Abstract
Background
Colorectal cancer is the third most common cancer in the world. In this study, we assessed the long-term survival characteristics and prognostic associations and potential time-varying effects of clinico-demographic variables and two molecular markers (microsatellite instability (MSI) and BRAF Val600Glu mutation) in a population-based patient cohort followed up to ~ 19 years.
Methods
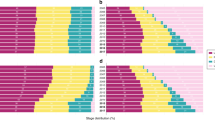
The patient cohort included 738 incident cases diagnosed between 1999 and 2003. Cox models were used to analyze the association between the variables and a set of survival outcome measures (overall survival (OS), disease-specific survival (DSS), recurrence-free survival (RFS), metastasis-free survival (MFS), recurrence/metastasis-free survival (RMFS), and event-free survival (EFS)). Cox proportional hazard (PH) assumption was tested for all variables, and Cox models with time-varying effects were used if any departure from the PH assumption was detected.
Results
During the follow-up, ~ 61% patients died from any cause, ~ 26% died from colorectal cancer, and ~ 10% and ~ 20% experienced recurrences and distant metastases, respectively. Stage IV disease and post-diagnostic recurrence or metastasis were strongly linked to risk of death from colorectal cancer. If a patient had survived the first 6 years without any disease-related event (i.e., recurrence, metastasis, or death from colorectal cancer), their risks became very minimal after this time period. Distinct sets of markers were associated with different outcome measures. In some cases, the effects by variables were constant throughout the follow-up. For example, MSI-high tumor phenotype and older age at diagnosis predicted longer MFS times consistently over the follow-up. However, in some other cases, the effects of the variables varied with time. For example, adjuvant radiotherapy treatment was associated with increased risk of metastasis in patients who received this treatment after 5.5 years post-diagnosis, but not before that.
Conclusions
This study describes the long-term survival characteristics of a prospective cohort of colorectal cancer patients, relationships between baseline variables and a detailed set of patient outcomes over a long time, and time-varying effects of a group of variables. The results presented advance our understanding of the long-term prognostic characteristics in colorectal cancer and are expected to inspire future studies and clinical care strategies.
Similar content being viewed by others
Background
Colorectal cancer is an important disease to control. It is one of the most commonly diagnosed cancers in the world, causing ~ 700,000 deaths each year [1]. Many patients with colorectal cancer also experience clinically important events, such as recurrences or metastases after diagnosis. Assessing the characteristics of potential disease outcomes and identifying their predictors are critical for effective patient surveillance, and to treat and control this disease in both the short term and long term. Studies have reported that the majority of the recurrences, metastases, and deaths from colorectal cancer occur within the first few years following the diagnosis or surgery [2, 3]. The main clinical surveillance guidelines recommend up to 5 years of follow-up [4].
Clinical features (e.g., disease stage, tumor grade, histology, location), demographic variables (e.g., age at diagnosis, sex, and familial risk status), and tumor characteristics (e.g., the MSI tumor phenotype and somatic mutations, including BRAF Val600Glu mutation) are among the most commonly investigated variables in colorectal cancer [5,6,7,8,9,10]. Familial risk status may indicate familial clustering of the disease and is an interest for both the susceptibility and prognostic studies [10, 11]. Microsatellite instability (MSI) is a tumor phenotype that is characterized by defects in the DNA mismatch repair system that leads to genomic instability [12]. Generally, MSI-high tumors are associated with better patient survival [7]. BRAF Val600Glu mutation occurs in ~ 10% of the colorectal tumors, causes oncogenic BRAF activity, and promotes cellular transformation [9]. Literature reports also suggest a prognostic role for this BRAF mutation in colorectal cancer [13].
Many prognostic studies aim to identify the markers to help distinguish the patients with different outcome risks. Potential time-varying effects of markers on the patient outcomes, however, are not well-studied. Markers with time-varying effects are those whose effect direction (e.g., protective or detrimental) or size (i.e., magnitude) changes over the follow-up [14,15,16,17,18]. There are at least two important implications of assessing the time-varying effects of the markers in prognostic studies. First, such markers are important as they can distinguish the patients who are at increased risk of events only during specific time periods (e.g., in the short term [early event markers] or the long term [late event markers or markers with late effects]). Second, examining the time-varying effects of variables is not a standard or widely utilized research practice, which potentially leads to loss of information or inaccurate inference [14, 19, 20].
In colorectal cancer, a few studies examined the clinical, demographic, or molecular variables for time-varying effects using statistical methods. For example, disease location [21]; age, disease stage, time period of diagnosis, or tumor site [15, 16, 18]; regional cancer, age, and tumor location (pelvic/sigmoid colon) [22]; age (in two of our previous studies using subsets of the patients included in this study) [23, 24]; tumor site (left or right), grade, sex, and stage [69,70,71]. As these authors discussed [69,70,71], a variety of potential mechanisms can explain this effect, such as the appearance or development of radiation-resistant tumor cells, changes in the tumor microenvironment or immune system response over time, or suppression of the tumor progression by radiation treatment that initially delays the tumor metastasis. These previous and our findings emphasize the need for new research revenues and potentially prolonged surveillance for late-onset metastatic lesions in colorectal cancer patients who are treated with adjuvant radiotherapy.
Strengths and limitations
Limitations of this study include the missing information on the cause of death for a portion of the patients; assuming that the non-colorectal cancer-related deaths were independent of colorectal cancer; having a small number of recurrences in the dataset, which may have limited the study power in analysis of recurrence-related outcomes; and examining select clinico-demographic and tumor molecular markers, which leaves it to future studies to examine the potential effects of other markers. Additionally, characteristics of the patients who are included in this study may differ from the patients who were diagnosed during the recruitment phase, but declined to consent and participate in NFCCR. This may affect the generalizability of the findings. However, it should also be noted that in some cases, the consent to access the medical records and tissue specimen was obtained from the close relatives/proxies of the patients who had died. Thus, the bias that may be introduced by the exclusion of advanced stage patients is expected to be lower in our study compared to many other studies [35]. This study also has a number of unique advantages: the cohort examined in this study is one of the longest followed up cohorts that allowed the systematic examination of long-term survival characteristics in colorectal cancer; this is a prospective cohort study that reduces information bias compared to retrospective cohort studies [72]; a comprehensive set of outcome measures were examined, which provided detailed information on survival patterns and relationships; and finally, the PH assumption in Cox regression models was checked, and the effects of variables were properly assessed—this not only increased the reliability of the effect estimations, but also allowed us to identify promising early and late effect markers.
Conclusions
In conclusion, this study describes the long-term survival characteristics of a prospective cohort of colorectal cancer patients and the detailed relationships between baseline variables and patient outcomes over a long time. Overall, our results increase the depth of information on patient outcomes and the markers of short-term and long-term risks and provide new insights that may assist future research and clinical care strategies in colorectal cancer.
Availability of data and materials
Data that support the findings of this study are available from Newfoundland Colorectal Cancer Registry/Memorial University but restrictions apply to the availability of this data, and so data are not publically available. The data used in this study cannot be made publicly available as patients were not consented to make their data publicly available or accessible. Data are available from the Newfoundland Colorectal Cancer Registry (NFCCR) for researchers who meet the criteria for access to confidential data. Permission to obtain the data can be requested from Newfoundland Colorectal Cancer Registry (Dr. Patrick Parfrey; pparfrey@mun.ca) and Research, Grant, and Contract Services (rgcs@mun.ca) at Memorial University of Newfoundland, St. John’s, NL, Canada, and the ethics approval shall be obtained from the Health Research Ethics Board (HREB), Ethics Office, Health Research Ethics Authority, Suite 200, 95 Bonaventure Avenue, St. John’s, NL, A1B 2X5, Canada.
Abbreviations
- CI:
-
Confidence interval
- DSS:
-
Disease-specific survival
- EFS:
-
Event-free survival
- HR:
-
Hazard ratio
- MFS:
-
Metastasis-free survival
- MSI:
-
Microsatellite instability
- MSI-H:
-
Microsatellite instability-high
- MSI-L:
-
Microsatellite instability-low
- MSS:
-
Microsatellite stable
- OS:
-
Overall survival
- PH:
-
Proportional hazard
- RFS:
-
Recurrence-free survival
- RMFS:
-
Recurrence/metastasis-free survival
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108.
Sargent D, Sobrero A, Grothey A, O’Connell MJ, Buyse M, Andre T, et al. Evidence for cure by adjuvant therapy in colon cancer: observations based on individual patient data from 20,898 patients on 18 randomized trials. J Clin Oncol. 2009;27(6):872–7.
Ryuk JP, Choi G, Park JS, Kim HJ, Park SY, Yoon GS, et al. Predictive factors and the prognosis of recurrence of colorectal cancer within 2 years after curative resection. Ann Surg Treat Res. 2014;86(3):143–51.
van Der Stok EP, Spaander MCW, Grünhagen DJ, Verhoef C, Kuipers EJ. Surveillance after curative treatment for colorectal cancer. Nat Rev Clin Oncol. 2017;14(5):297–315.
Compton CC, Fielding LP, Burgart LJ, Conley B, Cooper HS, Hamilton SR, et al. Prognostic factors in colorectal cancer: College of American Pathologists consensus statement 1999. Arch Pathol Lab Med. 2000;124(7):979–94.
Marzouk O, Schofield J. Review of histopathological and molecular prognostic features in colorectal cancer. Cancers (Basel). 2011;3(2):2767–810.
Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol. 2005;23(3):609–18.
Zlobec I, Lugli A. Prognostic and predictive factors in colorectal cancer. Postgrad Med J. 2008;84(994):403–11.
Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949–54.
Phipps AI, Ahnen DJ, Campbell PT, Win AK, Jenkins MA, Lindor NM, et al. Family history of colorectal cancer is not associated with colorectal cancer survival regardless of microsatellite instability status. Cancer Epidemiol Biomark Prev. 2014;23(8):1700–4.
Johns LE, Houlston RS. A systematic review and meta-analysis of familial colorectal cancer risk. Am J Gastroenterol. 2001;96(10):2992–3003.
Karran P. Microsatellite instability and DNA mismatch repair in human cancer. Semin Cancer Biol. 1996;7(1):15–24.
Ardekani GS, Jafarnejad SM, Tan L, Saeedi A, Li G. The prognostic value of BRAF mutation in colorectal cancer and melanoma: a systematic review and meta-analysis. PLoS One. 2012;7(10):e47054.
Bellera CA, MacGrogan G, Debled M, de Lara CT, Brouste V, Mathoulin-Pélissier S. Variables with time-varying effects and the Cox model: some statistical concepts illustrated with a prognostic factor study in breast cancer. BMC Med Res Methodol. 2010;10:20.
Bolard P, Quantin C, Esteve J, Faivre J, Abrahamowicz M. Modelling time-dependent hazard ratios in relative survival: application to colon cancer. J Clin Epidemiol. 2001;54(10):986–96.
Giorgi R, Abrahamowicz M, Quantin C, Bolard P, Esteve J, Gouvernet J, et al. A relative survival regression model using B-spline functions to model non-proportional hazards. Stat Med. 2003;22(17):2767–84.
Natarajan L, Pu M, Parker BA, Thomson CA, Caan BJ, Flatt SW, et al. Time-varying effects of prognostic factors associated with disease-free survival in breast cancer. Am J Epidemiol. 2009;169(12):1463–70.
Quantin C, Abrahamowicz M, Moreau T, Bartlett G, MacKenzie T, Tazi MA, et al. Variation over time of the effects of prognostic factors in a population-based study of colon cancer: comparison of statistical models. Am J Epidemiol. 1999;150(11):1188–200.
Altman D, De Stavola B, Love SB, Stepniewska KA. Review of survival analyses published in cancer journals. Br J Cancer. 1995;72(2):511–8.
Sigounas DE, Tatsioni A, Christodoulou DK, Tsianos EV, Ioannidis JP. New prognostic markers for outcome of acute pancreatitis: overview of reporting in 184 studies. Pancreas. 2011;40(4):522–32.
Roncucci L, Fante R, Losi L, Di Gregorio C, Micheli A, Benatti P, et al. Survival for colon and rectal cancer in a population-based cancer registry. Eur J Cancer. 1996;32A(2):295–302.
Zahl PH. Regression analysis with multiplicative and time-varying additive regression coefficients with examples from breast and colon cancer. Stat Med. 2003;22(7):1113–27.
Werdyani S, Yu Y, Skardasi G, Xu J, Shestopaloff K, Xu W, et al. Germline INDELs and CNVs in a cohort of colorectal cancer patients: their characteristics, associations with relapse-free survival time, and potential time-varying effects on the risk of relapse. Cancer Med. 2017;6(6):1220–32.
Yu Y, Cheng D, Parfrey P, Liu G, Savas S. Two functional indel polymorphisms in the promoter region of the Brahma gene (BRM) and disease risk and progression-free survival in colorectal cancer. PLoS One. 2018;13(6):e0198873.
Liu M, Li L, Yu W, Chen J, **ong W, Chen S, et al. Marriage is a dependent risk factor for mortality of colon adenocarcinoma without a time-varying effect. Oncotarget. 2017;8(12):20056–66.
Penney ME, Parfrey PS, Savas S, Yilmaz YE. A genome-wide association study identifies single nucleotide polymorphisms associated with time-to-metastasis in colorectal cancer. BMC Cancer. 2019;19(1):133.
Pavelitz T, Renfro L, Foster NR, Caracol A, Welsch P, Lao VV, et al. MRE11-deficiency associated with improved long-term disease free survival and overall survival in a subset of stage III colon cancer patients in randomized CALGB 89803 trial. PLoS One. 2014;9(10):e108483.
Farewell VT. The use of mixture models for the analysis of survival data with long-term survivors. Biometrics. 1982;38(4):1041–6.
Klein JP, Moeschberger ML. Survival analysis: techniques for censored and truncated data. 2nd ed. New York: Springer; 2003. p. 295–328.
Cortese G, Scheike TH, Martinussen T. Flexible survival regression modelling. Stat Methods Med Res. 2010;19(1):5–28.
Cox DR, Oakes D. Analysis of survival data. London: Chapman and Hall; 1984.
Cox DR. Regression models and life-tables. J R Stat Soc Series B Stat Methodol. 1972;34(2):187–220.
Kleinbaum DG, Klein M. Survival analysis: a self-learning text. 3rd ed. New York: Springer; 2001.
Green RC, Green JS, Buehler SK, Robb JD, Daftary D, Gallinger S, et al. Very high incidence of familial colorectal cancer in Newfoundland: a comparison with Ontario and 13 other population-based studies. Familial Cancer. 2007;6(1):53–62.
Woods MO, Younghusband HB, Parfrey PS, Gallinger S, McLaughlin J, Dicks E, et al. The genetic basis of colorectal cancer in a population-based incident cohort with a high rate of familial disease. Gut. 2010;59(10):1369–77.
Negandhi AA, Hyde A, Dicks E, Pollett W, Younghusband BH, Parfrey P, et al. MTHFR Glu429Ala and ERCC5 His46His polymorphisms are associated with prognosis in colorectal cancer patients: analysis of two independent cohorts from Newfoundland. PLoS One. 2013;8(4):e61469.
Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81(3):515–26.
Therneau TM. A package for survival analysis in S. version 2.38. 2015. Available at: https://CRAN.R-project.org/package=survival. Accessed Mar 12 2019.
R Development Core Team. R: a language and environment for statistical computing. Vienna; 2018. Available at: https://www.R-project.org/. Accessed May 28 2019
Bouvier AM, Launoy G, Bouvier V, Rollot F, Manfredi S, Faivre J, et al. Incidence and patterns of late recurrences in colon cancer patients. Int J Cancer. 2015;137(9):2133–8.
Broadbridge VT, Karapetis CS, Beeke C, Woodman RJ, Padbury R, Maddern G, et al. Do metastatic colorectal cancer patients who present with late relapse after curative surgery have a better survival? Br J Cancer. 2013;109(5):1338–43.
Berian JR, Benson AB III, Nelson H. Young age and aggressive treatment in colon cancer. JAMA. 2015;314(6):613–4.
Law JH, Koh FH, Tan KK. Young colorectal cancer patients often present too late. Int J Color Dis. 2017;32(8):1165–9.
McArdle CS, McMillan DC, Hole DJ. Male gender adversely affects survival following surgery for colorectal cancer. Br J Surg. 2003;90(6):711–5.
Wichmann MW, Müller C, Hornung HM, Lau-Werner U, Schildberg FW, Colorectal Cancer Study Group. Gender differences in long-term survival of patients with colorectal cancer. Br J Surg. 2001;88(8):1092–8.
Yang Y, Wang G, He J, Ren S, Wu F, Zhang J, et al. Gender differences in colorectal cancer survival: a meta-analysis. Int J Cancer. 2017;141(10):1942–9.
Wang WS, Lin JK, Chiou TJ, Liu JH, Fan FS, Yen CC, et al. Preoperative carcinoembryonic antigen level as an independent prognostic factor in colorectal cancer: Taiwan experience. Jpn J Clin Oncol. 2000;30(1):12–6.
Bertario L, Russo A, Sala P, Eboli M, Radice P, Presciuttini S, et al. Survival of patients with hereditary colorectal cancer: comparison of HNPCC and colorectal cancer in FAP patients with sporadic colorectal cancer. Int J Cancer. 1999;80(2):183–7.
Butterworth AS, Higgins JP, Pharoah P. Relative and absolute risk of colorectal cancer for individuals with a family history: a meta-analysis. Eur J Cancer. 2006;42(2):216–27.
Malesci A, Laghi L, Bianchi P, Delconte G, Randolph A, Torri V, et al. Reduced likelihood of metastases in patients with microsatellite-unstable colorectal cancer. Clin Cancer Res. 2007;13(13):3831–9.
Buckowitz A, Knaebel HP, Benner A, Bläker H, Gebert J, Kienle P, et al. Microsatellite instability in colorectal cancer is associated with local lymphocyte infiltration and low frequency of distant metastases. Br J Cancer. 2005;92(9):1746–53.
Mayo SC, Shore AD, Nathan H, Edil BH, Hirose K, Anders RA, et al. Refining the definition of perioperative mortality following hepatectomy using death within 90 days as the standard criterion. HPB (Oxford). 2011;13(7):473–82.
Rutegård M, Haapamäki M, Matthiessen P, Rutegård J. Early postoperative mortality after surgery for rectal cancer in Sweden, 2000–2011. Color Dis. 2014;16(6):426–32.
van Eeghen EE, den Boer FC, Loffeld RJ. Thirty days post-operative mortality after surgery for colorectal cancer: a descriptive study. J Gastrointest Oncol. 2015;6(6):613–7.
Obrand DI, Gordon PH. Incidence and patterns of recurrence following curative resection for colorectal carcinoma. Dis Colon Rectum. 1997;40(1):15–24.
Pugh SA, Shinkins B, Fuller A, Mellor J, Mant D, Primrose JN. Site and stage of colorectal cancer influence the likelihood and distribution of disease recurrence and postrecurrence survival: data from the FACS randomized controlled trial. Ann Surg. 2016;263(6):1143–7.
Singer G, Oldt R III, Cohen Y, Wang BG, Sidransky D, Kurman RJ, et al. Mutations in BRAF and KRAS characterize the development of low-grade ovarian serous carcinoma. J Natl Cancer Inst. 2003;95(6):484–6.
**ng M, Alzahrani AS, Carson KA, Shong YK, Kim TY, Viola D, et al. Association between BRAF V600E mutation and recurrence of papillary thyroid cancer. J Clin Oncol. 2015;33(1):42–50.
Sánchez-Torres JM, Viteri S, Molina MA, Rosell R. BRAF mutant non-small cell lung cancer and treatment with BRAF inhibitors. Transl Lung Cancer Res. 2013;2(3):244–50.
Huang D, Sun W, Zhou Y, Li P, Chen F, Chen H, et al. Mutations of key driver genes in colorectal cancer progression and metastasis. Cancer Metastasis Rev. 2018;37(1):173–87.
Palomba G, Doneddu V, Cossu A, Paliogiannis P, Manca A, Casula M, et al. Prognostic impact of KRAS, NRAS, BRAF, and PIK3CA mutations in primary colorectal carcinomas: a population-based study. J Transl Med. 2016;14(1):292.
Kadowaki S, Kakuta M, Takahashi S, Takahashi A, Arai Y, Nishimura Y, et al. Prognostic value of KRAS and BRAF mutations in curatively resected colorectal cancer. World J Gastroenterol. 2015;21(4):1275–83.
Won DD, Lee JI, Lee IK, Oh ST, Jung ES, Lee SH. The prognostic significance of KRAS and BRAF mutation status in Korean colorectal cancer patients. BMC Cancer. 2017;17(1):403.
Yokota T, Ura T, Shibata N, Takahari D, Shitara K, Nomura M, et al. BRAF mutation is a powerful prognostic factor in advanced and recurrent colorectal cancer. Br J Cancer. 2011;104(5):856–62.
Neugut AI, Matasar M, Wang X, McBride R, Jacobson JS, Tsai WY, et al. Duration of adjuvant chemotherapy for colon cancer and survival among the elderly. J Clin Oncol. 2006;24(15):2368–75.
Demicheli R, Miceli R, Moliterni A, Zambetti M, Hrushesky WJM, Retsky MW, et al. Breast cancer recurrence dynamics following adjuvant CMF is consistent with tumor dormancy and mastectomy-driven acceleration of the metastatic process. Ann Oncol. 2005;16(9):1449–57.
Dignam JJ, Dukic V, Anderson SJ, Mamounas EP, Wickerham DL, Wolmark N. Hazard of recurrence and adjuvant treatment effects over time in lymph node-negative breast cancer. Breast Cancer Res Treat. 2009;116(3):595–602.
Jatoi I, Bandos H, Jeong JH, Anderson WF, Romond EH, Mamounas EP, et al. Time-varying effects of breast cancer adjuvant systemic therapy. J Natl Cancer Inst. 2016;108(1):djv304.
Sofia Vala I, Martins LR, Imaizumi N, Nunes RJ, Rino J, Kuonen F, et al. Low doses of ionizing radiation promote tumor growth and metastasis by enhancing angiogenesis. PLoS One. 2010;5(6):e11222.
Sundahl N, Duprez F, Ost P, De Neve W, Mareel M. Effects of radiation on the metastatic process. Mol Med. 2018;24(1):16.
Vilalta M, Rafat M, Graves EE. Effects of radiation on metastasis and tumor cell migration. Cell Mol Life Sci. 2016;73(16):2999–3007.
Song JW, Chung KC. Observational studies: cohort and case - control studies. Plast Reconstr Surg. 2010;126(6):2234–42.
Acknowledgements
The authors thank the patients for making this study possible. We also wish to thank all the personnel and investigators who contributed to the patient recruitment and data collection at NFCCR as well as the staff at NLCHI and Provincial Tumor Registry-NL/Dr. H. Bliss Murphy Cancer Centre for their assistance with a portion of the patient outcome data. SS is a senior investigator of the Beatrice Hunter Cancer Research Institute (BHCRI).
Funding
This study was in part supported by the Dean’s Transition Funds (PI: SS). Yajun Yu has been supported by TPMI/NL Support Educational Funding Award and The Dean’s Fellowship (Faculty of Medicine, Memorial University) and is a trainee in the Cancer Research Training Program of the Beatrice Hunter Cancer Research Institute, with funds provided by the Terry Fox Research Institute. Funders had no involvement in the design of the study; collection, analysis, and interpretation of the data; and writing of the manuscript.
Author information
Authors and Affiliations
Contributions
YY helped design the statistical approach, performed all the analyses, interpreted the results, and drafted the manuscript. MC, ED, JG, WP, PP, and SS helped with the collection of patient-related data. YEY helped with the statistical methodology. SS conceptualized and led the study, helped design the study and interpret the results, and revised and submitted the manuscript. YY, MC, ED, JG, WP, PP, YEY, and SS approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval (reference numbers 09.106 and 15.294) was provided by the Health Research Ethics Board (HREB) of Newfoundland and Labrador prior to the start of this study. Since this is a secondary-use-of-data study, HREB has waived the need for patient consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
William Pollett is retired.
Additional file
Additional file 1:
Figure S1. Kaplan-Meier curves for the variables with a p value < 0.05 in the univariate Cox analyses and with a p value < 0.05 in the PH assumption test (type A variables). Figure S2. Kaplan-Meier curves for the variables with a p value ≥ 0.05 in the univariate Cox analyses and with a p value < 0.05 in the PH assumption test (type B variables). Figure S3. Kaplan-Meier curves for disease stage. Table S1. Pair-wise Pearson correlation coefficient values for the baseline variables. Table S2. Associations between clinico-demographic/molecular variables and overall survival (OS) in multivariate analysis. Table S3. Associations between clinico-demographic/molecular variables and disease-specific survival (DSS) in multivariate analysis. Table S4. Associations between clinico-demographic/molecular variables and recurrence-free survival (RFS) in multivariate analysis. Table S5. Associations between clinico-demographic/molecular variables and metastasis-free survival (MFS) in multivariate analysis. Table S6. Associations between clinico-demographic/molecular variables and recurrence/metastasis-free survival (RMFS) in multivariate analysis. Table S7. Associations between clinico-demographic/molecular variables and event-free survival (EFS) in multivariate analysis. (DOCX 556 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yu, Y., Carey, M., Pollett, W. et al. The long-term survival characteristics of a cohort of colorectal cancer patients and baseline variables associated with survival outcomes with or without time-varying effects. BMC Med 17, 150 (2019). https://doi.org/10.1186/s12916-019-1379-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12916-019-1379-5