Abstract
Background
Infection is more frequent, and serious in people aged > 65 as they experience non-specific signs and symptoms delaying diagnosis and prompt treatment. Monitoring signs and symptoms using decision support tools (DST) is one approach that could help improve early detection ensuring timely treatment and effective care.
Objective
To identify and analyse decision support tools available to support detection of infection in older people (> 65 years).
Methods
A sco** review of the literature 2010–2021 following Arksey and O’Malley (2005) framework and PRISMA-ScR guidelines. A search of MEDLINE, Cochrane, EMBASE, PubMed, CINAHL, Scopus and PsycINFO using terms to identify decision support tools for detection of infection in people > 65 years was conducted, supplemented with manual searches.
Results
Seventeen papers, reporting varying stages of development of different DSTs were analysed. DSTs largely focussed on specific types of infection i.e. urine, respiratory, sepsis and were frequently hospital based (n = 9) for use by physicians. Four DSTs had been developed in nursing homes and one a care home, two of which explored detection of non- specific infection.
Conclusions
DSTs provide an opportunity to ensure a consistent approach to early detection of infection supporting prompt action and treatment, thus avoiding emergency hospital admissions. A lack of consideration regarding their implementation in practice means that any attempt to create an optimal validated and tested DST for infection detection will be impeded. This absence may ultimately affect the ability of the workforce to provide more effective and timely care, particularly during the current covid-19 pandemic.
Similar content being viewed by others
Background
Infection is more frequent, and serious in people aged > 65 [1] as they experience non-specific signs and symptoms delaying diagnosis and prompt treatment [2]. Older adults who live in residential aged care are especially vulnerable to infection because of physical and cognitive decline, proximity to other residents and limited resources, as demonstrated during the Covid-19 pandemic [3]. Consequently, nursing home residents experience increased antibiotic usage, clinical complications, hospital admission, and mortality [4, 5].
The terms ‘nursing home’ and ‘residential care’ are defined and used differently between countries [6, 7]. For the sake of comparison, we will in this article use the term ‘nursing home’ to reflect care-homes with on-site qualified nurses; ‘care home’ to reflect those without on-site nursing, and housing that offer access to daily care [7], and ‘residential care’ as an umbrella term combining both, highlighting differences when relevant.
Nursing home residents are > 1.4 times risk of emergency admission and have > 50% unplanned hospital admissions compared to general population aged > 75 years [2, 8]. Unplanned hospital admissions cost the UK National Health Service (NHS) > £11 billion, US healthcare economy >$1.1 trillion/year and account for more than a third of admissions each year, and Swedish healthcare system >SEK 36 trillion a year for people aged > 65 years [9].
It is recognised that guidelines developed by the World Health Organisation can support management and surveillance of infection [10, 11]. However, in order to avoid inappropriate antibiotic therapy, unnecessary hospital admission and risk of complications there is also a need to improve the early detection of infection in older people many of whom present with non-specific clinical manifestations [2, 12,13,14].
Decision support tools (DST) comprise a wide range of approaches (i.e. algorithms simulation models, and/or techniques and methods) to support the decision making process related to patient care. DST provide a systematic approach to monitoring cognitive and behavioural changes [2, 15, 16] are one approach that could help improve early detection of infection. Ensuring a consistent approach to infection detection, prompt action and treatment [9], DSTs support decision-making and management of the situation [17], and can help reduce unplanned hospital admissions for nursing home residents [18, 19].
Identifying DSTs with the potential to improve detection of infection for older people, particularly for those in residential care is therefore crucial. Given the lack of evidence reporting acceptability and/or feasibility of DSTs for infection detection in older adults [9], a sco** review was undertaken to investigate DSTs designed to support the detection of infection in older people.
Methodology
A sco** review [20] of evidence published between January 2010–January 2021, and following Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Sco** Reviews (PRISMA-ScR) [21]. Sco** reviews are a recognised technique for ‘map**’ relevant literature, synthesizing and analysing a wide range of research and non-research related material in order to provide greater conceptual clarity about a specific topic or field of evidence. In the present case, the framework adopted was based on Arksey and O’Malley [20], and divided s into five stages.
Stage 1: identifying the research question
“What DSTs are available to support the detection of infection in older people (aged >65 years)?”
Stage 2: identifying relevant studies
Definition of terms: ‘Decision support tool’ was used as an umbrella term that allowed inclusion of other related concepts such as ‘decision support techniques’, ‘checklists’ or ‘decision aids’ [17].
Searches were conducted during October 2020–January 2021 using MEDLINE, Cochrane, EMBASE, PubMed, CINAHL, Scopus and PsycINFO databases. Database specific index terms, such as MeSH (MEDLINE) were used in searches together with keywords in the title/abstract, and synonyms and wildcard functions used for plurals and differences in US/UK spelling. Boolean logic was used and a string of keyword terms i.e. ‘decision support tool’, ‘clinical assessment tool’, ‘infection’. These sources were supplemented by hand searches. See Appendix 1 for search terms and example search string.
Articles were included that comprised:
-
Empirical studies, including meta-analyses, reporting a DST to support detection of suspected infection (including signs, symptoms and bio markers) in people > 65, any setting and by any member of staff.
-
DST at any stage of development/implementation to increase understanding regarding the degree of reliability in the diagnosis they can provide (see Appendix 2).
-
Peer reviewed articles published in English or Spanish.
Studies were excluded if they reported on DST use in diagnostic testing, predicting mortality, decisions about the use of do not resuscitate, specific therapy/drugs or treatment/procedure (i.e. pre-operative antibiotics), immunizations, or end of life scales. Review papers and grey literature were also excluded.
Stage 3: study selection
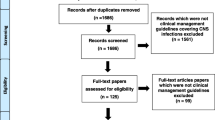
Results (n = 6513) were exported into Mendeley and duplicates removed (n = 1720) before titles and abstracts were screened in relation to inclusion/exclusion criteria.
Citations (n = 4793) were divided into 10 blocks with each block being independently screened, by title/abstract by two review team members (TB, JD, MS-L, CM, PT, CB, KH, JM, AM, VP). Discrepancies were moderated by four team members (OM, NC, AC, FM). After assessing for eligibility 47 articles were subject to full-text review (OM), with a resultant 17 papers included in the review (Fig. 1).
Stage 4: data extraction
Data extraction was conducted using a bespoke form to capture details about: study location; study type (methodology); setting and population; DST: stage of development and mode of use; infection(s) type; items or risk factors considered in the DST and results. Extraction was independently completed by one researcher (OM) then reviewed and discussed with three review team members (NC, AC & FM).
Stage 5: collating, summarising and reporting results
To chart, summarise and synthesise the findings, data extraction forms were used to group the DSTs by stage of development and infection type [16, 22, 23].
Results
Characteristics of included studies
Classified by stage of DST development, of the 17 included studies, two reported tool development [24, 25], one development and reliability [26], 7 development and validation [19, 27,28,29,30,31,32], three validation [33,34,35] and four testing [36,37,38,39] (see Table 1). Based in high income nations, most studies were conducted in single countries including: USA (n = 6) [32, 34, 37,38,39], UK (n = 3) [24, 27, 30], Sweden (n = 2) with one each from Canada [36], Denmark [35], Germany [33], Japan [26] and Spain [28]. Two international studies reported data from > 1 country [25, 31].
Most hospital based DSTs were designed for use only by physicians [31, 32, 35, 37, 39]. DSTs developed in NHs or care homes adopted a more multi-professional approach for use by physicians [24, 25, 36], nurses [24, 36, 38] and/ or nurse assistants [19, 24, 36]. The involvement of healthcare staff, using DSTs were also applicable to community care [30, 31, 34] and pre-hospital care [29].
Setting
Nine studies were based in the hospital [26,27,28, 31,32,33, 35, 37, 39], including two in an emergency department (ED) [33, 35] and one intensive care unit (ICU) [39]; four in nursing homes (NHs) [19, 25, 36, 38]; three in community [30, 31, 34], including one community ED [31]. One study was based in a pre-hospital ED (ambulance services) [29] with only one based in a care home [24].
Infection type
Fourteen articles focused on detecting a single type of infection including: pneumonia [26, 32], influenza [31], bacteraemia [27, 35], urinary tract infection (UTI) [28], sepsis [33, 37] and candida [39] in the hospital; UTI in nursing homes [25, 36, 38]; and wound [30], influenza [31] and sepsis [34] in the community. A tool to detect severe respiratory and central nervous system infection, and sepsis was developed for use in pre-hospital services [29]. Only two studies based in a nursing or care home reported on a tool to detect non-specific infection [19, 24].
A heterogeneous range of signs and symptoms were used to inform DST content. A summary of the signs and symptoms associated with the three most common types of infection addressed by DSTs i.e., sepsis, UTI and respiratory tract infection can be found in Table 2.
Fever and breathlessness were included as signs and symptoms reported in all four sepsis DSTs [29, 33, 34, 37]. Other signs and symptoms i.e. temperature < 36 °C and increased heart rate were included in three of the four sepsis tools, as they are also recognised criteria used to identify Systemic Inflammatory Response Syndrome (SIRS) [43]. A variety of signs and symptom (range n = 3–11) including acute dysuria, flank or suprapubic pain, haematuria, fever, urinary urgency/frequency, incontinence, and mental status change [25, 28, 36, 38] were frequently considered in DSTs designed to detect UTI. Of the four DSTs designed to detect respiratory tract infection [26, 29, 31, 32], change in mental status was the only sign or symptom considered in more than one DST [29, 32]. Other signs including oxygen saturation < 90%; fever, UTI, or aged > 70 years old were also considered by some authors [26, 29, 31, 32].
Stage of DST development and applications
DSTs are presented by their stage of development i.e. ‘development’; ‘development and reliability’, ‘development and validation’, ‘validation’ and ‘testing‘to increase understanding regarding their readiness for implementation and potential adoption in clinical practice in residential care [15, 16, 22, 23].
Development
Articles reporting DSTs at the ‘development stage’ (n = 2) each outlined an algorithm to improve infection detection: one focused on UTI [25], whereas Hughes et al. [24] considered three common infections (UTI, respiratory tract infection, skin and soft tissue infection).
Using a Delphi panel and series of consensus events Van Buul et al. [25] identified that UTI detection in frail older adults living in nursing homes was affected by the presence of a urinary catheter. A wide range of symptoms i.e., urinary, gastrointestinal, mental status change, general lack of well-being and decreased functional status for example, needed to be considered in those without catheters (see Table 2). For those with a catheter however, the algorithm required presence/absence of fever (> 24 h), rigors/shaking chills and clear-cut delirium in order to detect a UTI.
More recently, an algorithm based DST for use with common infections in UK care home residents was developed by Hughes et al. [24]. Informed by the Canadian-based Loeb et al. criteria [40] a multi-faceted approach including literature review, consensus meeting, focus groups and interviews was adopted to help improve management of the three infections (UTI, respiratory tract infection, skin and soft tissue infection) [24]. Based on presence of fever, change in functional status and psychological behaviour a revised and adapted algorithm describing management in terms of initial assessment, observation and action by the care home staff was produced (see Table 1).
Development and reliability
One study reported on the ‘development and reliability’ of a DST to detect pneumonia in hospital based patients, the ‘Bedridden Patient Pneumonia Risk’ (BPPR) [26]. Analysis of multiple risk factors confirmed that albumin < 3.5 g/dL and/or urinary bacteria were the only two risk factors associated independently with pneumonia. The resultant BPPR therefore is based on a score of 0, 1 or 2 according to their absence or presence (see Table 1).
Development and validation
Seven studies reported ‘development and validation’ of DSTs, five focused on specific infections [27,28,29, 31, 32], including three respiratory [29, 31, 32]; one wound infections [30] and one general [19] (see Tables 1 & 2).
Analysing data from a cohort of hospital based stroke patients Chumbler et al. [32] used logistic regression to inform the post-stroke pneumonia prediction system. Of the 22 variables considered in the development process, only dysphagia, history of pneumonia, National Institute of Health Stroke Scale (NIHSS) score, decreased cognitive and functional capacity and age > 70 years were independently associated with pneumonia. The discriminatory accuracy of the 3-level clinical prediction rule denoted low-risk (0 points; no risk factors present), medium-risk (presence of 1–3 risk factors) and high risks of pneumonia (4 or more risk factors). Authors [32] concluded that this clinical scoring system may be particularly relevant for hospitals using information technology systems.
Three exploratory models were used by Afonso et al. [31] to develop and validate a decision tree for the diagnosis of influenza with three models in the ED and primary care. Model 1 comprised seven terminal nodes based on temperature, symptom onset, presence of chills, cough and myalgia, whereas a simple tree with only two splits based on temperature and presence of chills was used for Model 2. Similarly model 3 had only two splits based on presence of fever and myalgia, with temperature treated as dichotomous variable (> 38 °C). Model 2 emerged as the most reliable model correctly classifying two thirds of patients as either low or high risk and in need of further evaluation for influenza, and treatment.
Finally, Johansson et al. [29] developed and validated a pre-hospital DST for detecting severe respiratory infection. With a required previous clinical suspicion, respiratory tract infection was detected by delirium, respiratory rate ≥ 30/min, systolic blood pressure < 90 mmHg, oxygen saturation < 90%. This pre-hospital DST however, was validated for diagnosis of severe central nervous system infection, and sepsis (Tables 1 & 2).
Two studies focussed on bacterial infection [27] and UTI [28], respectively. Rawson et al. developed a supervised machine learning (SML) algorithm for diagnosing any hospital based bacterial infection. In this case, microbiology records and six available blood parameters (C-reactive protein (CRP), white cell count (WCC), bilirubin, creatinine, alanine aminotransferase (ALT) and alkaline phosphatase) were used to detect bacteriemia. The validity results showed that those with infection were older and had a greater median CRP; WCC and ALT.
To predict probability of UTI by extended-spectrum beta-lactamase (ESBL)-producing microorganisms, García-Tello et al. [28] developed and validated a nomogram, a two-dimensional diagram designed to allow the approximate graphical computation of a mathematical function. Seven variables including sociodemographic data, history of UTI and living in a nursing home, were considered with results confirming the nomogram had reasonable accuracy in predicting the risk of infection by ESBL-producing bacteria (see Table 1).
Aiming to improve the detection of wound infection, Siaw-Saky [30] developed a ‘Wound Infection Risk- Assessment and Evaluation tool’ (WIRE) comprising three categories medical history (i.e. diabetes or malnutrition), local signs and symptoms (i.e., pain or erythema), and systemic signs and symptoms (i.e., temperature and rigors). Using audit data, the presence of infection was confirmed in 117/ 150 (78%) cases whose wounds were subject to both WIRE and swab assessment.
Finally, a clinical decision-making algorithm, ‘Early Detection of Infection Scale ‘EDIS, for detecting all type of infections in older adults living in NHs was developed by Sund-Levander [41] and validated by Tingström et al. [19] for use by Swedish care workers. Validation of the 13 item EDIS tool suggested that ‘he/she is not as usual’ along with ‘increased temperature’, and presence of ‘respiratory symptoms’ and/or ‘general signs and symptoms of illness’ made by nursing assistants should be taken seriously, and lead to follow up by a nurse or physician.
Validation
Three studies [33,34,35] reported on DST ‘validation’. Two studies focused on detecting sepsis [33, 34] were based on the signs and symptoms of SIRS [43] (see Tables 1 & 2); and one bacteriemia [35].
Using a computer algorithm, and categorising urgency of ED patients into ‘immediate’, or ‘within 10 or 30 minutes’ the ‘Manchester Triage System’ (MTS) [33] was validated for use as a ‘sepsis alert’, with results indicating the that the tool had significant potential to improve prioritisation and treatment of ED patients with septic illness.
Similarly, Walchok et al. [34] validated the ‘Prehospital Sepsis Assessment Tool’ (Pre-SAT) [42] (see Tables 1 & 2). The criteria were used after gaining consensus from the two receiving hospital systems EMS sepsis committees were that having two signs of SIRS and a known or ‘suspected source of infection’ required the paramedic to issue a ‘sepsis alert’ to the receiving ED. In terms of effectiveness, the application of this criteria provoked that EMS administered antibiotics matched blood culture growth in 72% of patients.
In order to improve clinical guidance regarding the need for obtaining blood cultures, Jessen et al. [35] validated a clinical decision rule to support rapid bedside estimation of bacteremia risk. Using several signs and symptoms i.e. suspected endocarditis; temperature; indwelling vascular catheter; age > 65 years; chills; vomiting; hypotension; white blood cell count; bands; platelets; and creatinine this DST was developed to support ED physicians and treatment consensus.
Testing
Testing of DSTs, to confirm factor structure on an independent data set, was used to determine how well the measured variables represent the number of constructs in four studies [36,37,38,39]: two UTI [36, 38], one sepsis [37] and one candidemia [39].
Both studies exploring DSTs for UTIs were undertaken in nursing homes and used the same signs and symptoms (see Table 2). Interesting, the ‘UTI Long-term care (LTC) Facilities Checklist’ [36] detects infection by considering whether or not residents are catheterised, whereas the decision-making aid for suspected UTI tested by McMaughan et al. [38] does not make this differentiation (see Tables 1 & 2).
Using a clinical decision support system (CDS) for early recognition of sepsis, the DST tested by Amland and Hahn-Cover [37] included SIRS criteria [43], cardiovascular items and blood analytical parameters (see Tables 1 & 2). The authors report the system’s activation rate appears to be acceptable in terms of being consistent with a flow sheet paradigm for capturing results, clinical events, and time stamps, These indicate [37] that future quality improvement initiatives should include the application of the sepsis CDS across patient care processes.
Finally, candida scores [45, 46] in ICU patients with sepsis were used to test a 4 item DST for candidema by Umberger et al. [39]. Infection was confirmed with a score of ≥3 points and based on items related to severe sepsis (2 points), surgery at baseline (1 point), total parenteral nutrition (1 point), and Candida colonization (1 point). Despite a relatively poor sensitivity (see Table 1), Umberger et al. [39] results indicate a reasonable specificity with a strong negative predictive value proposing this make this tool a viable option for screening medically ill patients who may require antifungal agents.
Discussion
This sco** review found a diverse group of DSTs available to support detection of infection in older people at varying stages of development, largely focused on specific types of infection, with few based in the nursing or care home setting (n = 5) [19, 24, 25, 36, 38]. Each article reported a different DST and only two reported a DST based on the adaptation of a previously developed tool [24, 33]. In addition to wider concerns regarding deficits in knowledge utilisation, and the need to ensure more efficient use of resources, the heterogenous nature of the DST dataset for infection detection reflects the need to expedite the translation of research findings in to clinical practice [47]. Given the concerns regarding the projected rise in older people, subsequent increase in the number of nursing and care home residents [13, 14, 48] and impact on future service utilisation, this review is timely and of international relevance. It is the first of its type to chart and synthesize the evidence on this issue.
Our review found DSTs for improving infection detection in a broad range of settings in high income countries. However, results highlighted that most infection detection DSTs had been developed for use in hospitals [26,27,28, 31,32,33, 35, 37, 39], in single countries [24, 26, 36,37,38,39, 27,28,29,30, 32,33,34,35]. We found no evidence exploring the feasibility of using these tools in other settings and/ or by other groups of health and social care professionals. While it is important to acknowledge the majority of articles reported key stages of DST tool development and testing, the lack of attention given to any aspect of implementation, feasibility and or acceptability in practice is significant.
The scope of the services, funding and legislative requirements vary considerably between countries and care settings [7]. Early consideration of implementation, as outlined by the MRC complex intervention framework [49], is important to ensure adoption and implementation at scale. Paying attention to cultural and contextual differences along with factors that facilitate, or hinder implementation is therefore key to ensuring the benefits of innovation in practice such as DSTs to help improve early detection of infection are fully realised.
Reviewed DSTs largely focused on single types of infection, and most did not specifically explore their use solely in older people [26,27,28, 31,32,33,34, 37, 39]. Although it is established that older people experience common infections including UTI, respiratory tract infection and wound infections more frequently [50], physiological changes associated with aging, and chronic diseases such as diabetes, dementia and stroke [41] mean they often exhibit non-specific signs and symptoms delaying diagnosis and treatment, particularly those in residential care [51, 52]. Consequently, DSTs that have been designed for a specific infection have limited applicability in residential care settings. Additionally, organisational factors such as staff ratios, workload, lack of specialist knowledge, and variable training of nursing assistants and carers [7] means it would not be practical to use multiple DSTs to detect the various types of infection experienced by nursing and care home residents. There is therefore a need for DSTs that detect infection in general for older adults who live in residential care. For example, the Early Detection of Infection Scale (EDIS), one of only two general infection DSTs included in this review [19, 24] is designed for completion by Swedish care workers who ultimately have the most direct contact with residents and tend to be the first people to identify change in psychological and or cognitive behaviour [41, 53].
Our results indicate that the use of DSTs for infection detection in older people is an emergent area of practice, with most studies reporting tool development and testing. Of the four studies reporting DST testing [36,37,38,39], two were based in nursing homes [36, 38], with only one designed for use by nurses, physicians and care workers [36]. The lack of robust evidence regarding the benefits or otherwise of DSTs in this area means that results should be treated with a degree of caution while the included tools are subject to further investigation.
In the UK alone, the National Patient Safety Agency National Reporting & Learning System report 7% of deaths/severe harm incidents in general are related to unrecognised infection [54]. Robust tools are used in acute care settings for early identification of deterioration, e.g. National Early Warning Score (NEWS), but as this review has shown are not commonly developed for use in residential care or by those providing the bulk of care in this setting i.e. nurses and care workers.
In addition to reducing spread of covid-19, evidence suggests training nursing and care home staff to recognise and communicate signs of deterioration through DSTs can provide patient benefit by reducing and/or preventing hospital transfers [53, 55,56,57]. Having improved instructions about what to do next was reported to be the most important action to help improve care of residents with suspected infection by 40% of 204 nurses and care workers recently surveyed in England, Sweden and Spain [58]. While nearly 90% reported they used DSTs for pressure sores, falls and pain, < 50% were aware of use for detecting infection. There is therefore a need for a step-change in how DSTs for infection detection in older people in residential care are developed and implemented in practice.
Limitations
We conducted a comprehensive search using key databases and hand searches. It is possible however that some papers may have been missed. Only papers in English and Spanish were included which means there could be other relevant papers. Grey literature was excluded, and hence it is also possible we could have missed evidence on DSTs that are already used in practice.
Conclusions
This sco** review has explored DSTs available to support detection of infection in older people. DSTs provide an opportunity to ensure a consistent approach to the early detection of infection supporting prompt action and treatment, thus avoiding emergency hospital admissions. The small number of DSTs that have undergone testing in residential care suggests a significant gap in the literature. Relatedly, given that older people often exhibit non-specific signs and symptoms, it was surprising that only two eligible studies reported DSTs to detect infection in general. Despite this, the results suggest that DSTs for infection detection are being used for a broad range of infections, and different settings. However, until consideration is given to their implementation in practice, any attempt to create an optimal validated and tested DST for infection detection will be impeded. This absence may ultimately affect the ability of the workforce to provide more effective and timely care, particularly during the current covid-19 pandemic.
Availability of data and materials
Not applicable.
Abbreviations
- ALP:
-
Alkaline Phosphatase
- ALT:
-
Alanine Aminotransferase
- AUC:
-
Area under the curve
- AUROCC:
-
Area under the receiver-operating characteristics curve
- BUN:
-
Blood Urea Nitrogen
- CI:
-
Confidence interval
- CNS:
-
Central nervous system
- CPK:
-
Creatinine Phosphokinase
- CRP:
-
C-Reactive Protein
- ED:
-
Emergency Department
- Hb:
-
Haemoglobin
- LR:
-
Likelihood ratio
- LTC:
-
Long Term Condition
- NIHSS:
-
National Institute of Health Stroke Scale
- MRC:
-
Medical Research Council
- ROC:
-
Receiver Operating Characteristic
- SAT:
-
Saturation
- SBP:
-
Systolic Blood Pressure
- SIRS:
-
Systemic Inflammatory Response Syndrome
- TC:
-
Total Count
- TP:
-
Total Protein
- USA:
-
United States of Americas
- UTI:
-
Urinary tract infection
- WCC:
-
White cell count
References
Estella Á, Marchante C, Cobos J, Navarro C. Infection in the elderly patient. Consensus recommendations for management in the emergency department. Rev Esp Geriatr Gerontol. 2016;51:120–1.
Smith P, Sherlaw-Johnson C, Ariti C, Bardsley M. Hospital admissions from care homes. Quality Watch The Health Foundation and NuffieldTrust 2015. www.qualitywatch.org.uk. Accessed 13 Jul 2021.
Organisation for Economic Co-operation and Development (OECD). Tackling coronavirus (COVID19): Contributing to a gloabl effort. 2020. https://www.oecd.org/dac/development-assistance-committee/daccovid19statement.htm. Accessed 29 Jun 2020.
Givens JL, Selby K, Goldfeld KS, Mitchell SL. Hospital transfers of nursing home residents with advanced dementia. J Am Geriatr Soc. 2012;60:905–9.
Mitchell SL, Teno JM, Kiely DK, Shaffer ML, Jones RN, Prigerson HG, et al. The clinical course of advanced dementia. N Engl J Med. 2009;361:1529–38.
Ågotnes G, McGregor MJ, Lexchin J, Doupe MB, Müller B, Harrington C. An international map** of medical Care in Nursing Homes. Heal Serv Insights. 2019;12:1178632918825083.
Siegel EO, Backman A, Cai Y, Goodman C, Ocho ON, Wei S, et al. Understanding contextual differences in residential LTC provision for cross-National Research: identifying internationally relevant CDEs. Gerontol Geriatr Med. 2019;5:233372141984059.
Dwyer R, Gabbe B, Stoelwinder JU, Lowthian J. A systematic review of outcomes following emergency transfer to hospital for residents of aged care facilities. Age Ageing. 2014;43:759–66.
Carey N, Alkhamees N, Cox A, Sund-Levander M, Tingström P, Mold F. Exploring views and experiences of how infections are detected and managed in practice by nurses, care workers and manager’s in nursing homes in England and Sweden: a survey protocol. BMJ Open. 2020;10:e038390.
World Health Organization. Infection prevention and control guidance for long-term care facilities in the context of COVID-19: interim guidance. World Health Organization. 2020. https://apps.who.int/iris/handle/10665/331508. Accessed 3 Aug 2021.
Perrotta F, Corbi G, Mazzeo G, Boccia M, Aronne L, D’Agnano V, et al. COVID-19 and the elderly: insights into pathogenesis and clinical decision-making. Aging Clin Exp Res. 2020;32:1599–608.
Yoshikawa TT, Reyes BJ, Ouslander JG. Sepsis in older adults in long-term care facilities: challenges in diagnosis and management. J Am Geriatr Soc. 2019;67:2234–9.
Dwyer R, Stoelwinder J, Gabbe B, Lowthian J. Unplanned transfer to emergency departments for frail elderly residents of aged care facilities: a review of patient and organizational factors. J Am Med Dir Assoc. 2015;16:551–62.
Lemoyne SE, Herbots HH, De Blick D, Remmen R, Monsieurs KG, Van Bogaert P. Appropriateness of transferring nursing home residents to emergency departments: a systematic review. BMC Geriatr. 2019;19:17.
Parameaswari PJ. Tool development in health care research. J Med Allied Sci. 2013;3:3–7.
Kumar A. Review of the steps for development of quantitative research tools. J Adv Pract Nurs. 2015;1:103.
Dreesens D, Kremer L, Burgers J, van der Weijden T. Lost in definitions: reducing duplication and clarifying definitions of knowledge and decision support tools. A RAND-modified Delphi consensus study. Health Policy (New York). 2020;124:531–9.
Ouslander JG, Bonner A, Herndon L, Shutes J. The interventions to reduce acute care transfers (INTERACT) quality improvement program: AN overview for medical directors and primary care clinicians in long term care. J Am Med Dir Assoc. 2014;15:162–70.
Tingström P, Milberg A, Rodhe N, Ernerud J, Grodzinsky E, Sund-Levander M. Nursing assistants: “he seems to be ill” - a reason for nurses to take action: validation of the early detection scale of infection (EDIS). BMC Geriatr. 2015;15:122.
Arksey H, O’Malley L. Sco** studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for sco** reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Altman DG, Bland JM. Diagnostic tests 2: predictive values. BMJ. 1994;309:102.
Altman DG, Bland JM. Diagnostic tests 1: sensitivity and specificity. BMJ. 1994;308:1552.
Hughes C, Ellard DR, Campbell A, Potter R, Shaw C, Gardner E, et al. Develo** evidence-based guidance for assessment of suspected infections in care home residents. BMC Geriatr. 2020;20:1–11.
van Buul LW, Vreeken HL, Bradley SF, Crnich CJ, Drinka PJ, Geerlings SE, et al. The development of a decision tool for the empiric treatment of suspected urinary tract infection in frail older adults: a Delphi consensus procedure. J Am Med Dir Assoc. 2018;19:757–64.
Matsusaka K, Kawakami G, Kamekawa H, Momma H, Nagatomi R, Itoh J, et al. Pneumonia risks in bedridden patients receiving oral care and their screening tool: malnutrition and urinary tract infection-induced inflammation. Geriatr Gerontol Int. 2018;18:714–22.
Rawson TM, Hernandez B, Moore LSP, Blandy O, Herrero P, Gilchrist M, et al. Supervised machine learning for the prediction of infection on admission to hospital: a prospective observational cohort study. J Antimicrob Chemother. 2019;74:1108–15.
García-Tello A, Gimbernat H, Redondo C, Meilán E, Arana DM, Cacho J, et al. Prediction of infection caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae: development of a clinical decision-making nomogram. Scand J Urol. 2018;52:70–5.
Johansson N, Spindler C, Valik J, Vicente V. Develo** a decision support system for patients with severe infection conditions in pre-hospital care. Int J Infect Dis. 2018;72:40–8.
Siaw-Sakyi V. Early wound infection identification using the WIRE tool in community health care settings: an audit report. Br J Community Nurs. 2017;22:S20–7.
Afonso AM, Ebell MH, Gonzales R, Stein J, Genton B, Senn N. The use of classification and regression trees to predict the likelihood of seasonal influenza. Fam Pract. 2012;29:671–7.
Chumbler NR, Williams LS, Wells CK, Lo AC, Nadeau S, Peixoto AJ, et al. Derivation and validation of a clinical system for predicting pneumonia in acute stroke. Neuroepidemiology. 2010;34:193–9.
Gräff I, Goldschmidt B, Glien P, Dolscheid-Pommerich RC, Fimmers R, Grigutsch D. Validity of the Manchester triage system in patients with sepsis presenting at the ED: a first assessment. Emerg Med J. 2017;34:212–8.
Walchok JG, Pirrallo RG, Furmanek D, Lutz M, Shope C, Giles B, et al. Paramedic-initiated CMS Sepsis Core measure bundle prior to hospital arrival: a stepwise approach. Prehospital Emerg Care. 2017;21:291–300.
Jessen MK, Mackenhauer J, Hvass AMW, Ellermann-Eriksen S, Skibsted S, Kirkegaard H, et al. Prediction of bacteremia in the emergency department: an external validation of a clinical decision rule. Eur J Emerg Med. 2016;23:44–9.
Pasay DK, Guirguis MS, Shkrobot RC, Slobodan JP, Wagg AS, Sadowski CA, et al. Antimicrobial stewardship in rural nursing homes: impact of interprofessional education and clinical decision tool implementation on urinary tract infection treatment in a cluster randomized trial. Infect Control Hosp Epidemiol. 2019;40:432–7.
Amland RC, Hahn-Cover KE. Clinical decision support for early recognition of Sepsis. Am J Med Qual. 2016;31:103–10.
McMaughan DK, Nwaiwu O, Zhao H, Frentzel E, Mehr D, Imanpour S, et al. Impact of a decision-making aid for suspected urinary tract infections on antibiotic overuse in nursing homes. BMC Geriatr. 2016;16:81.
Umberger R, Garsee K, Davidson B, Carringer JA, Kuhl D, Muthiah MP. The utility of the Candida score in patients with Sepsis. Dimens Crit Care Nurs. 2016;35:92–8.
Loeb M, Brazil K, Lohfeld L, McGeer A, Simor A, Stevenson K, et al. Effect of a multifaceted intervention on number of antimicrobial prescriptions for suspected urinary tract infections in residents of nursing homes: cluster randomised controlled trial. BMJ. 2005;331:669.
Sund-Levander M, Tingström P. Clinical decision-making process for early nonspecific signs of infection in institutionalised elderly persons: experience of nursing assistants. Scand J Caring Sci. 2013;27:27–35.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. The surviving Sepsis campaign guidelines committee including the pediatric subgroup. Surviving Sepsis campaign: international guidelines for management of severe sepsis and septic shock. Crit Care Med. 2013;39:165–228.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for theuse of innovative therapies in sepsis. The ACCP/SCCM ConsensusConference committee. American College of Chest Physicians/society ofCritical care medicine. Chest. 1992;101:1644–55.
Shapiro NI, Wolfe RE, Wright SB, Moore R, Bates DW. Who needs a blood culture? A prospectively derived and validated prediction rule. J Emerg Med. 2008;35:255–64.
León C, Ruiz-Santana S, Saavedra P, Galván B, Blanco A, Castro C, et al. Usefulness of the “candida score” for discriminating between Candida colonization and invasive candidiasis in non-neutropenic critically ill patients: a prospective multicenter study. Crit Care Med. 2009;37:1624–33.
León C, Ruiz-Santana S, Saavedra P, Almirante B, Nolla-Salas J, Álvarez-Lerma F, et al. A bedside scoring system (“Candida score”) for early antifungal treatment in nonneutropenic critically ill patients with Candida colonization. Crit Care Med. 2006;34:730–7.
Kessler R, Glasgow RE. A proposal to speed translation of healthcare research into practice: dramatic change is needed. Am J Prev Med. 2011;40:637–44.
Organisation for economic co-operation and development (OECD). Tackling wasteful spending on health. 2017. https://read.oecd-ilibrary.org/social-issues-migration-health/tackling-wasteful-spending-on-health_9789264266414-en#page4. Accessed 22 Oct 2021.
Craig P, Dieppe P, Macintyre S, Mitchie S, Nazareth I, Petticrew M. Develo** and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:979–83.
Edwards HE, Chang AM, Gibb M, Finlayson KJ, Parker C, O’Reilly M, et al. Reduced prevalence and severity of wounds following implementation of the champions for skin integrity model to facilitate uptake of evidence-based practice in aged care. J Clin Nurs. 2017;26:4276–85.
Cristofaro PA. Infections and fever in the elderly. J Pod Med Assoc. 2004;94:126–34.
Boockvar K, Lachs M. Predictive value of nonspecific symproms for acute illness in nursing home residents. J Am Geriatr Soc. 2003;51:1111–5.
Li Y, Temkin-Greener H, Shan G, Cai X. COVID-19 infections and deaths among Connecticut nursing home residents: facility correlates. J Am Geriatr Soc. 2020;68:1899–906.
The National Reporting and learning system (NRLS). National reporting and learning system. 2021. https://report.nrls.nhs.uk/nrlsreporting/. Accessed 22 Sep 2021.
Gorges RJ, Konetzka RT. Staffing levels and COVID-19 cases and outbreaks in U.S. nursing homes. J Am Geriatr Soc. 2020;68:2462–6.
Ashcraft AS, Owen DC. From nursing home to acute care: signs, symptoms, and strategies used to prevent transfer. Geriatr Nurs (Minneap). 2014;35:316–20.
Boockvar K, Brodie HD, Lacks M. Nursing assistants detect behavior changes in nursing home residents that precede acute illness: development and validation of an illness warning instrument. J Am Geriatr Soc. 2000;48:1086–91.
Carey N, Cox A, Sund-Levander M, Tingström P, Masot O, Botigue T. Views and experiences of how infections are detected and managed in practice by nurses, care workers, and manager’s in nursing homes in England, Spain and Sweden: an international survey; interim findings. In: Nightingale 2020 Virtual Conference: 27-28th October; 2020.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
The design of the review was carried out by OM, NC, AC, FM. Initial search results were screened, by title/abstract by review team members (TB, JD, MS-L, CM, PT, CB, KH, JM, AM, VP). Discrepancies were moderated by OM, NC, AC, FM. After assessing for eligibility 47 articles were subject to full-text review (OM). Extraction was independently completed by one researcher (OM) then reviewed and discussed with three review team members (NC, AC & FM). All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Masot, O., Cox, A., Mold, F. et al. Decision support-tools for early detection of infection in older people (aged> 65 years): a sco** review. BMC Geriatr 22, 552 (2022). https://doi.org/10.1186/s12877-022-03218-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03218-w