Abstract
Background
Previous studies showed that the triglyceride-glucose (TyG) index was a better predictor of adverse cardiovascular events than triglycerides or fasting blood glucose alone. However, few studies have focused on new-onset hypertension. We aimed to explore the association of TyG index with new-onset hypertension in Chinese adults.
Methods
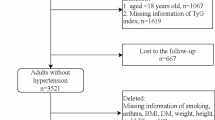
A total of 4,600 participants who underwent at least 2 rounds of visits from 2009 to 2015 in the China Health and Nutrition Survey were enrolled in this study. Our outcome of interest was new-onset hypertension. Multivariate Cox hazard regression models and restricted cubic spline were performed to explore the relationship between TyG index and new-onset hypertension.
Results
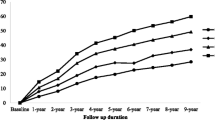
The mean (standard deviation, SD) age of the study population was 48.1 (13.6) years, and 2058 (44.7%) of the participants were men. The mean (SD) TyG index level was 8.6 (0.7). A total of 1,211 (26.3%) participants developed new-onset hypertension during a median (interquartile range) follow-up duration of 6.0 (2.0–6.1) years. The incidences of new-onset hypertension were 18.1%, 25.3%, 28.5%, and 33.4% by quartiles of TyG index [from quartile 1 (Q1) to Q4], respectively. The Cox model showed that high levels of TyG index were significantly associated with increased risk of new-onset hypertension (adjusted hazard ratio [aHR]: 1.29, 95% confidence interval [CI] 1.07–1.55, Q2; aHR, 1.24, 95% CI 1.03–1.49, Q3; aHR, 1.50, 95% CI 1.22–1.84, Q4) compared with Q1. Consistently, as a continuous variable, for every 1.0 increase in TyG index, there was a 17% increase in the risk of new-onset hypertension (aHR, 1.17; 95% CI 1.04–1.31). The associations were consistent in various subgroups and sensitivity analysis. The dose–response curve indicated a positive, linear association between TyG index and the risk of new-onset hypertension.
Conclusions
High TyG index was significantly associated with an increased risk of new-onset hypertension among Chinese adults. Our findings suggest that maintaining a relatively low level of TyG index might be effective in the primary prevention of hypertension.
Similar content being viewed by others
Introduction
Hypertension is the leading cause of cardiovascular events and all-cause mortality worldwide, which has become an emerging challenge for global public health [1]. In China, with an aging population and changing lifestyles, the prevalence of hypertension is also increasing year by year, with approximately one-third of the adult population, or more than 300 million people, suffering from hypertension between 2014 and 2015 [2, 3]. Therefore, early identifying the high-risk individuals and develo** effective primary prevention strategies are very urgent to reverse the rapidly rising trend of hypertension.
Disorders of lipoprotein metabolism, in particular elevated plasma triglycerides (TG), and elevated fasting blood glucose (FBG), are all established risk factors for cardiovascular disease, especially in hypertension [4, 5]. This could be explained by insulin resistance (IR) via at least three mechanisms: inflammatory endothelial dysfunction [6], ectopic synthesis of angiotensinogen [7], and hyperinsulinaemia overstimulating the renin-angiotensin–aldosterone system [8]. Recently, the triglyceride-glucose (TyG) index, which was calculated by using TG and FBG [9], has been proposed as a surrogate of IR, and correlated with various indices of IR [10, 11]. Previous research, however, has primarily focused on the association between TyG index and the incidence of prediabetes [12], diabetes [13], cardiovascular events [14, 15], and all-cause mortality [16, 17]. Very limited studies were conducted to explore the association of TyG index with new-onset hypertension [18,19,20,21,22,23,24,25,26,20,21,22,23], in children or adolescents [42], or in the elderly population [24]. Moreover, a prospective study in Spanish [18] reported a positive association between TyG index and hypertension in the general population during a long-term follow-up. Zheng et al. [19] also conducted another single-center, longitudinal study with 4,686 subjects followed up for 9 years, and demonstrated that TyG index could predict incident hypertension among the Chinese population. Of note, another study [28] reached a similar conclusion using a national cohort, but it was limited to middle-aged and older adults over 45 years. In addition, in a recent meta-analysis of 8 studies involving 200,044 general adult participants [43], the relative risk of hypertension was higher for the highest category of TyG index compared with the lowest. These studies were consistent with our study, which showed that high levels of TyG index were significantly associated with increased risk of new-onset hypertension and that a linear association was observed. Contrary to previous studies and our results, two cross-sectional studies [25, 26] did not find a significant association between TyG index and hypertension in obese or normal‐weight individuals. This may be attributed to the heterogeneity of the selected population and the sample size of the study. Therefore, further research on this topic is needed.
In stratified analysis, we found that most of the variables did not significantly modify the association between TyG index and new-onset hypertension, which indicates that the results of this study are applicable to the majority of the general population. However, the association between TyG index and new-onset hypertension was stronger in patients with low carbohydrate intake (< 288 g/day). Previous studies have reported that higher carbohydrate intake was related to a higher risk of hypertension [44, 45]. Therefore, individuals with higher carbohydrate intake will offset some of the risk from TyG index.
The potential mechanisms for the association between TyG index and new-onset hypertension may be explained by IR. IR has been confirmed by many studies to be significantly associated with hypertension by many mechanisms [6,7,8]. In recent years, many studies have concluded that TyG index is a surrogate of IR because it was correlated with various indices of IR, such as the M rates in the hyperinsulinaemic–euglycaemic clamp test [10] or the homeostasis of minimal assessment of insulin resistance (HOMA-IR) [46], and with the degree of carotid atherosclerosis [11]. More mechanistic studies are needed to further validate the relationship between TyG index, IR and hypertension.
The major strengths of this study were the 6-year national, longitudinal population-based study and the large number of subjects used to explore the relationship between TyG index and new-onset hypertension. However, certain limitations also existed in this study. First, although we adjusted for potential confounders such as demographics, dietary intake, and blood biochemical markers as much as possible, the E-values for the hazard ratio and lower confidence bound for the primary outcome were also small, which implies that little unmeasured confounding would be needed to reduce the observed association or its 95% CI to the null. However, residual confounding could not be completely eliminated. Second, limited by observational studies, we could not determine the causal relationship between TyG index and new-onset hypertension. Third, since the definition of hypertension was based on physician on-site blood pressure measurement data and questionnaires, there may be recall bias, but the findings remained consistent when we excluded questionnaire-based information on hypertension obtained in the sensitivity analysis. Forth, we could not explore the relationship between TyG index and different hypertension subtypes since information related to 24-h dynamic changes in blood pressure was not available. Fifth, considering that death was an inevitable competitive risk, we may underestimate the relationship between TyG index and new-onset hypertension. However, in our study population, only 74 (1.6%) participants died during the follow-up, which is unlikely to change the trend of results. Last, this study was limited to the Chinese general population, and more studies were needed to confirm the consistency of findings in other ethnic and national studies in the future.
Conclusions
In conclusion, we confirmed that high levels of TyG index were associated with higher risk of new-onset hypertension and showed a linear relationship through a longitudinal national cohort. Our findings suggest that maintaining a relatively low level of TyG index will help with the primary prevention of hypertension. In clinical practice, the TyG index is easily available, and clinicians could use this indicator to risk-stratify the general population in order to provide more personalized prevention or treatment.
Availability of data and materials
The datasets generated and/or analysed during the current study are available in the China Health and Nutrition Survey repository [http://www.cpc.unc.edu/projects/china].
Abbreviations
- TyG index:
-
Triglyceride-glucose index
- CHNS:
-
China Health and Nutrition Survey
- SD:
-
Standard deviation
- Q1:
-
Quartile 1
- Q2:
-
Quartile 2
- Q3:
-
Quartile 3
- Q4:
-
Quartile 4
- HR:
-
Hazard ratio
- aHR:
-
Adjusted hazard ratio
- TG:
-
Triglycerides
- FBG:
-
Fasting blood glucose
- IR:
-
Insulin resistance
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- BMI:
-
Body mass index
- WHR:
-
Waist to hip ratio
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- TC:
-
Total cholesterol
- HDL-C:
-
High density lipoprotein cholesterol
- LDL-C:
-
Low density lipoprotein cholesterol
- HbA1c:
-
Glycosylated hemoglobin
- BUN:
-
Blood urea nitrogen
- SCr:
-
Serum creatinine
- hsCRP:
-
High sensitivity C reactive protein
- FBI:
-
Fasting blood insulin
- DM:
-
Diabetes mellitus
- ADA:
-
American Diabetes Association
- CKD:
-
Chronic kidney disease
- eGFR:
-
Estimated glomerular filtration rate
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration equation
- WHO:
-
World Health Organization
- VIF:
-
Variance inflation factor
- RCS:
-
Restricted cubic spline
- IQR:
-
Interquartile range
- ACC:
-
American College of Cardiology
- AHA:
-
American Heart Association
- PS:
-
Propensity score
- PSM:
-
Propensity Score Matching
- ASCVD:
-
Atherosclerotic Cardiovascular Disease
- HOMA-IR:
-
Homeostasis of minimal assessment of insulin resistance
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021. https://doi.org/10.1016/j.jacc.2020.11.010.
Lewington S, Lacey B, Clarke R, Guo Y, Kong XL, Yang L, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016;176:524–32. https://doi.org/10.1001/jamainternmed.2016.0190.
Li Y, Yang L, Wang L, Zhang M, Huang Z, Deng Q, et al. Burden of hypertension in China: a nationally representative survey of 174,621 adults. Int J Cardiol. 2017;227:516–23. https://doi.org/10.1016/j.ijcard.2016.10.110.
Choi JW, Park JS, Lee CH. Interactive effect of high sodium intake with increased serum triglycerides on hypertension. PLoS One. 2020;15:e0231707. https://doi.org/10.1371/journal.pone.0231707.
Kuwabara M, Hisatome I. The relationship between fasting blood glucose and hypertension. Am J Hypertens. 2019;32:1143–5. https://doi.org/10.1093/ajh/hpz147.
Morales-Villegas E. Dyslipidemia, hypertension and diabetes metaflammation. A Unique mechanism for 3 risk factors. Curr Hypertens Rev. 2014. https://doi.org/10.2174/1573402110666140702091315.
Egan BM. Insulin resistance and the sympathetic nervous system. Curr Hypertens Rep. 2003;5:247–54. https://doi.org/10.1007/s11906-003-0028-7.
Franco OH, Massaro JM, Civil J, Cobain MR, O’Malley B, D’Agostino RB Sr. Trajectories of entering the metabolic syndrome: the framingham heart study. Circulation. 2009;120:1943–50. https://doi.org/10.1161/CIRCULATIONAHA.109.855817.
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6:299–304. https://doi.org/10.1089/met.2008.0034.
Guerrero-Romero F, Simental-Mendia LE, Gonzalez-Ortiz M, Martinez-Abundis E, Ramos-Zavala MG, Hernandez-Gonzalez SO, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metab. 2010;95:3347–51. https://doi.org/10.1210/jc.2010-0288.
Du T, Yuan G, Zhang M, Zhou X, Sun X, Yu X. Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol. 2014;13:146. https://doi.org/10.1186/s12933-014-0146-3.
Wen J, Wang A, Liu G, Wang M, Zuo Y, Li W, et al. Elevated triglyceride-glucose (TyG) index predicts incidence of prediabetes: a prospective cohort study in China. Lipids Health Dis. 2020;19:226. https://doi.org/10.1186/s12944-020-01401-9.
Xuan X, Hamaguchi M, Cao Q, Okamura T, Hashimoto Y, Obora A, et al. U-shaped association between the triglyceride-glucose index and the risk of incident diabetes in people with normal glycemic level: a population-base longitudinal cohort study. Clin Nutr. 2021;40:1555–61. https://doi.org/10.1016/j.clnu.2021.02.037.
Park B, Lee YJ, Lee HS, Jung DH. The triglyceride-glucose index predicts ischemic heart disease risk in Koreans: a prospective study using National Health Insurance Service data. Cardiovasc Diabetol. 2020;19:210. https://doi.org/10.1186/s12933-020-01186-2.
Barzegar N, Tohidi M, Hasheminia M, Azizi F, Hadaegh F. The impact of triglyceride-glucose index on incident cardiovascular events during 16 years of follow-up: Tehran lipid and glucose study. Cardiovasc Diabetol. 2020;19:155. https://doi.org/10.1186/s12933-020-01121-5.
Liao Y, Zhang R, Shi S, Zhao Y, He Y, Liao L, et al. Triglyceride-glucose index linked to all-cause mortality in critically ill patients: a cohort of 3026 patients. Cardiovasc Diabetol. 2022;21:128. https://doi.org/10.1186/s12933-022-01563-z.
Liu X, Tan Z, Huang Y, Zhao H, Liu M, Yu P, et al. Relationship between the triglyceride-glucose index and risk of cardiovascular diseases and mortality in the general population: a systematic review and meta-analysis. Cardiovasc Diabetol. 2022;21:124. https://doi.org/10.1186/s12933-022-01546-0.
Sanchez-Inigo L, Navarro-Gonzalez D, Pastrana-Delgado J, Fernandez-Montero A, Martinez JA. Association of triglycerides and new lipid markers with the incidence of hypertension in a Spanish cohort. J Hypertens. 2016;34:1257–65. https://doi.org/10.1097/HJH.0000000000000941.
Zheng R, Mao Y. Triglyceride and glucose (TyG) index as a predictor of incident hypertension: a 9-year longitudinal population-based study. Lipids Health Dis. 2017;16:175. https://doi.org/10.1186/s12944-017-0562-y.
Bala C, Gheorghe-Fronea O, Pop D, Pop C, Caloian B, Comsa H, et al. The association between six surrogate insulin resistance indexes and hypertension: a population-based study. Metab Syndr Relat Disord. 2019;17:328–33. https://doi.org/10.1089/met.2018.0122.
Wang K, He G, Zhang Y, Yin J, Yan Y, Zhang Y, et al. Association of triglyceride-glucose index and its interaction with obesity on hypertension risk in Chinese: a population-based study. J Hum Hypertens. 2021;35:232–9. https://doi.org/10.1038/s41371-020-0326-4.
Zhu B, Wang J, Chen K, Yan W, Wang A, Wang W, et al. A high triglyceride glucose index is more closely associated with hypertension than lipid or glycemic parameters in elderly individuals: a cross-sectional survey from the reaction study. Cardiovasc Diabetol. 2020;19:112. https://doi.org/10.1186/s12933-020-01077-6.
Lee DH, Park JE, Kim SY, Jeon HJ, Park JH. Association between the triglyceride-glucose (TyG) index and increased blood pressure in normotensive subjects: a population-based study. Diabetol Metab Syndr. 2022;14:161. https://doi.org/10.1186/s13098-022-00927-5.
Jian S, Su-Mei N, Xue C, Jie Z, Xue-Sen W. Association and interaction between triglyceride-glucose index and obesity on risk of hypertension in middle-aged and elderly adults. Clin Exp Hypertens. 2017;39:732–9. https://doi.org/10.1080/10641963.2017.1324477.
Liu XZ, Fan J, Pan SJ. METS-IR, a novel simple insulin resistance indexes, is associated with hypertension in normal-weight Chinese adults. J Clin Hypertens (Greenwich). 2019;21:1075–81. https://doi.org/10.1111/jch.13591.
Morales-Gurrola G, Simental-Mendía LE, Castellanos-Juárez FX, Salas-Pacheco JM, Guerrero-Romero F. The triglycerides and glucose index is associated with cardiovascular risk factors in metabolically obese normal-weight subjects. J Endocrinol Invest. 2020;43:995–1000. https://doi.org/10.1007/s40618-020-01184-x.
Zhang F, Zhang Y, Guo Z, Yang H, Ren M, **ng X, et al. The association of triglyceride and glucose index, and triglyceride to high-density lipoprotein cholesterol ratio with prehypertension and hypertension in normoglycemic subjects: a large cross-sectional population study. J Clin Hypertens (Greenwich). 2021;23:1405–12. https://doi.org/10.1111/jch.14305.
Liu T, Xuan H, Yin J, Wang L, Wang C, Xu X, et al. Triglyceride glucose index increases significantly risk of hypertension development in Chinese individuals aged >/=45 years old: analysis from the China health and retirement longitudinal study. J Multidiscip Healthc. 2023;16:63–73. https://doi.org/10.2147/JMDH.S391905.
Popkin BM, Du S, Zhai F, Zhang B. Cohort profile: the china health and nutrition survey–monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol. 2010;39:1435–40. https://doi.org/10.1093/ije/dyp322.
Zhang B, Zhai FY, Du SF, Popkin BM. The China health and nutrition survey, 1989–2011. Obes Rev. 2014;15(Suppl 1):2–7. https://doi.org/10.1111/obr.12119.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–7. https://doi.org/10.7326/0003-4819-147-8-200710160-00010.
Assoc AD. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2005;28:S37–42.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12. https://doi.org/10.7326/0003-4819-150-9-200905050-00006.
Kim JH. Multicollinearity and misleading statistical results. Korean J Anesthesiol. 2019;72:558–69. https://doi.org/10.4097/kja.19087.
Kim DK. Regression analysis of interval-censored survival data with covariates using log-linear models. Biometrics. 1997;53:1274–83.
Whelton PK, Carey RM, Aronow WS, Casey DE, Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension, 71: 1269–1324, 2018 https://doi.org/10.1161/HYP.0000000000000066
Zhao QY, Luo JC, Su Y, Zhang YJ, Tu GW, Luo Z. Propensity score matching with R: conventional methods and new features. Ann Transl Med. 2021;9:812. https://doi.org/10.21037/atm-20-3998.
Haneuse S, VanderWeele TJ, Arterburn D. Using the E-Value to assess the potential effect of unmeasured confounding in observational studies. JAMA. 2019;321:602–3. https://doi.org/10.1001/jama.2018.21554.
Tao LC, Xu JN, Wang TT, Hua F, Li JJ. Triglyceride-glucose index as a marker in cardiovascular diseases: landscape and limitations. Cardiovasc Diabetol. 2022. https://doi.org/10.1186/s12933-022-01511-x.
Sanchez-Inigo L, Navarro-Gonzalez D, Fernandez-Montero A, Pastrana-Delgado J, Martinez JA. The TyG index may predict the development of cardiovascular events. Eur J Clin Invest. 2016;46:189–97. https://doi.org/10.1111/eci.12583.
Won KB, Park EJ, Han D, Lee JH, Choi SY, Chun EJ, et al. Triglyceride glucose index is an independent predictor for the progression of coronary artery calcification in the absence of heavy coronary artery calcification at baseline. Cardiovasc Diabetol. 2020;19:34. https://doi.org/10.1186/s12933-020-01008-5.
Simental-Mendia LE, Hernandez-Ronquillo G, Gamboa-Gomez CI, Gomez-Diaz R, Rodriguez-Moran M, Guerrero-Romero F. The triglycerides and glucose index is associated with elevated blood pressure in apparently healthy children and adolescents. Eur J Pediatr. 2019;178:1069–74. https://doi.org/10.1007/s00431-019-03392-x.
Wang Y, Yang W, Jiang X. Association between triglyceride-glucose index and hypertension: a meta-analysis. Front Cardiovasc Med. 2021;8:644035. https://doi.org/10.3389/fcvm.2021.644035.
He DL, Sun N, **ong ST, Qiao YA, Ke CF, Shen YP. Association between the proportions of carbohydrate and fat intake and hypertension risk: findings from the China Health and Nutrition Survey. J Hypertens. 2021;39:1386–92. https://doi.org/10.1097/Hjh.0000000000002803.
Qi SF, Cao YJ, Wang HJ, Zhang B, Yan J, Tian QB. Associations of carbohydrate intake with new-onset hypertension subtypes: results from the China Health and Nutrition Survey (2000–2011). Front Nutr. 2021;8:728774. https://doi.org/10.3389/fnut.2021.728774.
Abbasi F, Reaven GM. Comparison of two methods using plasma triglyceride concentration as a surrogate estimate of insulin action in nondiabetic subjects: triglycerides x glucose versus triglyceride/high-density lipoprotein cholesterol. Metabolism. 2011;60:1673–6. https://doi.org/10.1016/j.metabol.2011.04.006.
Acknowledgements
This analysis uses data from CHNS. The authors thank the CHNS research team and the field team for collecting and providing the data. The authors also thank all volunteers and staff involved in this research.
Funding
This study is supported by grants the National Natural Science Foundation of China (81900626 to Dr S. Nie) and Guangzhou Basic and Applied Basic Research Foundation (SL2022A04J02062 to Dr Y. Li).
Author information
Authors and Affiliations
Contributions
Drs LS, SN and YL had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: LS, Gao, YL. Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: LS, Gao, YL, SN. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: SN, LS and Gao. Obtained funding: none. Supervision: SN, LS and YL. Other—data collection: YL, RX, Luo, RC, PL, YZ, Liu, ZD. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional review committees of the University of North Carolina at Chapel Hill, the National Institute of Nutrition and Food Safety, and the Chinese Center for Disease Control and Prevention. Each participant provided their written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
The variance inflation factor (VIF) values for all variables in our model.

Additional file 2: Figure S2.
Distribution of TyG index in the study population.
Additional file 3: Figure S3.
E-value analysis to assess the extent of unmeasured confounding that would be required to negate the observed results.
Additional file 4: Table S1.
Distribution of missing variables. Table S2. Baseline characteristics of excluded and included participants. Table S3. Baseline characteristics of participants stratified by outcome. Table S4. The association of TyG index with new-onset hypertension using interval censored Cox regression model. Table S5. The association of TyG index with new-onset hypertension after excluding the questionnaire data defining hypertension. Table S6. The association of TyG index with new-onset hypertension in participants limited with two follow-up visits. Table S7. The association of TyG index with new-onset hypertension defined by the novel diagnostic criteria (SBP/DBP: 130/80). Table S8. Baseline characteristics of participants stratified by TyG index quartiles after 1:1 propensity score matching. Table S9. The association of TyG index with new-onset hypertension after 1:1 propensity score matching. Table S10. The association of TyG index with new-onset hypertension after excluding individuals with DM and/or CKD. Table S11. The association of TyG index with new-onset hypertension after imputing the baseline missing values.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gao, Q., Lin, Y., Xu, R. et al. Positive association of triglyceride-glucose index with new-onset hypertension among adults: a national cohort study in China. Cardiovasc Diabetol 22, 58 (2023). https://doi.org/10.1186/s12933-023-01795-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-023-01795-7