Abstract
Context
Cholangiocarcinoma (CCA), a malignancy of the biliary tract epithelium is of increasing importance due to its rising incidence worldwide. There is a lack of data on cirrhosis in intrahepatic CCA (iCCA) and how it affects overall survival and prognosis.
Objectives
The primary objective of this study was to examine if there were differences in survival outcomes between iCCA patients with concomitant cirrhosis and those without cirrhosis.
Methods
The National Cancer Database (NCDB) was used to identify and study patients with iCCA from 2004 to 2017. The presence of cirrhosis was defined using CS Site-Specific Factor 2 where 000 indicated no cirrhosis and 001 indicated the presence of cirrhosis. Descriptive statistics were utilized for patient demographics, disease staging, tumor, and treatment characteristics. Kaplan-Meier (KM) method with log-rank test and a multivariate logistic regression model was used to assess if the presence of cirrhosis in iCCA was associated with survival status and long-term survival (60 or more months after diagnosis).
Results
There were 33,160 patients with CCA in NCDB (2004–2017), of which 3644 patients were diagnosed with iCCA. One thousand fifty-two patients (28.9%) had cirrhosis as defined by Ishak Fibrosis score 5–6 on biopsy and 2592 patients (71.1%) did not meet the definition for cirrhosis. Although in univariate analyses using KM/log-rank tests showed a survival advantage for non-cirrhotic patients, there was no statistically significant association found between cirrhosis and survival status (OR = 0.82, p = 0.405) or long-term survival (OR = 0.98, p = 0.933) when multivariate analysis was used. iCCA patients with cirrhosis and Stage 1 tumor had the highest median OS (132 months) vs 73.7 months in the non-cirrhotic arm, while patients with stage IV disease who had cirrhosis had half the survival time of those without. Our data thus indicates that the presence of cirrhosis is not an independent prognostic factor for survival.
Similar content being viewed by others
Introduction
Cholangiocarcinoma (CCA) is defined as an epithelial cell malignancy of the biliary tract that can arise from any location within the biliary tract and maintains markers of cholangiocyte differentiation. CCA is classified based on the anatomical location of origin – Intrahepatic, Perihilar and Extrahepatic [1]. Mixed hepatocelluar-cholangiocellular carcinomas (HC-CCA), also called combined HCC according to the WHO classification, were only recently identified as a subset of cholangiocarcinoma [2, 3]. Most CCAs are adenocarcinomas with varying grades of differentiation [4, 5].
Globally, the incidence of CCA shows a wide geographical variability with East Asia having the highest rates and Western Europe having the lowest rates of the disease. There is considerable variation in the incidence rates intra-nationally within East Asian countries with age adjusted incidence ratio for North-East Thailand being 85/100,000 and for North and Central Thailand being 14.5/100,000 [6]. Within the United States, age-adjusted incidence rates of CCA are lowest in Non-Hispanic Caucasians and Blacks with Hispanics and Asians showing the highest rates [7]. Since 1973, we have witnessed a gradual increase in the incidence of intrahepatic CCA (iCCA) with a concomitant decrease in the incidence of carcinoma of unknown primary (CUP). This is likely due to improvement in molecular profiling and the resultant ability to identify the tissue of origin [8].
As we identify more cases of CCA, the importance of prognostication is of prime importance. Not only does it enhance our knowledge about the disease but also helps in risk stratification for selection of treatment modality. Previous studies have shown a neutrophil/lymphocyte ratio greater than 3, multiple metastatic sites, an intrahepatic primary site and presence of liver metastases, the number of sites of advanced disease, a poor Eastern Cooperative Oncology Group (ECOG) performance status (PS) and elevated levels of alkaline phosphatase (ALP) to be associated with worse survival [9, 10, 11, 12]. The presence of cirrhosis in iCCA as a prognostic factor for OS has been a contested topic, with some studies showing a correlation between cirrhosis and worse OS, while other studies showing no statistically significant difference. Hence, our aim is to investigate, using a larger sample size of iCCA patients, if survival is affected by the presence of cirrhosis.
Methods
This study was approved as exempt by the Memorial Healthcare System (MHS) Institutional Review Board (MHS.2021.030). The 2004–2017 National Cancer Database (NCDB) was queried for patients with cholangiocarcinoma (CCA). NCDB is a national hospital-based cancer registry that contains de-identified patient level data, provided to Commission on Cancer (CoC)- accredited cancer programs to help investigators advance cancer research, which in 2012–2014, captured 72.5% of the cancer cases in the United States [13]. Patients with CCA were identified by International Classification of Diseases for Oncology, Third Edition (ICD-O-3)-Oncology morphologic codes 8160/3 (bile duct adenocarcinoma), 8161/3(bile duct cystadenocarcinoma), and 8162/3 (Klatskin tumor). iCCA patients were identified by ICD-O-3 morphologic code 8160/3 with topographical codes C220 (liver) and C221(intrahepatic bile duct). Extrahepatic CCA patients were identified by histology codes 8160/3, 8161/3, 8162/3 with topographical codes C239 (gallbladder) or C240 (extrahepatic bile duct) and not included in the study. The ICD-O-3 has two axis, morphological and topographical code. Morphological code describes the cell type or histology of tumor, while topographical code describes the anatomical site of origin. Patients with iCCA were further categorized by the presence of cirrhosis. The presence of cirrhosis was defined using CS Site Specific Factor 2 where 000 indicated no cirrhosis and 001 indicated the presence of cirrhosis.
Descriptive statistics were utilized for patient demographics, disease staging, tumor, and treatment characteristics. The primary objective of this study was to examine if there were differences in survival outcomes between iCCA patients with concomitant cirrhosis and those without cirrhosis. To assess the study’s primary objective- a multivariate logistic regression was employed. Factors found to be significant in Tables 1 and 2 and based expert knowledge was used as covariates in multivariate logistic regression models. Multivariate logistic regression models, adjusting for socio-demographic and clinical characteristics (insurance type, median income quartile, treatment facility, age, sex, race/ethnicity, Charlson-Deyo comorbidity score, timing of first course treatment, grade, pathological stage and tumor size) was then entered into a stepwise backward selection logistic regression model where variables with p ≥ 0.20 were removed to develop the final multivariate regression models to be used in the assessment of the presence of cirrhosis and its association with survival outcomes (survival status and long-term survival). In the assessment of survival status, the final multivariate model from stepwise backward selection adjusted for median income quartile, grade, and pathological stage. In the assessment of long-term survival, the final multivariate model from stepwise backward selection adjusted for facility type, grade, and pathological stage. This was then used to assess if the presence of cirrhosis among intrahepatic patients was associated with survival status (where patients who died served as the reference group) and long-term survival (survival of 60 or more months after the date of diagnosis).
Overall survival was defined as the time (in months) between the date of diagnosis and date of death or censored at last contact. Kaplan-Meier (KM) method with log-rank test was also used to compare and estimate overall survival rates between iCCA patients with concomitant cirrhosis and those without cirrhosis, as well as stratified by surgical intervention and tumor stage. Statistical significance was defined as p < 0.05. Palliative Care was defined as any care provided to palliate or alleviate symptoms, such as surgery, radiation therapy, systemic therapy (chemotherapy, hormone therapy, or other systemic drugs), and/or other pain management therapy. All analyses were conducted using Stata (version 15.1, StataCorp, College Station, Texas).
Results
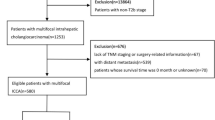
A total of 3644 patients with iCCA underwent biopsy during the NCDB study period of 2004–2017. iCCA patients with known CS Site Specific Factor 2, 1052 patients (28.9%) had cirrhosis as defined by Ishak Fibrosis score 5–6 on biopsy and 2592 patients (71.1%) did not meet the definition for cirrhosis (Fig. 1).
Demographics in iCCA patients by cirrhosis status
Table 1 presents demographics of iCCA patients by cirrhosis status. Most patients were seen at an academic/research program. Patients with cirrhosis presented at a younger age (median age: 63 years vs. 66 years) and had a higher percentage of male patients (66.8% vs 47.8%, p < 0.001). Both groups mostly included White (84.3% vs 83.6%, p = 0.034) and non-Hispanic patients. A higher proportion of patients with cirrhosis were Hispanic [12.4 vs 7.5%, p < 0.001)]). Cirrhotic patients also had a greater percentage of patients with three or more comorbidities at the time of diagnosis as defined by a Charlson Devo Co-Morbidity Score (18.3% vs 5.7%, p < 0.001).
Disease staging and tumor characteristics in iCCA patients by cirrhosis status
Table 2 presents disease staging, grade, and tumor characteristics based on cirrhosis status. Most patients were diagnosed between the years of 2011 to 2017. Statistically significant differences were found for grade, pathologic stage, tumor size and lymphovascular invasion. Cirrhotic patients were more likely to have a higher pathological grade at presentation with more patients presenting with poorly differentiated (Grade III) or undifferentiated (Grade IV) cancer as opposed to non-cirrhotic patients (38.3% vs 41.0%, p < 0.001). Similarly, there was a higher percentage of cirrhotic patients with pathologic stage 4 disease (43.7% vs 37.0%, p = 0.013). Regarding tumor size, cirrhotic patients were more likely to have tumor size less than 5 cm compared to non-cirrhotics (51.3% vs 37.8%, p < 0.001). Lymphovascular invasion was lower for cirrhotic iCCA patients than non-cirrhotic iCCA patients; (25.4% vs 36.7%, p = 0.001).
Treatment characteristics in iCCA patients by cirrhosis status
Table 3 presents treatment characteristics among iCCA patients by cirrhosis status. Overall, non-cirrhotic patients were more likely to undergo surgical intervention at primary site (44.9% vs. 31.7%, p < 0.001) and chemotherapy (52.3% vs. 44.1%, p < 0.001) compared to the cirrhotic cohort. However, both cohorts had similar proportions of patients who received radiation therapy. Compared to non-cirrhotic patients, a higher percentage of cirrhotic iCCA patients were not offered surgery as a part of the first planned treatment compared to non-cirrhotics (56.4% vs 48.0%, p < 0.001). Moreover, cirrhotics were more likely to not receive any treatment compared to non-cirrhotics (16.6% vs 12.6%, p = 0.004). Cirrhotics also had a higher percentage of patients having to wait longer than 60 days until first surgical procedure (30.3% vs 22.4%, p < 0.001), a lower percentage of patients without residual tumor after resection (20.2% vs 32.7%, p < 0.001) and a higher contraindication due to patient risk factors to undergo surgery (10.7% vs 6.4%, p < 0.001). Cirrhotics were more likely to not receive chemotherapy during treatment, and when chemotherapy was administered, cirrhotics were less likely to receive multiagent chemotherapy (27.0% vs 37.0% p < 0.001). No statistically significant difference in palliative care utilization was seen for cirrhotics compared to non-cirrhotics with majority of patients not receiving palliative care, 89.3% for the non-cirrhotic group and 90.1% for the cirrhotic group.
Cirrhosis and its association with survival outcomes
There were 3030 observations with cirrhosis status data for which survival information was present. Specifically, survival information was missing for 606 patients of the study population resulting in missing median survival. Furthermore, 8 patients had an elapsed time from the date of initial diagnosis to the date of last contact or death of 0 months and as such, could not be accounted for. Hence, the median OS was not calculated for a total of 614 patients.
Among the entire population of CCA patients with known survival status, 84.4% (n = 39,406) died. Among iCCA patients with known survival status, 72.4% (n = 1564) of iCCA patients without cirrhosis patients died compared to 78.7% (n = 690) of iCCA patients with cirrhosis. iCCA patients with concomitant cirrhosis had a median OS half that of patients without cirrhosis (8.9 vs. 18.0 months, P < 0.001) (Fig. 2 and Table 4). We further examined median OS among iCCA patients with and without cirrhosis stratified by surgical intervention received and tumor stage. Among both the cirrhosis and non-cirrhosis cohorts, patients who underwent surgery had a significantly longer median overall survival (OS) time. However, results suggest a survival advantage for the non-cirrhosis cohort (41.2 months) compared to the cirrhosis cohort (39.7 months) (p < 0.001), with regards to surgical intervention (Fig. 3 and Table 5). When median OS stratified by tumor stage was assessed, results indicated that the cirrhosis cohort with Stage I tumor had the highest median OS time (132 months). However, the upper limit of the 95% confidence interval for the aforementioned cohort could not be estimated. Similarly, among the non-cirrhosis cohort, patients with Stage I tumor had the highest median OS time (73.7 months). Patients with the highest tumor stages among both the cirrhosis and non-cirrhosis cohorts had the lowest median OS (cirrhosis with stage IV: 5.6 months vs. non-cirrhosis with stage IV: 12.2 months) (p < 0.001). Patients with cirrhosis and stage IV disease had half the survival time of patients without cirrhosis and stage IV disease (Fig. 4 and Table 6).
In univariate analyses using the KM method with log-rank tests, results consistently showed a survival advantage for non-cirrhotic patients. However, when a multivariate approach was used to assess survival outcomes and its association with the presence of cirrhosis among iCCA, there were no statistically significant associations found between cirrhosis and survival status (OR = 0.82, p = 0.405) (Table 7) or long-term survival (OR = 0.98, p = 0.933) (Table 7). In conclusion, while the initial results suggest that patients without cirrhosis had a survival advantage as measured by median overall survival in months, the presence of cirrhosis is not an independent prognostic factor of survival status or long-term survival.
Discussion
Despite groundbreaking advances in the field of oncology over the last few decades, surgical resection remains the treatment of choice for all subtypes of CCA. However, early surgical treatment is often limited by the presence of concomitant cirrhosis. As known widely, surgical intervention in cirrhosis is associated with a risk of decompensation as defined by the development of ascites, variceal hemorrhage and hepatic encephalopathy and worsening jaundice. Cirrhosis not only complicates post-surgical recovery but also increases overall mortality for the patient, with 1 month and 3-month mortality rates being reported as high as 17 and 21% respectively [14].
The average life expectancy for a patient with decompensated cirrhosis is 2 years in comparison to 12 years for compensated cirrhosis [15]. Unfortunately, unlike in the case of hepatocellular carcinoma, liver transplantation as a treatment modality has been established for only a select group of patients with perihilar cholangiocarcinoma [16]. Patients with iCCA have however not shown to benefit from this intervention due to high rates of recurrence and poor long-term survival, with the 5-year patient survival varying from 0 to 42% [17]. As such, the need for a prognostic marker in the setting of iCCA is of prime importance to help guide treatment and goals of care.
The presence of cirrhosis in the setting of iCCA has been a contested topic in terms of its importance as a factor for prognostication with previous studies showing conflicting results. As early as 2011, a study of 132 patients with iCCA, of which 32% had concomitant cirrhosis, showed cirrhosis to be an independent factor for poor prognosis following surgical resection [18]. Another study done in 2017 with patient population of 106, of which 23.6% had concomitant cirrhosis, showed no difference in prognosis between the cirrhotic and non-cirrhotic arms [19]. A SEER (Surveillance, Epidemiology and End Results) database study done in 2020 with 512 patients showed that the presence of advanced fibrosis (defined by Ishak fibrosis score 5–6) was associated with worse cancer-specific survival across follow up periods (HR 1.49 (1.13–1.96, p = 0.005); HR 1.44 (1.14–1.83, p = 0.002) and HR 1.45 (1.15–1.83, p = 0.002) for 12, 36 and 60 months, respectively [20]. A recent multicenter retrospective study comparing outcomes of patients with liver cirrhosis undergoing liver transplant or surgical intervention in patients with iCCA or combined hepatocellular cholangiocarcinoma, found that survival improved after liver resection in patients with cirrhosis if tumor size was less than 5 cm [21]. Another retrospective analysis of 156 patients after surgical resection, the presence of cirrhosis did not have a significant impact on survival [22]. In another study of 184 patients published in 2020, cirrhosis did not have a significant difference in survival in iCCA patients (32 vs 33 months, p-value = 0.8) [23].
To our knowledge, this is one of the largest retrospective studies, examining a total of 3644 patients with iCCA using the NCDB data to analyze the impact of cirrhosis in patients with iCCA. After adjusting for socio-demographic and clinical characteristics, results showed that the presence of cirrhosis among iCCA patients was not associated with survival status or long-term survival, reflecting similar findings as some of the studies mentioned above. iCCA patients with cirrhosis had OR of 0.71, but when adjusted for median income quartile, grade and pathological stage, there was no statistical significance, with OR 0.82 (0.52–1.31, p = 0.405). Long term survival (survival more than 60 months after diagnosis) yielded similar results with no statistically significant differences.
Interestingly, after stratifying by surgical intervention, iCCA patients with cirrhosis benefitted the most from surgical intervention. When stratifying by stage, iCCA patients with cirrhosis exhibited lower median OS for stage IV disease compared to patients without cirrhosis. Among both the cirrhosis and non-cirrhotic cohorts, patients who underwent surgery had a significantly longer median overall survival (OS) time. In the cirrhosis cohort, median overall survival was 39.7 months for those who underwent surgical intervention, compared to 5.1 months for those who did not. Similarly, in the non-cirrhosis cohort, those who underwent surgical intervention had a median OS of 41.2 months compared to 8.0 months. Our results suggest a slightly higher survival advantage for the non-cirrhotic cohort (41.2 months) compared to the cirrhosis cohort (39.7 months) (p < 0.001) regarding surgical intervention. In terms of presence of cirrhosis by tumor stage, the cirrhosis cohort with stage IV had a median OS of 5.6 months, compared to non-cirrhosis cohort with stage IV disease, which had a median OS of 12.2 months, indicating that patients with cirrhosis and stage IV disease had half the survival of those with stage IV disease without cirrhosis.
Based on our data, cirrhosis status may not uniquely explain survival status or long-term survival, but rather other clinical characteristics/markers within the cirrhotic group may affect survival status. For example, as seen in Table 2, a lower proportion of iCCA patients with cirrhosis had tumor size greater than or equal to 5 cm (48.8% vs. 62.2%) – this is likely due to regular screening/imaging protocols in cirrhotics leading to detection of smaller tumors. Cirrhotics had a higher percentage of poorly differentiated or undifferentiated tumors and a higher percentage of stage 4 disease, lower percentage of surgical intervention and chemotherapy received (including multiagent chemotherapy) with higher contraindications to surgery due to risk factors, and lower percentage of lymphovascular invasion. Future research needs to be done to further disentangle possible associations (such as prospective cohort studies) especially considering the limitations of using a cancer registry.
Socio-demographic factors can contribute to cancer survival, as reported in recent studies. For example, studies have documented that race/ethnicity, income, type of insurance resulted in failure to administer recommended chemotherapy. As demonstrated by Barrera et al, studies using the NCDB for common malignancies such as breast, lung and colon cancer, found that the aforementioned characteristics could impact receipt of chemotherapy [24].
Hepatic surgical resection is recommended by the American association for the Study of Liver Diseases (ASSLD) and European Association for the Study of Liver (EASL) for early-stage hepatocellular carcinoma– Barcelona Clinic Liver Cancer staging system (BCLC) Stage 0/A, it is contraindicated if there is presence of clinically significant portal hypertension or decompensated cirrhosis. As such, in the absence of liver transplantation, the initiation of palliative care in such patients becomes paramount. However, previous data has shown palliative care services remain heavily underutilized in patients with advanced liver disease who are not candidates for liver transplant. A single center retrospective study of 102 patients showed that of all patients who had cirrhosis and were denied transplant candidacy, only 11% received a palliative care consultation. Our study corroborates this finding as well. Although there was no statistically significant difference in the utilization of palliative care between the two arms, the utilization of palliative care was low for both groups, 10.7% for the non-cirrhotic vs 9.9% for the cirrhotic group, indicating the need to address this gap in the future.
Limitations
Misclassification of CCA subtypes based on ICD-O coding is a potential limitation in our study as previous studies have shown that perihilar CCA (pCCA) is frequently misclassified as iCCA instead of eCCA, which could lead to overestimation of iCCA incidence and misclassification of the data. For instance, in a study conducted by Welzel et al., 91% of pCCA were incorrectly coded as iCCA, resulting in overestimation of iCCA incidence by 13% and underestimation of eCCA by 15% [25]. Another potential limitation is the potential for selection bias as our study only included patients who underwent a liver biopsy to determine cirrhosis status. Only 3644 out of 33,160 iCCA patient underwent liver biopsy (10.9%). This population may exhibit systematic differences from those who did not have a liver biopsy. For example, those receiving a liver biopsy may have been more likely to be surgical candidates as liver biopsies are often performed intra-operatively at the time of resection. Moreover, with the use of a cancer registry, there is always potential for miscoding and potential for missing patient data.
Conclusion
In our study of 3644 patients with iCCA who underwent liver biopsy during the time of staging, there was no statistically significant difference in survival status or long-term survival between iCCA patients with cirrhosis compared to those without cirrhosis. When stratifying for surgical intervention, both groups tended to have improved median OS when surgery was performed, with slight advantage of the non-cirrhotic arm. When stratifying for stage, stage IV cirrhotic iCCA patients tended to have worse median OS than non-cirrhotic iCCA patients.
Availability of data and materials
The authors confirm that the data supporting our findings are available within the article and within. For further details regarding the data, please contact the corresponding author.
Abbreviations
- CCA:
-
Cholangiocarcinoma
- HC-CCA:
-
hepatocelluar-cholangiocellular carcinomas
- CUP:
-
Carcinoma of Unknown Primary
- ECOG:
-
Eastern Cooperative Oncology Group
- ALP:
-
Alkaline Phosphatase
- PS:
-
Performance Status
- OS:
-
Overall survival
References
Razumilava N, Gores GJ. Cholangiocarcinoma. Lancet. 2014;383(9935):2168–79. https://doi.org/10.1016/S0140-6736(13)61903-0.
Roskams T. Liver stem cells and their implication in hepatocellular and cholangiocarcinoma. Oncogene. 2006;25(27):3818–22. https://doi.org/10.1038/sj.onc.1209558.
de Jong MC, Nathan H, Sotiropoulos GC, et al. Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment. J Clin Oncol. 2011;29(23):3140–5. https://doi.org/10.1200/JCO.2011.35.6519.
Blechacz B, Gores GJ. Cholangiocarcinoma: advances in pathogenesis, diagnosis, and treatment. Hepatology. 2008;48(1):308–21. https://doi.org/10.1002/hep.22310.
Nakanuma Y, Sato Y, Harada K, Sasaki M, Xu J, Ikeda H. Pathological classification of intrahepatic cholangiocarcinoma based on a new concept. World J Hepatol. 2010;2(12):419–27. https://doi.org/10.4254/wjh.v2.i12.419.
Khan SA, Tavolari S, Brandi G. Cholangiocarcinoma: epidemiology and risk factors. Liver Int. 2019;39(Suppl 1):19–31. https://doi.org/10.1111/liv.14095.
Tyson GL, El-Serag HB. Risk factors for cholangiocarcinoma. Hepatology. 2011;54(1):173–84. https://doi.org/10.1002/hep.24351.
Forty-Year Trends in Cholangiocarcinoma Incidence in the U.S.: Intrahepatic Disease on the Rise. Accessed 9 Oct 2021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4861366/
Park I, Lee JL, Ryu MH, et al. Prognostic factors and predictive model in patients with advanced biliary tract adenocarcinoma receiving first-line palliative chemotherapy. Cancer. 2009;115(18):4148–55. https://doi.org/10.1002/cncr.24472.
McNamara MG, Templeton AJ, Maganti M, et al. Neutrophil/lymphocyte ratio as a prognostic factor in biliary tract cancer. Eur J Cancer. 2014;50(9):1581–9. https://doi.org/10.1016/j.ejca.2014.02.015.
Peixoto RD, Renouf D, Lim H. A population based analysis of prognostic factors in advanced biliary tract cancer. J Gastrointest Oncol. 2014;5(6):428–32. https://doi.org/10.3978/j.issn.2078-6891.2014.081.
Multivariate prognostic factors analysis for second-line chemotherapy in advanced biliary tract cancer. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4007244/. Accessed 9 Oct 2021.
Boffa DJ, Rosen JE, Mallin K, Loomis A, Gay G, Palis B, et al. Using the national cancer database for outcomes research a review. JAMA Oncol. 2017:3.
Farnsworth N, Fagan SP, Berger DH, Awad SS. Child-Turcotte-Pugh versus MELD score as a predictor of outcome after elective and emergent surgery in cirrhotic patients. Am J Surg. 2004;188(5):580–3. https://doi.org/10.1016/j.amjsurg.2004.07.034.
EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis - Journal of Hepatology. https://www.journal-of-hepatology.eu/article/S0168-8278(18)31966-4/fulltext. Accessed 2018.
Martin P, DiMartini A, Feng S, Brown R Jr, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatol. 2014;59(3):1144-65. https://doi.org/10.1002/hep.26972.
Hashimoto K, Miller CM. Liver transplantation for intrahepatic cholangiocarcinoma. J Hepato-Biliary-Pancreatic Sci. 2015;22(2):138–43. https://doi.org/10.1002/jhbp.159.
Li YY, Li H, Lv P, et al. Prognostic value of cirrhosis for intrahepatic cholangiocarcinoma after surgical treatment. J Gastrointest Surg. 2011;15(4):608–13. https://doi.org/10.1007/s11605-011-1419-8.
Jeong S, Gao L, Tong Y, et al. Prognostic impact of cirrhosis in patients with intrahepatic cholangiocarcinoma following hepatic resection. Can J Gastroenterol Hepatol. 2017;2017:6543423. https://doi.org/10.1155/2017/6543423.
Levy NA, Kern G, Shepshelovich D, Shibolet O, Hershkoviz R, Isakov O. Effect of liver fibrosis on survival in patients with intrahepatic cholangiocarcinoma: a SEER population-based study. Oncotarget. 2020;11(47):4438–47. https://doi.org/10.18632/oncotarget.27820.
De Martin E, Rayar M, Golse N, et al. Analysis of liver resection versus liver transplantation on outcome of small intrahepatic cholangiocarcinoma and combined hepatocellular-cholangiocarcinoma in the setting of cirrhosis. Liver Transpl. 2020;26(6):785–98. https://doi.org/10.1002/lt.25737.
Jesper D, Heyn SG, Schellhaas B, et al. Effects of liver cirrhosis and patient condition on clinical outcomes in intrahepatic cholangiocarcinoma: a retrospective analysis of 156 cases in a single center. Eur J Gastroenterol Hepatol. 2018;30(5):552–6. https://doi.org/10.1097/MEG.0000000000001036.
Tovoli F, Guerra P, Iavarone M, et al. Surveillance for hepatocellular carcinoma also improves survival of incidentally detected intrahepatic cholangiocarcinoma arisen in liver cirrhosis. Liver Cancer. 2020;9(6):744–55. https://doi.org/10.1159/000509059.
Becerra AZ, Eure D, Fungwe C, Justiniano CF, Aquina CT. To risk adjust or not to risk adjust for sociodemographics—that is the question, so what is the answer? J Hosp Manag Heal Policy. 2020:4.
Welzel TM, McGlynn KA, Hsing AW, O'Brien TR, Pfeiffer RM. Impact of classification of hilar cholangiocarcinomas (Klatskin tumors) on the incidence of intra- and extrahepatic cholangiocarcinoma in the United States. J Natl Cancer Inst. 2006;98(12):873-5. https://doi.org/10.1093/jnci/djj234.
Acknowledgements
Not applicable.
Statement of consent to participate
A waiver of consent was obtained from the Institutional Review Board at Memorial Healthcare System.
Data availability statement
All the data provided in the manuscript is available in the National Cancer Database. Please contact the corresponding author for further information and inquiries.
Funding
No financial support was utilized for this study.
Author information
Authors and Affiliations
Contributions
Nimish Thakral envisaged the study design, drafted the IRB protocol, and was involved in drafting the manuscript. Teresita Gonzalez, Olger Nano, Sang-Ha Shin were involved in drafting the manuscript. Shenae Samuels did the statistical analysis. Atif Hussein provided mentorship for the research idea and was involved in facilitating the project. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All experimental protocols were approved by the Institutional Review Board of Memorial Healthcare System. All methods were carried out in accordance with relevant guidelines and regulations. Data was obtained from the National Cancer Database, containing no identifiable patient information. The human data used in the study was anonymized.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Thakral, N., Gonzalez, T., Nano, O. et al. Cirrhosis in intrahepatic cholangiocarcinoma: prognostic importance and impact on survival. BMC Gastroenterol 23, 151 (2023). https://doi.org/10.1186/s12876-023-02710-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-023-02710-w