Abstract
Background
Patients with idiopathic pulmonary fibrosis (IPF) frequently have multiple comorbidities, which may influence survival but go under-recognised in clinical practice. We therefore report comorbidity, antifibrotic treatment use and survival of patients with IPF observed in the multi-national EMPIRE registry.
Methods
For this prospective IPF cohort, demographics, comorbidities, survival and causes of death were analysed. Comorbidities were noted by the treating physician based on the patient’s past medical history or as reported during follow-up. Comorbidities were defined as prevalent when noted at enrolment, or as incident when recorded during follow-up. Survival was analysed by Kaplan–Meier estimates, log-rank test, and Cox proportional hazards models. Hazard ratios (HR) were adjusted for gender, age, smoking status and FVC at enrolment.
Results
A population of 3,580 patients with IPF from 11 Central and Eastern European countries was followed every 6 months for up to 6 years. At enrolment, 91.3% of patients reported at least one comorbidity, whereas more than one-third (37.8%) reported four or more comorbidities. Five-year survival was 53.7% in patients with no prevalent comorbidities, whereas it was 48.4%, 47.0%, 43.8% and 41.1% in patients with 1, 2, 3 and ≥ 4 comorbidities, respectively. The presence of multiple comorbidities at enrolment was associated with significantly worse survival (log-rank test P = 0.007). Adjusted HRs indicate that risk of death was increased by 44% in patients with IPF reporting ≥ 4 comorbidities at baseline compared with no comorbidity (P = 0.021). The relationship between number of comorbidities and decreased survival was also seen in patients receiving antifibrotic treatment (63% of all patients; log-rank test P < 0.001). Comorbidity as cause of death was identified in at least 26.1% of deaths.
Conclusions
The majority of patients with IPF demonstrate comorbidities, and many have comorbidity-related deaths. Increasing numbers of comorbidities are associated with worse survival; and this pattern is also present in patients receiving antifibrotic therapy.
Similar content being viewed by others
Introduction
Idiopathic pulmonary fibrosis (IPF) is a devastating interstitial lung disease primarily affecting older adults, associated with progressive loss of lung function [1]. Prevalence estimates vary widely, ranging from 1.25 to 63 IPF cases per 100,000 persons, depending on definitions and study methodology [2,3,4,5]. Prognosis for IPF is poor and mortality rates are high, with a reported survival of 3–5 years after diagnosis [6, 7].
In patients with IPF, symptomatic disease is very frequent and associated with increased healthcare costs [8]. In addition to a high symptom burden, many patients have pulmonary or extrapulmonary comorbidities that can negatively impact on quality of life and survival [9, 10]. Causes of comorbidities include shared underlying risk factors such as age and smoking; IPF itself leading to hypoxemia and pulmonary hypertension; medications used for IPF treatment, such as diabetes mellitus following treatment with steroids; and a combination of these mechanisms [11, 12]. Recent data indicate that some of these associations are driven by genetic variations [13]. Coronary heart disease [14], diabetes mellitus [15], pulmonary hypertension [16, 17], chronic obstructive pulmonary disease (COPD) [12, 18], obstructive sleep apnoea (OSA) [19], gastroesophageal reflux [20, 21], and lung cancer [22] are all frequently associated with IPF. Given the effect of comorbidities on patients’ quality of life [10] and survival [9], comprehensive assessment of patients with IPF should include early recognition and appropriate management of comorbidities [23].
Antifibrotic treatment of IPF with nintedanib or pirfenidone can slow lung function decline, decrease the risk for acute exacerbation, and reduce mortality [24,25,26,27]. However, comorbidities, especially if left unrecognised and untreated, can have a negative impact on survival in patients with IPF and thus might reduce the positive effect of antifibrotic treatment [9, 23].
The reported prevalence of comorbidities in IPF varies widely, depending on the type of study or methodology involved (i.e., whether data are derived from clinical trials, patient registries or observational data), the population studied, and the diagnostic criteria applied. However, when data for comorbidities in IPF are compared from a single type of study, such as IPF patient registries, the pattern is more consistent [28].
We aimed to estimate the prevalence of comorbidities at the time of enrolment in the European MultiPartner IPF REgistry (EMPIRE) as well as the incidence of comorbidities during follow-up, and to analyse the impact on survival. For a well-defined IPF cohort, we included 3,580 patients from Central and Eastern Europe, with the EMPIRE registry currently the largest database of this kind [29].
In EMPIRE, patients were seen at least every 6 months and the presence of comorbidities assessed using a pre-defined, standardised, web-based data entry tool. We describe and analyse comorbidities in two ways. Firstly, we number comorbidities present at enrolment (prevalent), and secondly, we report the total number of comorbidities recorded at enrolment and up to the end of follow-up.
Methods
EMPIRE is a non-interventional, multinational registry of patients with IPF that was established in September 2014 (http://empire.registry.cz/index-en.php). The registry currently collects data from 11 Central and Eastern European countries: Austria, Bulgaria, Croatia, Czech Republic, Hungary, Israel, Macedonia, Poland, Serbia, Slovakia, and Turkey [29]. Patient data were entered into the registry database by the treating physician. When a patient completed their follow-up visit, clinical data were recorded using an online database based on the TrialDB system [28]. All data transfers were encrypted. Data validation took place both during data input (validation and testing for internal consistency between variables) and during data processing (identification and exclusion of missing, outlying, and otherwise implausible observations).
EMPIRE is conducted in accordance with the Declaration of Helsinki. The study protocol and its amendments were approved by the Ethics Committee of each participating institution. All records in the EMPIRE registry are fully anonymised and de-identified.
Data for all patients registered in EMPIRE between 5 December 2014 and 14 May 2020 were extracted for analysis. To be eligible for inclusion in this analysis, patients had to have a diagnosis of IPF defined according to 2011 European Respiratory Society/American Thoracic Society/Japanese Respiratory Society/Latin American Thoracic Society criteria [30, 31]. Final IPF diagnosis was always determined by a local multidisciplinary team (MDT). The date of IPF diagnosis was the date recorded by the treating physician. Patients were excluded if the date of diagnosis was unknown or if IPF diagnosis was changed during follow-up.
Multidisciplinary team diagnosis was reached according to the operational principles of study centres and strictly followed published guidelines. Date of IPF diagnosis, demographic characteristics, lung function, comorbidities, antifibrotic treatment, survival status, and cause of death were captured for analysis. Comorbidities were noted by the treating physician based on a patient’s medical history or as reported during follow-up.
Comorbidities present at the time of the first visit to EMPIRE (enrolment visit) were recorded as prevalent comorbidities, and comorbidities noted at the time of enrolment and during follow-up were recorded as the cumulative number of comorbidities. Prevalent comorbidities and the cumulative number of comorbidities were grouped according to the organ/ system involved (cardiovascular; gastrointestinal, metabolic; urogenital; pulmonary; blood and immunity; other) and classified according to specific disease (e.g., arterial hypertension, coronary heart disease, pulmonary hypertension). For survival analyses, patients were categorised according to the number of comorbidities (0, 1, 2, 3, and ≥ 4) as present at enrolment (prevalent), and as from enrolment to the end of follow-up (cumulative number).
Treatment of IPF with antifibrotics (pirfenidone or nintedanib) was recorded by the treating physician. Cause of death was recorded by the treating physician and then categorised centrally.
Statistical methods
Characteristics of patients from the time of enrolment in the registry and up to the end of follow-up are reported. Continuous variables are presented as median (5th and 95th percentile), and categorical outcomes are described by absolute and relative frequencies. The Kruskal–Wallis test was used for continuous data, and the maximum-likelihood chi-squared test was used for categorical data. For survival analyses, survival time was defined as the time between date of enrolment and date of death, loss to follow-up, or the end of follow-up defined by data analysis (i.e., 14 May 2020), whichever was earliest.
To analyse survival, Kaplan–Meier graphs were derived, and log-rank tests used to assess the difference between survival curves according to the number of comorbidities. For multiple comparisons, a Bonferroni correction was used to assess the difference between groups of patients. The association between the number of comorbidities (0 vs 1, 0 vs 2, 0 vs 3, and 0 vs ≥ 4) and survival was further described using Cox proportional hazards models; both unadjusted and adjusted (for gender, age, smoking status and forced vital capacity [FVC] % predicted at enrolment) estimates are presented. Statistical significance was set at P < 0.05.
Results
Study population
As of 14 May 2020, data from the EMPIRE registry were available for 3580 patients with an MDT-diagnosis of IPF; of those, 3286 (91.8%) had a high-resolution computed tomography scan, and 798 (22.3%) underwent lung biopsy (Table 1).
Data originated from 11 countries, with patients from the Czech Republic accounting for one-third (n = 1174; 32.8%) of the analysis population. At the time of analysis, 949/3580 (26.5%) patients had died and 451 (12.6%) had observations censored before the end of follow-up; of these, 331 were lost to follow-up; 73 underwent lung transplantation; and 47 were censored for other, unspecified reasons. Patient characteristics at enrolment are presented in Table 1. Median (5th–95th percentile) age at registry enrolment was 69 (53–82) years, and more than two-thirds of patients (70.7%) were male.
Comorbidities at enrolment and during follow-up
At the time of enrolment, most patients (91.3%) had at least one comorbidity, 56.4% had at least three, and more than one-third (37.8%) had at least four comorbidities. The number of comorbidities increased with age, as expected. Median follow-up time was 13.8 months (5th–95th percentile 0.0–58.3 months).
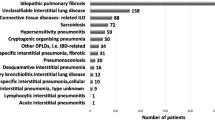
Most patients (73.9%) had a cardiovascular type of comorbidity recorded either at baseline or during follow-up. The most common disease-specific comorbidities were arterial hypertension (53.0%), diabetes mellitus (24.0%), hyperlipidaemia (23.5%), coronary heart disease (23.3%), and gastroesophageal reflux (21.1%) (Table 2). Less common, but still affecting ≥ 5– < 10% of patients, were comorbidities including cancer other than lung cancer, depression, thyroid disease, respiratory infection, obesity, COPD, embolism and heart attack (Table 2).
The frequency of comorbidities varied considerably between countries (Table 2; Additional file 1: Fig. S1). Data for each individual country are presented in Additional file 1: Figs. S1–7).
Survival outcomes
Up to the end of 5 years of follow-up, 949 patients had died (Table 3). The most frequently reported cause of death was IPF-related respiratory failure (54.6%), followed by acute exacerbation of IPF (9.5%). Causes of death not considered IPF-related included cardiovascular disease (heart failure, cardiac arrest, stroke; 11.1%), pneumonia (4.9%), lung cancer (3.9%), other malignancy (2.7%) and other causes (3.5%). In total, comorbidity-related death was evidenced in at least 26.1% of cases, while cause of death was unknown in 9.8%.
Some associated disorders recorded at initial visit were associated with significantly increased risk of death in comparison with patients with no comorbidities (adjusted hazard ratio [HR]): namely pulmonary hypertension (1.93, P < 0.001), stroke (2.17, P < 0.001), respiratory infection (3.20, P = 0.031), emphysema (2.08, P < 0.001), lung cancer (3.39, P < 0.001), and obesity (1.92, P = 0.001). Patients with gastroesophageal reflux had slightly lower risk of death, with a borderline statistical significance (0.70, P = 0.043) (Table 4).
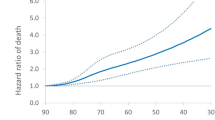
The presence of multiple comorbidities at enrolment was associated with significantly worse survival (log-rank test P = 0.007) (Fig. 1A); and both Kaplan–Meier curves and Cox proportional hazards analysis indicated a dose–response-like relationship. In unadjusted Cox proportional hazards models, presence of ≥ 4 comorbidities at baseline compared with no comorbidity was associated with an unadjusted 51% increased risk of death (P = 0.004); following adjustment for gender, age, and FVC at baseline, the risk was 44% (P = 0.021).
Median overall survival was 52.1 months for the whole cohort. Median overall survival was not reached for those patients with no comorbidities at enrolment, whereas it was 58.9 months for those with 1 comorbidity, and 56.6, 47.2 and 45.5 months in patients with 2, 3 and ≥ 4 comorbidities, respectively (Fig. 1A). The 5-year overall probability of survival was 53.7% (95% confidence interval [CI] 40.8–64.9) in patients with no comorbidities, whereas it was 48.4% (39.3–56.9) in those with a 1 comorbidity, and 47.0% (38.4–55.2), 43.8% (36.6–50.9) and 41.1% (35.8–46.0) in patients with 2, 3 and ≥ 4 comorbidities respectively at enrolment.
The cumulative number of comorbidities (those recorded at enrolment and during follow-up combined) was not associated with survival (log-rank test P = 0.216); in addition, neither the unadjusted nor adjusted HR analysis indicated a dose–response-like relationship (Fig. 1B).
During 5 years of follow-up nearly two-thirds of patients (2,257/3,580; 63.0%) had received antifibrotic treatment with pirfenidone and/or nintedanib. Median (5th; 95th percentile) duration of antifibrotic treatment was 10.3 (0.9; 45.3) months (Additional file 1: Table S1). Median overall survival was 66.3 months for patients receiving antifibrotic treatment and 36.0 months for those not receiving antifibrotic treatment. Survival analysis of patients receiving antifibrotic treatment indicated a significantly different survival according to the number of comorbidities at enrolment (log-rank test P < 0.001) (Fig. 2A). Cox proportional hazards models also indicated increased risk of death in parallel with the number of comorbidities. In patients receiving antifibrotic treatment, median overall survival was not reached for those with none, 1, or 2 comorbidities, whereas it was 57.8 and 59.0 months for those with 3 or ≥ 4 comorbidities, respectively (Fig. 2A). In patients not receiving antifibrotic treatment, no association between survival and number of comorbidities was seen (log-rank test P = 0.995) (Fig. 2B).
Overall survival in patients with IPF by comorbidities at enrolment according to antifibrotic therapy. Comorbidities for (a) those receiving antifibrotic therapy (n = 2257) and (b) those not receiving antifibrotic therapy (n = 1323). Antifibrotic therapies were nintedanib or pirfenidone. IPF, idiopathic pulmonary fibrosis
Discussion
Main findings
The multinational EMPIRE registry includes patients with IPF managed in real-world settings across 11 countries of Central and Eastern Europe. In this analysis of 3,580 patients in the registry (2014–2020), the median number of comorbidities at enrolment was three, and a greater number of comorbidities was associated with significantly worse survival, resulting in a 41% increased risk of death for those with four or more comorbidities at baseline.
Analysis of patients receiving antifibrotic treatment indicated comparable differences in survival according to the number of comorbidities at enrolment (42% increased risk of death associated with four or more comorbidities).
Comparison of reported comorbidities
Multimorbidity is known to be common in patients with IPF [12, 17, 21, 32] and, in agreement with published data, the majority of patients in the EMPIRE registry had at least one comorbidity. It is widely accepted that the risk of comorbidities such as arterial hypertension, coronary artery disease, lung cancer or osteoporosis increases with age, and this was confirmed in our study. Few studies provide detailed information on the number of comorbidities, and those have usually shown that multimorbidity is very common, especially in older IPF populations [12, 33], as reported in EMPIRE. Similarly, an analysis of 272 patients with IPF from a tertiary referral centre in Germany found that 89% had at least one comorbidity, and 30% had four or more comorbidities [9]. In another retrospective single-centre cohort of 352 patients with IPF, 79.3% had ≥ 1 comorbidities and 47.2% had ≥ 2 comorbidities [34].
The most frequently reported comorbidities in the EMPIRE registry were arterial hypertension, diabetes mellitus, hyperlipidaemia, coronary heart disease and, gastroesophageal reflux. Other registries have found similar patterns of comorbidities in IPF, but with sometimes strikingly different prevalence (Additional file 1: Fig. S8) [9, 16, 21, 35,36,37,38]. Publication of a systematic review of 126 clinical trials involving patients with IPF [12] has enabled comparisons to be made between highly scrutinised clinical trial populations and real-world patients from IPF registries [9, 16, 21, 35, 36]. The reported prevalence of comorbidities may differ, but almost all comorbidities listed are more common in clinical trial populations than in eight different registries, including EMPIRE (Additional file 1: Fig. S8) [9, 16, 21, 35,36,37,38]. This suggests that comorbidities are routinely and substantially under-recognised in clinical practice. Significant differences in reported comorbidities may be related to the type of study performed, which included retrospective analyses of single-centre experiences [9, 35], prospective or retrospective analyses of national registries [21, 36, 39] and analyses of administrative datasets [33, 40]. These differences are also dependent on the duration of the observation period [12, 41].
Comorbidities and survival
Comorbidities are known to impact on IPF [23], and are linked to poor quality of life and increased mortality [42,43,44,45]. However, there is no clear answer on whether, and to what extent, comorbidities influence IPF progression in addition to their own direct adverse health effects.
In this EMPIRE analysis, the presence of multiple comorbidities at enrolment was associated with significantly worse survival. These findings are in line with published data [9].
However, it should be noted that a simple numerical increase in comorbidities does not necessarily result in worse outcomes, without considering the type and severity of the condition. In the present analysis, the cumulative number of comorbidities noted from enrolment up to the end of follow-up was not related to survival, possibly because comorbidities appearing later in the course of IPF may not have as big an impact on survival as those present earlier in the disease.
Previous reports have identified cardiovascular disease as a significant predictor of mortality in patients with IPF [9, 12, 46]; arteriosclerosis, other cardiovascular diseases (e.g., valvular heart disease), malignancy, and gastroesophageal reflux have all been associated with reduced survival in IPF [9, 12, 46]. Cardiovascular causes accounted for a substantial number of deaths in the EMPIRE population. Mortality has previously been reported to be higher among patients with IPF who had pulmonary comorbidities such as COPD, lung cancer and OSA [46, 47]. A number of comorbidities have therefore been found to be consistently associated with shorter survival in IPF [9, 12, 14, 46,47,48,49].
Recently, Torrisi et al. developed and validated the first-ever clinical prediction model and an index point score (TORVAN model and index) for all-cause mortality in IPF that includes comorbidities as parameters [23]. Relatively few comorbidities influenced the prediction of survival, and gender became a less important prognostic factor within the context of comorbidities [23].
Antifibrotic treatment
Nearly two-thirds of all patients in this study had been prescribed pirfenidone or nintedanib, similarly to other studies [10, 16, 21, 36]. Treatment with antifibrotic therapy may indicate patients with more advanced disease stage or severity, which may be associated with more comorbidities. One of the main findings of this EMPIRE analysis was a significantly greater survival in patients with fewer comorbidities at enrolment. This finding was seen in patients treated with antifibrotics, but not in those who had not received antifibrotic treatment. Although there was no significant difference in the proportion of IPF-related versus non-IPF-related deaths between antifibrotic and non-antifibrotic-treated patients, the difference of survival as related to comorbidities was prominent only in those treated with antifibrotics, indicating that the influence of IPF itself on survival was lessened.
Recent analysis of the INSIGHT-IPF observational study demonstrated that antifibrotic treatment was associated with improved survival, independent from age [50], emphasising the importance of early introduction of antifibrotic treatment in IPF [50]—as also seen in the EMPIRE cohort.
Study limitations
Over 3500 patients are included in the analyses and data were derived from 11 different countries; therefore, between-country differences in clinical practice, access to diagnostic procedures, availability of treatment for IPF, and healthcare system financing may have influenced the findings. Differences between countries in comorbidity frequency may be explained by inconsistent reporting, under-reporting, or differences in case definitions and applied diagnostic criteria. In addition, the earliest data were recorded before the publication of updated IPF treatment guidelines in 2015 [31], meaning that some patients may have received corticosteroids as well as antifibrotic therapy once it was available. Thus, reported longitudinal (survival) outcomes might reflect different treatment approaches over time. Another limitation is that the analysis of survival by number of comorbidities does not account for differences in type or severity of comorbidity. However, the survival analysis was adjusted for gender, age, smoking status and FVC% predicted at baseline as these factors could be associated with comorbidities and may influence survival [11, 12].
Summary
Patient registries can provide valuable real-world information about the prevalence of comorbidities. Findings from the EMPIRE registry in Central and Eastern Europe, the largest IPF registry in the world, indicate that multimorbidity is common. The presence of multiple comorbidities at enrolment appears to be associated with worse survival, an effect particularly present in patients receiving antifibrotic treatment.
In conclusion, comorbidities in IPF are common but may often be under-recognised in clinical practice. Raising awareness of the impact that comorbidities can have on these patients would help to improve recognition and management in clinical practice. Optimising detection and management of comorbidities would help to improve outcomes in patients with IPF; with improved survival associated with antifibrotic treatment, the influence of comorbidities now has greater influence than previously.
Availability of data and materials
Data can be requested from the EMPIRE registry following approval from the steering committee.
Abbreviations
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- EMPIRE:
-
European MultiPartner IPF REgistry
- FVC:
-
Forced vital capacity
- HR:
-
Hazard ratio
- IPF:
-
Idiopathic pulmonary fibrosis
- MDT:
-
Multidisciplinary team
- OSA:
-
Obstructive sleep apnoea
References
King TE Jr, Pardo A, Selman M. Idiopathic pulmonary fibrosis. Lancet. 2011;378(9807):1949–61.
Raghu G, Chen SY, Hou Q, Yeh WS, Collard HR. Incidence and prevalence of idiopathic pulmonary fibrosis in US adults 18–64 years old. Eur Respir J. 2016;48(1):179–86.
Fernandez Perez ER, Daniels CE, Schroeder DR, St Sauver J, Hartman TE, Bartholmai BJ, Yi ES, Ryu JH. Incidence, prevalence, and clinical course of idiopathic pulmonary fibrosis: a population-based study. Chest. 2010;137(1):129–37.
Nalysnyk L, Cid-Ruzafa J, Rotella P, Esser D. Incidence and prevalence of idiopathic pulmonary fibrosis: review of the literature. Eur Respir Rev. 2012;21(126):355–61.
Lee HE, Myong JP, Kim HR, Rhee CK, Yoon HK, Koo JW. Incidence and prevalence of idiopathic interstitial pneumonia and idiopathic pulmonary fibrosis in Korea. Int J Tuberc Lung Dis. 2016;20(7):978–84.
Nathan SD, Shlobin OA, Weir N, Ahmad S, Kaldjob JM, Battle E, Sheridan MJ, du Bois RM. Long-term course and prognosis of idiopathic pulmonary fibrosis in the new millennium. Chest. 2011;140(1):221–9.
Strongman H, Kausar I, Maher TM. Incidence, prevalence, and survival of patients with idiopathic pulmonary fibrosis in the UK. Adv Ther. 2018;35(5):724–36.
Diamantopoulos A, Wright E, Vlahopoulou K, Cornic L, Schoof N, Maher TM. The burden of illness of idiopathic pulmonary fibrosis: a comprehensive evidence review. Pharmacoeconomics. 2018;36(7):779–807.
Kreuter M, Ehlers-Tenenbaum S, Palmowski K, Bruhwyler J, Oltmanns U, Muley T, Heussel CP, Warth A, Kolb M, Herth FJ. Impact of comorbidities on mortality in patients with idiopathic pulmonary fibrosis. PLoS ONE. 2016;11(3): e0151425.
Kreuter M, Swigris J, Pittrow D, Geier S, Klotsche J, Prasse A, Wirtz H, Koschel D, Andreas S, Claussen M, Grohe C, Wilkens H, Hagmeyer L, Skowasch D, Meyer JF, Kirschner J, Glaser S, Herth FJF, Welte T, Neurohr C, Schwaiblmair M, Held M, Bahmer T, Frankenberger M, Behr J. Health related quality of life in patients with idiopathic pulmonary fibrosis in clinical practice: insights-IPF registry. Respir Res. 2017;18(1):139.
King CS, Nathan SD. Idiopathic pulmonary fibrosis: effects and optimal management of comorbidities. Lancet Respir Med. 2017;5(1):72–84.
Raghu G, Amatto VC, Behr J, Stowasser S. Comorbidities in idiopathic pulmonary fibrosis patients: a systematic literature review. Eur Respir J. 2015;46(4):1113–30.
Duckworth A, Gibbons MA, Allen RJ, Almond H, Beaumont RN, Wood AR, Lunnon K, Lindsay MA, Wain LV, Tyrrell J, Scotton CJ. Telomere length and risk of idiopathic pulmonary fibrosis and chronic obstructive pulmonary disease: a Mendelian randomisation study. Lancet Respir Med. 2021;9(3):285–94.
Nathan SD, Basavaraj A, Reichner C, Shlobin OA, Ahmad S, Kiernan J, Burton N, Barnett SD. Prevalence and impact of coronary artery disease in idiopathic pulmonary fibrosis. Respir Med. 2010;104(7):1035–41.
Suzuki A, Kondoh Y. The clinical impact of major comorbidities on idiopathic pulmonary fibrosis. Respir Investig. 2017;55(2):94–103.
Guenther A, Krauss E, Tello S, Wagner J, Paul B, Kuhn S, Maurer O, Heinemann S, Costabel U, Barbero MAN, Muller V, Bonniaud P, Vancheri C, Wells A, Vasakova M, Pesci A, Sofia M, Klepetko W, Seeger W, Drakopanagiotakis F, Crestani B. The European IPF registry (eurIPFreg): baseline characteristics and survival of patients with idiopathic pulmonary fibrosis. RespirRes. 2018;19(1):141.
Oldham JM, Collard HR. Comorbid conditions in idiopathic pulmonary fibrosis: recognition and management. Front Med (Lausanne). 2017;4:123.
Karkkainen M, Kettunen HP, Nurmi H, Selander T, Purokivi M, Kaarteenaho R. Effect of smoking and comorbidities on survival in idiopathic pulmonary fibrosis. Respir Res. 2017;18(1):160.
Lancaster LH, Mason WR, Parnell JA, Rice TW, Loyd JE, Milstone AP, Collard HR, Malow BA. Obstructive sleep apnea is common in idiopathic pulmonary fibrosis. Chest. 2009;136(3):772–8.
Raghu G, Freudenberger TD, Yang S, Curtis JR, Spada C, Hayes J, Sillery JK, Pope 2nd CE, Pellegrini CA. High prevalence of abnormal acid gastro-oesophageal reflux in idiopathic pulmonary fibrosis. Eur Respir J. 2006;27(1):136–42.
Wuyts WA, Dahlqvist C, Slabbynck H, Schlesser M, Gusbin N, Compere C, Maddens S, Kirchgaessler KU, Bartley K, Bondue B. Baseline clinical characteristics, comorbidities and prescribed medication in a real-world population of patients with idiopathic pulmonary fibrosis: the PROOF registry. BMJ Open Respir Res. 2018;5(1): e000331.
Kato E, Takayanagi N, Takaku Y, Kagiyama N, Kanauchi T, Ishiguro T, Sugita Y. Incidence and predictive factors of lung cancer in patients with idiopathic pulmonary fibrosis. ERJ Open Res. 2018;4(1):00111–2016.
Torrisi SE, Ley B, Kreuter M, Wijsenbeek M, Vittinghoff E, Collard HR, Vancheri C. The added value of comorbidities in predicting survival in idiopathic pulmonary fibrosis: a multicentre observational study. Eur Respir J. 2019;53(3):1801587.
Nathan SD, Albera C, Bradford WZ, Costabel U, Glaspole I, Glassberg MK, Kardatzke DR, Daigl M, Kirchgaessler KU, Lancaster LH, Lederer DJ, Pereira CA, Swigris JJ, Valeyre D, Noble PW. Effect of pirfenidone on mortality: pooled analyses and meta-analyses of clinical trials in idiopathic pulmonary fibrosis. Lancet Respir Med. 2017;5(1):33–41.
Noble PW, Albera C, Bradford WZ, Costabel U, du Bois RM, Fagan EA, Fishman RS, Glaspole I, Glassberg MK, Lancaster L, Lederer DJ, Leff JA, Nathan SD, Pereira CA, Swigris JJ, Valeyre D, King TE Jr. Pirfenidone for idiopathic pulmonary fibrosis: analysis of pooled data from three multinational phase 3 trials. Eur Respir J. 2016;47(1):243–53.
Crestani B, Huggins JT, Kaye M, Costabel U, Glaspole I, Ogura T, Song JW, Stansen W, Quaresma M, Stowasser S, Kreuter M. Long-term safety and tolerability of nintedanib in patients with idiopathic pulmonary fibrosis: results from the open-label extension study, INPULSIS-ON. Lancet Respir Med. 2019;7(1):60–8.
Richeldi L, Kreuter M, Selman M, Crestani B, Kirsten AM, Wuyts WA, Xu Z, Bernois K, Stowasser S, Quaresma M, Costabel U. Long-term treatment of patients with idiopathic pulmonary fibrosis with nintedanib: results from the TOMORROW trial and its open-label extension. Thorax. 2018;73(6):581–3.
Gao J, Kalafatis D, Carlson L, Pesonen IHA, Li CX, Wheelock A, Magnusson JM, Skold CM. Baseline characteristics and survival of patients of idiopathic pulmonary fibrosis: a longitudinal analysis of the Swedish IPF Registry. Respir Res. 2021;22(1):40.
European MultiPartner IPF REgistry. 2019. http://empire.registry.cz/index-en.php. Accessed 15 Oct 2019.
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier JF, Flaherty KR, Lasky JA, Lynch DA, Ryu JH, Swigris JJ, Wells AU, Ancochea J, Bouros D, Carvalho C, Costabel U, Ebina M, Hansell DM, Johkoh T, Kim DS, King TE Jr, Kondoh Y, Myers J, Muller NL, Nicholson AG, Richeldi L, Selman M, Dudden RF, Griss BS, Protzko SL, Schunemann HJ, ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183(6):788–824.
Raghu G, Rochwerg B, Zhang Y, Garcia CA, Azuma A, Behr J, Brozek JL, Collard HR, Cunningham W, Homma S, Johkoh T, Martinez FJ, Myers J, Protzko SL, Richeldi L, Rind D, Selman M, Theodore A, Wells AU, Hoogsteden H, Schunemann HJ, American Thoracic Society, European Respiratory Society, Japanese Respiratory Society, Latin American Thoracic Association. An official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis. An update of the 2011 Clinical Practice Guideline. Am J Respir Crit Care Med. 2015: 192(2): e3–19.
Collard HR, Ward AJ, Lanes S, Cortney Hayflinger D, Rosenberg DM, Hunsche E. Burden of illness in idiopathic pulmonary fibrosis. J Med Econ. 2012;15(5):829–35.
Weiss CO, Boyd CM, Yu Q, Wolff JL, Leff B. Patterns of prevalent major chronic disease among older adults in the United States. JAMA. 2007;298(10):1160–2.
Sharif R, Zouk A, Kulkarni T, Acosta P, Luckhardt T, Thannickal V, de Andrade JA. The impact of comorbidities on idiopathic pulmonary fibrosis outcomes. Chest. 2016;150(4):471A.
Hyldgaard C, Hilberg O, Bendstrup E. How does comorbidity influence survival in idiopathic pulmonary fibrosis? Respir Med. 2014;108(4):647–53.
Behr J, Kreuter M, Hoeper MM, Wirtz H, Klotsche J, Koschel D, Andreas S, Claussen M, Grohe C, Wilkens H, Randerath W, Skowasch D, Meyer FJ, Kirschner J, Glaser S, Herth FJ, Welte T, Huber RM, Neurohr C, Schwaiblmair M, Kohlhaufl M, Hoffken G, Held M, Koch A, Bahmer T, Pittrow D. Management of patients with idiopathic pulmonary fibrosis in clinical practice: the INSIGHTS-IPF registry. Eur Respir J. 2015;46(1):186–96.
Cottin V, Koschel D, Günther A, Albera C, Azuma A, Sköld CM, Tomassetti S, Hormel P, Stauffer JL, Strombom I, Kirchgaessler KU, Maher TM. Long-term safety of pirfenidone: results of the prospective, observational PASSPORT study. ERJ Open Res. 2018;4(4):00084–2018.
Snyder LD, Mosher C, Holtze CH, Lancaster LH, Flaherty KR, Noth I, Neely ML, Hellkamp AS, Bender S, Conoscenti CS, de Andrade JA, Whelan TP. Time to diagnosis of idiopathic pulmonary fibrosis in the IPF-PRO Registry. BMJ Open Respir Res. 2020;7(1):e000567.
Jo HE, Glaspole I, Grainge C, Goh N, Hopkins PM, Moodley Y, Reynolds PN, Chapman S, Walters EH, Zappala C, Allan H, Keir GJ, Hayen A, Cooper WA, Mahar AM, Ellis S, Macansh S, Corte TJ. Baseline characteristics of idiopathic pulmonary fibrosis: analysis from the Australian Idiopathic Pulmonary Fibrosis Registry. Eur Respir J. 2017;49(2):1601592.
Mortimer K, Hartmann N, Chan C, Norman H, Wallace L, Enger C. Characterizing idiopathic pulmonary fibrosis patients using US Medicare-advantage health plan claims data. BMC Pulm Med. 2019;19(1):11.
Caminati A, Madotto F, Cesana G, Conti S, Harari S. Epidemiological studies in idiopathic pulmonary fibrosis: pitfalls in methodologies and data interpretation. Eur Respir Rev. 2015;24(137):436–44.
Butler SJ, Li LSK, Ellerton L, Gershon AS, Goldstein RS, Brooks D. Prevalence of comorbidities and impact on pulmonary rehabilitation outcomes. ERJ Open Res. 2019;5:00264-2019.
Szentes BL, Kreuter M, Bahmer T, Birring SS, Claussen M, Waelscher J, Leidl R, Schwarzkopf L. Quality of life assessment in interstitial lung diseases: a comparison of the disease-specific K-BILD with the generic EQ-5D-5L. Respir Res. 2018;19(1):101.
Schwarzkopf L, Witt S, Waelscher J, Polke M, Kreuter M. Associations between comorbidities, their treatment and survival in patients with interstitial lung diseases—a claims data analysis. Respir Res. 2018;19(1):73.
Caminati A, Lonati C, Cassandro R, Elia D, Pelosi G, Torre O, Zompatori M, Uslenghi E, Harari S. Comorbidities in idiopathic pulmonary fibrosis: an underestimated issue. Eur Respir Rev. 2019;28:190044.
Torrisi SE, Vancheri A, Pavone M, Sambataro G, Palmucci S, Vancheri C. Comorbidities of IPF: how do they impact on prognosis. Pulm Pharmacol Ther. 2018;53:6–11.
Koo HJ, Do KH, Lee JB, Alblushi S, Lee SM. Lung cancer in combined pulmonary fibrosis and emphysema: a systematic review and meta-analysis. PLoS ONE. 2016;11(9): e0161437.
Lettieri CJ, Nathan SD, Barnett SD, Ahmad S, Shorr AF. Prevalence and outcomes of pulmonary arterial hypertension in advanced idiopathic pulmonary fibrosis. Chest. 2006;129(3):746–52.
Caminati A, Cassandro R, Harari S. Pulmonary hypertension in chronic interstitial lung diseases. Eur Respir Rev. 2013;22(129):292–301.
Leuschner G, Klotsche J, Kreuter M, Prasse A, Wirtz H, Pittrow D, Frankenberger M, Behr J, Kneidinger N. Idiopathic pulmonary fibrosis in elderly patients: analysis of the INSIGHTS-IPF observational study. Front Med (Lausanne). 2020;7: 601279.
Acknowledgements
The authors would like to thank Mordechai R Kramer, Natalia Stoeva, and Biserka Jovkovska-Kjaeva for their contributions to the data presented in this manuscript. The authors would also like to thank the EMPIRE registry patients, and the following study investigators for their invaluable participation: Austria: Stefan Zembacher, Michael Studnicka (Clinical Research Center Salzburg GmbH); David Lang, Bernd Lamprecht (Kepler University Hospital, Linz); Bulgaria: Natalia Stoeva (Acibadem City Clinic Tokuda Hospital, Sofia); Croatia: Suzana Mladinov, Dino Ilak (Split University Hospital Center); Mirna Vergles, Neven Tudorić, Jasna Tekavec-Trkanjec (University Hospital Dubrava, Zagreb); Czech Republic: Martina Vašáková, Martina Šterclová (Thomayer Hospital, Prague); Jiří Homolka (General University Hospital in Prague); Ladislav Lacina (Hospital Na Bulovce, Prague); Pavlína Lisá (University Hospital in Motol, Prague); Radka Bittenglová (University Hospital Plzeň); Vladimír Bartoš (University Hospital Hradec Králové); Renata Králová (Hospital Pardubice); Vladimíra Lošťáková, Monika Žurková (University Hospital Olomouc); Jana Pšíkalová (Hospital Kroměříž); Ilona Binková, Martina Doubková (University Hospital Brno); Jan Kervitzer (Hospital Znojmo); Tomáš Snížek (Hospital Jihlava); Pavel Reiterer (Masaryk Hospital in Ústí nad Labem); Hana Šuldová (Hospital České Budějovice); Martina Plačková (University Hospital Ostrava); Richard Tyl (Hospital Nový Jičín); Vladimír Řihák (Tomáš Baťa Regional Hospital, Zlín); Ladislav Dušek, Karel Hejduk, Jakub Gregor, Ondřej Májek, Simona Littnerová, Michal Svoboda (Institute of Biostatistics and Analyses, Faculty of Medicine, Masaryk University, Brno); Hungary: Miklós Zsiray (National Korányi Tuberculosis and Pulmonology Institute, Budapest); Veronika Müller, Anikó Bohács (Semmelweis University, Budapest); Maria Szilasi (Debrecen University Clinical Centre); Zsuzsanna Szalai (Petz Aladár County Teaching Hospital, Győr); Zoltán Balikó (Pécs University); Attila Somfay, Imre Lajkó (University of Szeged); Israel: Mordechai Kramer (Clalit Health Services through the Rabin Medical Centre, Petah Tikva); Yochai Adir (Carmel Medical Center, Haifa); North Macedonia: Biserka Jovkovska Kjaeva (Clinic of Pulmonology and Allergology, Skopje); Poland: Ewa Jassem, Alicja Sieminska, Amelia Szymanowska-Narloch (University Hospital Gdańsk); Adam Barczyk (Medical University of Silesia, Katowice); Krzysztof Sladek, Aleksander Kania, Lukasz Kasper, Tomasz Stachura, Paulina Jurek (Jagiellonian University, Kraków); Sebastian Majewski (Medical University of Łódź); Agata Nowicka, Lukasz Borucki (Poznań University of Medical Sciences); Katarzyna Lewandowska, Małgorzata Sobiecka, Beate Zolnowska, Pawel Sliwinski, Damian Korzybski, Magdalena Martusewicz-Boros, Elzbieta Wiatr (Institute of Tuberculosis and Lung Diseases, Warsaw); Marta Maskey-Warzęchowska, Katarzyna Górska, Małgorzata Barnaś (Medical University of Warsaw); Serbia: Violeta Vučinić-Mihailović, Branislava Milenković, Milica Kontić, Natalija Samardžić, Marina Roksandić, Dragana Jovanovic (School of Medicine Belgrade, Clinical Centre of Serbia, Belgrade); Tatjana Pejcic, Desa Nastasijevic Boravac, Emilija Videnovic, Tatjana Radjenovic Petkovic, Ivanka Djordejevic (Clinical Centre of Niš); Svetlana Kašiković Lečić, Vesna Kuruc, Živka Eri, Milana Panjković, Aleksandra Lovrenski, Darinka Kukavica, Ana Jakić (Institute for Pulmonary Diseases of Vojvodina, Sremska Kamenica); Slavica Mojsilovic (Clinical Centre Kragujevac); Slovakia: Marta Hájková, Štefan Laššán (University Hospital Bratislava); Štefan Tóth (L. Pasteur University Hospital Košice); Ján Plutinský (ZAPA JJ Ltd., Levice); Róbert Vyšehradský (University Hospital Martin); Bohumil Matula (St. Svorad’s Specialised Hospital Zobor, Nitra); Róbert Slivka, Imrich Jonner (National Institute of Tuberculosis, Lung Disorders and Thoracic Surgery Vyšné Hagy); Turkey: Nesrin Mogulkoc (Ege University Medical School, Izmir).
Consortium members: Dr. Stefan Zembacher1, Prim. Univ.-Prof. Dr. Michael Studnicka1, David Lang, MD2, Prof. Bernd Lamprecht, MD2, Anton Penev, MD3, Suzana Mladinov, MD4, Dino Ilak, MD4, Mirna Vergles, MD5, Prof. Neven Tudorić, MD, PhD5, Jasna Tekavec-Trkanjec, MD, PhD5, Prof. Martina Vašáková, MD, PhD6, Martina Šterclová, MD, PhD6, Ladislav Lacina, MD7, Pavlína Lisá, MD8, Radka Bittenglová, MD9, Vladimír Bartoš, MD10, Renata Králová, MD11, Vladimíra Lošťáková, MD, PhD12, Monika Žurková, MD12, Jana Pšíkalová, MD13, Ilona Binková, MD14, Martina Doubková, MD14, Jan Kervitzer, MD15, Tomáš Snížek, MD16, Pavel Reiterer, MD17, Hana Šuldová, MD18, Martina Plačková, MD19, Richard Tyl, MD20, Vladimír Řihák, MD21, Dr. Miklós Zsiray, MD22, Prof. Veronika Müller, MD, PhD23, Dr. Anikó Bohács MD, PhD23, Prof. Maria Szilasi MD, PhD24, Dr. Zsuzsanna Szalai, MD25, Dr. Zoltán Balikó, MD, habil. PhD26, Prof. Attila Somfay, MD, PhD27, Imre Lajkó, MD27, Prof. Mordechai Kramer, MD28, Prof. Yochai Adir29, Zoran Arsovski, MD30, Ewa Jassem, MD, PhD31, Alicja Sieminska, MD31, Amelia Szymanowska-Narloch, MD31, Prof. Adam Barczyk, MD, PhD32, Prof. Krzysztof Sladek, MD, PhD33, Aleksander Kania, MD, PhD33, Lukasz Kasper, MD, PhD33, Tomasz Stachura, MD33, Paulina Jurek, MD33, Sebastian Majewski, MD34, Lukasz Borucki, MD, PhD35, Agata Nowicka, MD, PhD35, Katarzyna Lewandowska, MD36, Małgorzata Sobiecka, MD36, Beata Zolnowska, MD36, Prof. Pawel Sliwinski, MD36, Damian Korzybski, MD36, Magdalena Martusewicz-Boros, MD36, Prof. Elzbieta Wiatr, MD, PhD36, Dr n. med. Marta Maskey-Warzęchowska37, Katarzyna Górska MD, PhD37, Małgorzata Barnaś MD, PhD37, Prof. Violeta Vučinić-Mihailović, MD, PhD38, Prof. Branislava Milenković, MD, PhD38, Assist. Prof. Milica Kontić, MD, PhD38, Prim. Natalija Samardžić, MD, PhD38, Assist. Prof. Marina Roksandić, MD38, Assist. Prof. Sanja Dimic Janjic, MD, PhD38, Prof. Tatjana Pejcic, MD39, Desa Nastasijevic Boravac, MD, PhD39, Emilija Videnovic, MD39, Tatjana Radjenovic Petkovic, MD, PhD39, Ivanka Djordejevic, MD, PhD39, Prof. Svetlana Kašiković Lečić, MD, PhD40, Prof. Vesna Kuruc, MD, PhD40, Prof. Živka Eri, MD, PhD40, Prof. Milana Panjković, MD, PhD40, Assist Prof. Aleksandra Lovrenski, MD, PhD40, Darinka Kukavica, MD, PhD40, Ana Jakić, MD40, Slavica Mojsilovic, MD41, Assoc. Prof. Marta Hájková, MD, PhD, MPH, MUDr.42, Štefan Laššán, PhD42, Štefan Tóth, MD43, Assoc. Prof. Ján Plutinský, MD, PhD44, Assoc. Prof. Róbert Vyšehradský, MD, PhD45, Bohumil Matula, MD46, Róbert Slivka, MD, PhD47, Imrich Jonner, MD47, Peter Paluch, MD48, Prof. Nesrin Mogulkoc, MD49
1Clinical Research Center Salzburg GmbH, Salzburg, Austria; 2Kepler University Hospital, Linz, Austria; 3Acibadem City Clinic Tokuda Hospital, Sofia, Bulgaria; 4Split University Hospital Center, Split, Croatia; 5University Hospital Dubrava, Zagreb, Croatia; 6Thomayer University Hospital, Prague, Czechia; 7Hospital Na Bulovce, Prague, Czechia; 8University Hospital Motol, Prague, Czechia; 9University Hospital Plzeň, Plzeň, Czechia; 10University Hospital Hradec Králové, Hradec Králové, Czechia; 11Regional Hospital Pardubice, Pardubice, Czechia; 12University Hospital Olomouc, Olomouc, Czechia; 13Hospital Kroměříž, Kroměříž, Czechia; 14University Hospital Brno, Brno, Czechia; 15Hospital Znojmo, Znojmo, Czechia; 16Hospital Jihlava, Jihlava, Czechia; 17Masaryk Hospital, Ústi nad Labem, Czechia; 18Hospital České Budějovice, České Budějovice, Czechia; 19University Hospital Ostrava, Ostrava, Czechia; 20Hospital Nový Jičín, Nový Jičín, Czechia; 21Tomáš Baťa Regional Hospital, Zlín, Czechia; 22National Korányi Tuberculosis and Pulmonology Institute, Budapest, Hungary; 23Semmelweis University, Budapest, Hungary; 24Debrecen University Clinical Centre, Debrecen, Hungary; 25Petz Aladár County Teaching Hospital, Győr, Hungary; 26Pécs University, Pécs, Hungary; 27University of Szeged, Szeged, Hungary; 28Clalit Health Services through the Rabin Medical Centre, Petah Tikva, Israel; 29Carmel Medical Center, Haifa, Israel; 30Clinic of Pulmonology and Allergology, Skopje, North Macedonia; 31University Hospital Gdańsk, Gdańsk, Poland; 32Medical University of Silesia, Katowice, Poland; 33Jagiellonian University, Kraków, Poland; 34Medical University of Łódź, Łódź, Poland; 35Poznan University of Medical Sciences, Poznań, Poland; 36Institute of Tuberculosis and Lung Diseases, Warsaw, Poland; 37Medical University of Warsaw, Warsaw, Poland; 38Clinical Centre of Serbia, Belgrade, Serbia; 39Clinical Centre of Niš, Niš, Serbia; 40Institute for Pulmonary Diseases of Vojvodina, Sremska Kamenica, Serbia; 41Clinical Centre Kragujevac, Kragujevac, Serbia; 42University Hospital Bratislava, Bratislava, Slovakia; 43LPasteur University Hospital Košice, Košice, Slovakia; 44ZAPA JJ Ltd., Levice, Slovakia; 45University Hospital Martin, Martin, Slovakia; 46St. Svorad’s Specialised Hospital Zobor, Nitra, Slovakia; 47National Institute of Tuberculosis, Lung Disorders and Thoracic Surgery, Vyšné Hagy, Slovakia; 48F. D. Roosevelt University Hospital, Banská Bystrica, Slovakia; 49Ege University Medical School, Izmir, Turkey
Funding
The EMPIRE registry is supported in part by Boehringer Ingelheim and Roche. The authors did not receive payment for the development of the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
DMJ: study proposal, literature analysis, critical review of statistical evaluation, writing, critical review and editing, approval of final draft. MŠ, NM, KL, VM, MH, MS, JTT: approval of study proposal, patient enrolment, critical review and editing. SL: critical review of statistical analysis and results, critical review and editing, approval of final draft. MV: founder and scientific leader of the EMPIRE registry, approval of study proposal, critical review of statistical analysis and results, critical review and editing, approval of final draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. The study protocol and its amendments were approved by the Ethics Committee of each participating institution. Owing to the partially retrospective nature of the study, written informed consent could not be obtained from each patient due to objective reasons, e.g., following preliminary oral consent some patients may have died or been too ill to travel to a follow-up appointment to provide written consent. Nevertheless, all records in the EMPIRE registry are fully anonymised and de-identified.
Consent for publication
Not applicable.
Competing interests
The authors meet criteria for authorship as recommended by the International Committee of Medical Journal Editors (ICMJE). This study was supported by Boehringer Ingelheim International GmbH (BI). BI had no role in the design, analysis or interpretation of the results in this study. BI was given the opportunity to review the manuscript for medical and scientific accuracy as it relates to BI substances, as well as intellectual property considerations. Writing/editorial support and formatting assistance was provided by Helen Keyworth, PhD, of Nucleus Global, which was contracted and funded by BI. DMJ reports personal fees from Boehringer Ingelheim and Roche outside the submitted work; and advisory board participation for Boehringer Ingelheim and Roche. NM reports consulting fees paid to their institution for advisory board participation or consultancy from Boehringer Ingelheim, Roche, Bayer and Novartis Turkey; speaker honoraria paid to their institution from Boehringer Ingelheim, Roche and Nobel; and support for congress participation from Roche, Actelion and Boehringer Ingelheim. KL reports grants, consulting fees, honoraria, support for congress participation and personal fees from Roche and Boehringer Ingelheim; and is the vice-president of the Polis IPF Patients Society. VM reports personal fees from Boehringer Ingelheim and Roche outside the submitted work; and travel grants from Boehringer Ingelheim and Roche. JTT reports personal lecture fees from Roche and Boehringer Ingelheim; and advisory board participation for Boehringer Ingelheim. MV reports personal fees or honoraria for lectures or presentations from Boehringer Ingelheim and Roche; support for conference attendance from Boehringer Ingelheim and Roche; advisory board participation for Boehringer Ingelheim; is the president of the Czech Pneumologic and Phtisiologic Society; and is the head of the EMPIRE registry. MŠ, MH, MS and SL have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Duration of antifibrotic therapies. Table S2. Survival of patients with IPF by number of comorbidities. Table S3. Survival of patients with IPF by number of comorbidities according to antifibrotic therapy. Figure S1. Comorbidities by body system in participating EMPIRE countries. Figure S2. Cardiovascular comorbidities in participating EMPIRE countries. Figure S3. Metabolic and gastrointestinal comorbidities in participating EMPIRE countries. Figure S4. Pulmonary comorbidities in participating EMPIRE countries. Figure S5. Urogenital comorbidities in participating EMPIRE countries. Figure S6. Blood and immunity disorders in participating EMPIRE countries. Figure S7. Other comorbidities in participating EMPIRE countries. Figure S8. Comorbidities in patients with IPF in EMPIRE compared other real-world registries and clinical trials.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jovanovic, D.M., Šterclová, M., Mogulkoc, N. et al. Comorbidity burden and survival in patients with idiopathic pulmonary fibrosis: the EMPIRE registry study. Respir Res 23, 135 (2022). https://doi.org/10.1186/s12931-022-02033-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-022-02033-6