Abstract
Background
This study was designed to determine the Human papillomavirus (HPV) prevalence and its distribution of genotypes in various regions of Yunnan Province, China.
Method
In this study, participants were recruited during routine gynecologic examination between Oct 2013 and Feb 2015. A total of 17,898 women were recruited. Polymerase chain reaction was used for detecting the HPV positive samples and HPV geno-array test was used for genoty**.
Results
The overall HPV infection rate (19.9 %) among the south-western women was significantly higher (P = 0.001) than that among the north-western (18.0 %), south-eastern (13.3 %), north-eastern (11.1 %) and central women (12.9 %). The high-risk (HR) (18.1 %, P = 0.001) and single genotype (16.7 %, P = 0.001) infection rates among the South-western women were also significantly higher than those of among the north-western (13.9 %, 11.3 %), south-eastern (11.6 %, 10.5 %), north-eastern (9.6 %, 9.1 %) and central women (10.5 %, 10.0 %), respectively. While, the infections with multiple HPV (4.2 %) genotypes were significantly more common (P = 0.001) among women in north-western Yunnan than women in the south-western (1.3 %, 3.1 %), south-eastern (1.7 %, 2.7 %), north-eastern (1.5 %, 2.0 %) and central Yunnan (2.4 %, 2.9 %). A total of 30 HPV genotypes were detected; among them 13 were HR-HPV, 3 were PHR-HPV (Potential High risk), 8 were LR-HPV (Low risk) and six were unclassified. The most common HPV genotypes were HPV-52, 16, 58, 53 in control group, HPV-16, 52, 58, 39 and 53 in CINI (Cervical intraepithelial Neoplasia), HPV-52, 16, 58, 33, 53 and 81 in CINII, HPV16, 58, 18, 52, 81 in CINIII and HPV-16 18, 58, 52 in cervical cancer (CC), respectively. Such variation has also been observed about distribution of HPV genotypes distribution among single and multiple infections.
Conclusion
This study gives an epidemiological estimate of HPV prevalence and different genotype distribution in various region of Yunnan province and further explains its prevalence in different neoplastic lesions. Overall HPV-16, 52, 58, and 18 are the leading HR-HPV genotypes.
Similar content being viewed by others
Background
Human papillomavirus (HPV) infections are the most frequently sexually transmitted infections throughout the world. Worldwide, the prevalence of HPV is approximately 11–12 % [1], and 85 % of the infections and 88 % of the deaths caused by this virus occur in develo** countries [2]. The prevalence of HPV varies substantially with respect to ethnicity and geographic location [Histo-pathological analysis During colposcopy, the cervix was divided into four parts and each part was observed individually. All visually abnormal areas were biopsied. Every part with normal colposcopic impressions had one random biopsy collected at the squamo-columnar junction. Endocervical curettage was then performed. All cervical biopsies were performed with standard 2 mm POI biopsy forceps, which allows rapid healing of the biopsy sites and minimizes patient distress. Histological slides were reviewed by two senior pathologists from Yunnan First Peoples Hospital. The cervical intraepithelial neoplasia grading and cervical cancer was diagnosed according to the World Health Organization classification system (CIN I–III) [19]. Samples that tested positive for β-globin were analysed by PCR amplification of HPV DNA. HPV-positive samples were confirmed by PCR with universal L1 primer MY09/11 and GP5/6 systems [20]. DNA from HeLa and Caski cell lines was used as positive controls, and mixtures without sample DNA were used as negative controls. HPV genotypes were determined using an HPV GenoArray Test Kit (Hybribio, Chaozhou, China), according to the manufacturer’s instructions. Geno-Array is an L1 consensus primer-based PCR assay [21] that is capable of amplifying 23 HPV genotypes, including 13 HR-HPV genotypes (HPV-16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 68), 3 PHR-HPV genotypes (HPV-53, 66, and 81) and 7 low-risk HPV (LR-HPV) genotypes (HPV-6, 11, 42, 43, 44 and 61). The assay was conducted according to the manufacturer’s recommendations. PCR was performed in a reaction volume of 25 μl containing 5 μl of DNA template, 19.25 μl of the provided master mix, and 0.75 μl DNA Taq polymerase, using a Perkin-Elmer GeneAmp PCR System 9700 (Applied Biosystems) The amplification procedure was performed as follows: 9 min of denaturation at 95 °C, followed by 40 cycles of 20 s of denaturation at 95 °C, 30 s of annealing at 55 °C, 30 s of elongation at 72 °C, and a final extension for 5 min at 72 °C. All the samples that were identified as positive through PCR were genotype with two methods. First we run Geno-Array test and secondly we performed direct sequencing. For the DNA sequencing, new PCR was run with reaction mixture 50 μL containing 6 μL of the DNA extract, 1 μL of 10 μmolar MY09 primer, 1 μL of 10 μmolar MY11 primer and 25 μL of the provided master mixture, and 15 μL dH2O. The consensus primer products were separated by electrophoresis on a 2 % agarose gel and purified with Tiangel PCR purification kit. The DNA was then directly sequenced using the ABI PRISM Big Dye Terminator Cycle Sequencing Ready Reaction (Invitrogen, Bei**g, CN) on an ABI 310 DNA analyzer. The nucleotide sequences were aligned and compared with those of known HPV genotypes available through Genbank by using the BLAST 2.0 software server (http://blast.ncbi.nlm.nih.gov/Blast.cgi). The sample was identified as a particular HPV genotype if the sequence was 95 % homologous with the reference standard. The Chi-square test was performed to compare the differences in HPV genotype distribution among the histo-pathologically normal and abnormal samples and among the various regions. Data analysis was performed using SPSS 20.0 (SPSS, Chicago, USA). All statistical tests were two-sided; P values < 0.05 were considered statistically significant.HPV genoty**
Statistical analysis
Results
Population characteristics
All of the participants were recruited from various regions of Yunnan province, China (Table 1 and Fig. 1 show the regions inhabited by the study participants). The median age of the 17,898 women included in this study was 38 years, with a range of 18 to 93 years (mean = 40.5 years, SD = 8.79 years, 95 % CI, 40.37–40.63). A total of 75.2 % women were Han, and 24.8 % were of other ethnicities. In addition, 38.3 % of the women came from rural areas, and 61.7 % were from urban areas. Most of the women (82.3 %) were married and reported having a single sexual partner, and the mean number of years of sexual activity was 17. Only 57.7 % of the women had delivered a single baby. A summary of the participants’ characteristics is shown in Table 1. Of the 17,898 women, 16,968 (94.8 %) had normal, 458 had CIN1, 247 had CIN2, 181 had CIN3, and 44 had CC (Table 3).
HPV genotype distribution by region
The overall HPV infection rate (19.9 %) among the south-western women was significantly higher than that among the north-western (18.0 %), south-eastern (13.3 %), north-eastern (11.1 %) and central women (12.9 %). The high-risk (HR) (18.1 %) and single genotype (16.7 %) infection rates among the South-western women were also significantly higher than those of among the north-western (13.9 %, 11.3 %), south-eastern (11.6 %, 10.5 %), north-eastern (9.6 %, 9.1 %) and central women (10.5 %, 10.0 %), respectively. While, the infections with other HPV (4.1 %) and with multiple HPV (4.2 %) genotypes were significantly more common (P = 0.001) among women in north-western than women in the south-western (1.3 %, 3.1 %), south-eastern (1.7 %, 2.7 %), north-eastern (1.5 %, 2.0 %) and central women (2.4 %, 2.9 %). The HPV genotype distribution data by region is shown in Table 4. The prevalence of HPV-16 (5.9 %) and HPV-58 (3.5 %) were significantly (P = 0.001, P = 0.001) more frequent in the southwest region compared with those in the central, north-east, south-east, and north-west regions. With the exception of the above-mentioned genotypes, no significance differences in the distributions of any of the other HPV genotypes were observed among the five regions of Yunnan province (Table 2).
HPV genotypes and histo-pathological grades
The prevalence of overall, HR-HPV, and single genotypes infection significantly increased as the infection progressed in advanced lesions. While, the prevalence of multiple genotypes infection and other genotypes were decreased as the infection progressed in advanced lesions but the difference was not significant. HPV-16, 58, 52, and 18 were significantly more frequent in advance abnormal cervical lesion that those of other genotypes (Fig. 2). The distribution of HPV genotypes according to cervical histo-pathological stage is shown in Table 2. A total of 23 HPV genotypes were detected in the histo-pathologically abnormal samples with different prevalence rates. The six most common HPV genotypes detected in the CINI samples were HPV-16, 52, 58, 53, 39, and 81. In the CINII samples, HPV-52 was the most prevalent, followed by HPV-16, 58, 33, 81, and 51. However, in the CINIII and CC samples, HPV-16 was more prevalent, followed by HPV-58, 18, and 52. A total of 30 HPV genotypes were detected in the normal group, the most common of which were HPV-52, followed by HPV-16, 58, 53, 18, 51, 68 and 81 (Table 3).
In this study, three PHR-HPV genotypes (HPV-53, 66, and 81) were also detected, and they were highly prevalent in the CIN1 and CIN2 samples. Only three CC samples were found to have a co-infection with the HPV-66 and HR-HPV genotypes. Interestingly, eight single and multiple LR-HPV infections were detected in both the normal and abnormal cytology groups. Some of the unclassified HPV genotypes, such as HPV-67, 69, 70, 71, 82 and 83, were also found in the control group. Table 3 shows the genotype distributions among the abnormal cytology and control groups.
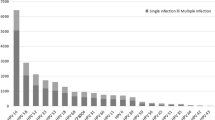
HPV genotypes and infection
The distribution of HPV genotypes according to the type of infection is shown in Table 3. A total of 16,968 women had normal cytological (normal group) results, and of them, 8.3 % (1402/16968) were infected with a single HPV genotype. In contrast we identified the presence of HPV DNA in 60.4 % (562/930) of the women in the abnormal histo-pathological group. Multiple genotype infections were the most common, and the rate of this type of infection was significantly higher (Table 2, P = 0.001) in the abnormal histo-pathological group (236/930, 24.4 %) compared with that in the normal group (1.8 %, 304/16968). The proportion of uncharacterised infection was also higher in the abnormal histo-pathological group (7.1 %, 68/930) compared with that in the normal group (0.75 %, 128/16968). The distribution of HPV genotypes according to the type of infection is shown in Table 3. In cases of single infection, HPV-16 (abnormal histo-pathological group = 136/562, 24.2 %; normal group = 280/16968, 1.6 %; P = 0.001), 18 (abnormal histo-pathological group = 48/562, 8.5 %; normal group = 84/16968, 0.5 %; P = 0.003), 33 (abnormal histo-pathological group = 36/562, 6.4 %; normal group = 48/16968, 0.3 %; P = 0.001), and 58 (abnormal histo-pathological group = 88/562, 15.7 %; normal group = 152/16968, 0.9 %; P = 0.001) were detected significantly more frequently in the abnormal histo-pathological group compared with the control group. In addition, HPV-31 (abnormal histo-pathological group = 3/562, 0.5 %; normal group = 36/16968, 0.21 %; P = 0.002), 51 (abnormal histo-pathological group = 8/562, 1.4 %; normal group = 52/1402, 0.3 %; P = 0.001), 61 (abnormal histo-pathological group = 3/562, 0.5 %; normal group = 24/16968, 0.1 %; P = 0.05), 66 (abnormal histo-pathological group = 3/562, 0.5 %; normal group = 24/16968, 0.1 %; P = 0.05), and 68 (abnormal histo-pathological group = 10/562, 1.8 %; normal group = 52/16968, 0.3 %; P = 0.001) were significantly more common in the normal group compared with the abnormal histo-pathological group (Table 4).
To determine the possible variation in HPV genotype distribution among the various age groups, the abnormal histo-pathological and normal groups were stratified into three groups according to age. Correlation analysis revealed that HPV prevalence was more complex in the younger and older participants compared with the middle age group (Figs. 3 and 4). The highest overall, HR-HPV and multiple HPV prevalence was observed in the <35 years age group, and it declined thereafter with increasing age. A less pronounced second peak in prevalence was observed for the normal women in the older age group (>46 years). However, overall, high-risk and multiple-genotype infections among the abnormal histo-pathological women exhibited two peaks in prevalence, with the first peaks of 88.9, 63.5 and 25.5 %, respectively, occurring at <35 years and the second peaks of 95.5, 64.3 and 31.2 % occurring at >46 years. Overall, we did not find significant differences among the various age groups in HPV genotype distribution. Correlation analysis revealed that the HPV genotype prevalence’s were highly correlated in single and multiple infections among the younger women (<35 years) and older women in both the normal and abnormal histo-pathological groups. However, HPV-16 was more frequent in the younger women (<35 years) in both the normal and abnormal histo-pathological groups. The prevalence’s of other genotypes, such as HPV-52, 58, 68, 33, 53, and 66, were found vary among the different age groups and varying histo-pathological grades (Table 5).
Discussion
Many studies have reported the HPV prevalence and its genotype distributions in various provinces of P. R. China [22, 23]. However, no relevant epidemiological data are available for Yunnan province. To the best of our knowledge, the current study is the first to report the epidemiological prevalence and distribution of HPV genotypes in various region of Yunnan. Samples screened in this study were obtained from different ethnic populations from different geographic regions of Yunnan province. Therefore, the results of this study provide precise estimations of the HPV prevalence and genotype distributions in histo-pathological abnormal and normal cervical samples obtained from women throughout Yunnan province.
In this study, the overall HPV infection rate of 14.0 % was higher than the documented rates in neighbouring countries (6.2 % in Southeast Asia, 6.6 % in south central Asia and 8.0 % in other Asian countries [15, 24]. However, reports from some regions of mainland China have stated that the overall prevalence is 18.4 % in Shenzhen city [25], 13.3 % in Zhejiang province [26] and 14.8 % in Shanxi province [27], in agreement with our reported HPV prevalence. HPV prevalence has been documented to vary in different geographic regions, e.g., it is 8.1 % in Europe, 11.3 % in North America, 22.1 % in Africa and 8.0 % in Asia [15]. Here, we found that its prevalence was significantly higher among the south-western women (19.9 %) than the women from other four regions. The HPV prevalence in the south-western and north-western region was in line with the previously reported infection rate for north-western region of Yunnan (18.4 %) [27, 32, 33] (Table 1).
Analysis of the specific HPV genotype distribution in the abnormal histo-pathological group indicated that it was highly variable in the histo-pathological abnormal lesions. HPV-16 (45.4 %) was the most frequently detected genotype in SCC, followed by HPV-58 (18.2 %), 18 (18.2 %), and 52 (15.9 %). Interestingly, 8 SCC patients were also found to have a multiple genotype infection (co-infection of HPV-59 and 66 with HPV-52 and 58, and 18). These findings are in complete agreement with previously reported data, indicating that HPV-16, 18, 52, and 58 are most frequently present in cervical cancer [9, 34]. HPV-16, 58, 18 and 52 were also frequent in the CIN3 samples, which is consistent with previous reports [25, 33, 37]. However, in this study, we did not find them to be highly carcinogenic, which may be due to variable geographic factors, biological factors, lifestyle, or human and viral genetic factors. Further, we found a high prevalence of PHR-HPV, particularly HPV-53 and 81 and the LR-HPV genotypes HPV-6 and 11. However, these genotypes were only identified in multiple genotype infections. These findings are in line with previously reported data [38]. In this study, the prevalence of HR-HPV was increased in samples with advanced histo-pathological grades. The incidence of HR-HPV infection, and particularly that of single genotype infection, was very high in the abnormal histo-pathological group compared with that in the normal group. These findings are in accordance with those of Castle et al. [39]. On the basis of these observations, we suggest that attention should be paid to the histo-pathological outcomes of CIN2, CIN3 and higher-grade lesions, even in the absence of specific genotype information.
In this study, we also evaluated the HPV genotype distributions among different age groups. HPV-16 was more frequent in women less than 35 years old in both the normal and abnormal cytology groups. However, the distributions of the other genotypes varied among the different age groups with lesions of differing cytology grades. HPV-52 and 18 showed double-peak prevalence in the normal cytology group. The prevalence of HPV-52 in the abnormal cytology group decreased with increasing age; however, that of HPV-18 increased with increasing age in this group. Such variation has also been observed for other genotypes, as shown in Table 4. These findings indicate that various age groups possess different genotypes in lesions with differing cytological grades [40]. Thus, it is very important to determine the potential roles of the different HPV genotypes in carcinogenesis development among various age groups and to further determine their potential risk and contribution to carcinogenesis in future studies.
The results of this study suggest that cervical screening is vital for women, particularly minority ethnic women, to prevent HPV-related cervical cancer [41]. An important link between HPV infection and development of cervical neoplasia has been identified in this study. Thus, the timely detection of HPV infection would be very helpful for preventing disease progression, considering that its early detection in patients with cervical lesions has been well established to result in a decrease in the rate of cancer development [42].
There are some limitations of this study that must be considered when interpreting our findings. Yunnan includes 26 state-certified ethnic minorities who live in different regions of the province. Most of them do not want to participate in epidemiological studies due to their ethnic beliefs. In this study, we focused only on those women who visited a public hospital with routine gynaecological examination.
Conclusion
This study provides epidemiological estimates of HPV genotype distributions in different regions of the province and further reports the prevalence of these genotypes in neoplastic lesions with differing cytological grades. We have found that overall, HPV-16, 52, 58, and 18 are the most common HR-HPV genotypes. However, the prevalence rates of these genotypes significantly differ in different regions of the province. PHR-HPV-53 is also a predominant genotype in some regions. These variations could be due to the large number of ethnic populations residing in the province. A vaccine currently under trial has been formulated for HPV-16, 18, 11, and 6, and it will be introduced nationally in the coming years. However, HPV-52 and 58 are the predominant genotypes in several regions. Thus, based on our observations, a new tetravalent vaccine may be more effective than a bivalent vaccine in China, and particularly in Yunnan province. Further, due to large-scale geographic variation in HPV genotype distribution, a future large-scale, multi-ethnic population-based study must be conducted to obtain comprehensive information on the prevalence and genotype distribution of HPV in various Chinese ethnic populations.
Abbreviations
HPV, human papillomavirus; HR-HPV, high risk-HPV; PHR-HPV, potential high risk-HPV; LR-HPV, low risk-HPV; CIN, cervical intraepithelial neoplasia; CC, cervical cancer.
References
Bruni L, Diaz M, Castellsague X, Ferrer E, Bosch FX, de Sanjose S. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J Infect Dis. 2010;202:1789–99.
Ferlay J, Shin HR, Bray F, Forman D, Mathers C. Parkin, D. M.; GLOBOCAN 2008 v2.0. Cancer incidence and mortality worldwide in 2008 IARC Cancer Base No. 10 (2010) http://www.iarc.fr/en/media-centre/iarcnews/2010/globocan2008.php. 20 Feb 2015.
Baloch Z, Yue L, Yuan T, Feng Y, Tai W, Liu Y, Wang B, Li X, Liu L, Zhang AM, Wu X, **a X. Status of Human Papillomavirus Infection in the Ethnic Population in Yunnan Province, China. Biomed Res Int. 2015;2015:314815.
Yang L, Parkin DM, Li L. Time trends in cancer mortality in China: 1987–1999. Int J Cancer. 2003;106:771–83.
Clifford GM, Gallus S, Herrero R, Munoz N, Snijders PJ, et al. Worldwide distribution of human papillomavirus types in cytologically normal women in the International Agency for Research on Cancer HPV prevalence surveys: a pooled analysis. Lancet. 2005;366:991–8.
Liu X, Feng A, Cui Y, Tobe RG. Prevention of human papillomavirus (HPV) infection and cervical cancer in China: How does HPV vaccination bring about benefits to Chinese women? Biosci Trends. 2013;7:159–67.
Koutsky L. Epidemiology of genital human papillomavirus infection. Am J Med. 1997;102:3–8.
Li N, Franceschi S, Howell-Jones R, Snijders PJ, Clifford GM. Human papillomavirus type distribution in 30,848 invasive cervical cancers worldwide: Variation by geographical region, histological type and year of publication. Int J Cancer. 2011;128:927–35.
Crow JM. HPV: The global burden. Nature. 2012;488:S2–3.
Lacey CJ, Lowndes CM, Shah KV. Chapter 4: Burden and management of non-cancerous HPV-related conditions: HPV-6/11 disease. Vaccine. 2006;24:S35–41.
Munoz N, Bosch FX, Castellsague X, de Sanjose S, et al. Against which human papillomavirus types shall we vaccinate and screen? The international perspective. Int J Cancer. 2004;111:278–85.
Huang S, Afonina I, Miller BA, Beckmann AM. Human Papillomavirus types 52 and 58 are prevalent in cervical cancers from Chinese women. Int J Cancer. 1997;70:408–11.
Lo KW, Wong YF, Chan MK, Li JC, Poon JS, Wang V, Zhu SN, Zhang TM, He ZG, et al. Prevalence of human Papillomavirus in cervical cancer: a multi-center study in China. Int J Cancer. 2002;100:327–31.
Liu J, Rose B, Huang X, Liao G, Carter J, Wu X, Thompson C. Comparative analysis of characteristics of women with cervical cancer in high-versus low-incidence regions. Gynecol Oncol. 2004;94:803–10.
de Sanjose S, Diaz M, Castellsague X, Clifford G, Bruni L, Muñoz N, Bosch FX. Worldwide prevalence and genotype distribution of cervical human papillomavirs DNA in women with normal cytology: a meta-analysis. Lancet Infect Dis. 2007;7:453–9.
Chow CS. Cultural diversity and tourism development in Yunnan province. China Geogr. 2005;90(3):294–303.
Linda Stone, Kinship and Gender, 2006, Westview, 3rd ed., ch. 6. The Center for Research on Tibet Papers on Tibetan Marriage and Polyandry. https://www.coursehero.com/file/p7n9h6l/This-process-is-significant-because-it-ensures-the-continuation-of-a-specific/. Accessed 10 Jan 2015.
Zou H, Sun Y, Zhang G, Tu Y, Meng X, Liu T, ** Z, Fan X, Gao Y. Positivity and incidence of human papillomavirus in women attending gynecological department of a major comprehensive hospital in Kunming, China 2012-2014. J Med Virol. 2015 Sep 12. doi: 10.1002/jmv.24377. [Epub ahead of print]
Kurman RJ, Norris HJ, Wilkinson EJ. Tumors of the Cervix, Vagina, and Vulva. Washington: Armed Forces Institute of Pathology; 1992.
Husnjak K, Grce M, Magdic L, Paveli K. Comparison of five different polymerase chain reaction methods for detection of human papillomavirus in cervical cell specimens. J Virol Methods. 2000;88:125–34.
Liu SS, Leung RC, Chan KK, Cheung AN, Ngan HY. Evaluation of a newly developed GenoArray human papillomavirus (HPV) genoty** assay and comparison with the Roche Linear Array HPV genoty** assay. J Clin Microbiol. 2010;48:758–64.
Li J, Huang R, Schmidt JE, Qiao YL. Epidemiological features of Human Papillomavirs (HPV) infection among women living in Mainland China. Asian Pac J Cancer Prev. 2013;14(7):4015–23.
Hou R, Xu C, Zhang S, Wu M, Zhang W. Distribution of human papillomavirus genotype and cervical neoplasia among women with abnormal cytology in Bei**g, China. Int J Gynaecol Obstet. 2012;119:257–61.
Sukvirach S, Smith JS, Tunsakul S, Muñoz N, Kesararat V, et al. Population-based human papillomavirus prevalence in Lampang and Songkla, Thailand. J Infect Dis. 2003;187:1246–56.
Wu RF, Dai M, Qiao YL, Clifford GM, Liu ZH, Arslan A, et al. Human papillomavirus infection in women in Shenzhen City, People’s Republic of China, a population typical of recent Chinese urbanisation. Int J Cancer. 2007;121:1306–11.
Li N, Dai M. Human papillomavirus infection in China: a multi-centric cross-sectional study. Chin J Dis Control Prev. 2008;12:411–5.
** Q, Shen K, Li H, Zhou XR, Huang HF, et al. Age-specific prevalence of human papillomavirus by grade of cervical cytology in Tibetan women. Chin Med J. 2010;123:2004–11.
Baloch Z, Yuan T, Wang B, Tai W, Feng Y, Liu Y, Li X, Liu L, Zhang AM, Wu X, **a X. Ethnic and geographic variations in HPV prevalence and genotype distribution in north-western Yunnan, China. J Med Virol. 2015;88:532–40.
Dai M, Bao YP, Li N, Clifford GM, Vaccarella S, et al. Human papillomavirus infection in Shanxi Province, People’s Republic of China: a population-based study. Br J Cancer. 2006;95:96–101.
Ye J, Cheng X, Chen X, Ye F, Lu W, **e X. Prevalence and risk profile of cervical Human papillomavirus infection in Zhejiang Province, southeast China: a population-based study. Virol J. 2010;7:66.
Yuan X, Yang Y, Gu D, Liu H, Yang H, et al. Prevalence of human papillomavirus infection among women with and without normal cervical histology in Shandong Province, China. Arch Gynecol Obstet. 2011;283:1385–9.
Chung MY, Kim YW, Bae SM, Kwon EH, Chaturvedi PK, Battogtokh G, Ahn WS. Development of a bead-based multiplex genoty** method for diagnostic characterization of HPV infection. PLoS One. 2010;7:e32259.
Doménech-Peris A, Conesa-Zamora P, Sahuquillo-Frias L, Ortiz-Reina S, Moya Biosca J, Acosta-Ortega J, Pérez Guillermo M, Egea-Cortines M. Human papillomavirus genoty** in histological sections of precursor lesions of cervical carcinoma: its role as a possible adjunct for the evaluation of the oncogenic potential of specific human papillomavirus genotypes – a study in a coastal region of Southeastern Spain. Gynecol Obstet Invest. 2010;70:113–9.
Smith JS, Lindsay L, Hoots B, Keys J, Franceschi S, Winer R, Clifford GM. Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: a meta-analysis update. Int J Cancer. 2007;121:621–32.
Chen Q, **e LX, Qing ZR, Li LJ, Luo ZY, et al. Epidemiologic characterization of human papillomavirus infection in rural Chaozhou, eastern Guangdong Province of China. PLoS One. 2012;7:e32149.
Formentin A, Archambault J, Koushik A, Richardson H, Brassard P, Franco EL, Coutlee F. Human papillomavirus type 52 polymorphism and high-grade lesions of the uterine cervix. Int J Cancer. 2013;132:1821–30.
Clifford GM, Rana RK, Franceschi S, Smith S, Gough G, Pimenta JM. Human papillomavirus genotype distribution in low-grade cervical lesions: comparison by geographic region and with cervical cancer. Cancer Epidemiol Biomarkers Prev. 2005;14:1157–64.
De Sanjose S, Quint WG, Alemany L, Geraets DT, Klaustermeier JE, Lloveras B, et al. Retrospective International Survey and HPV Time Trends Study Group: Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11:1048–56.
Castle PE, Fetterman B, Thoma Cox J, Shaber R, Poitras N, Lorey T, Kinney W. The age-specific relationships of abnormal cytology and human papillomavirus DNA results to the risk of cervical precanc er and cancer. Obstet Gynecol. 2010;116:76–84.
Ronco G, Giorgi-Rossi P, Carozzi F, Confortini M, Dalla PP, Del Mistro A, et al. Efficacy of human papillomavirus testing for the detection of invasive cervical cancers and cervical intraepithelial neoplasia: a randomised controlled trial. Lancet Oncol. 2012;11:249–57.
Forman D, de Martel C, Lacey CJ, Soerjomataram I, Lortet-Tieulent J, et al. Global Burden of Human Papillomavirus and Related Diseases. Vaccine. 2012;30:F12–23.
Laara E, Day NE, Hakama M. Trends in mortality from cervical cancer in the Nordic countries: Association with organized screening programs. Lancet. 1987;1:1247–9.
Acknowledgments
We sincerely thank all the participants who took part in this study. We also sincerely thank Saqlain Abbas and Nafeesa Yasmeen (UVAS, Lahore) for their assistance with manuscript revision.
Funding
This study was supported by research grants from the Natural Science Foundation of China (81260248), Scientific and technological innovation talent support project (2015HC030) and the Key & New Product Development Project of Yunnan province (2013BC009). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The aggregate data supporting findings contained within this manuscript will be shared upon request submitted to the corresponding author. Identifying patient data will not be shared.
Authors’ contributions
ZB and LY designed the study, performed the data collection and genoty**, analysed the data and wrote the paper. TY, YL, and FY performed the data collection. LL, AZ, and WB contributed to collecting information from the participants. Prof. XX and XW supervised the study. All of the authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Ethics and consent to participate
Ethical approval was obtained from the Ethics Committee at Kunming University of Science and Technology and the Center for Disease Control and Prevention (CDC) in Yunnan Province, China. Written consent was individually obtained from each participant.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Baloch, Z., Li, Y., Yuan, T. et al. Epidemiologic characterization of human papillomavirus (HPV) infection in various regions of Yunnan Province of China. BMC Infect Dis 16, 228 (2016). https://doi.org/10.1186/s12879-016-1562-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-016-1562-7