locoregional radiotherapy (RT) after palliative chemotherapy (PCT) in patients with de novo metastatic nasopharyngeal carcinoma (mNPC).
Methods
A total of 746 patients with mNPC from 2000 to 2017 at our hospital were retrospectively reviewed. Among them, 355 patients received PCT followed by RT. Overall survival (OS) and progression-free survival (PFS), including locoregional progression-free survival (LRPFS) and distant progression-free survival (DPFS) were estimated with the Kaplan–Meier method and log-rank test. Cox proportional-hazards models, landmark analyses, propensity score matching, and subgroup analyses were used to address confounding.
Results
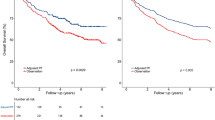
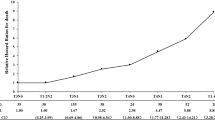
Of the patients included in our study, 192 received radiotherapy alone after PCT (PCT + RT), and 163 received concurrent chemoradiotherapy after PCT (PCT + CCRT). The prognosis of PCT + CCRT was significantly better than that of PCT + RT (5 year OS, 53.0 vs 36.2%; P = 0.004). After matching, the 5 year OS rates of the two groups were 55.7 and 39.0%, respectively (P = 0.034) and the median DPFS were 29.4 and 18.7 months, respectively (P = 0.052). Multivariate Cox regression analysis indicated that PCT + CCRT was an independent favorable prognostic factor (P = 0.009). In addition, conducting concurrent chemoradiotherapy after 4–6 cycles of PCT or conducting concurrent chemotherapy with single-agent platinum was associated with significant survival benefit in the matched cohort (5 year OS rate, 60.4 or 57.4%, respectively). The survival difference between groups remained significant when evaluating patients who survived for ≥ 1 year (P = 0.028).
Conclusions
The optimal treatment strategy of mNPC is the combination of PCT followed by concurrent chemoradiotherapy. More specifically, concurrent chemoradiotherapy with single-agent platinum after 4–6 cycles of PCT is suggested.
Similar content being viewed by others
Background
Nasopharyngeal carcinoma (NPC) is a malignant tumor of the nasopharyngeal epithelium that exhibits an unbalanced geographical distribution [1]. In endemic regions, especially in South China, the worldwide age-standardized incidence rate of NPC is up to 25.39/100 000 person-years [2]. Among them, 4–10% of patients present with de novo metastatic nasopharyngeal carcinoma (mNPC), and the 5-year survival rate of mNPC is approximately 20% [3, 4]. According to the current National Comprehensive Cancer Network (NCCN) guidelines, platinum-based palliative chemotherapy (PCT) with or without locoregional radiotherapy (RT) is the cornerstone of treatment for patients with mNPC [5]. Many retrospective studies have asserted that cycles of PCT are not always positively related to survival and 4–6 cycles are recommended [31]. A phase I clinical trial of 27 patients with recurrent or metastatic NPC suggested that pembrolizumab treatment resulted in a median OS of 16.5 months. [32] Another phase II trial of nivolumab also suggested the potential use of immunotherapy for mNPC as the median OS of 44 patients receiving nivolumab was 17.1 months. [33] In addition to monotherapy, a phase I clinical trial from China demonstrated that the therapeutic effect of camrelizumab combined with chemotherapy was superior to that of camrelizumab alone [34]. The superior efficacy of the camrelizumab combination was recently confirmed in a phase III randomized study [35]. Therefore, how to use immunotherapy in addition to chemotherapy and radiotherapy to maximize the survival of patients with mNPC is worth further effort.
Our study had several limitations that should be mentioned. The source of patients who underwent PCT followed by RT was restricted to one hospital, and the sample size was not sufficiently large. As this study was retrospective in nature, selection bias and imbalances existed. Plasma EBV testing results were not available, although EBV was an important factor for therapeutic monitoring and prognostic evaluations. In addition, quality of life, late toxicity and some details on the following lines of therapy were not considered in this study. Thus, prospective studies are warranted to support our findings.
Conclusions
The real-world study suggests that concurrent chemoradiotherapy significantly improves OS compared with radiotherapy alone after palliative chemotherapy in patients with de novo metastatic nasopharyngeal carcinoma. More specifically, concurrent chemoradiotherapy with single-agent platinum after 4–6 cycles of chemotherapy can be considered.
Availability of data and materials
The authenticity of this article has been validated by uploading the key raw data onto the Research Data Deposit public platform (www.researchdata.org.cn). All data will be shared upon request to the corresponding author.
Abbreviations
- NPC:
-
Nasopharyngeal carcinoma
- mNPC:
-
De novo metastatic nasopharyngeal carcinoma
- NCCN:
-
National Comprehensive Cancer Network
- PCT:
-
Palliative chemotherapy
- RT:
-
Radiotherapy
- OS:
-
Overall survival
- CCRT:
-
Concurrent chemoradiotherapy
- HR:
-
Hazard ratio
- WHO:
-
World Health Organization
- PF:
-
Cisplatin plus 5-fluorouracil
- TP:
-
Cisplatin plus docetaxel
- TPF:
-
Cisplatin plus docetaxel plus 5-fluorouracil
- IMRT:
-
Intensity-modulated radiotherapy
- CR:
-
Complete response
- PR:
-
Partial response
- SD:
-
Stable disease
- PD:
-
Progressive disease
- PFS:
-
Progression-free survival
- LRPFS:
-
Locoregional progression-free survival
- DPFS:
-
Distant progression-free survival
- PSM:
-
Propensity score matching
- CI:
-
Confidence interval
- KPS:
-
Karnofsky performance score
- EBV:
-
Epstein-Barr virus
References
Chen Y, Chan ATC, Le Q, et al. Nasopharyngeal carcinoma. Lancet. 2019;394(10192):64–80.
Wei KR, Zheng RS, Zhang SW, et al. Nasopharyngeal carcinoma incidence and mortality in China, 2013. Chin J Cancer. 2017;36(1):90.
Lee AW, Poon YF, Foo W, et al. Retrospective analysis of 5037 patients with nasopharyngeal carcinoma treated during 1976–1985: overall survival and patterns of failure. Int J Radiat Oncol Biol Phys. 1992;23(2):261–70.
Liao W, Tian M, Chen N. Characteristic and novel therapeutic strategies of nasopharyngeal carcinoma with synchronous metastasis. Cancer Manag Res. 2019;11:8431–42.
Head and Neck Cancers. NCCN clinical practice guidelines in oncology. Version 3.2021. https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf. Accessed 27 Apr 2021.
Tian YH, Zou WH, **ao WW, et al. Oligometastases in AJCC stage IVc nasopharyngeal carcinoma: A subset with better overall survival. Head Neck. 2016;38(8):1152–7.
Zeng L, Tian YM, Huang Y, et al. Retrospective analysis of 234 nasopharyngeal carcinoma patients with distant metastasis at initial diagnosis: therapeutic approaches and prognostic factors. PLoS ONE. 2014;9(9):e108070.
Chen M, Jiang R, Guo L, et al. Locoregional radiotherapy in patients with distant metastases of nasopharyngeal carcinoma at diagnosis. Chin J Cancer. 2013;32(11):604–13.
Rusthoven CG, Lanning RM, Jones BL, et al. Metastatic nasopharyngeal carcinoma: Patterns of care and survival for patients receiving chemotherapy with and without local radiotherapy. Radiother Oncol. 2017;124(1):139–46.
Verma V, Allen PK, Simone CN, et al. Addition of definitive radiotherapy to chemotherapy in patients with newly diagnosed metastatic nasopharyngeal cancer. J Natl Compr Canc Netw. 2017;15(11):1383–91.
You R, Liu YP, Huang PY, et al. Efficacy and safety of locoregional radiotherapy with chemotherapy vs chemotherapy alone in de novo metastatic nasopharyngeal carcinoma. JAMA Oncol. 2020;6(9):1345–52.
Soran A, Ozmen V, Ozbas S, et al. Randomized trial comparing resection of primary tumor with no surgery in stage IV breast cancer at presentation: protocol MF07-01. Ann Surg Oncol. 2018;25(11):3141–9.
Mickisch GH, Garin A, van Poppel H, et al. Radical nephrectomy plus interferon-alfa-based immunotherapy compared with interferon alfa alone in metastatic renal-cell carcinoma: a randomised trial. Lancet. 2001;358(9286):966–70.
Lin SJ, Tham IWK, Pan JJ, et al. Combined high-dose radiation therapy and systemic chemotherapy improves survival in patients with newly diagnosed metastatic nasopharyngeal cancer. Am J Clin Oncol. 2012;35(5):474–9.
Hu SX, He XH, Dong M, et al. Systemic chemotherapy followed by locoregional definitive intensity-modulated radiation therapy yields prolonged survival in nasopharyngeal carcinoma patients with distant metastasis at initial diagnosis. Med Oncol. 2015. https://doi.org/10.1007/s12032-015-0663-2.
Wang BC, Cao RB, Fu C, et al. The efficacy and safety of PD-1/PD-L1 inhibitors in patients with recurrent or metastatic nasopharyngeal carcinoma: A systematic review and meta-analysis. Oral Oncol. 2020;104:104640.
Lin JC, Jan JS, Hsu CY, et al. Phase III study of concurrent chemoradiotherapy versus radiotherapy alone for advanced nasopharyngeal carcinoma: positive effect on overall and progression-free survival. J Clin Oncol. 2003;21(4):631–7.
Guan Y, Liu S, Wang H, et al. Long-term outcomes of a phase II randomized controlled trial comparing intensity-modulated radiotherapy with or without weekly cisplatin for the treatment of locally recurrent nasopharyngeal carcinoma. Chin J Cancer. 2016. https://doi.org/10.1186/s40880-016-0081-7.
Crane CH, Janjan NA, Abbruzzese JL, et al. Effective pelvic symptom control using initial chemoradiation without colostomy in metastatic rectal cancer. Int J Radiat Oncol Biol Phys. 2001;49(1):107–16.
Kim MM, Rana V, Janjan NA, et al. Clinical benefit of palliative radiation therapy in advanced gastric cancer. Acta Oncol. 2008;47(3):421–7.
Bae SH, Park W, Choi DH, et al. Palliative radiotherapy in patients with a symptomatic pelvic mass of metastatic colorectal cancer. Radiat Oncol. 2011;6(1):52–52.
Wang Z, Ren ZG, Ma NY, et al. Intensity modulated radiotherapy for locally advanced and metastatic pancreatic cancer: a mono-institutional retrospective analysis. Radiat Oncol. 2015;10(1):14.
Comen E, Norton L, Massague J. Clinical implications of cancer self-seeding. Nat Rev Clin Oncol. 2011;8(6):369–77.
Reynders K, Illidge T, Siva S, et al. The abscopal effect of local radiotherapy: using immunotherapy to make a rare event clinically relevant. Cancer Treat Rev. 2015;41(6):503–10.
** Y, Shi YX, Cai XY, et al. Comparison of five cisplatin-based regimens frequently used as the first-line protocols in metastatic nasopharyngeal carcinoma. J Cancer Res Clin Oncol. 2012;138(10):1717–25.
Chan AT, Leung SF, Ngan RK, et al. Overall survival after concurrent cisplatin-radiotherapy compared with radiotherapy alone in locoregionally advanced nasopharyngeal carcinoma. J Natl Cancer Inst. 2005;97(7):536–9.
Shen LJ, Wang SY, **e GF, et al. Subdivision of M category for nasopharyngeal carcinoma with synchronous metastasis: time to expand the M categorization system. Chin J Cancer. 2015;34(10):450–8.
Zou X, You R, Liu H, et al. Establishment and validation of M1 stage subdivisions for de novo metastatic nasopharyngeal carcinoma to better predict prognosis and guide treatment. Eur J Cancer. 2017;77:117–26.
Sun XS, Liu LT, Liu SL, et al. Identifying optimal candidates for local treatment of the primary tumor among patients with de novo metastatic nasopharyngeal carcinoma: a retrospective cohort study based on Epstein-Barr virus DNA level and tumor response to palliative chemotherapy. BMC Cancer. 2019. https://doi.org/10.1186/s12885-019-5281-5.
Li WZ, Lv SH, Liu GY, et al. Development of a prognostic model to identify the suitable definitive radiation therapy candidates in de novo metastatic nasopharyngeal carcinoma: a real-world study. Int J Radiat Oncol Biol Phys. 2021;109(1):120–30.
Masterson L, Howard J, Gonzalez-Cruz J, et al. Immune checkpoint inhibitors in advanced nasopharyngeal carcinoma: Beyond an era of chemoradiation? Int J Cancer. 2020;146(8):2305–14.
Hsu C, Lee SH, Ejadi S, et al. Safety and antitumor activity of Pembrolizumab in patients with programmed death-ligand 1-positive nasopharyngeal carcinoma: results of the KEYNOTE-028 study. J Clin Oncol. 2017;35(36):4050–6.
Ma BBY, Lim WT, Goh BC, et al. Antitumor activity of Nivolumab in recurrent and metastatic nasopharyngeal carcinoma: an international, multicenter study of the Mayo Clinic phase 2 consortium (NCI-9742). J Clin Oncol. 2018;36(14):1412–8.
Fang WF, Yang YP, Ma YX, et al. Camrelizumab (SHR-1210) alone or in combination with gemcitabine plus cisplatin for nasopharyngeal carcinoma: results from two single-arm, phase 1 trials. Lancet Oncol. 2018;19(10):1338–50.
Yang Y, Qu S, Li J, et al. Camrelizumab versus placebo in combination with gemcitabine and cisplatin as first-line treatment for recurrent or metastatic nasopharyngeal carcinoma (CAPTAIN-1st): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 2021;S1470–2045(21):00302–8.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Key R & D Program of Precise Medical Research of China (NO. 2016YFC0904600), the National Natural Science Foundation of China (No. 81872464), and the Natural Science Foundation of Guangdong Province (No. 2018A030310236).
Author information
Authors and Affiliations
Contributions
Conception and design: SHZ, YTW and YFX; Administrative support: SRL, CC and YFX; Provision of study materials or patients: SRL and YFX; Collection and assembly of data: SHZ, YTW, ZLH, GNW, JTLand SRD; Data analysis and interpretation: SHZ, CC and YFX; Manuscript writing: All authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics board of Sun Yat-sen University Cancer Center and individual consent for this retrospective analysis was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Description of the radiotherapy. Figure S1.
Patient selection diagram. Figure S2. Overall Survival (OS) for patients treated with chemoradiotherapy (CRT) or palliative chemotherapy (PCT) in de novo metastatic nasopharyngeal carcinoma. Table S1. Details of common chemotherapy regimens. Table S2. Summary of studies related to locoregional radiotherapy in de novo metastatic nasopharyngeal carcinoma. Table S3. Adverse effects. References.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, SH., Wang, YT., Liu, SR. et al. Addition of chemoradiotherapy to palliative chemotherapy in de novo metastatic nasopharyngeal carcinoma: a real-world study. Cancer Cell Int 22, 36 (2022). https://doi.org/10.1186/s12935-022-02464-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12935-022-02464-7